Purpose
We describe a case of ultrasound-guided needle localization of an osteoid osteoma of the wrist.
Introduction
Osteoid osteomas are benign small (typically less than 1.5 cm) osteoid-forming tumors accounting for 10–12% of all primary bone tumors. The most common sites are in the appendicular skeleton, but osteoid osteomas can occur in any bone. Classically, these tumors appear as a small sclerotic lesion with a circular lucent defect, the nidus. The nidus represents “osteoid and interconnected bone superimposed on highly vascularized connective tissue” [1, 2].
Treatment most commonly consists of medical management with nonsteroidal anti-inflammatory drugs (NSAIDs), surgical excision, and/or radiofrequency ablation. Fast scanning now made possible with multidetector computed tomography (CT) has resulted in CT-guided drilling (curettage or burr) and CT-guided percutaneous resection. More recently, there has been increased use of radiofrequency ablation of osteoid osteoma utilizing percutaneous guidance with CT [3–6].
This paper illustrates a case of an osteoid osteoma of the wrist, which was treated with surgical excision and radiofrequency ablation after needle localization under ultrasound guidance.
Case report
A 14-year-old male with no significant medical history presented with a 4-month history of worsening right wrist pain. The patient reported no history of trauma or other inciting event. His pain was present both at night and during the day and was relieved with a regimen of ibuprofen 400 mg three times daily.
Consultation was obtained at an outside institution, a magnetic resonance imaging (MRI) study of the wrist was obtained, and the patient was treated for presumptive diagnosis of avascular necrosis of the capitate. The patient continued to experience pain in the center and dorsum of the right wrist despite casting, splinting, and bone stimulator therapy for 52 days.
On exam, the patient had a moderate amount of swelling over the dorsum of the wrist, particularly over the midcarpal joint. His pain was exquisite to palpation over the dorsum of the capitate. Patient could not tolerate a midcarpal shift test, and translation of the wrist was difficult because of pain. He also demonstrated a loss of 30° of flexion and extension secondary to pain at both extremes. The patient's entire right upper extremity was neurologically intact.
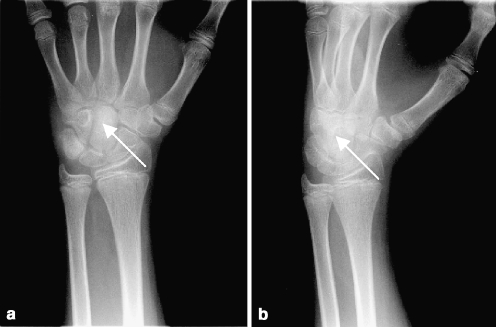
Plain radiographs were obtained (Fig. 1) and demonstrated a small lucency surrounded by diffuse sclerosis of the distal pole of the capitate. Mild soft tissue swelling over the dorsum of the right wrist was also noted.
Fig 1.
Plain radiographs demonstrate a small lucency (arrow) surrounded by diffuse sclerosis of the distal pole of the capitate
Magnetic resonance imaging demonstrated a 6-mm, low-signal lesion in the capitate surrounded by high signal reflecting a bone marrow edema pattern. A joint effusion and extensive synovitis was noted in the dorsal midcarpal row (Fig. 2).
Fig 2.
Coronal IR (a), and axial T1 with fat suppression (b), MRI through the wrist demonstrate a low–signal nidus in the capitate surrounded by high signal reflecting a bone marrow edema pattern
A presumptive diagnosis of osteoid osteoma was made, and the patient was scheduled for a combined surgical excision and radiofrequency ablation of the lesion. To obtain a minimally invasive approach, needle localization of the nidus was requested using ultrasound.
Ultrasound technique
Scans were performed using an intermediate frequency linear transducer with the scan plane corresponding to the anatomic axial plane. Grayscale sonography demonstrated hypoechoic tissue corresponding to inflammatory soft tissue edema. Power Doppler interrogation demonstrated hyperemia (Fig. 3).
Fig 3.
Ultrasound demonstrates an area of focal cortical irregularity in the midportion of the dorsoradial aspect of the capitate (arrow) surrounded by hypoechoic soft tissue edema and hyperemia on Doppler
Preoperatively, the lesion was localized by ultrasound (Fig. 4). The tip of a 22-gauge needle was placed at the edge of the lesion, which appeared on ultrasound as an area of focal cortical irregularity in the midportion of the dorsoradial aspect of the capitate.
Fig 4.
The tip of a 22-gauge needle was placed at the edge of the lesion preoperatively by ultrasound guidance
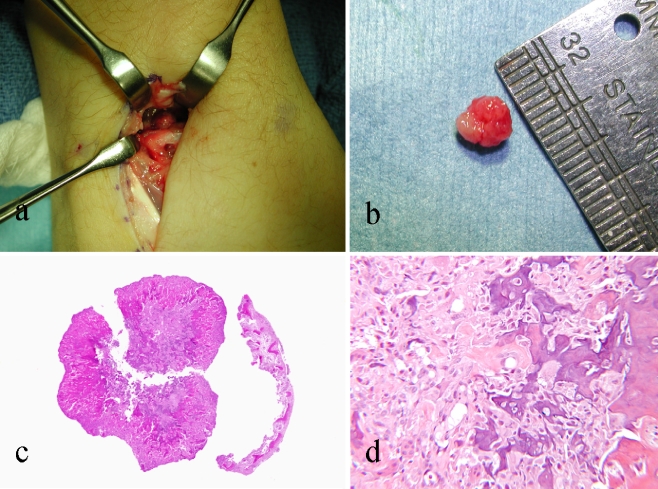
The patient was taken to operating room where a 2-cm incision was made over the dorsal aspect of the wrist in the interval between the extensor digitorum communis and the extensor carpi radialis brevis. A 5-mm hard, cherry red mass was excised and sent to pathology (Fig. 5).
Fig 5.
(a) Intra-operative photograph showing mass on dorsal aspect of right wrist in interval between extensor digitorum comminus and extensor carpi radialis brevis. (b) Small, round, cherry-red mass immediately after excision. (c) Low-power photomicrograph (stain, hematoxylin and eosin, magnification X 40) demonstrating central nidus separated from dense, surrounding bone. (d) Medium-power photomicrograph (stain, hematoxylin and eosin, magnification X 100) illustrating interconnecting seams of osteoid, osteoblasts, and osteoclasts surrounded by loose, fibrovascular stroma.
Radiofrequency ablation was subsequently performed utilizing a 22-gauge, 5-cm probe. The tip of the probe was placed into the surgical bed postexcision. Ablation was performed at 90°C for a total of 6 min.
Histological analysis confirmed the diagnosis of osteoid osteoma (Fig. 5).
At 6-week follow-up, the patient's symptoms had nearly completely resolved with only a slight discomfort with wrist flexion. He returned to activities without a splint.
Discussion
Osteoid osteomas may be cortical, cancellous, or subperiosteal. Cortical osteomas are the most common and result in a dense sclerosis surrounding the lucent nidus. Cancellous osteoid osteomas occur most commonly in the juxta-articular portion of the femoral neck, the posterior elements of the spine, and in the small bones of the hand and feet [1–5]. Subperiosteal osteoid osteoma, the most uncommon, is usually without reactive changes and involves the juxta- or intra-articular regions of the medial aspect of the femoral neck and the hands and feet.
Classically, osteoid osteomas are found in young people, more commonly males, and present with an insidious onset of a dull aching pain worse at night and relieved by NSAIDs. The mean time from the onset of symptoms to diagnosis is 15 months [1].
Radiographic, CT, and the MRI appearance of osteoid osteomas are well known. There has been a limited role for ultrasound in the diagnosis of osteoid osteoma. Likely explanations include the limited number of sonographers who are comfortable with imaging the musculoskeletal system and the fact that other imaging modalities have reliably imaged the most common osteoid osteomas [9]. Traditional modalities are usually diagnostic and most often demonstrate the classic appearance of a central lucent nidus surrounded by reactive sclerosis. Depending on the location, however, osteoid osteoma may have a different appearance. For example, intra-articular osteomas are characterized by little or no reactive sclerosis and are accordingly radiographically occult and not diagnosed for months or years. Performing CT and MRI on all patients would be costly. Ultrasound provides a less expensive, quick, and noninvasive option. A study of three patients performed by Ebrahim et al. [9] in 2001 demonstrated the utility of ultrasonography in alerting clinicians to the possibility of an occult osteoma.
In this case, the nidus produced a focal contour deformity along the dorsal aspect of the capitellum, surrounded by hyperemic inflammatory tissue. This is in concordance with its appearance during surgical excision.
Osteoid osteomas of the capitate, although rare, are well documented [7, 8]. Prior studies have demonstrated radiographic and MRI correlation of osteoid osteomas of the capitate. To our knowledge, correlation of conventional radiology, MRI, and ultrasonography for osteoid osteomas of the wrist has not appeared in the literature. We further demonstrate the novel use of preoperative needle localization of an osteoid osteoma of the capitate utilizing sonographic guidance.
Percutaneous needle localization prior to excision permits the surgeon to limit the incision and reduce the risk of injury to the many small ligaments and tendons in the wrist.
References
- 1.Athanasian EA (1993) Principles of diagnosis and management of musculoskeletal tumors. In: Green DP, Hotchkiss RN (eds) Green's Operative Hand Surgery. 3rd edn. Churchill Livingstone, New York, NY, pp 2206–2295
- 2.Picci P, Mirra JM (1989) Osteoid osteoma. In: Mirra JM, Picci P, Gold RH (eds) Bone Tumors: Clinical, Radiologic, and Pathologic Correlations. Lea & Febiger, Philadelphia, pp 226–248
- 3.Dupuy DE, Zagoria RJ, Akerley W, Mayo-Smith WW, Kavanagh PV, Safran H (2000) Percutaneous radiofrequency ablation of malignancies in the lung. Am J Roentgenol 174:57–59 [DOI] [PubMed]
- 4.Goldberg SN, Dupuy DE (2001) Image-guided radiofrequency tumor ablation: challenges and opportunities—part I. J Vasc Interv Radiol 12:1021–1032 [DOI] [PubMed]
- 5.Weber KL (2004) What's new in musculoskeletal oncology. J Bone Jt Surg Am 86:1104–1109 [DOI] [PubMed]
- 6.Woertler K, Vestring T, Boettner F, Winkelmann W, Heindel W, Lindner N (2001) Osteoid osteoma: CT-guided percutaneous radiofrequency ablation and follow-up in 47 patients. J Vasc Interv Radiol 12(6):717–722, Jun [DOI] [PubMed]
- 7.Jensen EG (1979) Osteoid osteoma of the capitate bone. Hand 11(1):102–105, Feb [DOI] [PubMed]
- 8.Ambrosia JM, Wold LE, Amadio PC (1987) Osteoid osteoma of the hand and wrist. J Hand Surg (Am) 12(5 Pt 1):794–800, Sep [DOI] [PubMed]
- 9.Ebrahim FS, Jacobson JA, Lin J, Housner JA, Hayes CW, Resnick D (2001) Intraarticular osteoid osteoma: sonographic findings in three patients with radiographic, CT, and MR imaging correlation. Am J Roentgenol 177(6):1391–1395, Dec [DOI] [PubMed]