Abstract
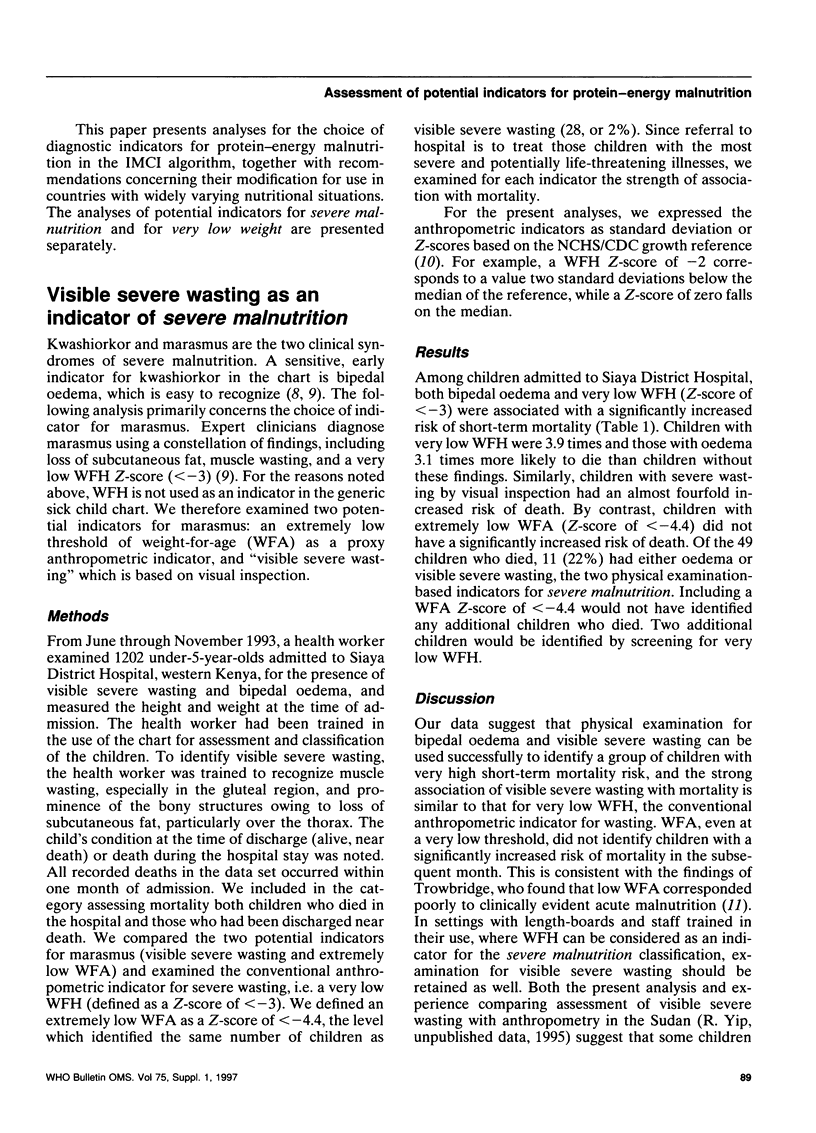
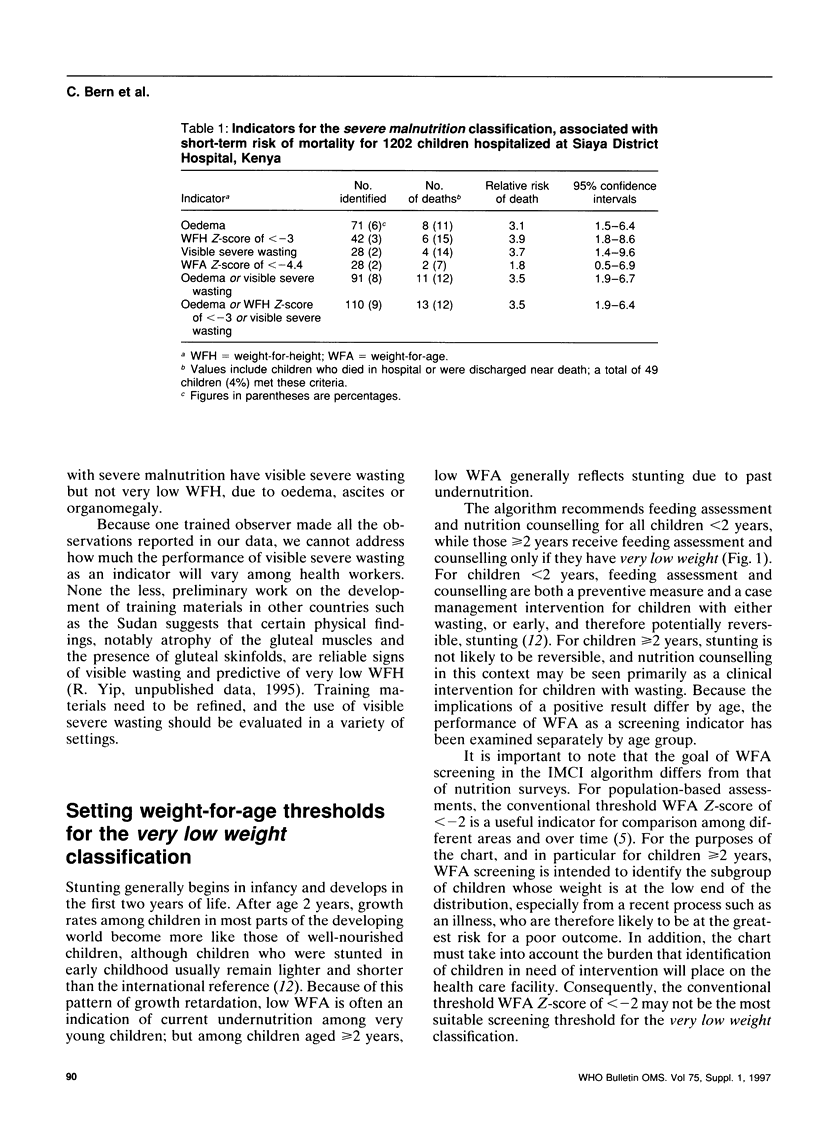
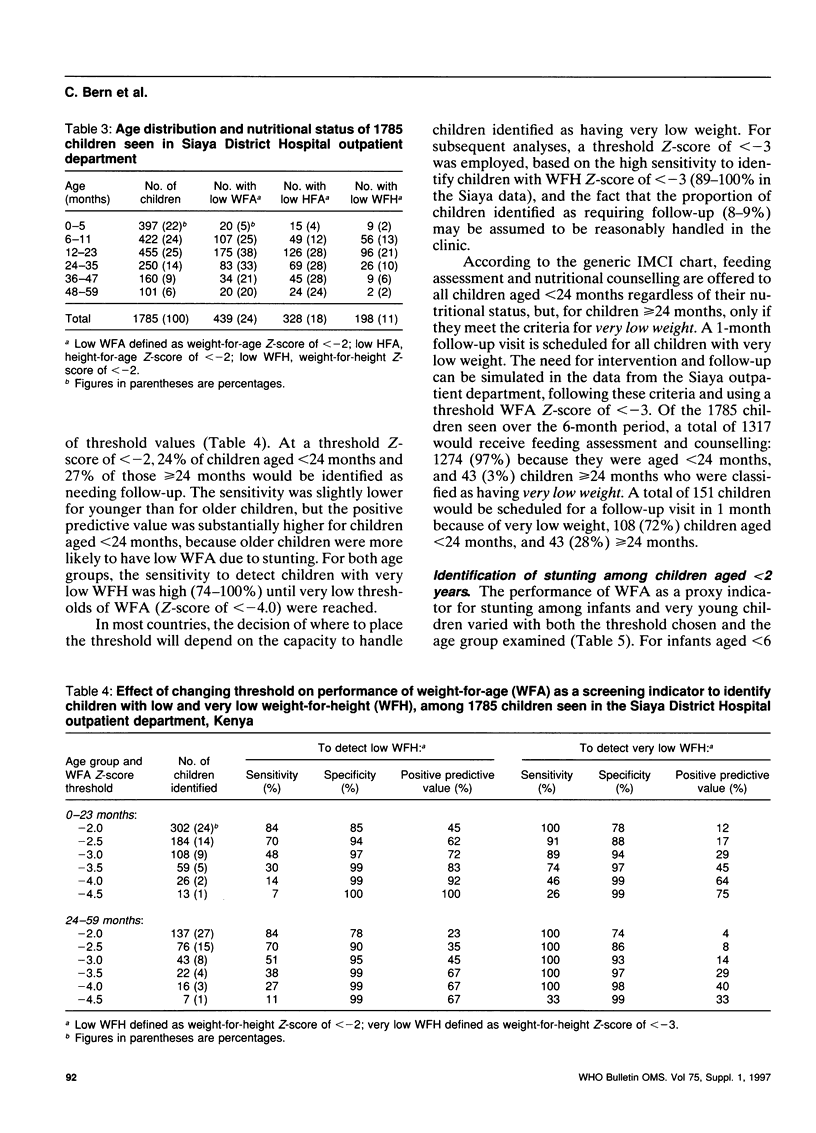
Potential indicators were assessed for the two classifications of protein-energy malnutrition in the guidelines for integrated management of childhood illness: severe malnutrition, which requires immediate referral to hospital, and very low weight, which calls for feeding assessment, nutritional counselling and follow-up. Children aged < 2 years require feeding assessment and counselling as a preventive intervention. For severe malnutrition, we examined 1202 children admitted to a Kenyan hospital for any association of the indicators with mortality within one month. Bipedal oedema indicating kwashiorkor, and two marasmus indicators (visible severe wasting and weight-for-height (WFH) Z-score of < -3) were associated with a significantly increased mortality risk (odds ratios, 3.1-3.9). Very low weight-for-age (WFA) (Z-score of < -4.4) was not associated with an increased risk of mortality. Because first-level health facilities generally lack length-boards, bipedal oedema and visible severe wasting were chosen as indicators of severe malnutrition. To assess potential WFA thresholds for the very low weight classification, our primary source of data came from 1785 Kenyan outpatient children, but we also examined data from surveys in Nepal, Bolivia, and Togo. We examined the performance of WFA at various thresholds to identify children with low WFH and, for children aged < or = 2 years, low height-for-age (HFA). Use of a WFA threshold Z-score of < -2 identified a considerable proportion of children (from 13% in Bolivia to 68% in Nepal) which, in most settings, would pose an enormous burden on the health facility. Among ill children in Kenya, a threshold WFA Z-score of < -3 had a sensitivity of 89-100% to detect children with WFH Z-scores of < -3, and, with an identification rate of 9%, would avoid overburdening the clinics. Potential modifications include use of a more restrictive cut-off in countries with high rates of stunting, or the elimination of the WFA screen in order to concentrate efforts on intervention for all children below the 2-year age cut-off. Key issues in every country include the capacity to provide counselling for many children and linkage to nutritional improvement programmes in the community.
Full text
PDF




Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brink E. W., Khan I. H., Splitter J. L., Staehling N. W., Lane J. M., Nichaman M. Z. Nutritional status of children in Nepal, 1975. Bull World Health Organ. 1976;54(3):311–318. [PMC free article] [PubMed] [Google Scholar]
- Gorstein J., Sullivan K., Yip R., de Onís M., Trowbridge F., Fajans P., Clugston G. Issues in the assessment of nutritional status using anthropometry. Bull World Health Organ. 1994;72(2):273–283. [PMC free article] [PubMed] [Google Scholar]
- Martorell R., Khan L. K., Schroeder D. G. Reversibility of stunting: epidemiological findings in children from developing countries. Eur J Clin Nutr. 1994 Feb;48 (Suppl 1):S45–S57. [PubMed] [Google Scholar]
- Pelletier D. L., Frongillo E. A., Jr, Schroeder D. G., Habicht J. P. A methodology for estimating the contribution of malnutrition to child mortality in developing countries. J Nutr. 1994 Oct;124(10 Suppl):2106S–2122S. doi: 10.1093/jn/124.suppl_10.2106S. [DOI] [PubMed] [Google Scholar]
- Perkins B. A., Zucker J. R., Otieno J., Jafari H. S., Paxton L., Redd S. C., Nahlen B. L., Schwartz B., Oloo A. J., Olango C. Evaluation of an algorithm for integrated management of childhood illness in an area of Kenya with high malaria transmission. Bull World Health Organ. 1997;75 (Suppl 1):33–42. [PMC free article] [PubMed] [Google Scholar]
- Ruel M. T., Rivera J., Habicht J. P. Length screens better than weight in stunted populations. J Nutr. 1995 May;125(5):1222–1228. doi: 10.1093/jn/125.5.1222. [DOI] [PubMed] [Google Scholar]
- Schroeder D. G., Brown K. H. Nutritional status as a predictor of child survival: summarizing the association and quantifying its global impact. Bull World Health Organ. 1994;72(4):569–579. [PMC free article] [PubMed] [Google Scholar]
- Trowbridge F. L. Clinical and biochemical characteristics associated with anthropometric nutritional categories. Am J Clin Nutr. 1979 Apr;32(4):758–766. doi: 10.1093/ajcn/32.4.758. [DOI] [PubMed] [Google Scholar]
- Use and interpretation of anthropometric indicators of nutritional status. WHO Working Group. Bull World Health Organ. 1986;64(6):929–941. [PMC free article] [PubMed] [Google Scholar]
- Van Den Broeck J., Eeckels R., Vuylsteke J. Influence of nutritional status on child mortality in rural Zaire. Lancet. 1993 Jun 12;341(8859):1491–1495. doi: 10.1016/0140-6736(93)90632-q. [DOI] [PubMed] [Google Scholar]
- Yip R., Scanlon K. The burden of malnutrition: a population perspective. J Nutr. 1994 Oct;124(10 Suppl):2043S–2046S. doi: 10.1093/jn/124.suppl_10.2043S. [DOI] [PubMed] [Google Scholar]
- de Onís M., Monteiro C., Akré J., Glugston G. The worldwide magnitude of protein-energy malnutrition: an overview from the WHO Global Database on Child Growth. Bull World Health Organ. 1993;71(6):703–712. [PMC free article] [PubMed] [Google Scholar]



