Abstract
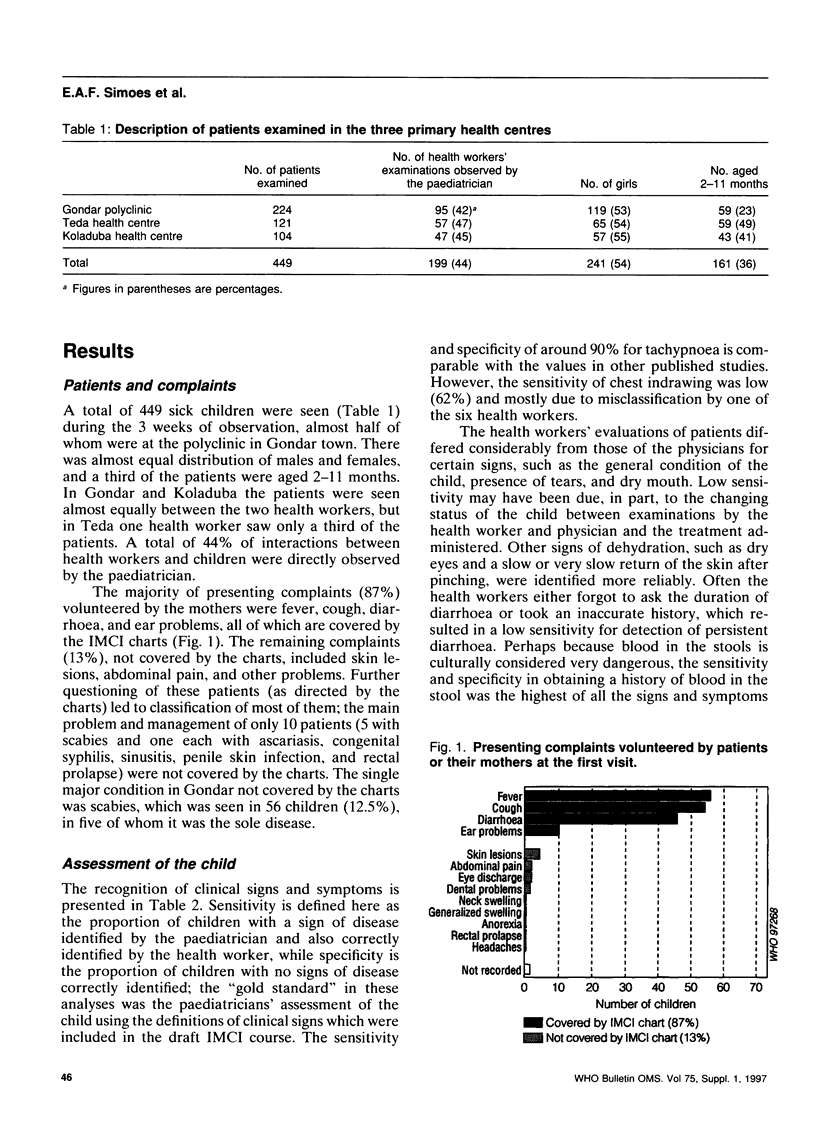
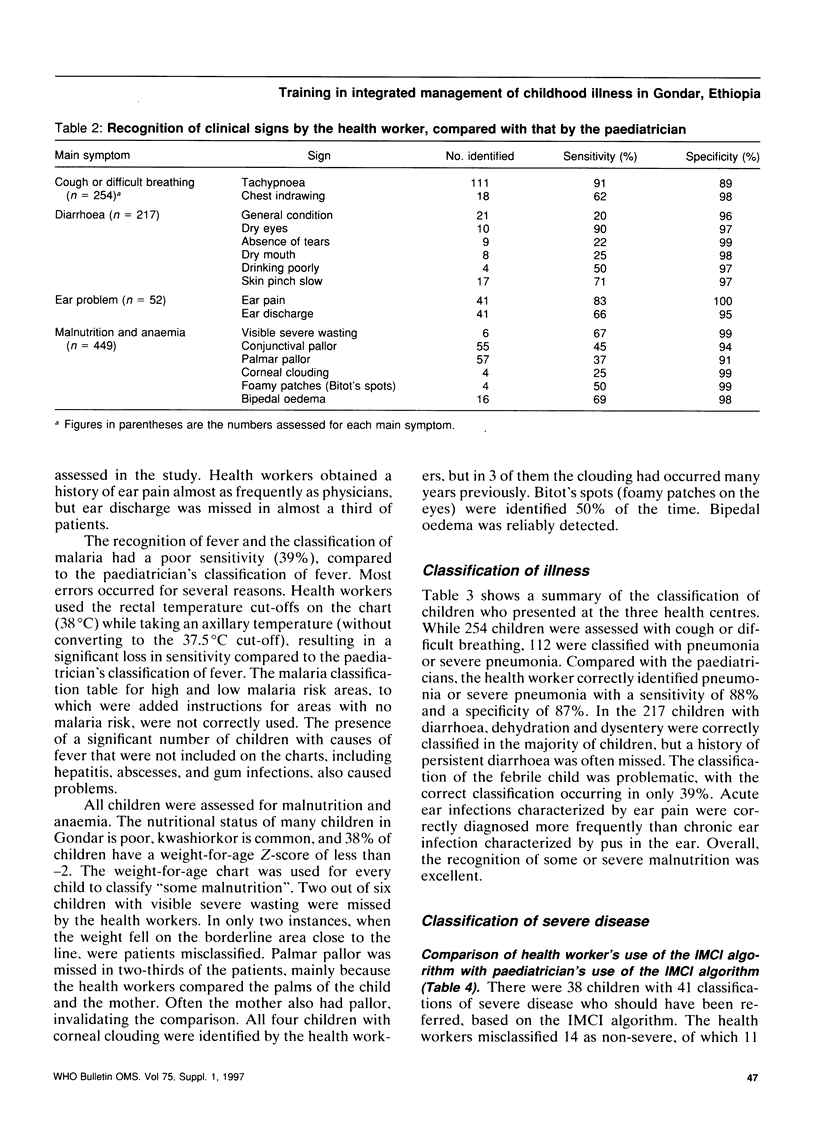
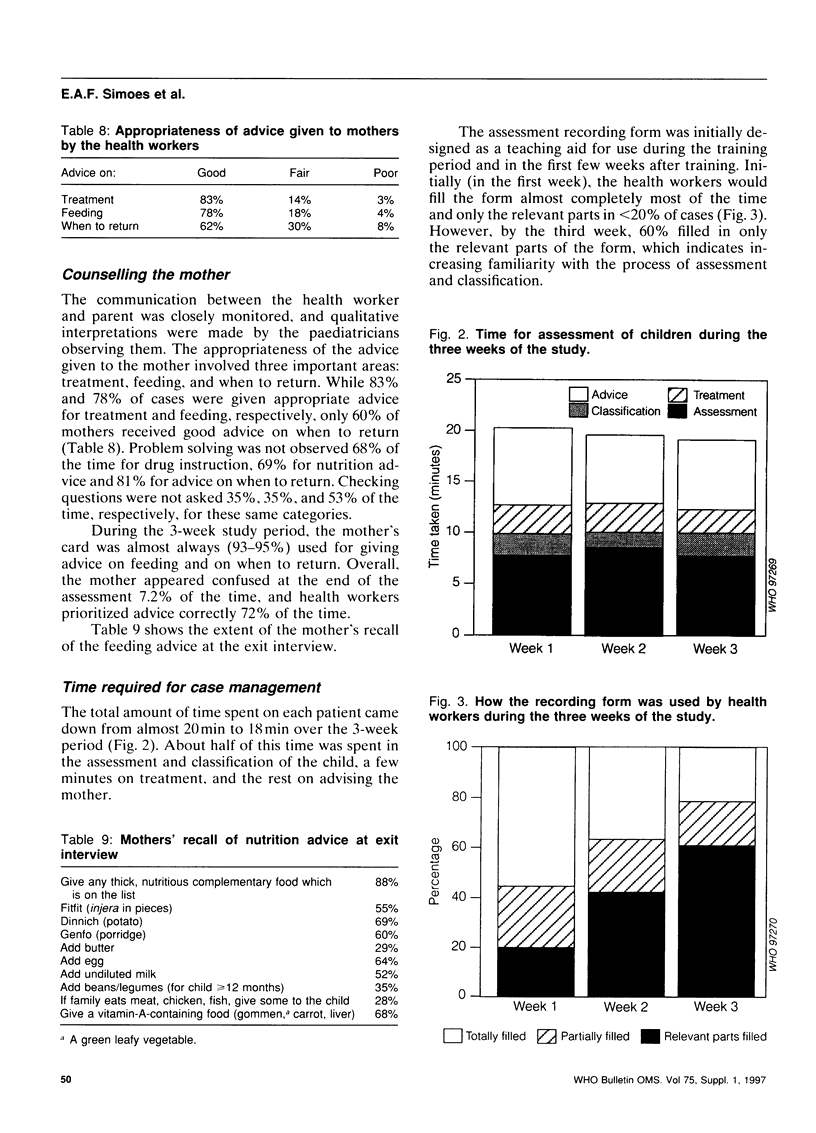
The performance of six primary health workers was evaluated after following a 9-day training course on integrated management of childhood illness (IMCI). The participants were selected from three primary health centres in the Gondar District, Ethiopia, and the course was focused on assessment, classification, and treatment of sick children (aged 2 months to 5 years) and on counselling of their mothers. Immediately following this training, a 3-week study was conducted in the primary health centres to determine how well these workers performed in assessing, classifying and treating the children and in counselling the mothers. A total of 449 sick children who presented at the three primary health centres during the study period were evaluated. Most of the complaints (87%) volunteered by the mothers (fever, cough, diarrhoea, and ear problems) were covered by the IMCI charts. The assessment of commonly seen signs (tachypnoea or ear pain) or easily identifiable signs (slow return after skin pinch, wasting, or pedal oedema) was good, with sensitivities of 67-91%, whereas the assessment of uncommonly seen signs (dry mouth, corneal clouding) or less easily quantifiable signs (eyelid pallor, absence of tears) had a fair or poor sensitivity of 20-45%. The classification of pneumonia, diarrhoea with signs of dehydration, and malnutrition showed sensitivities of 88%, 76%, and 85% and specificities of 87%, 98%, and 96%, respectively. However, the classification of febrile illnesses had a sensitivity of only 39% due to problems in using the draft algorithm in areas with a mixture of high, low, and no malaria risk, and due to confusion between axillary and rectal temperature thresholds. Of 39 children classified as having severe disease, 9 were misclassified, mostly by one nurse. Treatment of patients improved over the three weeks of observation, their completeness increasing from 69% to 88%. Health workers usually communicated appropriate advice to the mother. They learned to use checking questions but failed to adequately solve problems in the majority of cases. The mother's counselling card, which summarized recommendations on feeding and home fluids, and advice on when to return, was widely used to aid communication. The time taken to perform the complete management of children did not change significantly (20 to 19 minutes) during the study. Lessons from our findings have been incorporated into an improved version of the IMCI charts.
Full text
PDF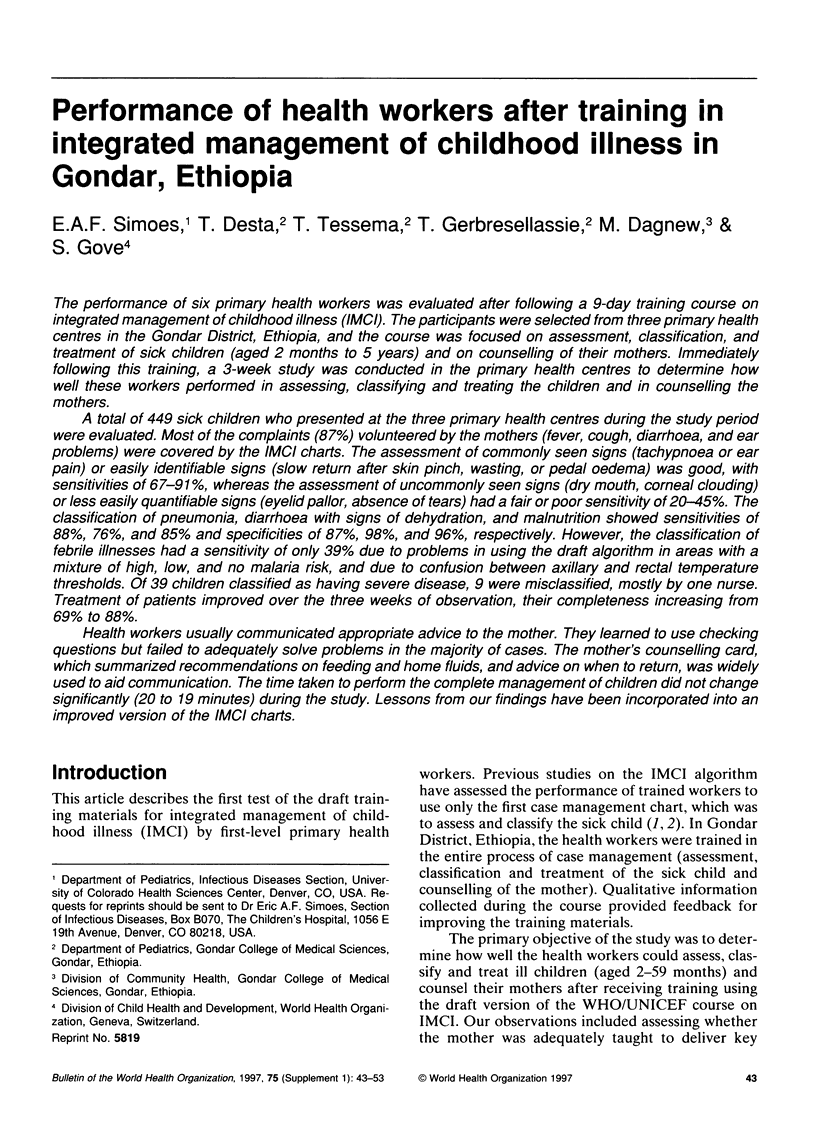



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Weber M. W., Kellingray S. D., Palmer A., Jaffar S., Mulholland E. K., Greenwood B. M. Pallor as a clinical sign of severe anaemia in children: an investigation in the Gambia. Bull World Health Organ. 1997;75 (Suppl 1):113–118. [PMC free article] [PubMed] [Google Scholar]
- Zucker J. R., Perkins B. A., Jafari H., Otieno J., Obonyo C., Campbell C. C. Clinical signs for the recognition of children with moderate or severe anaemia in western Kenya. Bull World Health Organ. 1997;75 (Suppl 1):97–102. [PMC free article] [PubMed] [Google Scholar]



