Abstract
This pilot study examined preliminary effects of Parent Skills Training with Behavioral Couples Therapy on children’s behavioral functioning. Participants were men (N = 30) entering outpatient alcohol treatment, their female partners, and a custodial child between 8 and 12 years of age. Couples were randomly assigned to one of three equally intensive conditions: (a) Parent Skills with Behavioral Couples Therapy (PSBCT), (b) BCT (without parent training), and (c) Individual-Based Treatment (IBT; without couples-based or parent skills interventions). Parents completed measures of child externalizing and internalizing behaviors at pretreatment, post-treatment, 6-and 12-month follow-up; children completed self-reports of internalizing symptoms at each assessment. Only PSBCT participants reported significant effects on all child measures throughout the 12-month follow up. PSBCT showed medium to large effects in child functioning relative to IBT, and small to medium effects relative to BCT from baseline through follow up. Effect sizes suggest clinically meaningful differences between PSBCT and both BCT and IBT that warrant further empirical evaluation of BCT with parent training for alcohol-abusing men and their partners.
Keywords: children of alcoholics, parent training, behavioral couples therapy, alcoholism treatment, child functioning
It has been widely documented that children living with an alcohol-abusing parent (COAs) are more likely than their peers to exhibit behavioral problems that encompass both internalizing and externalizing symptoms (e.g., Hussong, Wirth, Edwards, Curran, Chassin, & Zucker, 2007). Although many factors contribute to these problems, inadequate parenting has been strongly linked to increased risks for COAs (e.g., Wells, 2006). Family-based treatments that involve both an alcohol-abusing parent and his/her partner can have even stronger positive effects on COAs than individual-based approaches (Kelley & Fals-Stewart, 2002). However, because most parents who enter substance abuse treatment are reluctant to involve their children in services (Fals-Stewart, Fincham, & Kelley, 2004), interventions that do not directly involve COAs, but nonetheless improve the family environment may hold the most potential for effecting change.
A promising approach is Behavioral Couples Therapy (BCT) for substance-abusing patients and their partners, which has been shown to reduce substance use and improve family adjustment (Fals-Stewart, O’Farrell, Birchler, Cordova, & Kelley, 2005). Moreover, Kelley and Fals-Stewart (2002, 2007) found children of substance-abusing fathers and nonsubstance-abusing mothers receiving BCT displayed greater psychosocial adjustment across a 12-month follow up than children of parents in individual- or couples-based attention control treatment. Younger children showed greater improvements than adolescent siblings, suggesting preadolescence as a critical developmental period to intervene with parents.
Although these findings are important in their own right, it is plausible that adding a parent component to BCT might further enhance benefits to children. Parent training has well-established effectiveness at improving child behavior (Serketich & Dumas, 1996). This pilot study sought to develop and test a new, hybrid treatment of parent training with BCT. We hypothesized that relative to children of parents participating in Individual-Based Treatment (IBT) or BCT, children of alcohol-abusing fathers participating in PSBCT with nonsubstance-abusing partners would demonstrate improved functioning as rated by mothers, fathers, and children. We also examined whether PSBCT would yield clinically meaningful effects compared to IBT and BCT, which would support the need for a larger randomized trial of PSBCT for alcoholic parents.
1. Methods
Participants were male patients entering outpatient treatment for an alcohol use disorder. Men were eligible for the study if they (a) were at least 18 years of age; (b) met DSM-IV criteria for alcohol abuse or dependence; (c) were married (>1 year) or cohabitating (>2 years) with a female partner at the time of admission; (d) the female partner did not meet DSM-IV criteria for substance abuse or dependence; and (e) had legal guardianship of at least one child 8 to 12 years old living in the home. If more than one child was eligible, one target child was randomly selected for participation. DSM-IV eligibility criteria were determined by the Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon, & Williams, 1995). Consecutively admitted males (n = 51) who met initial eligibility screening were invited to participate in informational sessions. Of these, 15 patients or their partners (29%) met at least one exclusion criteria and 6 patients or partners (12%) declined to participate. The final sample included 30 father-mother-child triads.
Children’s adjustment
The Internalizing and Externalizing broadband T-scores from the Child Behavior Checklist (CBCL; Achenbach, 1991) were used to assess parents= perceptions of children’s problem behavior. The CBCL has high internal consistency, test-retest reliability, and concurrent validity with other measures of child problem behaviors. The Children’s Depression Inventory (CDI; Kovacs, 1992) was used to assess children’s depression. The CDI is a 27-item self-report measure with strong reliability (α=.86) and validity for children over 7 years. The Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds & Paget, 1983) was used as a psychometrically sound, self-report measure of worry and anxiety for children 6 to 19 years.
Substance use
The Timeline Followback Interview (TLFB; Sobell & Sobell, 1996) uses a calendar assessment to determine Percent Days Abstinent (PDA) from drinking and other drug use over a given time period, excluding jail or hospital stays.
Within one week of entering treatment, alcohol-abusing fathers and their partners completed self-report and clinically-structured interviews at baseline, posttreatment, 6-, and 12-month follow up. After baseline assessment, participants first were randomized to one of three equally intensive treatments: (a) PSBCT, (b) BCT, or (c) IBT, then were randomly assigned to one therapist who delivered the full course of that treatment. Master’s level therapists experienced in BCT and coping skills therapy for substance abuse were trained and certified by therapy developers to deliver all treatments.
The experimental and control conditions consisted of 24 total 60-minute sessions: 12 weekly sessions of either BCT, PSBCT, or IBT, which were interleaved with 12, weekly standard care sessions of individual, cognitive-behavioral therapy for substance abuse with identified male patients. Primary elements of the treatment conditions were as follows:
Behavioral Couples Therapy (BCT)
Both partners attended 12 manualized BCT sessions, which included collecting urine screens, reviewing the previous week’s homework, improving communication and problem-solving skills, and reinforcing sobriety (O’Farrell & Fals-Stewart, 2006). No parent skills training interventions were provided. Parent Skills Behavioral Couples Therapy (PSBCT). Both partners attended 12 PSBCT sessions, which included eight core BCT sessions and four parent skills training sessions. The parenting component was adapted from an established treatment with documented effectiveness at improving parent and child functioning (McMahon & Forehand, 2003). Individual-Based Therapy (IBT). Only male patients participated in IBT, which included 12 individual-based coping skills sessions modified from Monti and colleagues’ (1989) cognitive-behavioral treatment for alcoholism.
Data Analysis
Growth curve modeling was used as the primary analytic tool, estimated within a linear mixed effects model framework. Pairwise contrasts compared differences in children’s adjustment between PSBCT versus (vs.) IBT, and PSBCT vs. BCT at each follow up by moving the intercept for each assessment point. Effect sizes were determined using formulae described in Xu (2003) for measuring explained variance in mixed linear models. As Table 3 notes, differences between PSBCT and IBT and BCT outcomes were interpreted using effect size r (Cohen, 1998), consistent with other pilot studies of substance abuse treatment (O’Farrell, Murphy, Alter & Fals-Stewart, 2007).
Table 3.
z Statistics (and Effect Sizes--rs) for Pairwise Comparisons of PSBCT with IBT and with BCT
| Assessment Period | |||
|---|---|---|---|
| Rater and Contrast | Posttreatment | 6-month | 12-Month |
| EXTERNALIZING BEHAVIOR | |||
| Mother–CBCL Externalizing | |||
| PSBCT vs. IBT | 1.52 (.31) | 1.17 (.25) | 1.20 (.26) |
| PSBCT vs BCT | 0.87 (.21) | 0.89 (.23) | 0.84 (.20) |
| Father–CBCL Externalizing | |||
| PSBCT vs. IBT | 1.60 (.35) | 1.18 (.25) | 1.23 (.27) |
| PSBCT vs BCT | 0.88 (.21) | 0.92 (.22) | 0.86 (.20) |
| INTERNALIZING BEHAVIOR | |||
| Mother–CBCL Internalizing | |||
| PSBCT vs. IBT | 1.21 (.26) | 1.26 (.28) | 1.39 (.31) |
| PSBCT vs BCT | 0.86 (.21) | 0.88 (.23) | 0.89 (.24) |
| Father–CBCL Internalizing | |||
| PSBCT vs. IBT | 1.22 (.26) | 1.19 (.25) | 1.24 (.27) |
| PSBCT vs BCT | 0.81 (.18) | 0.83 (.20) | 0.81 (.19) |
| Child–CDI | |||
| PSBCT vs. IBT | 2.05* (.43) | 2.17* (.46) | 2.09* (.44) |
| PSBCT vs BCT | 1.28 (.28) | 1.20 (.25) | 1.21 (.26) |
| Child–RCMAS | |||
| PSBCT vs. IBT | 2.10* (.45) | 2.07* (.43) | 2.02* (.41) |
| PSBCT vs BCT | 1.20 (.26) | 0.89 (.21) | 1.17 (.24) |
p < .05 (without an alpha correction).
Note. Cohen’s (1998) characterizations were to interpret effect size r: small effect: r ≥.10; medium effect: r ≥.30; and large effect: r ≥.50 r ≥ .20 was interpreted as clinically meaningful.
The majority of couples (n = 25, 83%) provided complete data at all assessments. Of the remaining couples, 2 (7%) had incomplete data from one or both partners, and 3 (10%) were lost to contact. Missing data were handled by data imputation procedures in multilevel models described in Goldstein (2003) to account for uncertainty in true values of missing values by including a correction factor when estimating fixed and random parameters.
2. Results
Examination of participant background characteristics, presented in Table 1, revealed no significant differences across the three conditions on any of these variables (all ps > .30).
Table 1.
Pretreatment Characteristics of PSBCT, BCT, and IBT Participants
| Characteristic | PSBCT | BCT | IBT |
|---|---|---|---|
| Mean (SD)
|
|||
| Male partners’ age (in years) | 33.4 (5.1) | 34.6 (4.9) | 34.2 (4.4) |
| Female partners’ age (in years) | 33.2 (5.4) | 32.8 (5.4) | 33.1 (5.2) |
| Male partners education (in years) | 12.8 (1.3) | 13.0 (1.1) | 12.9 (1.2) |
| Female partners’ education (in years) | 13.7 (1.4) | 13.5 (1.5) | 13.5 (1.4) |
| Years married or cohabiting | 7.4 (2.9) | 7.2 (3.3) | 7.3 (3.4) |
| Children’s age | 8.9 (2.1) | 9.0 (2.0) | 8.8 (2.2) |
| Number of children | 2.3 (1.3) | 2.2 (1.4) | 2.4 (1.3) |
| Annual family income (in $1,000s) | 35.2 (15.6) | 34.0 (14.9) | 34.6 (15.3) |
|
|
|||
| Number (%)
|
|||
| Male children | 6 (50) | 5 (50) | 5 (50) |
| Male partners’ race/ethnicity | |||
| White | 7 (70) | 6 (60) | 6 (60) |
| African-American | 2 (20) | 3 (30) | 2 (20) |
| Hispanic | 1 (10) | 0 (10) | 1 (10) |
| ‘Other’ | 0 (10) | 1 (10) | 1 (10) |
| Female partners’ race/ethnicity | |||
| White | 7 (70) | 7 (70) | 6 (60) |
| African-American | 1 (10) | 1 (10) | 2 (20) |
| Hispanic | 0 (0) | 1 (10) | 1 (10) |
| ‘Other’ | 2 (20) | 1 (10) | 2 (20) |
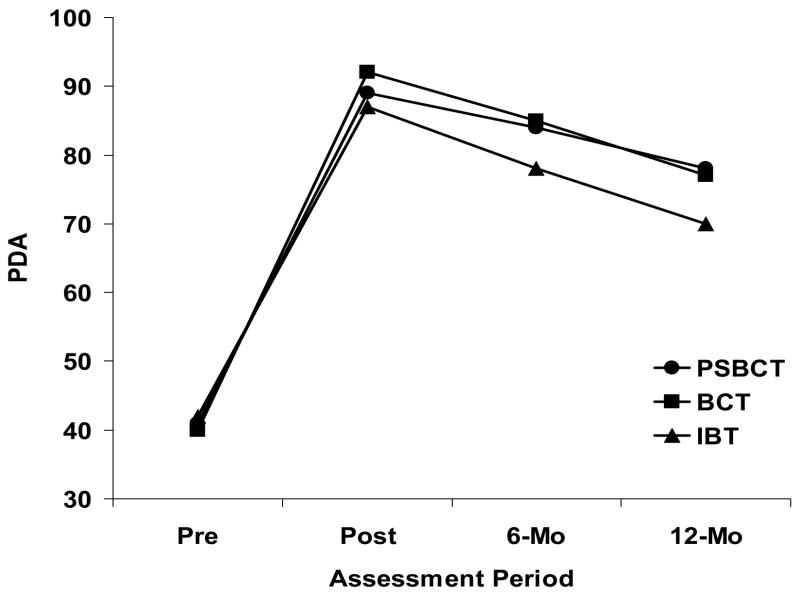
Drinking
PDA for men in PSBCT, BCT, and IBT at baseline, posttreatment, and 12-month follow-up are presented in Figure 1. As expected, pairwise comparisons revealed small differences on PDA at baseline between PSBCT vs. IBT (z = .24, ns; r = .03) and PSBCT vs. BCT (z = .11, ns; r = .02). Similarly, there were small differences at posttreatment for PSBCT vs. IBT (z = -.28, ns, r = .03) and PSBCT vs. BCT (z = .39, ns, r = .03), and PSBCT vs. BCT at 6- (z = .13, r = .02) and 12-month follow-up (z = .10, ns, r = .02). Largest differences were found for PSBCT vs. IBT at 6- (z = 1.08, ns, r =.23) and 12-month follow-up (z = 1.40, ns, r = .33).
Figure 1.
Fathers’ Percent Days Abstinent (PDA) by Treatment Condition at Each Assessment.
Note. The PDA measurement interval at pretreatment was the past 12 months; the interval for each follow up was the time since the previous interview.
Children’s Adjustment
Children’s externalizing and internalizing behavior as rated by mothers and fathers (CBCL Internalizing- and Externalizing T-scores) and children (CDI and RCMAS T-scores) are reported in Table 2. Only children of PSBCT participants showed significant improvements from baseline to each follow-up assessment for all measures (all ps < .05). BCT yielded similar significant differences at posttreatment, though only parent-report of externalizing behaviors were sustained at 6- and 12-month follow up. IBT had no significant effects on child behavior functioning over time.
Table 2.
Mean (SD) Ratings of Child Functioning by Mothers, Fathers, and Children
| Assessment Period | ||||
|---|---|---|---|---|
| Rater and condition | Pretreatment | Posttreatment | 6-month | 12-month |
| EXTERNALIZING BEHAVIOR | ||||
| CBCL Externalizing T-scores | ||||
| Mother | ||||
| PSBCT | 62.1 (11.6) | 52.0 (11.5) | 53.3 (9.3) | 54.0 (10.9) |
| BCT | 64.4 (12.3) | 56.4 (11.0) | 57.9 (10.6) | 57.8 (10.7) |
| IBT | 63.5 (13.0) | 60.4 (12.1) | 60.9 (11.8) | 61.0 (12.9) |
| Father | ||||
| PSBCT | 60.2 (13.4) | 52.5 (11.5) | 52.8 (11.6) | 53.0 (11.0) |
| BCT | 61.3 (10.6) | 57.2 (10.6) | 56.9 (12.6) | 57.5 (10.4) |
| IBT | 61.0 (12.4) | 61.2 (12.1) | 60.2 (13.0) | 59.9 (10.9) |
|
| ||||
| INTERNALIZING BEHAVIOR | ||||
| CBCL Internalizing T-scores | ||||
| Mother | ||||
| PSBCT | 58.4 (10.6) | 50.0 (11.1) | 50.2 (11.3) | 51.0 (10.2) |
| BCT | 58.3 (11.6) | 54.2 (9.7) | 54.3 (12.3) | 55.3 (11.7) |
| IBT | 59.9 (11.0) | 56.5 (12.2) | 57.2 (11.3) | 57.9 (11.0) |
| Father | ||||
| PSBCT | 57.7 (12.3) | 50.1 (10.2) | 49.9 (12.9) | 50.9 (10.3) |
| BCT | 58.4 (10.8) | 53.9 (10.9) | 54.6 (11.9) | 54.8 (11.4) |
| IBT | 57.1 (10.9) | 56.1 (11.8) | 57.2 (13.0) | 57.0 (11.8) |
| Child | ||||
| CDI | ||||
| PSBCT | 63.4 (9.3) | 48.4 (10.2) | 49.6 (9.1) | 50.3 (10.3) |
| BCT | 64.7 (10.2) | 54.0 (9.3) | 55.0 (10.2) | 56.1 (11.6) |
| IBT | 65.0 (11.0) | 58.3 (10.4) | 58.8 (10.0) | 60.7 (11.1) |
| RCMAS | ||||
| PSBCT | 65.3 (10.2) | 49.2 (9.3) | 50.2 (10.1) | 51.0 (9.6) |
| BCT | 64.4 (11.6) | 54.4 (10.2) | 55.0 (9.6) | 55.9 (10.0) |
| IBT | 64.9 (9.9) | 58.8 (10.0) | 59.2 (10.2) | 60.6 (11.6) |
Table 3 shows z-statistic and effect size estimates for pairwise comparisons of PSBCT vs. IBT and PSBCT vs. BCT. Effect sizes for PSBCT vs. IBT comparisons were medium to large; PSBCT vs. BCT effect sizes were small to medium, with most surpassing .20.
3. Discussion
This pilot study found that PSBCT versus IBT showed medium-to-large effect size differences in child functioning across 12-month follow up (rs range from .25 to .46). These effect sizes are clinically significant, and comparable to those found in other published studies that favor family-based treatments over individual-based treatments for substance use (O’Farrell et al., 2007). The majority of observed effect sizes between PSBCT and BCT were also clinically meaningful (r>.20) across the one-year follow up. Importantly, only PSBCT participants showed significant improvements from baseline to each follow up on all child measures (p<.05). Although preliminary, results suggest that adding parenting skills to BCT for alcoholism may improve child behavior and maintain these effects over time, which is particularly critical during the transition from preadolescence to adolescence for these high-risk youth.
The present study had many strengths: sustained trends in expected directions and clinically meaningful effects; use of a 3-group, randomized clinical trial; multiple raters of child outcomes in two distinct domains; well-established measures; and assessment at four points across a one year follow-up period. High feasibility also was evidenced. The majority (84%) of eligible couples allowed their child to participate. However, the small sample size and scope of this pilot limit conclusions, and preclude formal tests of parenting as the primary mediator of treatment effects. These limitations also hinder full use of multiple respondent data to disentangle influences of parent psychopathology on children. Nonetheless, promising findings clearly support a larger, sufficiently powered, randomized trial to more rigorously evaluate PSBCT and its effects.
Acknowledgments
This project was supported by the National Institute on Alcohol Abuse and Alcoholism (R21AA013690). We acknowledge Dr. Frank Fincham and the project team for their invaluable help in conducting this study. A full version of this short report is available upon request from the first author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. Manual for the child behavior checklist. Burlington: Univ of VT; 1991. [Google Scholar]
- Cohen J. Statistical power analysis for the social sciences. 2. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Fals-Stewart W, Fincham F, Kelley ML. Substance-abusing parents’ attitudes toward allowing their custodial children to participate in treatment: A comparison of mothers versus fathers. Journal of Family Psychology. 2004;18:666–671. doi: 10.1037/0893-3200.18.4.666. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O’Farrell TJ, Birchler GR, Cordova J, Kelley ML. Behavioral Couples Therapy for alcoholism and drug abuse: Where we’ve been, Where we are, and Where we’re going. Journal of Cognitive Psychotherapy. 2005;30:1479–1495. [Google Scholar]
- First M, Spitzer L, Gibbon M, Williams J. Structural clinical interview for Axis I DSM-IV disorders (SCID) Washington, DC: American Psychiatric Association; 1995. [Google Scholar]
- Goldstein H. Multilevel statistical models. Arnold; London: 2003. [Google Scholar]
- Hussong AM, Wirth RJ, Edwards MC, Curran PJ, Chassin LA, Zucker RA. Externalizing symptoms among children of alcoholic parents: Entry points for an antisocial pathway to alcoholism. Journal of Abnormal Psychology. 2007;116:529–542. doi: 10.1037/0021-843X.116.3.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley ML, Fals-Stewart W. Couples- versus individual-based therapy for alcholism and drug abuse: Effects on children’s psychosocial functioning. Journal of Consulting and Clinical Psychology. 2002;70:417–427. doi: 10.1037//0022-006x.70.2.417. [DOI] [PubMed] [Google Scholar]
- Kelley ML, Fals-Stewart W. Treating paternal alcoholism using Learning Sobriety Together: Effects on adolescents versus preadolescents. Journal of Family Psychology. 2007;21:435–444. doi: 10.1037/0893-3200.21.3.435. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory. New York: Multi-Health Systems; 1992. [Google Scholar]
- McMahon RJ, Forehand R. Helping the noncompliant child: A clinician’s guide to effective parent training. 2. New York: Guilford; 2003. [Google Scholar]
- Monti PM, Abrams DB, Kadden RM, Cooney NL. Treating alcohol dependence: A coping skills training guide. New York: Guilford Press; 1989. [Google Scholar]
- O’Farrell TJ, Fals-Stewart W. Behavioral Couples Therapy for Alcoholism and Drug Abuse. New York: Guilford Press; 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Murphy M, Alter J, Fals-Stewart W. Brief family treatment intervention to promote aftercare among male substance abusing patients in inpatient detoxification: A quasi-experimental pilot study. Addictive Behaviors. 2007;32:1681–1691. doi: 10.1016/j.addbeh.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds CR, Paget KD. National normative and reliability data for the Revised Children’s Manifest Anxiety Scale. School Psychology Review. 1983;12:324–333. [Google Scholar]
- Serketich W, Dumas J. The effectiveness of behavioral training to modify antisocial behavior in children: A meta-analysis. Behavior Therapy. 1996;27:171–186. [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback user’s guide: A calendar method for assessing alcohol and drug use. Toronto, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- Wells KM. Substance abuse and child maltreatment. In: Brittain CR, editor. Understanding the medical diagnosis of child maltreatment. New York, NY: Oxford; 2006. pp. 179–189. [Google Scholar]
- Xu R. Measuring explained variation in linear mixed effects models. Statistics in Medicine. 2003;22:527–541. doi: 10.1002/sim.1572. [DOI] [PubMed] [Google Scholar]