Abstract
Acetabular fractures in the elderly population are marked by a high degree of variability in terms of patient and fracture characteristics. Successful outcomes depend on application of highly individualized management principles by experienced teams. Reviewed are indications and outcomes associated with various management options, including closed treatment, open reduction internal fixation, and acute or staged total hip arthroplasty. Proper initial management choices are critical, as early failures and subsequent salvage surgery can be accompanied by significant morbidity. Clinical results after ORIF closely follow the quality of articular reduction and the ability to maintain a congruent reduction of the hip joint. Fracture characteristics predictive of anatomic articular reduction should be treated with ORIF. Fracture characteristics predictive of early post-traumatic arthritis should be treated with simultaneous ORIF and THA. Presented is one referral institution’s treatment algorithm and management approach.
Key words: acetabulum, fracture, elderly, osteoporosis, total hip arthroplasty
Introduction
The U.S. population is aging. By 2030, it is estimated that 17% of the population (55 million Americans) will be over 65 years [12]. Elderly individuals consequently represent the most rapidly growing subgroup of patients currently sustaining acetabular fractures [19]. The incidence of such fractures is expected to approximately double over the next 20 years [1]. The goal of treatment is to reconstitute the hip joint to provide a stable, painless construct capable of rapidly recovering its preinjury level of function. Successful open reduction and internal fixation (ORIF) and total hip arthroplasty (THA) are both treatment options compatible with achieving these goals in properly selected patients. However, treatment decisions must be highly individualized. Early referral to an appropriate center experienced in acetabular reconstruction is to be encouraged.
Multiple subsets exist within the elderly population. These can be generally categorized as patient factors, injury factors, or treatment factors. Patient factors in the elderly include physiologic age, degree of underlying osteoporosis, comorbid medical conditions, preexisting degenerative joint disease (DJD), premorbid activity level, and baseline mental function. Injury factors include injury mechanism, fracture characteristics, and presence of associated injuries. Treatment factors include the chosen management pathway, the quality and timing of treatment rendered, and the deleterious effects of any perioperative complications. Of these, only treatment factors are under the control of the operative team. Optimal management of the elderly patient with an acetabular fracture requires that each of these factors be considered when formulating the treatment plan.
Clinical presentation
Acetabular fractures in the elderly can occur in the setting of high- or low-energy trauma. The degree of underlying osteoporosis determines the resultant fracture characteristics. Structurally compromising osteoporosis is heralded by fractures induced by minor trauma, such as a fall from standing height [21]. In this instance, forces are commonly directed through the greater trochanter resulting in comminuted fractures of the anterior column and quadrilateral plate with central dislocation of the femoral head. In the face of minimal osteoporotic changes, high-energy mechanisms often result in typical fracture patterns as encountered in younger patients. As the severity of osteoporosis increases, however, so does the extent of comminution, impaction, and cartilage loss. Difficulties associated with achieving anatomic reduction of such patterns results in an increased likelihood of posttraumatic changes.
Although rare, concomitant femoral neck or intertrochanteric femur fractures can occur, and should be ruled out radiographically. Finally, pathologic or insufficiency fractures of the hip or acetabulum can occur in the absence of significant trauma. Complaints of groin or hip pain in an elderly patient in the face of essentially normal radiographs warrants a thorough diagnostic workup [36].
Fracture classification
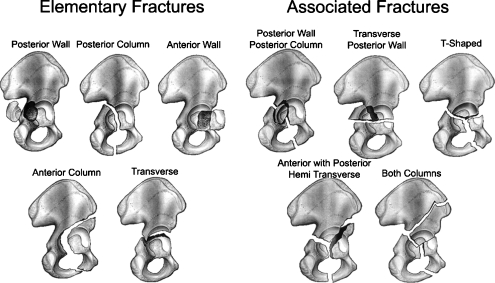
The standard classification used for acetabular fractures is the Judet and Letournel classification system. This classification system subdivides acetabular fractures into Elementary Fracture Types (posterior wall, posterior column, anterior wall, anterior column and transverse) and Associated Fracture Types (T-shaped, posterior column and wall, anterior wall or column with posterior hemitransverse, and both column) (Fig. 1) [10].
Fig. 1.
The Judet and Letournel acetabular fracture classification system
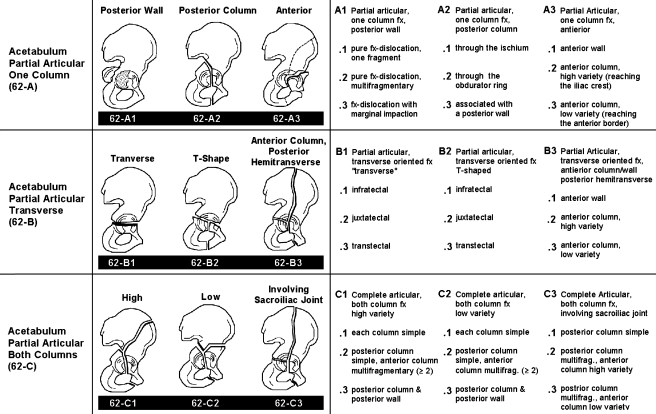
Subsequent to the pioneering work of Judet and Letournel, their classification was then used as the basis for formulating an alphanumeric computerized format and the Comprehensive Classification of Fractures of the Acetabulum was developed. This effort was spearheaded by SICOT International Documentation and Evaluation Committee and the AO/ASIF Foundation under the leadership of Maurice E. Muller. Each fracture is classified according to morphological characteristics, and subdivided into types, groups, and subgroups (Fig. 2). The system is especially beneficial for research database applications [10].
Fig. 2.
The Comprehensive Classification of Fractures of the Acetabulum developed by SICOT International Documentation and Evaluation Committee and the AO/ASIF Foundation under the leadership of Maurice E. Muller
Conservative management
Conservative management of acetabular fractures in the elderly is indicated only in the context of select fracture or patient characteristics. Fractures with no or minimal displacement out of traction can be expected to exhibit good outcomes with appropriate nonoperative management. Prolonged bed rest or skeletal traction in an effort to maintain a congruent reduction, however, is inappropriate—the reductions are often inadequate, and the morbidities associated with prolonged recumbency can be life-threatening [9]. Both column fractures (type C) exhibiting secondary congruence in the absence of traction have also been shown to do well with nonoperative management in the elderly. In spite of the resultant ilial malunion, hip function remains satisfactory when congruency is maintained [35]. Elderly patients exhibiting significant medical risk factors or limited preinjury functional capacities may also be best treated conservatively, despite the presence of operative indications. Should surgical risks outweigh potential benefits, benign neglect or delayed intervention will prove prudent.
Proper conservative management mandates effective pain control, functional physical therapy, deep venous thrombosis (DVT) prophylaxis, and frequent radiographic follow-up throughout the healing process to exclude late displacement. In select cases, such as those exhibiting severe underlying osteoporosis, metabolic workup and proactive treatment with healing protagonists may be indicated. If compliance and motor coordination are deemed sufficient, patients are allowed pivoting during transfers and toe-touch weight bearing on the effected extremity during walker-assisted weight bearing.
Any instability and/or incongruity conferred by fracture displacement will be poorly tolerated by the hip joint and represent contraindications to conservative management. Spencer [32] retrospectively reviewed the results of nonoperative treatment of 25 acetabular fractures in patients age 65–95 years. In 17 patients there was no initial gross displacement; nine were treated in traction for 6 weeks. Two patients died of their injuries. Of the survivors, 30% (7/23) demonstrated an unacceptable functional result, underscoring the need for frequent early follow-up and intervention in all but those cases with minimal displacement out of traction. Matta et al. [18] reported similar poor results in 33% (3/9) of elderly patients treated nonoperatively.
Acute ORIF
Acute ORIF is indicated for the majority of elderly patients sustaining displaced acetabular fractures [9, 24, 35]. Regardless of age, ORIF of acetabular fractures will consistently provide satisfactory results when:
An anatomic acetabular reduction with a congruent hip joint is achieved and maintained through healing.
The femoral head is preserved as a bearing surface.
Complications are avoided.
It is critical to select those patients at high risk for early failure and joint destruction. Should any of the above requirements be deemed unattainable due to underlying patient, injury, or treatment factors, an alternative to ORIF should be sought.
In all age groups, the best predictor of successful ORIF is the quality of reduction [16–18, 35]. In a recent metaanalysis [8] (comprising seven studies with 685 patients; all age groups), the reported incidence of posttraumatic arthritis following satisfactory reduction (≤2 mm) was 13.2%. If the reduction was not satisfactory (>2 mm), this increased to 43.5%. Factors effecting reduction quality include fracture type, fracture characteristics (comminution, impaction), time to surgery, and experience level of the operative team. Matta [17] reported the ability to anatomically reduce 96% of simple fractures, but only 64% of associated fractures, as classified by Letournel [15]. In his report on 424 acetabular fractures treated operatively, Mears et al. [22] reported the ability to anatomically reduce 87% of simple fractures, but only 59% of associated fractures. Beyond 2 weeks, anatomic reductions become progressively harder to obtain because of the presence of callus, organizing hematoma, and granulation tissue [35]. Mears et al. [22] noted that their anatomic reduction rate decreased significantly if surgery was delayed beyond 11 days. Letournel noted his ability to achieve an anatomic reduction after 3 weeks decreased to 62%. Finally, Matta et al. [18] demonstrated a direct correlation between the rate of anatomic reductions and the experience level of the operative surgeon, which again emphasizes the need for early transfer to specialty centers if outcomes are to be optimized. Unfortunately, in spite of anatomic reduction, significant posttraumatic arthritis will still develop in some joints. The likely mechanism, as recently demonstrated by Murray et al. [25], is an increased rate of chondrocyte apoptosis following intraarticular fractures.
Letournel and Judet's [16] published series reported 120 fractures in patients older than 60 years, of which 103 were treated with ORIF. When results were stratified by age, the best outcomes were noted in younger patients, with the poorest results occurring in patients over 50 years old. Although results progressively deteriorated with increasing age, of those available for follow-up 76% (44/58) demonstrated good to excellent clinical results. They therefore cautioned against abandoning ORIF as a treatment option in this age group. Matta [17] also noted progressively poorer results with increasing age, inactivity, and osteoporosis. However, when fracture reduction is controlled for in this series, the data indicate that it was the quality of reduction, and not the age of the patient, that impacted clinical outcome. Anatomic reduction was relatively more difficult to achieve in the older population. In patients younger than 60 years, anatomic reduction was achieved in 74% as compared to 44% in patients older than 60. When achieved, however, outcomes in the elderly were similar to their younger counterparts.
Helfet et al. [9] reported on the results of ORIF in 18 patients who were older than 60 years, of which 16 sustained complex fracture patterns. All were treated via a single approach (Kocher-Langenbeck or ilioinguinal) within 16 days of injury. A concentric reduction was achieved in 17 of 18, and the average Harris hip score was 90. Of the 17 patients available for follow-up, one progressed to THA because of posttraumatic arthritis and one suffered a partial loss of reduction because of noncompliance with physical therapy. This study clearly demonstrates that appropriately selected patients treated by an experienced surgeon can be expected to achieve good functional results (Fig. 3). An unpublished series evaluating 45 patients aged 55 years or older with an acetabular fracture treated with ORIF by Helfet and Virkus [11] again showed that in properly selected patients ORIF led to good outcomes, with a low complication rate (4–7%). Indications for ORIF were a fracture pattern amenable to fixation through a single nonextensile exposure without performing a trochanteric osteotomy or disrupting the abductor musculature, adequate bone quality for fixation, no femoral head injury, and a reasonable surgical time (3–4 h).
Fig. 3.
a An active 58 year-old male was struck by an automobile while bicycling. Anteroposterior (AP) and Judet radiographs revealed a left-sided comminuted both column acetabular fracture. No associated injuries were present and past history was significant only for previous aortic valve replacement. He was treated with ORIF via an ilioinguinal approach three days following the injury. EMG and SSEP monitoring were used during the procedure. b CT-scan images further delineate the fracture lines. c,d The patient was treated with ORIF via an ilioinguinal approach three days following the injury with EMG and SSEP used during the procedure. Intraoperative fluoroscopic images (c) illustrate an anatomic reduction and AP radiograph at 6 weeks (d) demonstrate maintenance of fixation. e Postoperative CT-scan images at 2 days following acetabular surgery demonstrating congruency and acceptable hardware placement. f AP and Judet views at 57 months following ORIF illustrate a healed acetabular fracture and an excellent radiographic result. The patient reported complete pain resolution and a return to participation in cross-country bicycling
In Matta's [17] series, the most significant prognostic indicator of a poor result was a fracture or impaction injury to the femoral head. Mears and Velyvis [21] noted difficulty in accurately determining the degree of damage sustained by the femoral head and acetabulum radiographically. Not infrequently in osteoporotic patients, a femoral head, which had appeared intact radiographically, is found to be significantly impacted at surgery. Predictors of a poor outcome in the Helfet study [11] were femoral head injury (fracture, impaction, AVN) or die-punch type acetabular impaction fracture. Anglen et al. [2] described the radiographic appearance of the acetabular impaction fracture at the medial roof as the “seagull sign.” In his series, this finding was 100% predictive of failure of reduction and/or fixation. Saterbak et al.'s [29] review of posterior wall fractures found that comminution and extended fracture patterns (into the subchondral roof arc) were statistically significant predictors of complete loss of joint space at 1 year.
Individuals who are at high risk for ORIF failure require an alternative treatment. Options include acute THA or delayed THA following either conservative or open fracture management. Although indications for each of these options continue to be defined, all share common goals, namely, avoidance of the morbidities associated with a protracted and difficult postoperative course, and avoidance of initial construct failure requiring subsequent additional major surgical intervention.
Delayed THA
Delayed THA following acetabular fracture is conducted as either a staged procedure following initial treatment, or as a salvage procedure in response to failed ORIF or progressive posttraumatic degenerative arthritis. Delayed THA following conservative management can be complicated by malunion or nonunion at the fracture site. Salvage THA following ORIF can be complicated by heterotopic ossification, proliferative scar formation, obstructive hardware, or occult infection [13, 38].
The results of late THA for posttraumatic arthritis have historically proven inferior to those for primary THA in the face of degenerative arthritis. This increased failure rate is attributable to the extent of bone stock loss and abnormal anatomy encountered after trauma, which makes it difficult to restore normal anatomy and biomechanics with a hip implant [30]. Although commonly presented as a shortcoming of delayed THA, such comparison is in fact a classic case of “comparing apples to oranges.” As noted by Bellabarba [5], complication rates and prevalence of radiolucencies associated with delayed THA following acetabular fracture more closely match those associated with THA revision surgery than those with primary THA. Clearly, the revision setting more closely resembles the postfracture THA setting, as both represent the second structural insult to the hip joint and share in common underlying deficiencies in acetabular bone stock and sclerosis in remaining bone [38].
Results of treatment for posttraumatic arthritis using cemented cups have been inconsistent. Boardman and Charnley [6] reported good to excellent results in the majority of their posttraumatic arthritis patients and recommended late cemented arthroplasty as an excellent treatment option in this population. Other studies, however, have documented poor results and high complication rates [27].
Romness and Lewallen [28] presented a retrospective review of delayed THA conducted at the Mayo clinic after acetabular fracture. Results were not stratified according to initial fracture treatment (ORIF and definitive traction). In the 26 patients older than 60 years included in this study, late acetabular loosening occurred in 38.5%. This represents a fivefold increase in late loosening rates when compared to cemented cups inserted for degenerative arthritis at the Mayo clinic by Stauffer [33]. No acetabular loosening, however, occurred in the five patients who were bone grafted (two prior to, and three concurrent with salvage THA), suggesting that restoration of bony anatomy after fracture may have benefits with regard to subsequent arthroplasty, even though it may fail to prevent posttraumatic degeneration.
Weber et al. [38] presented results of 63 delayed THA followed for a minimum of 2 years. All fractures were initially treated with ORIF. Acetabular components were cemented in 41 and uncemented in 22 subjects. Mean age at time of fracture was 43 years (range, 14–79). Mean age at time of arthroplasty was 52 years (range, 19–80). Within the cemented group, 15 (36.6%) of the acetabular components experienced mechanical failure, of which nine had undergone revision, at a mean follow-up of 14.9 years. Cemented acetabular component failure was strongly associated with the degree of deficiency of acetabular bone. Within the uncemented group, none of the acetabular components loosened or required revision at a mean follow-up of 4.6 years. Bone grafting was conducted in 15 patients, but outcomes were not analyzed according to this variable. The follow-up period was too short in the uncemented group to demonstrate significant differences between the two groups. Scarring from the previous procedure, retained hardware, heterotopic bone, and residual osseous deformity and deficiency increased the complexity of these cases as compared to primary THA. Although operative times were longer, and blood loss was greater, only one operative complication was encountered. Padgett et al. [26] recommended restoration of osseous anatomy at the time of ORIF and use of cementless cups as described for acetabular revison surgery.
Bellabarba [5] followed up 30 patients treated with delayed THA for an average of 63 months (range, 24–140). Average age at time of THA was 51 years (range, 26–86). Average time from acetabular fracture to THA was 37 months (range, 8–444). All injuries were a result of high-energy trauma. An uncemented modular hemispheric component was utilized and bone grafting performed as required [9] patients) to provide two-column support and to maintain the integrity of the dome and medial wall. Ninety percent (27/30) exhibited a good or excellent result at this intermediate term follow-up. These results were similar to those for primary THA conducted for degenerative arthritis. Results were also stratified according to initial acetabular fracture treatment (15 closed, 15 ORIF). Intraoperatively, the ORIF group required less bone grafting, but experienced approximately twice the intraoperative blood loss and longer OR times (45 min greater) than the closed group. The ORIF group did exhibit approximately double the rate of heterotopic ossification as compared to the closed group, but in none was it clinically significant. Otherwise, there was no significant difference between the two groups with respect to postoperative complications, radiographic stability of the acetabular component, or postoperative Harris hip scores.
Not one study can be applied to the elderly acetabular fracture with respect to the results of delayed THA. Quoted studies present patients treated over the course of the past four decades, during which significant advances in arthroplasty materials and techniques have significantly impacted outcomes. In addition, most studies do not stratify results according to age, injury energy level, or initial fracture treatment approach. In general, however, it does appear that:
Delayed THA after closed treatment or ORIF of an acetabular fracture can predictably provide satisfactory outcomes
Bone grafting to restore structural anatomy improves results.
Use of cemented cup fixation can only be advocated in exceptional cases.
Delayed THA following ORIF is a technically more demanding procedure than after closed treatment, but does seem to provide better bone stock.
Acute THA
Select acetabular fractures in the elderly have a predictably poor prognosis when treated either conservatively or with ORIF. Frequently, staged or acute THA is ultimately required. Although the role for acute THA remains somewhat controversial, this solution does provide the shortest overall recovery period for these injuries [1]. The rationale for acute THA in this setting is similar to that applied to femoral neck fractures, namely, early mobilization and avoidance of a subsequent surgical procedure [14]. To date, most literature regarding THA following acetabular fracture evaluates delayed THA versus acute THA. Conduct of acute THA, therefore, requires further evaluation and definition.
Predictors of poor outcomes in acetabular fractures at any age treated with ORIF have been identified by Mears and Velyvis [21] as follows: intraarticular comminution (10 or more fragments) with full-thickness abrasive loss of the articular cartilage of the femoral head; impaction of the femoral head; impaction of the acetabulum involving greater than 40% of the joint surface including the weight-bearing region; preexisting severe degenerative arthritis with a complete loss of articular cartilage and loss of hip joint congruity; displaced, comminuted fracture of the femoral head; or, completely displaced fracture of the femoral neck. An additional predictor for the elderly population was the degree of osteopenia, as determined by a review of the patient's history and radiographic findings. All 27 patients in Mears and Velyvis' [21] acute THA study with minor trauma had extensive impaction or comminution of the acetabulum, or substantial damage to the femoral head. Of these, 21 had a Singh index [31] consistent with marked osteoporosis of the hip.
Tidermark et al. [34] reported 10 patients, mean age 73 years (range, 57–87), treated acutely with a THA supported by a reinforcement ring (Burch–Schneider antiprotrusion cage) and autologous bone grafting of the acetabulum. No attempt was made to reduce the fractures. At a mean follow-up of 38 months (range, 11–84), good to excellent outcomes were achieved in 60% (6/10), bone graft was completely incorporated in all cases, and no evidence of loosening encountered. Early dislocations occurred in 30% of the subjects (3/10). Overall, there was an increased need for walking aids postoperatively. Migration of the cup was not reported. Both column fractures are not amenable to fixation with the reinforcement ring. The utility of this approach remains uncertain.
Mears and Velyvis [21] followed up 57 patients who underwent acute THA with minimal internal fixation for a mean of 8.1 years (range, 2–12 years). Mean age was 69 years (range, 26–89; 18 patients were younger than 60 years). Transverse and comminuted anterior column fractures with displacement of the quadrilateral surface were stabilized with two 2.0-mm braided cables [20]; both-column fractures received an additional percutaneous lag screw. Good to excellent outcomes were achieved in 79% (45/57). When the elderly were considered in isolation, functional outcomes were noted to decrease with increasing age, although results still appeared favorable. The adequacy of fixation, however, has been questioned [3]. The main concern when utilizing THA for an acute acetabular fracture is acetabular component fixation. At 6 weeks postoperatively, an average of 2 mm vertical and 3 mm medial displacement of the cups was noted with this technique, although long-term follow-up showed no clinical or radiographic evidence of loosening. However, with radiolucencies noted in 19%, osteolysis noted in 21%, and a mean of greater than 0.2 mm/year acetabular wear noted in 16%, the risk for revision surgery is not negligible [3]. Moushine et al. [24] followed up 18 patients, mean age of 76 years (range, 65–93), who were also treated with the cable fixation and acute THA for acetabular fracture, for a mean period of 36 months (range, 12–46). Good results were achieved in 17 of 18 patients. All had evidence of fracture healing, although similar early migration occurred in 87% during the first 3 months. No radiographic evidence of loosening was encountered during this short-term follow-up.
Beaule et al. [4] reported on 10 consecutive acetabular fractures treated with rigid internal fixation and acute THA via the Levine anterior approach. At a mean follow-up of 36 months (range, 24–53), all fractures united, and all acetabular components remained fixed with no evidence of migration or loosening. They recommended rigid internal fixation in accordance with the principles of Letournel, via a single incision. The Kocher-Langenbeck approach is utilized for posterior lesions, and the Levine anterior approach for anterior lesions. Rather than approaching THA as an alternative treatment for this select group of difficult fractures, this management philosophy considers acute THA as an adjunct to the continuum of ORIF management currently provided for all acetabular fractures. Properly conducted ORIF for any acetabular fracture will simultaneously stabilize the acetabular columns, and anatomically reconstruct the articular surface. Although articular reconstruction may be in the form of THA in these select cases, this does not preclude the requirement for concurrent column stabilization.
The significance of early migration in this setting is unclear. There is concern that early migration encountered with the cabling technique is indicative of inadequate fixation. Although no tendency for nonunion has been demonstrated in several published series [21, 24], the long-term effect on acetabular component longevity has yet to be determined. In a relatively large series by Mears and Velyvis [21], no evidence of loosening was found. Rigid internal fixation clearly provides the most stable construct early. With increasing age or medical comorbidities, minimal fixation may prove advantageous, as operative morbidity is lessened. The minimal functional demands and shortened life expectancy in this population makes the likelihood of revision low. In the younger, more active part of the population, rigid internal fixation may be the better choice. Familiarity and experience with this tactic provides predictably solid fixation, and the lack of early migration predicts acetabular component longevity. Regardless of the fixation method chosen, these are technically demanding cases, which should be managed by surgical teams familiar with both acetabular reconstruction and arthroplasty techniques.
Hospital for Special Surgery treatment regimen
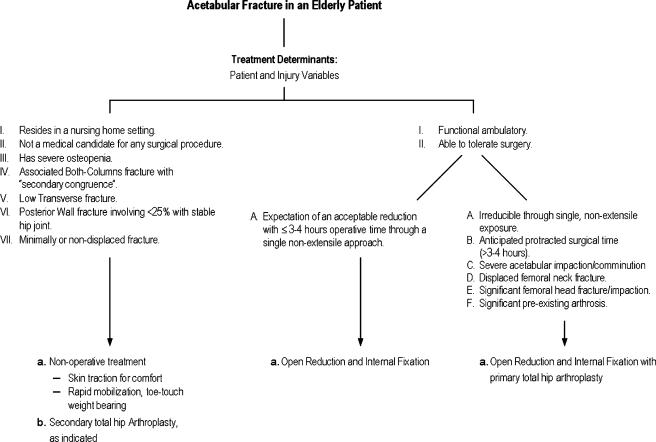
Elderly patients with acute acetabular fractures presenting to the Orthopedic Trauma Service at Hospital for Special Surgery (HSS) are treated according to the following recommendations [37] (Fig. 4) [35].
Acute ORIF with an acceptable reduction of the acetabulum and restoration of joint congruity through a single anterior or posterior approach if no femoral head injury and the patient is a candidate for surgery.
Acute ORIF with THA if femoral head injury or reduction not attainable. The acetabular columns are reduced and stabilized with rigid internal fixation prior to insertion of the acetabular component. (Other acute THA techniques have been used at our institution with good early results [7].)
Delayed THA if not a surgical candidate acutely, or salvage THA if ORIF failure.
Fig. 4.
Treatment algorithm for acetabular fractures in the elderly
Should the patient meet the criteria predictive of successful ORIF, they are enrolled in a standard treatment protocol, applied to all adult acetabular fractures.
Initially, the patient is evaluated in accordance with advanced trauma life support (ATLS) principles, to include complete primary and secondary surveys. Emergent surgical indications are ruled out during this stage. A–P pelvis radiographs obtained during this stage initially identify the acetabular injury. Complete medical, surgical, and social histories are obtained with emphasis regarding those factors, which could affect the hospital course, surgical intervention, or ability to fully participate in rehabilitation. These include premorbid ambulatory status, occupation, living conditions, use of tobacco, alcohol or illicit drugs, history of DVT, bleeding disorders, allergies, underlying DJD, chronic medications that may have deleterious effects on bone healing, and history of previous irradiation to the pelvis.
Further radiographic imaging is directed by the orthopedic physical exam in an effort to identify any associated injuries. The pelvis is further evaluated with Judet views and CT of the pelvis with 2 mm cuts. These studies allow complete elucidation of the fracture pattern, and are critical for initial management decisions (operative vs. nonoperative; ORIF vs. THA). Fracture classification as described by Letournel [15] is useful for selecting the appropriate operative approach and for planning fracture reductions. Any evidence of continued cartilage impaction or instability requires application of skeletal traction to avoid abrasive erosion or vascular compromise to the femoral head.
A comprehensive medical evaluation is mandatory. This ensures medical optimization prior to operative intervention, and provides operative risk assessment. This includes, as indicated, a standard laboratory battery (complete blood count, chemistry panel, coag's, urinalysis, urine culture), cardiac evaluation (12-lead EKG, cardiac enzymes, echocardiogram), pulmonary evaluation (chest x-ray, pulmonary function testing with spirometry), renal function tests, hepatic evaluation and carotid Doppler ultrasound. Neurologic deficits are confirmed and followed through the postoperative period by the neurology service. Early social work intervention is initiated for postoperative planning, placement, and prepositioning of home health care services.
Preoperatively, adequate pain management and DVT prophylaxis (pneumatic compression boots and pharmacologic intervention if not contraindicated) are provided. Foley catheters are commonly placed for patient comfort, but are removed at least 24 h prior to surgery in an effort to minimize infection. Magnetic resonance venography (MRV) is conducted one day before surgery to rule out DVT. MRV is advantageous over duplex ultrasound as a screening tool because of its ability to accurately image pelvic thrombi [23]. Inferior vena cava (IVC) filters are placed preoperatively in patients with demonstrated DVT or those considered at high risk (past history of DVT). Two to four units of PRBC are typed and crossed for use in the main operating room. Fresh frozen plasma (FFP) should be available in cases with underlying coagulopathy or hepatic dysfunction.
In the main operating room, positioning is dependent upon the operative approach. Foley catheters are placed in all patients. Care is taken to pad all bony prominences and to properly place axillary rolls in case of lateral decubitus positioning. In most cases, epidural anesthesia is provided by the anesthesia team. Antibiotics (a cephalosporin, unless contraindicated) are provided approximately 30 min before initial skin incision. EMG and SSEP monitoring is conducted throughout the procedure. Hypotensive anesthesia and careful hemostasis minimize blood loss. A cell saver is utilized in all cases, and blood is returned to the patient whenever sufficient quantities are obtained. PRBC are provided as indicated.
Surgical approaches, as well as reduction and fixation techniques are dependent upon the fracture type, and are well described elsewhere [35]. In all cases, however, effort is taken to ensure anatomic reduction of the articular surface. When accessible, the joint is debrided and femoral head inspected for evidence of articular damage. Intraoperative radiographic verification of reduction quality and hardware positioning is conducted prior to closure. Atraumatic handling of soft tissues and wound closure over hemovac drains minimizes postoperative wound complications.
Postoperatively, elderly patients are commonly maintained in the PACU or ICU overnight to ensure an adequate level of care. Initial PCA (patient-controlled analgesia) pain control is managed by the Pain Service; DVT prophylaxis (typically a Coumadin pathway and pneumatic compression boots) is initiated; antibiotics are continued for 48 h, or until drains are discontinued; and heterotopic ossification prophylaxis initiated in case of an extensile approach and absence of contraindications. Posterior hip precautions are maintained for 6 weeks in case of a Kocher‐Langenbeck approach. Drains are continued until output is minimal and the patient has mobilized. Physical therapy is initiated early with emphasis on transfers, walker-assisted ambulation with toe-touch weight bearing and pivoting on the effected extremity, range of motion at the hip, and quadriceps strengthening. Medical management remains critical throughout this period. Postoperative CT of the acetabulum is obtained before discharge to quantify the quality of reduction.
During the subacute recovery phase, patients are most commonly transferred to rehabilitation facilities with continued supervised physical therapy. Initial clinic follow-ups occur at 2 weeks for wound check, and at 6 weeks for functional and radiographic evaluation. Metabolic workup and treatment for future fracture prevention are indicated for patients with low-energy mechanisms or other evidence of significant osteoporosis. In Mears and Velyvis' series [21], of the 27 patients who sustained acetabular fractures from simple falls, 19 had a history of a previous fracture provoked by minor trauma and 5 had a prior hip fracture, highlighting fracture prevention as an intervention requiring improvement.
Conclusion
Elderly patients presenting with acetabular fractures display a high degree of diversity. Fracture treatment must therefore be highly individualized. Proper initial management choices are critical, as early construct failure resulting in a protracted postoperative course and subsequent salvage surgery can be accompanied by significant morbidity. ORIF is indicated for most acetabular fractures in the elderly. Clinical and radiographic results after ORIF closely follow the quality of the articular reduction and the ability to maintain a congruent reduction of the hip joint. Fracture characteristics predictive of anatomic articular reduction should be treated by ORIF. Fracture characteristics predictive of early posttraumatic arthritis following ORIF should be treated with simultaneous ORIF and THA.
Footnotes
The views expressed in this article are those of the author and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the U.S. Government.
References
- 1.An YH (2002) Internal fixation in osteoporotic bone. Thieme, New York
- 2.Anglen JO, Burd TA, Hendricks KJ, Harrison P (2003) The “Gull Sign”: a harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma 17:625–634, Oct [DOI] [PubMed]
- 3.Beaule PE (2002) Open reduction and internal fixation versus total hip arthroplasty for the treatment of acute displaced acetabular fractures. J Bone Jt Surg Am 84-A:2103–2104, Nov [DOI] [PubMed]
- 4.Beaule PE, Griffin DB, Matta JM (2004) The Levine anterior approach for total hip replacement as the treatment for an acute acetabular fracture. J Orthop Trauma 18:623–629, Oct [DOI] [PubMed]
- 5.Bellabarba C, Berger RA, Bentley CD, Quigley LR, Jacobs JJ, Rosenberg AG, Sheinkop MB, Galante JO (2001) Cementless acetabular reconstruction after acetabular fracture. J Bone Jt Surg Am 83-A:868–876, Jun [DOI] [PubMed]
- 6.Boardman KP, Charnley J (1978) Low friction arthroplasty after fracture dislocations of the hip. J. Bone Jt Surg 60(B):495–497 [DOI] [PubMed]
- 7.Cornell CN (2005) Management of acetabular fractures in the elderly patient. HSS J 1:25–30 [DOI] [PMC free article] [PubMed]
- 8.Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H (2005) Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Jt Surg Br 87:2–9, Jan [PubMed]
- 9.Helfet DL, Borrelli J, Di Pasquale T, Sanders R (1992) Stabilization of acetabular fractures in elderly patients. J Bone Jt Surg Am 74:753–765, Jun [PubMed]
- 10.Helfet DL, Shonnard P (1996) Mini-symposium: Acetabular fractures (I) classification. Curr Orthop 10:69–73 [DOI]
- 11.Helfet DL, Virkus W (2002) Acetabular fractures in the elderly. unpublished data
- 12.Holbrook TL, Grazier K, Kelsey JL, Stauffer RN (1984) The frequency of occurrence, impact, and cost of selected musculoskeletal conditions in the United States. American Academy of Orthopedic Surgeons, Chicago
- 13.Jimenez ML, Tile M, Schenk RS (1997) Total hip replacement after acetabular fracture. Orthop Clin North Am 28:435–446 [DOI] [PubMed]
- 14.Johansson T, Jacobsson SA, Ivarsson I, Knutsson A, Wahlstrom O (2000) Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthop Scand 71:597–602, Dec [DOI] [PubMed]
- 15.Letournel E (1980) Acetabulum fractures: classification and management. Clin Orthop 151:81–106 [PubMed]
- 16.Letournel E, Judet R (1993) Fractures of the acetabulum, 2nd edn. Springer-Verlag, Berlin
- 17.Matta JM (1996) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks of the injury. J Bone Jt Surg 78(A):1632–1645 [PubMed]
- 18.Matta JM, Anderson LM, Epstein HC, Hendricks P (1986) Fractures of the acetabulum: a retrospective analysis. Clin Orthop 205:241–250 [PubMed]
- 19.Mears DC (1999) Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg 7:128–141, Mar–Apr [DOI] [PubMed]
- 20.Mears DC, Shirahama M (1998) Stabilization of an acetabular fracture with cables for acute total hip arthroplasty. J Arthroplasty 13:104–107, Jan [DOI] [PubMed]
- 21.Mears DC, Velyvis JH (2002) Acute total hip arthroplasty for selected displaced acetabular fractures: two to twelve-year results. J Bone Jt Surg Am 84-A:1–9, Jan [DOI] [PubMed]
- 22.Mears DC, Velyvis JH, Chang CP (2003) Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop 173–186, Feb [DOI] [PubMed]
- 23.Montgomery KD, Potter HG, Helfet DL (1995) Magnetic resonance venography to evaluate the deep venous system of the pelvis in patients who have an acetabular fracture. J Bone Jt Surg Am 77:1639–1649, Nov [DOI] [PubMed]
- 24.Mouhsine E, Garofalo R, Borens O, Blanc CH, Wettstein M, Leyvraz PF (2004) Cable fixation and early total hip arthroplasty in the treatment of acetabular fractures in elderly patients. J Arthroplasty 19:344–348, Apr [DOI] [PubMed]
- 25.Murray MM, Zurakowski D, Vrahas MS (2004) The death of articular chondrocytes after intra-articular fracture in humans. J Trauma 56:128–131, Jan [DOI] [PubMed]
- 26.Padgett DE, Kull L, Rosenberg A (1993) Revision of the acetabular component without cement after total hip arthroplasty. J Bone Jt Surg 75:663–673 [DOI] [PubMed]
- 27.Rogan IM, Weber FA, Solomon L (1979) Total hip replacement following fracture dislocation of the acetabulum. J Bone Jt Surg 61:252
- 28.Romness DW, Lewallen DG (1990) Total hip arthroplasty after fracture of the acetabulum. J Bone Jt Surg 72-B:761–764 [DOI] [PubMed]
- 29.Saterbak AM, Marsh JL, Nepola JV, Brandser EA, Turbett T (2000) Clinical failure after posterior wall acetabular fractures: the influence of initial fracture patterns. J Orthop Trauma 14:230–237, May [DOI] [PubMed]
- 30.Schreurs BW, Zengerink M, Welten ML, van Kampen A, Slooff TJ (2005) Bone impaction grafting and a cemented cup after acetabular fracture at 3–18 years. Clin Orthop Relat Res 145–151, Aug [DOI] [PubMed]
- 31.Singh M, Nagrath AR, Maini PS, Haryana R (1970) Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Jt Surg 52(A):457–467 [PubMed]
- 32.Spencer RF (1989) Acetabular fractures in older patients. J Bone Jt Surg [Br] 71B:774–776 [DOI] [PubMed]
- 33.Stauffer RN (1982) Ten-year follow-up study of total hip replacement with particular reference to roentgenographic loosening of the components. J Bone Jt Surg 64:983–990 [PubMed]
- 34.Tidermark J, Blomfeldt R, Ponzer S, Soderqvist A, Tornkvist H (2003) Primary total hip arthroplasty with a Burch–Schneider antiprotrusion cage and autologous bone grafting for acetabular fractures in elderly patients. J Orthop Trauma 17:193–197, Mar [DOI] [PubMed]
- 35.Tile M, Helfet DL, Kellam JF (2003) Fractures of the pelvis and acetabulum, 3rd edn. Lippincott, Philadelphia
- 36.Tornkvist H, Schatzker J (1993) Acetabular fractures in the elderly: an easily missed diagnosis. J Orthop Trauma 7:233–235 [DOI] [PubMed]
- 37.Toro JB, Hierholzer C, Helfet DL (2004) Acetabular fractures in the elderly. Bull Hosp Jt Dis 62:53–57 [PubMed]
- 38.Weber M, Berry DJ, Harmsen WS (1998) Total hip arthroplasty after operative treatment of an acetabular fracture. J Bone Jt Surg Am 80:1295–1305, Sep [DOI] [PubMed]