Abstract
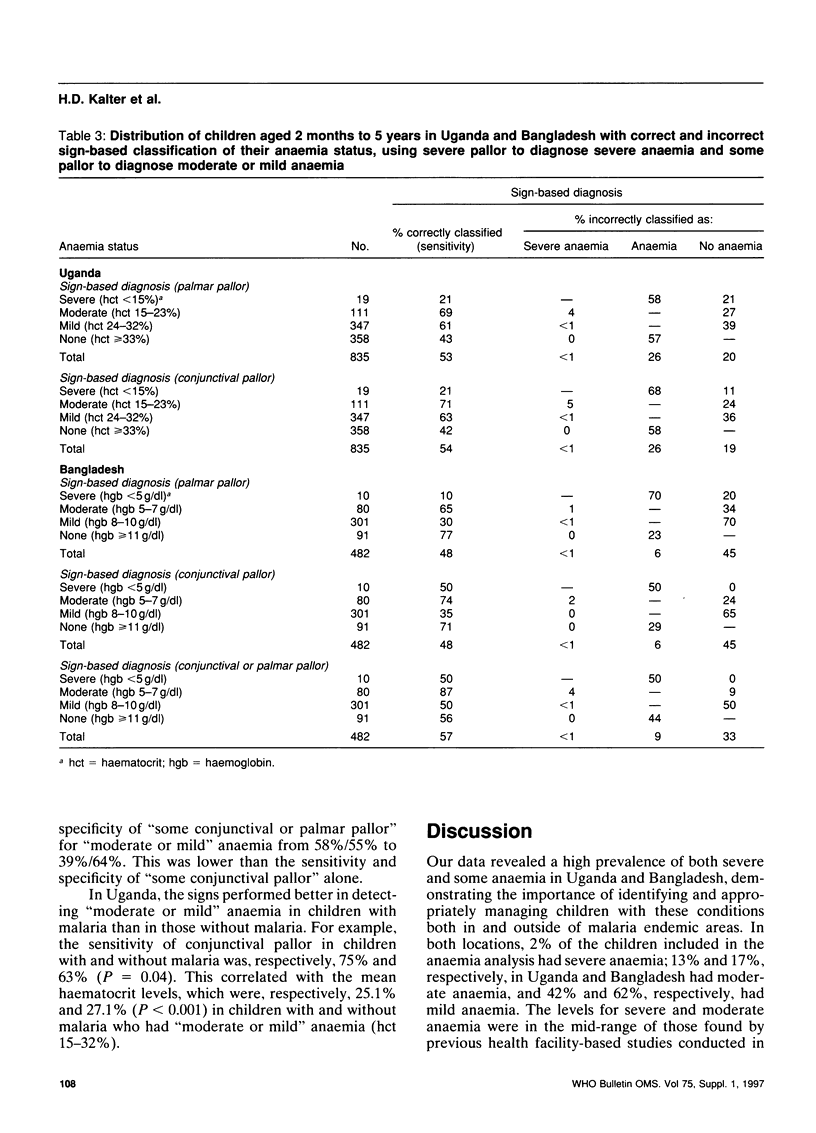
The object of this study was to assess the ability of pallor and other clinical signs, including those in the Integrated Management of Childhood Illness (IMCI) guidelines developed by WHO and UNICEF, to identify severe anaemia and some anaemia in developing country settings with and without malaria. A total of 1226 and 668 children aged 2 months to 5 years were prospectively sampled from patients presenting at, respectively, a district hospital in rural Uganda and a children's hospital in Dhaka, Bangladesh. The study physicians obtained a standardized history and carried out a physical examination that included pallor, signs of respiratory distress, and the remaining IMCI referral signs. The haematocrit or haemoglobin level was determined in all children with conjunctival or palmar pallor, and in a sample of the rest. Children with a blood level measurement and assessment of pallor at both sites were included in the anaemia analysis. Using the haematocrit or haemoglobin level as the reference standard, the correctness of assessments using severe and some pallor and other clinical signs in classifying severe and some anaemia was determined. While the full IMCI process would have referred most of the children in Uganda and nearly all the children in Bangladesh with severe anaemia to hospital, few would have received a diagnosis of severe anaemia. Severe palmar and conjunctival pallor, individually and together, had 10-50% sensitivity and 99% specificity for severe anaemia; the addition of grunting increased the sensitivity to 37-80% while maintaining a reasonable positive predictive value. Palmar pallor did not work as well as conjunctival pallor in Bangladesh for the detection for severe or some anaemia. Combining "conjunctival or palmar pallor" detected 71-87% of moderate anaemia and half or more of mild anaemia. About half the children with no anaemia were incorrectly classified as having "moderate or mild" anaemia. Anaemia was more easily diagnosed in Uganda in children with malaria. Our results show that simple clinical signs can correctly classify the anaemia status of most children. Grunting may serve as a useful adjunct to pallor in the diagnosis of severe anaemia. Conjunctival pallor should be added to the IMCI anaemia box, or the guidelines need to be adapted in regions where palmar pallor may not readily be detected.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aukett M. A., Parks Y. A., Scott P. H., Wharton B. A. Treatment with iron increases weight gain and psychomotor development. Arch Dis Child. 1986 Sep;61(9):849–857. doi: 10.1136/adc.61.9.849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatia D., Seshadri S. Growth performance in anemia and following iron supplementation. Indian Pediatr. 1993 Feb;30(2):195–200. [PubMed] [Google Scholar]
- Blot I., Vovor A. Les anémies chez l'enfant du tiers monde. Rev Prat. 1989 Oct 21;39(24):2125–2127. [PubMed] [Google Scholar]
- Cook J. D., Skikne B. S., Baynes R. D. Iron deficiency: the global perspective. Adv Exp Med Biol. 1994;356:219–228. doi: 10.1007/978-1-4615-2554-7_24. [DOI] [PubMed] [Google Scholar]
- Hedberg K., Shaffer N., Davachi F., Hightower A., Lyamba B., Paluku K. M., Nguyen-Dinh P., Breman J. G. Plasmodium falciparum-associated anemia in children at a large urban hospital in Zaire. Am J Trop Med Hyg. 1993 Mar;48(3):365–371. doi: 10.4269/ajtmh.1993.48.365. [DOI] [PubMed] [Google Scholar]
- Integrated management of the sick child. Bull World Health Organ. 1995;73(6):735–740. [PMC free article] [PubMed] [Google Scholar]
- Johnson S. R., Winkleby M. A., Boyce W. T., McLaughlin R., Broadwin R., Goldman L. The association between hemoglobin and behavior problems in a sample of low-income Hispanic preschool children. J Dev Behav Pediatr. 1992 Jun;13(3):209–214. [PubMed] [Google Scholar]
- Kasili E. G. Malnutrition and infections as causes of childhood anemia in tropical Africa. Am J Pediatr Hematol Oncol. 1990 Fall;12(3):375–377. doi: 10.1097/00043426-199023000-00023. [DOI] [PubMed] [Google Scholar]
- Lackritz E. M., Campbell C. C., Ruebush T. K., 2nd, Hightower A. W., Wakube W., Steketee R. W., Were J. B. Effect of blood transfusion on survival among children in a Kenyan hospital. Lancet. 1992 Aug 29;340(8818):524–528. doi: 10.1016/0140-6736(92)91719-o. [DOI] [PubMed] [Google Scholar]
- Luby S. P., Kazembe P. N., Redd S. C., Ziba C., Nwanyanwu O. C., Hightower A. W., Franco C., Chitsulo L., Wirima J. J., Olivar M. A. Using clinical signs to diagnose anaemia in African children. Bull World Health Organ. 1995;73(4):477–482. [PMC free article] [PubMed] [Google Scholar]
- Masawe A. E. Nutritional anaemias. Part 1: Tropical Africa. Clin Haematol. 1981 Oct;10(3):815–842. [PubMed] [Google Scholar]
- Nardone D. A., Roth K. M., Mazur D. J., McAfee J. H. Usefulness of physical examination in detecting the presence or absence of anemia. Arch Intern Med. 1990 Jan;150(1):201–204. [PubMed] [Google Scholar]
- Renaudin P., Lombart J. P. L'anémie de l'enfant de moins de un an à Moundou, Tchad: prévalence et étiologies. Med Trop (Mars) 1994;54(4):337–342. [PubMed] [Google Scholar]
- Strobach R. S., Anderson S. K., Doll D. C., Ringenberg Q. S. The value of the physical examination in the diagnosis of anemia. Correlation of the physical findings and the hemoglobin concentration. Arch Intern Med. 1988 Apr;148(4):831–832. [PubMed] [Google Scholar]
- Thaver I. H., Baig L. Anaemia in children: Part I. Can simple observations by primary care provider help in diagnosis? J Pak Med Assoc. 1994 Dec;44(12):282–284. [PubMed] [Google Scholar]
- Walter T., De Andraca I., Chadud P., Perales C. G. Iron deficiency anemia: adverse effects on infant psychomotor development. Pediatrics. 1989 Jul;84(1):7–17. [PubMed] [Google Scholar]
- Walter T. Effect of iron-deficiency anaemia on cognitive skills in infancy and childhood. Baillieres Clin Haematol. 1994 Dec;7(4):815–827. doi: 10.1016/s0950-3536(05)80126-x. [DOI] [PubMed] [Google Scholar]
- Zucker J. R., Perkins B. A., Jafari H., Otieno J., Obonyo C., Campbell C. C. Clinical signs for the recognition of children with moderate or severe anaemia in western Kenya. Bull World Health Organ. 1997;75 (Suppl 1):97–102. [PMC free article] [PubMed] [Google Scholar]
- von Schenck H., Falkensson M., Lundberg B. Evaluation of "HemoCue," a new device for determining hemoglobin. Clin Chem. 1986 Mar;32(3):526–529. [PubMed] [Google Scholar]


