Abstract
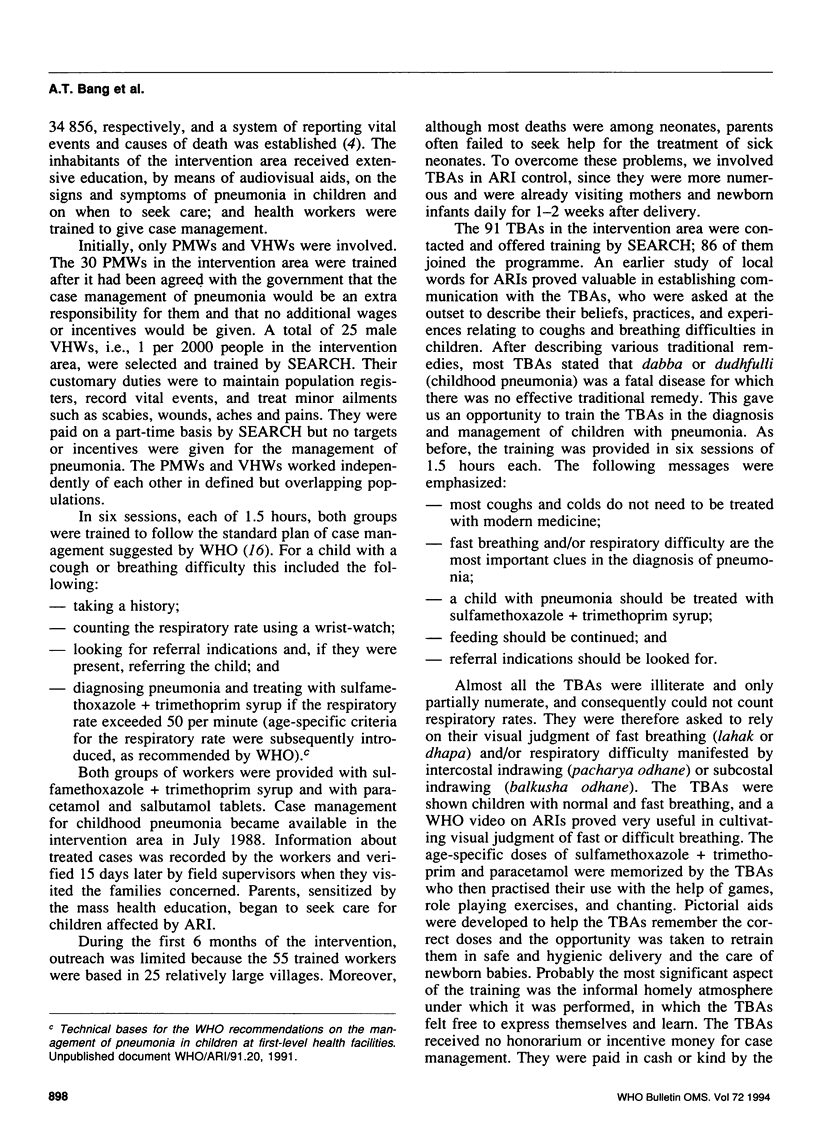
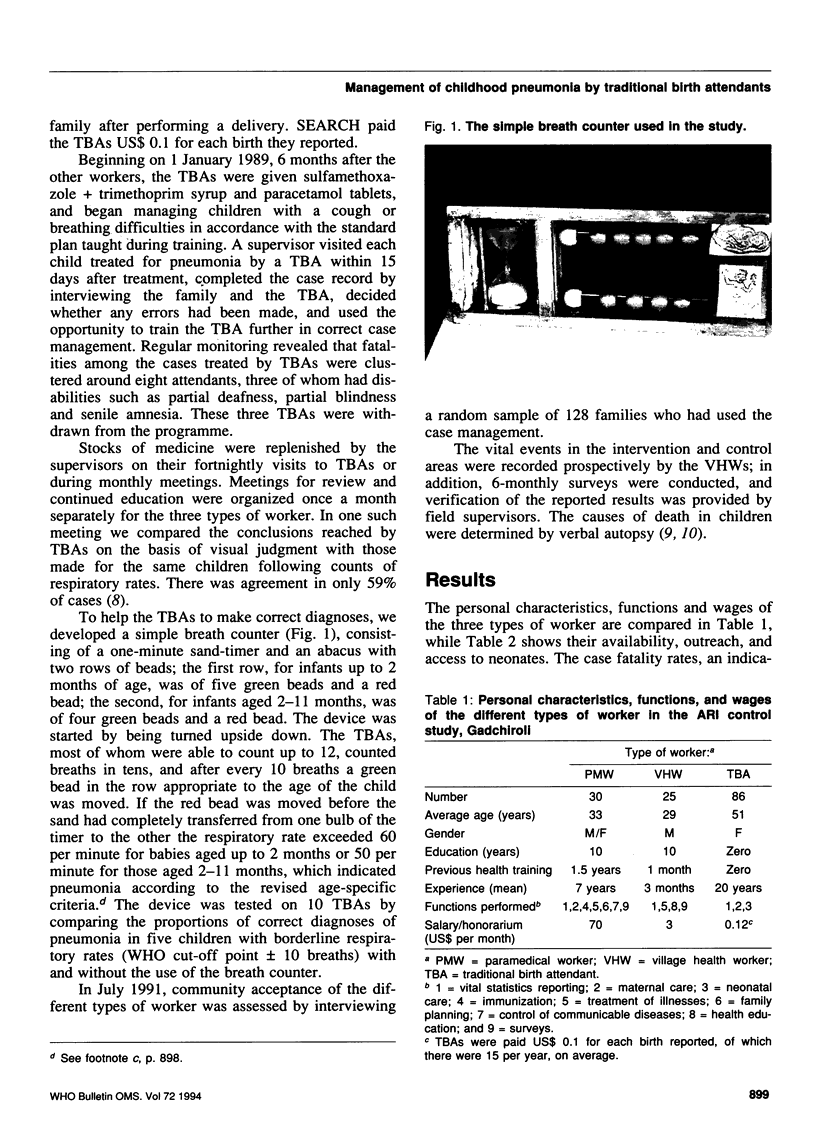
In a field trial in Gadchiroli, India, we trained 30 paramedical workers (PMWs), 25 village health workers (VHWs) and 86 traditional birth attendants (TBAs) from 58 villages to diagnose childhood pneumonia and treat it with sulfamethoxazole+trimethoprim. Continued training, the development of a breath counter, and educative supervision progressively reduced errors in case management made by the TBAs. Over the 3.5-year period 1988-91, 2568 attacks of childhood pneumonia were managed and the case fatality rate was 0.9%, compared with a rate of 13.5% in the control area. The case fatality rates for the three types of worker were similar. The TBAs were superior to the other workers in terms of their availability, outreach, access to neonates, and cost. Satisfaction with the VHWs, and PMWs was expressed by 85%, 69% and 18% of users, respectively. In the intervention area the mortality rate attributable to pneumonia among neonates declined by 44% (P < 0.01) while the total neonatal mortality fell by 20%, presumably because of the involvement of TBAs in the control of acute respiratory infections (ARI). If adequately supported by the health system, TBAs can successfully manage childhood pneumonia in villages at the lowest possible cost and with a high degree of community acceptance. TBAs and VHWs are the most suitable community-based health workers for ARI control programmes in developing countries.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bang A. T., Bang R. A. Breath counter for diagnosis of childhood pneumonia. Lancet. 1991 Jul 13;338(8759):116–116. doi: 10.1016/0140-6736(91)90108-2. [DOI] [PubMed] [Google Scholar]
- Bang A. T., Bang R. A. Diagnosis of causes of childhood deaths in developing countries by verbal autopsy: suggested criteria. The SEARCH Team. Bull World Health Organ. 1992;70(4):499–507. [PMC free article] [PubMed] [Google Scholar]
- Bang A. T., Bang R. A., Morankar V. P., Sontakke P. G., Solanki J. M. Pneumonia in neonates: can it be managed in the community? Arch Dis Child. 1993 May;68(5 Spec No):550–556. doi: 10.1136/adc.68.5_spec_no.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauveau V., Stewart M. K., Chakraborty J., Khan S. A. Impact on mortality of a community-based programme to control acute lower respiratory tract infections. Bull World Health Organ. 1992;70(1):109–116. [PMC free article] [PubMed] [Google Scholar]
- Khatua S. P., Gangwal A., Basu P., Palodhi P. K. The incidence and etiology of respiratory distress in newborn. Indian Pediatr. 1979 Dec;16(12):1121–1126. [PubMed] [Google Scholar]
- Pandey M. R., Daulaire N. M., Starbuck E. S., Houston R. M., McPherson K. Reduction in total under-five mortality in western Nepal through community-based antimicrobial treatment of pneumonia. Lancet. 1991 Oct 19;338(8773):993–997. doi: 10.1016/0140-6736(91)91847-n. [DOI] [PubMed] [Google Scholar]
- Sazawal S., Black R. E. Meta-analysis of intervention trials on case-management of pneumonia in community settings. Lancet. 1992 Aug 29;340(8818):528–533. doi: 10.1016/0140-6736(92)91720-s. [DOI] [PubMed] [Google Scholar]
- Shann F. Etiology of severe pneumonia in children in developing countries. Pediatr Infect Dis. 1986 Mar-Apr;5(2):247–252. doi: 10.1097/00006454-198603000-00017. [DOI] [PubMed] [Google Scholar]
- Thomas S., Verma I. C., Singh M., Menon P. S. Spectrum of respiratory distress syndrome in the newborn in North India: a prospective study. Indian J Pediatr. 1981 Jan-Feb;48(390):61–65. doi: 10.1007/BF02895190. [DOI] [PubMed] [Google Scholar]