Abstract
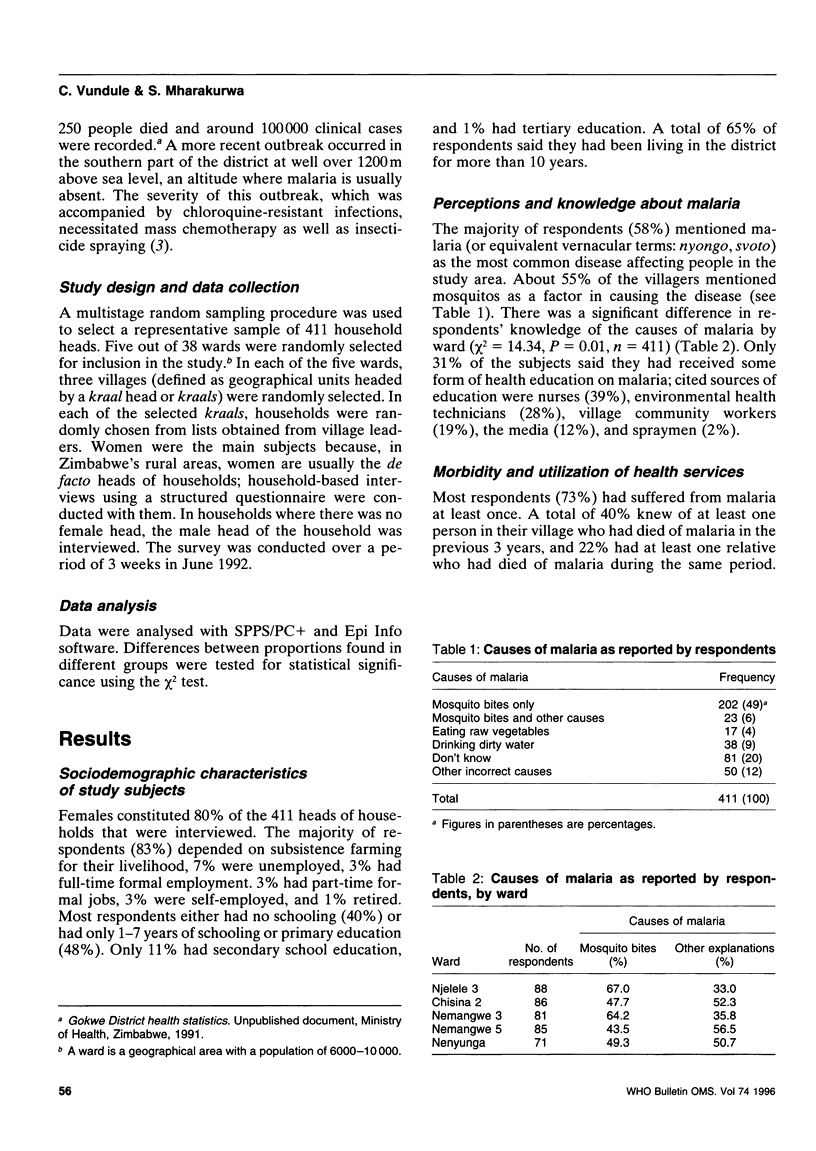
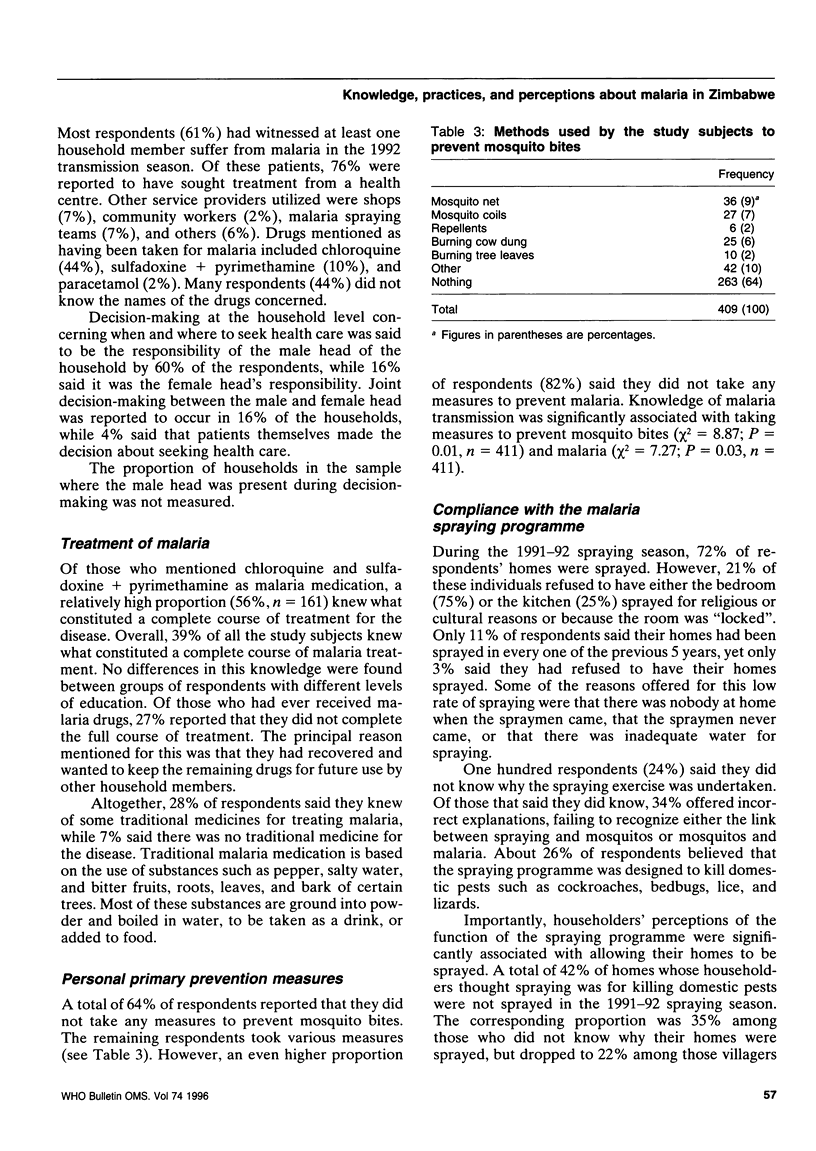
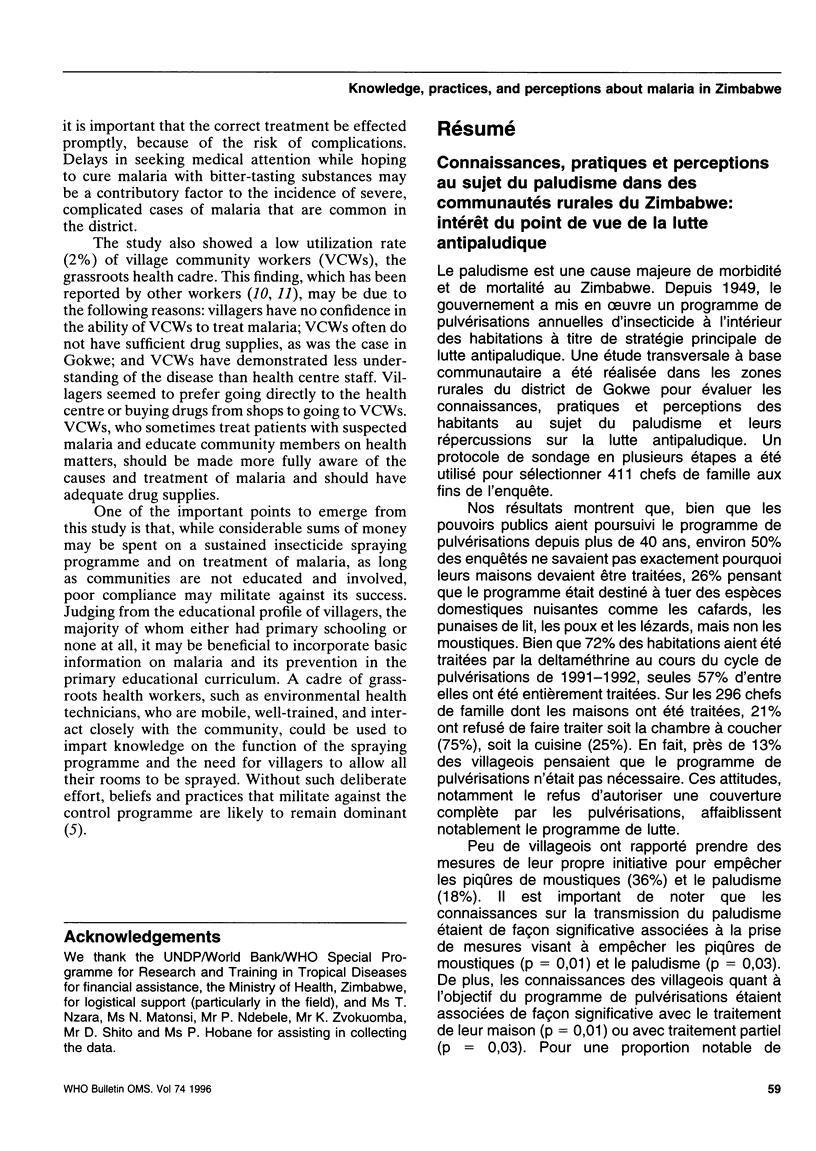
A survey of 411 household heads was undertaken in Gokwe district, Zimbabwe, to assess villagers' knowledge, practices and perceptions about malaria and their implications for malaria control. Our results show that although the government has sustained an annual indoor insecticide spraying programme for over four decades, about 50% of respondents did not adequately understand its purpose, with 26% believing that the programme was intended to kill domestic pests, not including mosquitos. During the 1991-92 spraying cycle, 72% of the villagers had their homes sprayed. However, 21% of such villagers refused to have some rooms in their homes sprayed. Householders' understanding of the function of the spraying programme was significantly related to their compliance with it (P < 0.05). A total of 82% of respondents reported not taking any measures to protect themselves from malaria. Taking preventive measures was significantly related to knowledge of the causes of malaria (P < 0.05). The study shows the importance of involving communities in a control programme intended to be to their benefit and of informing them about available options for protection against malaria.
Full text
PDF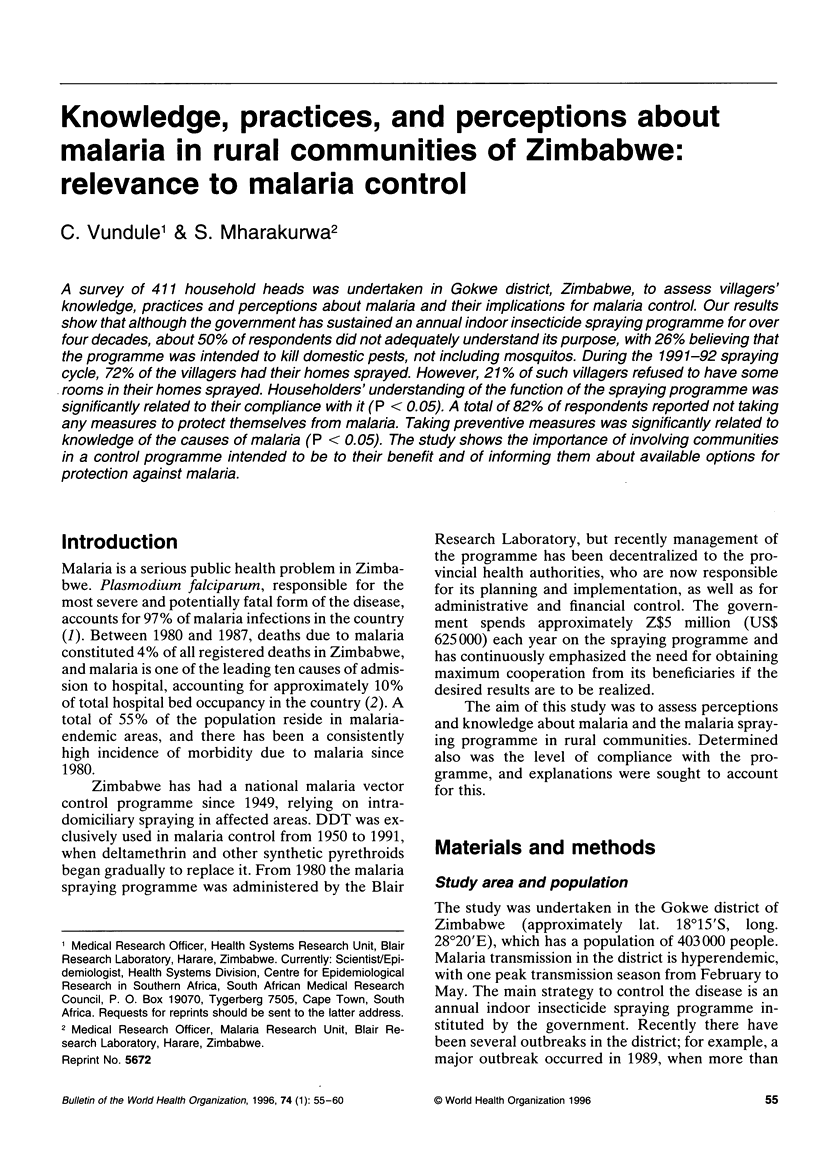

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Agyepong I. A. Malaria: ethnomedical perceptions and practice in an Adangbe farming community and implications for control. Soc Sci Med. 1992 Jul;35(2):131–137. doi: 10.1016/0277-9536(92)90160-r. [DOI] [PubMed] [Google Scholar]
- Castilla R. E., Sawyer D. O. Malaria rates and fate: a socioeconomic study of malaria in Brazil. Soc Sci Med. 1993 Nov;37(9):1137–1145. doi: 10.1016/0277-9536(93)90253-z. [DOI] [PubMed] [Google Scholar]
- Mharakurwa S., Mugochi T. Chloroquine-resistant falciparum malaria in an area of rising endemicity in Zimbabwe. J Trop Med Hyg. 1994 Feb;97(1):39–45. [PubMed] [Google Scholar]
- Mpofu S. M. Seasonal vector density and disease incidence patterns of malaria in an area of Zimbabwe. Trans R Soc Trop Med Hyg. 1985;79(2):169–175. doi: 10.1016/0035-9203(85)90327-x. [DOI] [PubMed] [Google Scholar]
- Ruebush T. K., 2nd, Weller S. C., Klein R. E. Qualities of an ideal volunteer community malaria worker: a comparison of the opinions of community residents and national malaria service staff. Soc Sci Med. 1994 Jul;39(1):123–131. doi: 10.1016/0277-9536(94)90172-4. [DOI] [PubMed] [Google Scholar]
- Sauerborn R., Nougtara A., Diesfeld H. J. Low utilization of community health workers: results from a household interview survey in Burkina Faso. Soc Sci Med. 1989;29(10):1163–1174. doi: 10.1016/0277-9536(89)90359-6. [DOI] [PubMed] [Google Scholar]
- Silva K. T. Ayurveda, malaria and the indigenous herbal tradition in Sri Lanka. Soc Sci Med. 1991;33(2):153–160. doi: 10.1016/0277-9536(91)90175-c. [DOI] [PubMed] [Google Scholar]
- Yeneneh H., Gyorkos T. W., Joseph L., Pickering J., Tedla S. Antimalarial drug utilization by women in Ethiopia: a knowledge-attitudes-practice study. Bull World Health Organ. 1993;71(6):763–772. [PMC free article] [PubMed] [Google Scholar]


