Abstract
The sporadic nature of Alzheimer's disease (AD) argues for an environmental link that may drive AD pathogenesis; however, the triggering factors and the period of their action are unknown. Recent studies in rodents have shown that exposure to lead (Pb) during brain development predetermined the expression and regulation of the amyloid precursor protein (APP) and its amyloidogenic β-amyloid (Aβ) product in old age. Here, we report that the expression of AD-related genes [APP, BACE1 (β-site APP cleaving enzyme 1)] as well as their transcriptional regulator (Sp1) were elevated in aged (23-year-old) monkeys exposed to Pb as infants. Furthermore, developmental exposure to Pb altered the levels, characteristics, and intracellular distribution of Aβ staining and amyloid plaques in the frontal association cortex. These latent effects were accompanied by a decrease in DNA methyltransferase activity and higher levels of oxidative damage to DNA, indicating that epigenetic imprinting in early life influenced the expression of AD-related genes and promoted DNA damage and pathogenesis. These data suggest that AD pathogenesis is influenced by early life exposures and argue for both an environmental trigger and a developmental origin of AD.
Keywords: amyloidogenesis, development, environmental exposure, Pb, epigenetic regulation, transcription factor
Introduction
Alzheimer's disease (AD) is a progressive and irreversible neurodegenerative disorder that results in dementia and death. AD pathology is characterized by senile plaques and neurofibrillary tangles (NFTs), combined with massive neuronal loss, mainly in the hippocampus and association regions of the neocortex (Ball and Lo, 1977). The major constituents of senile plaques are 39–43 aa peptides [β-amyloid (Aβ)], snipped from a larger protein called Aβ precursor protein (APP) (Glenner and Wong, 1984; Masters et al., 1985; Goldgaber et al., 1987). Recent studies indicate that APP is processed by a group of secretases (Dominguez et al., 2004). The α-secretase generates a soluble product, whereas β-secretase and γ-secretase generate Aβ from APP (Walsh et al., 2007).
The sporadic nature of most AD cases strongly argues for an environmental link that may drive AD pathogenesis; however, it is not clear when this may occur. Reconstructions of neonatal and medical histories of birth cohorts have led to the origin of the “Barker hypothesis” (Barker et al., 1989; Osmond and Barker, 2000), which links early life experiences and adult diseases. These observations resulted in a new concept regarding certain adult diseases that emphasizes the role of environmental factors operating during the preconceptual, fetal, and infantile phases of life (Gluckman and Hanson, 2004).
The pathological manifestations in AD patients are presumed to result from defects of old age; however, it is unlikely that the disease process begins late in life. Therefore, amyloidogenesis associated with AD can also be viewed as a pathological outcome that is evident during aging; however, the preceding initiating event may have occurred during early stages of brain development (Zawia and Basha, 2005). Specifically, this event would have been a LEARn (latent early-life associated regulation) alteration (Lahiri et al., 2007) affecting the expression of genes associated with a later-manifest condition.
Previous work from our laboratories showed that developmental exposure of rats to the metal Pb from birth to postnatal day 20 showed a delayed overexpression of APP and elevation of its amyloidogenic Aβ product in old age (Basha et al., 2005). We also observed elevations in the oxidative DNA marker 8-hydroxy-2′-deoxyguanosine (8-oxo-dG) in older rats that had been developmentally exposed to Pb (Bolin et al., 2006). These findings suggested that environmental influences occurring during brain development predetermined the expression, regulation, and processing of APP later in life, potentially influencing the course of amyloidogenesis and oxidative damage.
To link these molecular and oxidative perturbations observed in rats to pathological consequences associated with AD, we examined the brains of aged cynomolgus monkeys that were similarly exposed to Pb as infants. Primates are among a few animal models that express amyloid plaques and other pathological features that are absent in wild-type/nontransgenic rodents. This study was undertaken to determine whether nonhuman primates that exhibit similar AD-like pathology in old age (Price and Sisodia, 1994) would be influenced by developmental perturbations, and to explore the potential mechanisms that could mediate such latent effects.
Materials and Methods
Animal exposure.
In 1980–1981, a cohort of female monkeys (Macaca fascicularis) was randomly assigned at birth to one of two exposure groups: one received 1.5 mg · kg−1 · d−1 of lead acetate (Pb) from birth until 400 d of age via infant formula and vehicle after weaning, whereas the other group served as a control group and received formula or vehicle only. No overt signs of toxicity or health-related problems were evident in the animals as a result of Pb exposure (Rice, 1990, 1992). They were then transferred to National Institutes of Health (NIH) facility until termination in 2003 at ∼23 years of age and all animal procedures were conducted under the supervision of a licensed veterinarian according to a National Institute on Environmental Health Sciences–NIH-approved animal protocol. As previously reported, the blood lead levels of these animals at 400 d of age averaged 19–26 μg/dl in Pb-exposed monkeys compared with 3–6 μg/dl in the controls (Rice, 1990, 1992). The monkeys were terminated in 2003 (23 years later), and multiple organ tissues, including the brain, were collected, cut in 1 cm sections, and immediately processed in 10% formalin for histopathology or frozen on dry ice and stored at −80°C. At this time, the animals were in good health, and there were no indications of adverse health effects as a result of early Pb exposure.
Total RNA isolation, synthesis of cDNA, and real-time PCR.
RNA from various control and exposed monkey cortical tissues was isolated according to the TRIzol method (Invitrogen, San Diego, CA). The RNA was reverse transcribed to obtain cDNAs, catalyzed by SuperScript III Reverse Transcriptase (RT). The RNA/primer mixture containing 500 ng of total RNA, 1 μl of 10 mm dNTP mix, and 1 μl of oligo-dT was incubated at 65°C for 5 min. A reaction mixture containing 2 μl of 10× RT buffer (200 mm Tris-HCl, pH 8.4, 500 mm KCl), 4 μl of 25 mm MgCl2, 2 μl of 0.1 m DTT, and 1 μl of RNaseOUT recombinant RNase inhibitor (40 U/μl) was added. One microliter of SuperScript III RT (200 U/μl) was then added and incubated at 50°C for 50 min. The reaction was terminated at 85°C for 5 min. One microliter of RNase H was added, and the reaction was incubated for 20 min at 37°C. The resulting cDNA was stored at −20°C and used in the real-time PCR step. The primer pairs used for APP, Sp1, β-site APP cleaving enzyme 1 (BACE1), and GAPDH were as follows: Sp1, sense, 5′-CAA GCC CAA ACA ATC ACC TT-3′, and antisense, 5′-CAA TGG GTG TGA GAG TGG TG-3′; BACE1, sense, 5′-TTT GTG GAG ATG GTG GAC AA-3′, and antisense, 5′-CAG CAC CCA CTG CAA AGT TA-3′; APP, sense, 5′-GCT GGC TGA ACC CCA GAT-3′, and antisense, 5′-CCC ACT TCC CAT TCT GGA CAT-3′; GAPDH, sense, 5′-TGA AGC AGG CGT CGG AGG G-3′, and antisense, 5′-CGA AGG TGG AAG AGT GGG TG-3′. Each real-time PCR mix contained 1 μl of cDNA, 1 μl of primer mix (final concentration, 200 nm), 10.5 μl of nuclease-free water, and 12.5 μl of SYBR GREEN PCR Master Mix (Applied Biosystems, Foster City, CA). Each sample had triplicates. Real-time PCR was conducted for all of the above genes with respective primer pairs in a 7500 Real-Time PCR System following standard protocol, that was, 50°C for 2 min followed by 95°C for 10 min, and then 40 cycles of 95°C for 15 s and 60°C for 1 min. Real-time PCR products were checked with agarose gel to confirm that no nonspecific products formed. Results were analyzed with 7500 system software with relative quantification method using GAPDH as endogenous control. Other housekeeping genes such as β-actin were also used.
Aβ1–40 and Aβ1–42 assay.
The levels of Aβ were measured using human Aβ (1–40 and 1–42) assay kits (Immuno-Biological Laboratories, Gunma, Japan). These kits were designed as solid-phase sandwich ELISA with two kinds of highly specific antibodies. The assay conditions were followed according to the method described by Morishima-Kawashima et al. (2000), with slight modifications. Brain tissue was homogenized in Tris-saline (TS) [50 mm Tris-HCl buffer, pH 7.4, 150 mm NaCl, 1 μg/ml TLCK (N-α-p-tosyl-l-lysine chloromethyl ketone), 1 μg/ml antipain, 0.5 mm DIFP (diisopropyl fluorophosphates), 0.5 mm PMSF, 0.1% protease inhibitor mixture] and centrifuged at 100,000 × g for 20 min at 4°C. The pellet was resuspended in 4 vol of TS and centrifuged at 70,000 × g for 20 min at 4°C. The resultant pellet was dissolved in 500 μl of 6 m guanidine-HCl (in 50 mm Tris buffer, pH 7.6), incubated at room temperature for 30 min, and centrifuged at 70,000 × g for 20 min at 4°C. The resultant supernatant was collected and diluted by enzyme immunoassay (EIA) buffer (supplied with the kit) to 12× to reduce sample guanidine-HCl concentration, and aliquots (200 μg of protein in 100 μl of EIA buffer) and assay standards were added to a 96-well plate [precoated with anti-human Aβ (35–40) (1A10) Mouse IgG MoAb] and incubated overnight at 4°C. The wells were washed seven times with EIA buffer. Then, 100 μl of labeled antibody was added to each well containing sample or standard and incubated at 4°C for 1 h. The wells were washed nine times with EIA buffer followed by the addition of 100 μl of TMB buffer, and incubated in the dark for 30 min at room temperature. The reaction was stopped by adding 100 μl of 1N H2SO4, and the colorimetric absorption was performed at 450 nm. The levels of Aβ in the test samples were calculated relative to the standard curve generated on each plate.
Immunohistochemistry.
The cellular distribution of APP, SP1, and Aβ was examined in paraffin-embedded brain tissue of control (Con) and developmentally, Pb-exposed (Pb-E), 23-year-old cynomolgus monkeys. The sections were subjected to brief washes in 1× PBS and 3% hydrogen peroxide. After rinsing, the sections were incubated in PBS containing 2% BSA and 1% Triton X-100 blocking solution for 30 min, and then incubated in the presence of primary antibody for APP (22C11; 1:200; Sigma, St. Louis, MO), Aβ (6E10; 1:50; Sigma), or SP1 (SC-59; 1:100; Santa Cruz Biotechnology, Santa Cruz, CA) overnight at 4°C. Sections were washed with PBS and incubated along with the species-specific biotinylated secondary antibody mouse/rabbit (1:200; Vector Laboratories, Burlingame, CA) for 30 min. The sections were incubated with streptavidin (Vector Laboratories) for 30 min, rinsed briefly with PBS, and immunoreactivity was detected with the substrate DAB (3–3′-diaminobenzidine-tetrahydrochloride) (Vector Laboratories). Coverslips were mounted with Permanent Mounting Medium (Vector Laboratories).
In all cases, negative controls were run on slides from each animal by omitting the primary antibody incubation. No signal was evident after incubation of tissues in secondary antibody alone.
Nuclear protein extraction.
Nuclear proteins were extracted from the frontal association cortical tissue of control and Pb-exposed animals according to the method described by Dignam et al. (1983), with slight modifications. Tissue samples were homogenized with 1 ml of PBS, pH 7.4, and centrifuged at 2500 × g for 10 min at room temperature. The pellets obtained were suspended in 5 vol of buffer A (10 mm HEPES at pH 7.9, 1.5 mm MgCl2, 0.5 mm DTT, 0.5 mm EDTA, and 0.2 mm PMSF) and centrifuged at 6000 × g for 2 min at 4°C. The pellets were resuspended in 3 vol of buffer A and centrifuged at 6000 × g for 2 min at 4°C. The resulting pellets were then resuspended in 5 vol of buffer C (20 mm HEPES at pH 7.9, 1.5 mm MgCl2, 0.5 mm DTT, 0.5 mm EDTA, 420 mm NaCl, 20% glycerol, 0.2 mm PMSF, 0.002 mg/ml aprotinin, and 0.0005 mg/ml leupeptin) and homogenized. The final suspensions were centrifuged at 12,000 × g for 10 min. The supernatants were transferred to 1.5 ml tubes, snap frozen in an ethanol dry-ice bath, and stored at −80°C (Basha et al., 2005).
Primary mice cortical neuronal cell culture.
Because the animals we studied were 23 years of age and we did not have early time points to measure the progression of the molecular or epigenetic changes, we used a cell culture model to address some of the mechanistic questions. We used the C57BL/6 mouse as a source of primary fetal cortical neurons based on the wide use of this genetic background strain for various transgenic mice AD models. The C57BL/6 mice (Charles River Laboratories, Wilmington, MA) fetuses were used to generate primary cortical neuronal cultures. Animal usage was approved (Approval AN00-01-007) and monitored by the Institutional Animal Care and Use Committee of the University of Rhode Island. Brains were excised, and cortices were dissected from day 15 mouse pups from the same dam. Meninges were removed and cortical tissue was incubated for 15 min at 37°C in 5 ml of HBSS containing papain (2 mg/ml). Tissue was centrifuged at 125 × g for 5 min, and the resulting pellet was resuspended in HBSS and cells were dissociated with trituration through a fire-polished Pasteur pipette and repeated three times. After centrifugation, cells were plated at a constant density of 6.5 × 104/well, in 24-well poly-d-lysine-precoated plates. The plating medium contained 2% B27, 0.5 mm [scap]l-glutamine, and 25 μm glutamic acid in Neurobasal medium (Invitrogen) and maintained at 37°C in a humidified atmosphere of 5% CO2. After 4 d in culture, one-half of the medium was replaced with fresh medium devoid of glutamic acid and the cultures were maintained. To determine methyltransferase activity, cells in the 24-well plates were treated with 0.1 μm Pb at the time of medium change for 24 h. Pb was removed and cells were aged for 7 d before nuclear extract was harvested and subjected to methyltransferase activity assay.
8-oxo-dG determination.
8-oxo-dG levels were determined by HPLC as described previously (Bolin et al., 2006). Briefly, sample tissue was homogenized in nuclease-free homogenization buffer followed by digestion with proteinase K to remove proteins. The DNA was precipitated by three consecutive organic extractions, precipitation by 2 vol of ethanol (with respect to the aqueous volume), and incubated overnight at −20°C. The purified DNA was prepared for HPLC analysis by nuclease digestion into deoxynucleoside components. The amount of 8-oxo-dG and 2′-deoxyguanosine (2′-dG) was calculated by comparing the peak areas of 8-oxo-dG and 2′-dG obtained from the enzymatic hydrolysate of the DNA sample to a calibration curve for both compounds. Levels of 8-oxo-dG in the samples were expressed relative to the content of 2′-dG [e.g., the molar ratio of 8-oxo-dG/2′-dG (femtomoles of 8-oxo-dG per nanomole of 2′-dG)]. The HPLC method used for analysis of the samples was as follows: the mobile phase consisted of 100 mm sodium acetate, pH 5.2, with 5% methanol. Flow rate was kept at 1 ml/min using a Model 582 Solvent Delivery Module (ESA, Chelmsford, MA). DNA was analyzed using a reverse-phase YMC basic HPLC column (4.6 × 150 mm) with a 3 μm particle size (YMC, Wilmington, NC). 8-oxo-dG and 2′-dG were detected by a Model 5600A CoulArray Detector (ESA) with three model 6210 four-channel electrochemical cells; potentials were set at 175, 200, and 250 V for 8-oxo-dG and at 785, 850, and 890 V for 2′-dG. Data were recorded, stored, and analyzed with CoulArray for Windows32 Software (ESA). Data were expressed as femtomoles of 8-oxo-dG per nanomole of 2′-dG.
DNA methyltransferase assay.
DNA methyltransferase activity was determined in nuclear extracts derived from the control and Pb-exposed frontal associated cortical tissue. Nuclear extracts were derived as described above, and the DNA methyltransferase activity was assayed following the method described by Takiguchi et al. (2003). Nuclear extracts containing 60 μg of protein (source of methyltransferase) were incubated with 50 ng of deoxyinosine-deoxycytidine (poly[dI.dC].poly[dI.dC]) double-stranded DNA template (Sigma) as a substrate, 1 μm 3H-labeled S-adenosyl methionine (SAM) (79 Ci/mmol), 100 mm Tris-HCl, pH 8.2, in a final volume of 30 μl. The reaction was initiated by the addition of SAM for 1 h at 37°C and terminated by chilling on ice. A 15 μl aliquot was spotted on DE81 filter paper and washed with sodium phosphate buffer, pH 7.0, twice, once with 70% ethanol, and once with 100% ethanol. The filter was dried and counted in a scintillation counter.
Statistical treatment.
Data were analyzed using two-tailed Student's t test, and the values marked with an asterisk were significantly different from the control group (p < 0.05).
Results
Pb levels
The exposure of these primate animals to low levels of inorganic Pb from birth to 400 d resulted in blood Pb levels of 19–26 μg/dl when being dosed with Pb after weaning from infant formula. This level is slightly above the 10 μg/dl considered safe for humans by the Centers for Disease Control and Prevention (1991) and is similar to the exposure scenario we previously used in lifetime studies with rats (Basha et al., 2005). Sampling during young adulthood demonstrated clearance of Pb from the blood and levels were similar for both control and Pb-exposed monkeys (Rice, 1992). Thus, any significant exposure was limited to the developing and adolescent period. In the aged animals, Pb levels in brain tissue were analyzed using Elemental Analyzer ICP-MS, and we found that Pb levels for both exposed and control animals remained below the detection levels (<0.1 ng/g wet weight of tissue).
Latent expression of APP, Aβ, BACE1, and Sp1
The amino acid sequence of APP of cynomolgus monkeys is homologous (96%) to that of humans, making it a good model for studies of the pathological effects of Aβ in the primate brain (Podlisny et al., 1991). The enzyme BACE1 plays a major role in the cleavage of APP (Singer et al., 2005), and transcription factor Sp1 (Lahiri and Robakis, 1991; Christensen et al., 2004) is a known regulator of both genes. Therefore, we compared APP, BACE1, and Sp1 mRNA levels in the control and developmentally Pb-exposed aged primates. The mRNA levels of all three genes (Fig. 1) were elevated in primates exposed to Pb as infants; however, the elevation in BACE1 was not statistically significant (p = 0.063). Quantification of results indicated that APP mRNA levels increased 50% (p = 0.045); Aβ1–40 levels increased 50% (p = 0.011); and Aβ1–42 levels increased 100% (p = 0.029), in a manner similar to that previously seen in rodents (Fig. 2 A,B). Whereas rodents have non-plaque-forming Aβ with 3 aa different from that of primates, APP of cynomolgus monkey shares 96% sequence homology with human, and both species have same plaque-forming Aβ peptides, which is more clinically relevant. Furthermore, the ratio of Aβ1–42 to Aβ1–40 increased as a result of developmental exposure to Pb (Fig. 2 B). Exposure of cultured mouse primary neurons to these peptides confirmed that both of these peptides were toxic to the cells even in the soluble form and that Aβ1–42 was more cytotoxic than Aβ1–40 (supplemental Fig. 1, available at www.jneurosci.org as supplemental material).
Figure 1.

Changes in mRNA expression of APP, BACE1, and Sp1 in the frontal association cortex of aged monkeys after developmental exposure to Pb. The frontal association cortical tissue of 23-year-old control (Con) and Pb-exposed (Pb-E) monkeys were analyzed for mRNA expression of APP, BACE1, and Sp1. The mRNA expression of APP, BACE1, and Sp1 were validated by real-time PCR. Data shown represent the mean ± SEM (4 animals in each group). Values marked with an asterisk are significantly different from their corresponding controls (p < 0.05) as determined by Student's t test.
Figure 2.
Elevation of Aβ levels in the frontal association cortex of 23-year-old cynomolgus monkeys after developmental exposure to Pb. Brain tissue of control (Con) and Pb-exposed (Pb-E) 23-year-old cynomolgus monkeys was used for the analysis of Aβ levels (A, B). The levels of Aβ were measured in the frontal association cortical tissue using ELISA as described in Materials and Methods. Data shown represent the mean ± SEM for four animals in each group. Values marked with an asterisk are significantly different from their corresponding controls (p < 0.05) as determined by Student's t test.
Alteration of AD pathology
Immunohistochemical analysis of the frontal association cortex was undertaken to determine whether the observed molecular changes in APP expression and Aβ levels were accompanied by changes in the pathological features of the brains of these animals. The brains of the aged monkeys developmentally exposed to Pb revealed an increase in the intracellular staining of total Aβ and dense-core plaques compared with age-matched controls (Fig. 3). Higher magnification of intracellular Aβ staining revealed the accumulation of immunoreactive Aβ aggregates inside neuronal cells, the budding of some of these Aβ species from the membrane as well as their deposition in the extracellular space (Fig. 3). We also observed diffuse and cored plaques and NFTs morphologically similar to those observed in human brain. The Aβ plaques were found to be rich in Aβ1–42, the more amyloidogenic species of Aβ, and were detectable using Congo red staining.
Figure 3.
Photomicrographs showing AD-like pathology in the frontal association cortex of 23-year-old cynomolgus monkeys after developmental exposure to Pb. Brain tissue of control (Con) and Pb-exposed (Pb-E) 23-year-old cynomolgus monkeys was used for the analysis of immunohistochemical analysis of AD-like pathology. Sections were prepared and stained with the Aβ-specific antibody, which recognizes both Aβ1–40 and Aβ1–42 as discussed in Materials and Methods. The arrows point to Aβ-containing plaques as well as granular and intracellular staining. The staining characteristics are similar to those reported in the literature.
DNA methylation
The latent expression of genes observed in these animals may be mediated through epigenetic pathways that are regulated via DNA methylation. To determine whether developmental exposure to Pb interfered with DNA-methylation patterns, we examined the activity of DNA methyltransferase 1 (DNMT1) in the 23-year-old primate brain tissues. The activity of this methylating enzyme is selective for cytosine in a CpG dinucleotide, which is base-paired to a methylated CpG sequence on the complementary strand of DNA and is directly proportional to the abundance of methyl groups on CpG dinucleotides in the DNA (Poirier and Vlasova, 2002; Takiguchi et al., 2003). We found the activity of DNMT1 to be reduced by ∼20% in brain tissue derived from developmentally Pb-exposed primates (Fig. 4 B). Exposure of mouse primary cells from the cortex to low levels of Pb (0.1 μm) for a transient 24 h period followed by aging of the cells for 1 week produced a similar trend in DNMT1 activity (Fig. 4 A).
Figure 4.
DNA methyltransferase activity in cortical neuronal cells of mice and in monkey brains. A, B, Control and Pb-exposed mouse cortical neuronal cells (A) and frontal association cortical tissue of 23-year-old control (Con) and Pb-exposed (Pb-E) monkeys (B) were used to estimate the DNA methyltransferase activity as described in Materials and Methods. Data shown represent the mean ± SEM for four independent determinations (4 animals in each group for monkey data). Values marked with an asterisk are significantly different from their corresponding controls (p < 0.05) as determined by Student's t test.
DNA oxidation
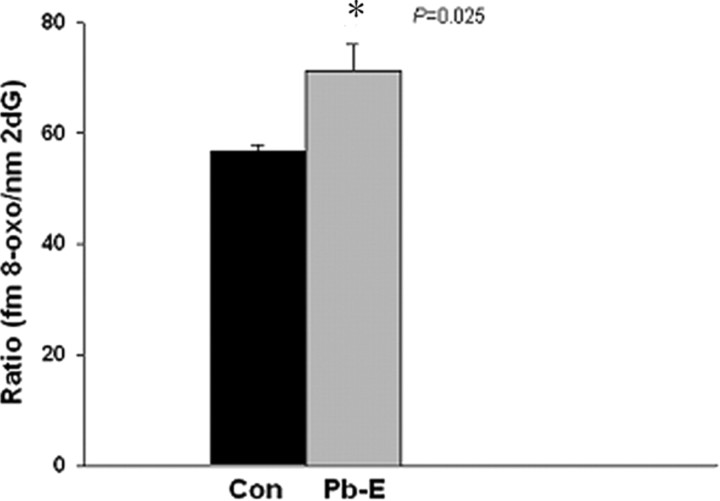
In addition to the alteration in APP and Aβ deposition, age-related accumulation of oxidative damage is suspected to play a role in the pathogenesis of AD. Aβ levels are well known to induce functional disturbance in vivo through their pro-oxidant and neurotoxic properties (Castellani et al., 2006). Along with the increase seen in Aβ levels in the cortex of developmentally Pb-exposed animals, higher levels of the biomarker of oxidative DNA damage, 8-oxo-dG were noted (Fig. 5).
Figure 5.
Oxidative DNA damage in control and infantile-exposed aged monkey brains. Frontal association cortical tissues were obtained from 23-year-old control (Con) and Pb-exposed (Pb-E) monkeys and used to measure the marker of oxidative DNA damage as described in Materials and Methods. Data shown represent the mean ± SEM for four animals in each group. Values marked with an asterisk are significantly different from their corresponding controls (p < 0.05) as determined by Student's t test.
Discussion
The data presented in this paper show that monkeys exposed to Pb at birth to 400 d upregulate the expression of APP, BACE1, and Sp1 in old age. The upregulation of both APP and BACE1 gene expression is mediated by Sp1, and the essentiality of Sp1 as a mediator of these delayed transcriptional upregulations has been previously shown by us (Basha et al., 2005). Moreover, both APP and BACE1 gene promoters are rich in CpG dinucleotides and GC box elements (Pollwein et al., 1992), making them subjected to epigenetic reprogramming and transcriptional regulation via DNA methylation pathways (Lahiri et al., 2007). This is further reinforced by preliminary microarray screens, which showed that >95% of the differentially expressed genes screened in control versus Pb-exposed monkeys were also CpG-rich (supplemental Table 1, available at www.jneurosci.org as supplemental material). This transcriptional reprogramming at the gene level is also translated into biological consequences. Levels of amyloidogenic products of APP were also increased in the aged animals that were exposed to Pb as infants (Fig. 2 A). This is consistent with previous findings in rodents (Basha et al., 2005) and argues for a transcriptional process that promotes neurodegeneration in old age (Lahiri et al., 2007).
Notably, these molecular and biochemical changes observed in 23-year-old animals are accompanied by altered features of AD-like pathology in the exposed monkeys. Our intracellular staining closely resembles what is seen in humans and other animal models (Mochizuki et al., 1996; Schmitz et al., 2004). It reveals granular, oval, and crescent-shaped Aβ localization in pyramidal cells and globular-shaped neurons in layers II–IV of the cortex. The occurrence of these molecular, biochemical, and pathological changes in primates that develop plaques and tangles in old age, in response to developmental exposure to Pb, suggests that developmental exposure can influence latent pathogenesis, hence bearing a direct relevance to humans. The possibility that developmental exposure to Pb could result in the formation of AD pathology in humans is further supported by findings in a patient who survived from severe Pb toxicity at 2 years of age, but died of severe mental deterioration at the age of 42 (Niklowitz and Mandybur, 1975). The brain of this patient revealed many senile plaques and NFTs (Niklowitz and Mandybur, 1975). Although this is a single case, the plausibility that early exposure to Pb could be a risk factor for AD warrants additional study.
One way to achieve permanent changes or long-term alteration in gene expression is to alter the structural makeup of the DNA bases that determine the sequence-specific DNA-binding of a transcription factor. Our findings with changed DNA methyltransferase activity argue that exposure to Pb early in life interferes with gene imprinting and could thus leave a permanent molecular damage on the DNA. That is to say, expression has been reprogrammed through imposition of a pathogenic somatic epitype (Lahiri and Maloney, 2007). Consistent with such a potential mechanism is the decreased activity of the DNA methylating enzyme in the aged animals exposed to Pb as infants, as well as the delayed decrease in the activity of this enzyme in cells that had previous exposure to Pb (Fig. 4).
This is further supported by studies that show that regions of the human APP promoter upstream of −500 bp displayed tissue and brain region-specific profiles of methylation, which approximately reflect APP expression patterns (Rogaev et al., 1994) and age-related reduction in methylcytosine (−224 to −101) that occur on the human APP promoter (Tohgi et al., 1999). To link the association of an epigenetic phenomenon in current model, we hypothesize that genes that are regulated by methylation can be reprogrammed in adulthood as a result of infantile exposure to inorganic Pb. This hypothesis was supported by our microarray screening of 588 neurobiology-related genes. We found that most of the genes (20 of 22) that were altered because of infantile exposure to Pb were rich (>60%) in CpG dinucleotides (supplemental Table 1, available at www.jneurosci.org as supplemental material). However, our own work herein and previously (Basha et al., 2005) has shown that, although SP1 and APP are upregulated in a latent manner after early exposure to Pb in both cynomolgus monkeys and rats, other genes regulated by SP1, such as BACE1 (Christensen et al., 2004), do not respond in rodents (Bolin et al., 2006) and show a modest trend in primates.
In addition, SP1 regulates a wide variety of other genes that have not been shown to respond in this latent manner to early Pb exposure. This does not exclude SP1 from an active role in latent Pb-induced pathogenesis. Although the APP and BACE1 promoters from humans and primates contain sites for SP1 binding (Song and Lahiri, 1998; Sambamurti et al., 2004), the specific position of these sites differ with regard to their respective transcription start sites. For example, active SP1 sites in the APP gene appear in its 5′-untranslated region (UTR) (Villa et al., 2004), whereas the active SP1 site in the BACE1 promoter is ∼1 kb upstream of the transcription start (Christensen et al., 2004). Alternatively, general density of CpG dinucleotides in combination with presence of transcription factor sites (such as SP1) may explain the differential effects between APP and BACE1. Comparison of the cumulative potential methyl CpG dinucleotides 2 kb upstream of the transcription start sites indicated that the proximal promoter regions surveyed by Bolin et al. (2006) suggested a difference in methylation site density centered around −100.
Ample evidence has accumulated that oxidative damage to macromolecules such as DNA, protein, and lipids (Cecchi et al., 2002; Esposito et al., 2006), as well as a downregulation in antioxidant enzymes are associated with AD (Smith and Perry, 1995). We previously found elevations in the oxidative DNA marker 8-oxo-dG in older rats that had been developmentally exposed to Pb (Bolin et al., 2006). Here, we also find a similar accumulation of 8-oxo-dG (Fig. 5). This latent accumulation of oxidized DNA could possibly come from two sources. The latent increase in Aβ could promote the formation of reactive oxygen species, thus damaging the DNA; and/or epigenetic modulation in the methylation pattern of cytosines could interfere with the repair of oxidized guanines or render them more susceptible to oxidative damage (Evans and Cooke, 2004).
Few studies address both DNA methylation and DNA oxidative damage as an epigenetic phenomenon. Researchers using synthetic DNA oligonucleotides with both methylation and oxidative damage in a single CpG site or oxidized dG at a complementary strand have found oxidation of guanine in a CpG dinucleotide reduced the methyl group binding domain (MBD) binding to that site (Valinluck et al., 2004). Even the oxidation on the guanine in the opposite strand diminished the MBD binding but not so much as the same strand G-oxidation. When 5-methylcytosine was oxidized to 5-hydroxymethylcytosine, its affinity to MBD is greatly reduced to the same level as unmethylated cytosine. We thus hypothesize that epigenetic mechanisms such as DNA methylation can influence oxidative damage and make organisms more susceptible to the pathogenesis of AD and that this process can be modulated by environmental exposure.
We, therefore, propose a model (Fig. 6) of interaction between methylation and oxidative damage in genes reprogramming. Using the APP gene proximal promoter/5′-UTR sequence as an example, in undamaged genes, methyl CpG binding protein 2 (MECP2) would compete against transcription factors such as SP1 for regulation. The resulting competition would downregulate a given gene. If target DNA is altered via oxidation to 8-oxo-dG or 5-hydroxymethylcytosine, MECP2 binding may be partially or completely blocked, but insufficiently to permit sufficient competing SP1 interaction with the sequence to change expression (Fig. 6 B). Normal changes of development, maturity, and aging result in triggering of latent SP1 regulatory alterations, which significantly increase levels of the transcription factor (Fig. 6 C). The greater levels of SP1, when combined with partial blockage of MECP2 binding, permit sufficient SP1 interaction with the sequence to result in greater target gene expression. It is likely that other transcription factors may function as competitive targets for MECP2 in addition to SP1.
Figure 6.
Model of effects of oxidative damage on SP1-mediated expression of APP via interference with MECP2 binding of methylated CpG dinucleotides. The APP promoter and 5′-UTR from −1000 bp to the “ATG” start codon at +148 are shown. CpG dinucleotides are indicated on the sequence, as is the +1 transcription start site. A, Undamaged DNA, showing the binding of one or more MECP2 to methylated CpG, competing against SP1. APP expression is at normal levels. B, Conversion of G residues to 8-oxo-dG or mC to 5-hydroxymethylcytosine blocks binding of some MECP2 to methylated CpG, potentially permitting additional binding of SP1 but with insufficient levels to significantly alter target gene expression levels. C, Normal changes of development, maturity, and aging result in triggering of latent SP1 regulatory alterations, which significantly increase levels of the transcription factor, permitting SP1 to outcompete remaining MECP2 binding, increasing expression of target genes.
Adult diseases such as schizophrenia have also been linked to infection, fetal malnutrition, or hypoxia in early life (Dalman et al., 1999; Van Erp et al., 2002; Boksa and El-Khodor, 2003). A study by Bilbo et al. (2005) showed that perinatal exposure to an infectious agent affected how the nervous system responded to an immune challenge and memory consolidation later in adulthood. The authors also found that neonatal pathogen exposure decreased the number of adult hippocampal astrocytes, increased their reactivity, and decreased brain IL-1β levels after adult lipopolysaccharide exposure. Work in autism spectrum disorders has demonstrated at least some contribution of differential methylation (Jiang et al., 2004). In this context, recent results showing increased plasma-soluble APPα levels in patients of “autism with aggression” may provide an epigenetic role for APP in autism spectrum disorders, as per environmentally mediated LEARn regulation (Sokol et al., 2006). Hypomethylation of the DRD2 and HTR2A genes have been implicated in both schizophrenia and bipolar disorder (Abdolmaleky et al., 2004). However, hypermethylation of the RELN gene has been shown to associate with schizophrenia (Abdolmaleky et al., 2005), indicating that latent pathogenic effects of epigenetic perturbations may work on more than one mechanism. Although our work specifically addressed latent effects of Pb, other metals may have a similar effect (Poirier and Vlasova, 2002; Takiguchi et al., 2003).
In conclusion, this study presents novel findings in primates that implicate an environmental agent (Pb) in the pathogenesis of AD and demonstrate that development is an important period of vulnerability, which could increase future susceptibility to neurodegeneration and AD pathology.
Footnotes
This work was supported by National Institutes of Health (NIH) Grants ES013022 and AG027246 (N.H.Z.) and University of Rhode Island Core Facility Grant P20RR016457 funded by the National Center for Research Resources, a component of NIH. Work at F.C.-P.'s laboratory was supported by the Division of Intramural Research of National Institute on Environmental Health Sciences–NIH, National Institute on Aging Grant 1R15AG023604-01; and work at D.K.L.'s laboratory was supported by a Zenith award from the Alzheimer's Association, and NIH Grants R0AG18379 and R0AG18884.
References
- Abdolmaleky HM, Smith CL, Faraone SV, Shafa R, Stone W, Glatt SJ, Tsuang MT. Methylomics in psychiatry: modulation of gene-environment interactions may be through DNA methylation. Am J Med Genet B Neuropsychiatr Genet. 2004;127:51–59. doi: 10.1002/ajmg.b.20142. [DOI] [PubMed] [Google Scholar]
- Abdolmaleky HM, Cheng KH, Russo A, Smith CL, Faraone SV, Wilcox M, Shafa R, Glatt SJ, Nguyen G, Ponte JF, Thiagalingam S, Tsuang MT. Hypermethylation of the reelin (RELN) promoter in the brain of schizophrenic patients: a preliminary report. Am J Med Genet B Neuropsychiatr Genet. 2005;134:60–66. doi: 10.1002/ajmg.b.30140. [DOI] [PubMed] [Google Scholar]
- Ball MJ, Lo P. Granulovacuolar degeneration in the ageing brain and in dementia. J Neuropathol Exp Neurol. 1977;36:474–487. doi: 10.1097/00005072-197705000-00006. [DOI] [PubMed] [Google Scholar]
- Barker DJ, Winter PD, Osmond C, Margetts B, Simmonds SJ. Weight in infancy and death from ischaemic heart disease. Lancet. 1989;2:577–580. doi: 10.1016/s0140-6736(89)90710-1. [DOI] [PubMed] [Google Scholar]
- Basha MR, Wei W, Bakheet SA, Benitez N, Siddiqi HK, Ge YW, Lahiri DK, Zawia NH. The fetal basis of amyloidogenesis: exposure to lead and latent overexpression of amyloid precursor protein and β-amyloid in the aging brain. J Neurosci. 2005;25:823–829. doi: 10.1523/JNEUROSCI.4335-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilbo SD, Levkoff LH, Mahoney JH, Watkins LR, Rudy JW, Maier SF. Neonatal infection induces memory impairments following an immune challenge in adulthood. Behav Neurosci. 2005;119:293–301. doi: 10.1037/0735-7044.119.1.293. [DOI] [PubMed] [Google Scholar]
- Boksa P, El-Khodor BF. Birth insult interacts with stress at adulthood to alter dopaminergic function in animal models: possible implications for schizophrenia and other disorders. Neurosci Biobehav Rev. 2003;27:91–101. doi: 10.1016/s0149-7634(03)00012-5. [DOI] [PubMed] [Google Scholar]
- Bolin CM, Basha R, Cox D, Zawia NH, Maloney B, Lahiri DK, Cardozo-Pelaez F. Exposure to lead and the developmental origin of oxidative DNA damage in the aging brain. FASEB J. 2006;20:788–790. doi: 10.1096/fj.05-5091fje. [DOI] [PubMed] [Google Scholar]
- Castellani RJ, Lee HG, Perry G, Smith MA. Antioxidant protection and neurodegenerative disease: the role of amyloid-beta and tau. Am J Alzheimers Dis Other Demen. 2006;21:126–130. doi: 10.1177/153331750602100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cecchi C, Fiorillo C, Sorbi S, Latorraca S, Nacmias B, Bagnoli S, Nassi P, Liguri G. Oxidative stress and reduced antioxidant defenses in peripheral cells from familial Alzheimer's patients. Free Radic Biol Med. 2002;33:1372–1379. doi: 10.1016/s0891-5849(02)01049-3. [DOI] [PubMed] [Google Scholar]
- Christensen MA, Zhou W, Qing H, Lehman A, Philipsen S, Song W. Transcriptional regulation of BACE1, the beta-amyloid precursor protein beta-secretase, by Sp1. Mol Cell Biol. 2004;24:865–874. doi: 10.1128/MCB.24.2.865-874.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalman C, Allebeck P, Cullberg J, Grunewald C, Koster M. Obstetric complications and the risk of schizophrenia: a longitudinal study of a national birth cohort. Arch Gen Psychiatry. 1999;56:234–240. doi: 10.1001/archpsyc.56.3.234. [DOI] [PubMed] [Google Scholar]
- Dignam JD, Lebovitz RM, Roeder RG. Accurate transcription initiation by RNA polymerase II in a soluble extract from isolated mammalian nuclei. Nucleic Acids Res. 1983;11:1475–1489. doi: 10.1093/nar/11.5.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominguez DI, Hartmann D, De Strooper B. BACE1 and presenilin: two unusual aspartyl proteases involved in Alzheimer's disease. Neurodegener Dis. 2004;1:168–174. doi: 10.1159/000080982. [DOI] [PubMed] [Google Scholar]
- Esposito L, Raber J, Kekonius L, Yan F, Yu GQ, Bien-Ly N, Puolivali J, Scearce-Levie K, Masliah E, Mucke L. Reduction in mitochondrial superoxide dismutase modulates Alzheimer's disease-like pathology and accelerates the onset of behavioral changes in human amyloid precursor protein transgenic mice. J Neurosci. 2006;26:5167–5179. doi: 10.1523/JNEUROSCI.0482-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans MD, Cooke MS. Factors contributing to the outcome of oxidative damage to nucleic acids. Bioessays. 2004;26:533–542. doi: 10.1002/bies.20027. [DOI] [PubMed] [Google Scholar]
- Glenner GG, Wong CW. Alzheimer's disease: initial report of the purification and characterization of a novel cerebrovascular amyloid protein. Biochem Biophys Res Commun. 1984;120:885–890. doi: 10.1016/s0006-291x(84)80190-4. [DOI] [PubMed] [Google Scholar]
- Gluckman PD, Hanson MA. Living with the past: evolution, development, and patterns of disease. Science. 2004;305:1733–1736. doi: 10.1126/science.1095292. [DOI] [PubMed] [Google Scholar]
- Goldgaber D, Lerman MI, McBride OW, Saffiotti U, Gajdusek DC. Characterization and chromosomal localization of a cDNA encoding brain amyloid of Alzheimer's disease. Science. 1987;235:877–880. doi: 10.1126/science.3810169. [DOI] [PubMed] [Google Scholar]
- Jiang YH, Sahoo T, Michaelis RC, Bercovich D, Bressler J, Kashork CD, Liu Q, Shaffer LG, Schroer RJ, Stockton DW, Spielman RS, Stevenson RE, Beaudet AL. A mixed epigenetic/genetic model for oligogenic inheritance of autism with a limited role for UBE3A. Am J Med Genet A. 2004;131:1–10. doi: 10.1002/ajmg.a.30297. [DOI] [PubMed] [Google Scholar]
- Lahiri DK, Maloney B. Genes are not our destiny: the somatic epitype bridges between the genotype and the phenotype. Nat Rev Neurosci. 2007 in press. [Google Scholar]
- Lahiri DK, Robakis NK. The promoter activity of the gene encoding Alzheimer beta-amyloid precursor protein (APP) is regulated by two blocks of upstream sequences. Brain Res Mol Brain Res. 1991;9:253–257. doi: 10.1016/0169-328x(91)90009-m. [DOI] [PubMed] [Google Scholar]
- Lahiri DK, Maloney B, Basha MR, Ge YW, Zawia NH. How and when environmental agents and dietary factors affect the course of Alzheimer's disease: the “LEARn” model (latent early-life associated regulation) may explain the triggering of AD. Curr Alzheimer Res. 2007;4:219–228. doi: 10.2174/156720507780362164. [DOI] [PubMed] [Google Scholar]
- Masters CL, Simms G, Weinman NA, Multhaup G, McDonald BL, Beyreuther K. Amyloid plaque core protein in Alzheimer disease and Down syndrome. Proc Natl Acad Sci USA. 1985;82:4245–4249. doi: 10.1073/pnas.82.12.4245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mochizuki A, Peterson JW, Mufson EJ, Trapp BD. Amyloid load and neural elements in Alzheimer's disease and nondemented individuals with high amyloid plaque density. Exp Neurol. 1996;142:89–102. doi: 10.1006/exnr.1996.0181. [DOI] [PubMed] [Google Scholar]
- Morishima-Kawashima M, Oshima N, Ogata H, Yamaguchi H, Yoshimura M, Sugihara S, Ihara Y. Effect of apolipoprotein E allele epsilon4 on the initial phase of amyloid beta-protein accumulation in the human brain. Am J Pathol. 2000;157:2093–2099. doi: 10.1016/s0002-9440(10)64847-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niklowitz WJ, Mandybur TI. Neurofibrillary changes following childhood lead encephalopathy. J Neuropathol Exp Neurol. 1975;34:445–455. doi: 10.1097/00005072-197509000-00006. [DOI] [PubMed] [Google Scholar]
- Osmond C, Barker DJ. Fetal, infant, and childhood growth are predictors of coronary heart disease, diabetes, and hypertension in adult men and women. Environ Health Perspect. 2000;108(Suppl 3):545–553. doi: 10.1289/ehp.00108s3545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podlisny MB, Tolan DR, Selkoe DJ. Homology of the amyloid beta protein precursor in monkey and human supports a primate model for beta amyloidosis in Alzheimer's disease. Am J Pathol. 1991;138:1423–1435. [PMC free article] [PubMed] [Google Scholar]
- Poirier LA, Vlasova TI. The prospective role of abnormal methyl metabolism in cadmium toxicity. Environ Health Perspect. 2002;110(Suppl 5):793–795. doi: 10.1289/ehp.02110s5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollwein P, Masters CL, Beyreuther K. The expression of the amyloid precursor protein (APP) is regulated by two GC-elements in the promoter. Nucleic Acids Res. 1992;20:63–68. doi: 10.1093/nar/20.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price DL, Sisodia SS. Cellular and molecular biology of Alzheimer's disease and animal models. Annu Rev Med. 1994;45:435–446. doi: 10.1146/annurev.med.45.1.435. [DOI] [PubMed] [Google Scholar]
- Rice DC. Lead-induced behavioral impairment on a spatial discrimination reversal task in monkeys exposed during different periods of development. Toxicol Appl Pharmacol. 1990;106:327–333. doi: 10.1016/0041-008x(90)90251-o. [DOI] [PubMed] [Google Scholar]
- Rice DC. Effect of lead during different developmental periods in the monkey on concurrent discrimination performance. Neurotoxicology. 1992;13:583–592. [PubMed] [Google Scholar]
- Rogaev EI, Lukiw WJ, Lavrushina O, Rogaeva EA, St George-Hyslop PH. The upstream promoter of the beta-amyloid precursor protein gene (APP) shows differential patterns of methylation in human brain. Genomics. 1994;22:340–347. doi: 10.1006/geno.1994.1393. [DOI] [PubMed] [Google Scholar]
- Sambamurti K, Kinsey R, Maloney B, Ge YW, Lahiri DK. Gene structure and organization of the human beta-secretase (BACE) promoter. FASEB J. 2004;18:1034–1036. doi: 10.1096/fj.03-1378fje. [DOI] [PubMed] [Google Scholar]
- Schmitz C, Rutten BP, Pielen A, Schafer S, Wirths O, Tremp G, Czech C, Blanchard V, Multhaup G, Rezaie P, Korr H, Steinbusch HW, Pradier L, Bayer TA. Hippocampal neuron loss exceeds amyloid plaque load in a transgenic mouse model of Alzheimer's disease. Am J Pathol. 2004;164:1495–1502. doi: 10.1016/S0002-9440(10)63235-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer O, Marr RA, Rockenstein E, Crews L, Coufal NG, Gage FH, Verma IM, Masliah E. Targeting BACE1 with siRNAs ameliorates Alzheimer disease neuropathology in a transgenic model. Nat Neurosci. 2005;8:1343–1349. doi: 10.1038/nn1531. [DOI] [PubMed] [Google Scholar]
- Smith MA, Perry G. Free radical damage, iron, and Alzheimer's disease. J Neurol Sci. 1995;134(Suppl):92–94. doi: 10.1016/0022-510x(95)00213-l. [DOI] [PubMed] [Google Scholar]
- Sokol DK, Chen D, Farlow MR, Dunn DW, Maloney B, Zimmer JA, Lahiri DK. High levels of Alzheimer beta-amyloid precursor protein (APP) in children with severely autistic behavior and aggression. J Child Neurol. 2006;21:444–449. doi: 10.1177/08830738060210062201. [DOI] [PubMed] [Google Scholar]
- Song W, Lahiri DK. Molecular cloning of the promoter of the gene encoding the Rhesus monkey beta-amyloid precursor protein: structural characterization and a comparative study with other species. Gene. 1998;217:151–164. doi: 10.1016/s0378-1119(98)00337-0. [DOI] [PubMed] [Google Scholar]
- Takiguchi M, Achanzar WE, Qu W, Li G, Waalkes MP. Effects of cadmium on DNA-(cytosine-5) methyltransferase activity and DNA methylation status during cadmium-induced cellular transformation. Exp Cell Res. 2003;286:355–365. doi: 10.1016/s0014-4827(03)00062-4. [DOI] [PubMed] [Google Scholar]
- Tohgi H, Utsugisawa K, Nagane Y, Yoshimura M, Genda Y, Ukitsu M. Reduction with age in methylcytosine in the promoter region −224 approximately −101 of the amyloid precursor protein gene in autopsy human cortex. Brain Res Mol Brain Res. 1999;70:288–292. doi: 10.1016/s0169-328x(99)00163-1. [DOI] [PubMed] [Google Scholar]
- Valinluck V, Tsai HH, Rogstad DK, Burdzy A, Bird A, Sowers LC. Oxidative damage to methyl-CpG sequences inhibits the binding of the methyl-CpG binding domain (MBD) of methyl-CpG binding protein 2 (MeCP2) Nucleic Acids Res. 2004;32:4100–4108. doi: 10.1093/nar/gkh739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Erp TG, Saleh PA, Rosso IM, Huttunen M, Lonnqvist J, Pirkola T, Salonen O, Valanne L, Poutanen VP, Standertskjold-Nordenstam CG, Cannon TD. Contributions of genetic risk and fetal hypoxia to hippocampal volume in patients with schizophrenia or schizoaffective disorder, their unaffected siblings, and healthy unrelated volunteers. Am J Psychiatry. 2002;159:1514–1520. doi: 10.1176/appi.ajp.159.9.1514. [DOI] [PubMed] [Google Scholar]
- Villa A, Santiago J, Belandia B, Pascual A. A response unit in the first exon of the beta-amyloid precursor protein gene containing thyroid hormone receptor and Sp1 binding sites mediates negative regulation by 3,5,3′-triiodothyronine. Mol Endocrinol. 2004;18:863–873. doi: 10.1210/me.2003-0260. [DOI] [PubMed] [Google Scholar]
- Walsh DM, Minogue AM, Sala Frigerio C, Fadeeva JV, Wasco W, Selkoe DJ. The APP family of proteins: similarities and differences. Biochem Soc Trans. 2007;35:416–420. doi: 10.1042/BST0350416. [DOI] [PubMed] [Google Scholar]
- Zawia NH, Basha MR. Environmental risk factors and the developmental basis for Alzheimer's disease. Rev Neurosci. 2005;16:325–337. doi: 10.1515/revneuro.2005.16.4.325. [DOI] [PubMed] [Google Scholar]