Abstract
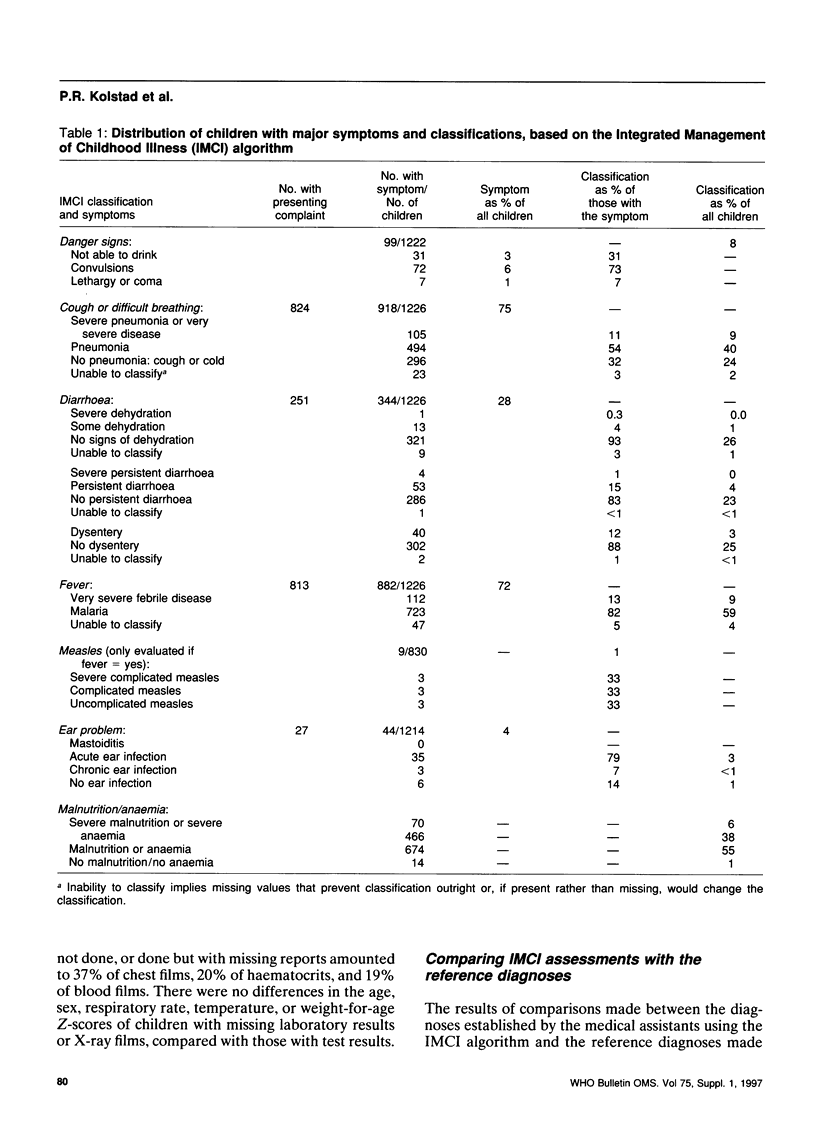
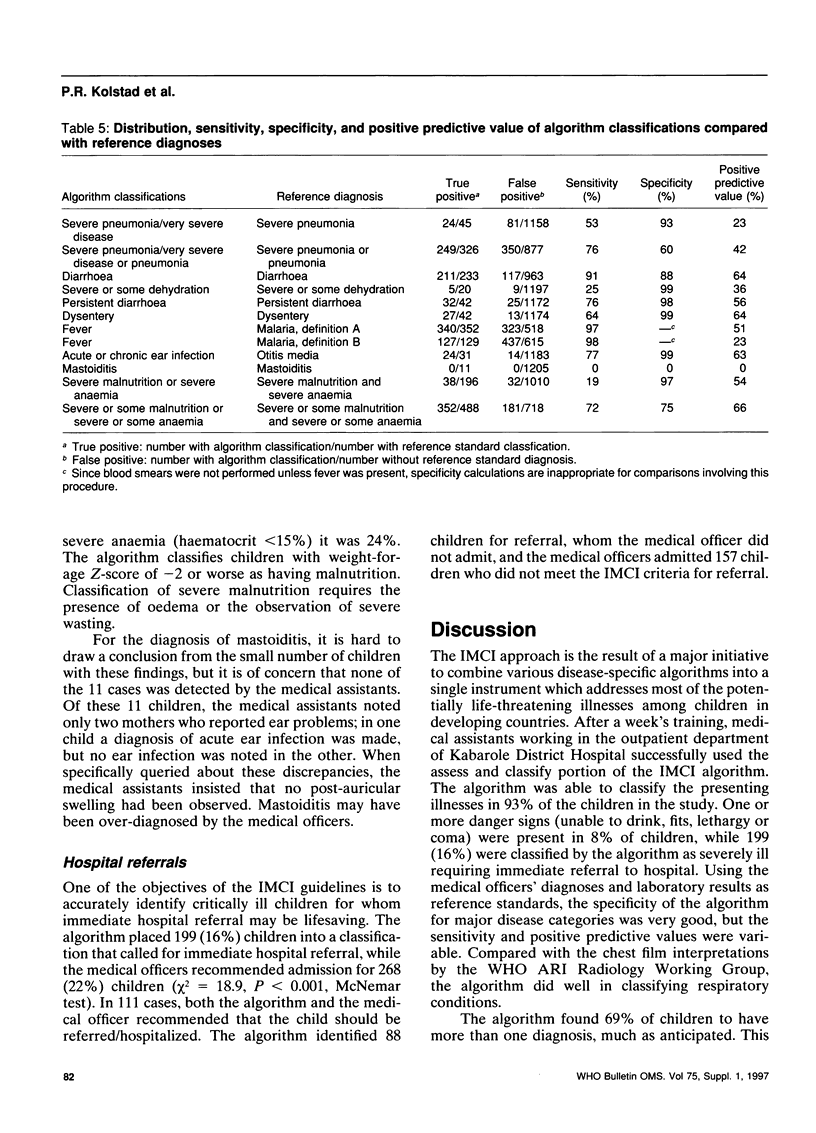
Bringing together various disease-specific guidelines for sick children, WHO and UNICEF have developed an Integrated Management of Childhood Illness (IMCI) algorithm, one component of which (assess and classify) was tested in the outpatient department of a rural district hospital in western Uganda. Children aged 2-59 months were seen first by a Ugandan medical assistant trained in IMCI, and then evaluated by a medical officer. Sensitivity, specificity and positive predictive values were determined by comparing the IMCI classifications with a reference standard based on the medical officers' diagnoses and laboratory tests. Of the 1226 children seen, 69% were classified into more than one symptom category, 7% were not classified in any symptom category, 8% had a danger sign, and 16% were classified into a severe category, for which the IMCI approach recommended urgent hospital referral. Specificity for most classifications was good, though sensitivity and positive predictive values were variable. We conclude that the IMCI algorithm is an important advance in the primary care of sick children in developing countries.
Full text
PDF






Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cherian T., John T. J., Simoes E., Steinhoff M. C., John M. Evaluation of simple clinical signs for the diagnosis of acute lower respiratory tract infection. Lancet. 1988 Jul 16;2(8603):125–128. doi: 10.1016/s0140-6736(88)90683-6. [DOI] [PubMed] [Google Scholar]
- Fagbule D., Kalu A. Case management by community health workers of children with acute respiratory infections: implications for national ARI control programme. J Trop Med Hyg. 1995 Aug;98(4):241–246. [PubMed] [Google Scholar]
- Gove S., Tulloch J., Cattani J., Schapira A. Usefulness of clinical case-definitions in treatment of childhood malaria or pneumonia. Lancet. 1993 Jan 30;341(8840):304–305. doi: 10.1016/0140-6736(93)92655-d. [DOI] [PubMed] [Google Scholar]
- Sazawal S., Black R. E. Meta-analysis of intervention trials on case-management of pneumonia in community settings. Lancet. 1992 Aug 29;340(8818):528–533. doi: 10.1016/0140-6736(92)91720-s. [DOI] [PubMed] [Google Scholar]
- Simoes E. A., McGrath E. J. Recognition of pneumonia by primary health care workers in Swaziland with a simple clinical algorithm. Lancet. 1992 Dec 19;340(8834-8835):1502–1503. doi: 10.1016/0140-6736(92)92757-7. [DOI] [PubMed] [Google Scholar]
- Singhi S., Dhawan A., Kataria S., Walia B. N. Validity of clinical signs for the identification of pneumonia in children. Ann Trop Paediatr. 1994;14(1):53–58. doi: 10.1080/02724936.1994.11747692. [DOI] [PubMed] [Google Scholar]


