Abstract
This study investigates the relationship between intraoperative extreme flexion and tibia-femoral dislocation during total knee arthroplasty on the prevalence of postoperative deep venous thrombosis. Knees were randomized into two groups. The control group underwent the procedure according to normal protocol, which kept the knee in extreme flexion and maintained dislocation for the duration of the exposure, whereas the variable group underwent the procedure modified to minimize the total amount of time the knee was hyperflexed and dislocated. Venograms were positive in 42% (39/92) of the control knees and 38% (30/79) of the modified group (p = 0.6). Proximal deep venous thrombosis were found in 12% (11/92) of the control knees and in 16% (13/79) of the modified knees (p = 0.4). No statistical difference could be detected between the two techniques in regards to the incidence of deep venous thrombosis.
Key words: total knee arthroplasty, deep venous thrombosis, flexion, tibial femoral dislocation, venography
Introduction
The benefits from total knee arthroplasty are well documented in the literature; patients achieve restored ambulation through the restitution of a painless and functional knee joint. Total knee arthroplasty, however, is associated with several risks, including the development of deep venous thrombosis [1–13, 13–54]. Deep venous thrombi commonly occur in the calf after total knee arthroplasties and are more frequent after bilateral total knee arthroplasties than unilateral total knee arthroplasties [27, 47]. Thrombi in the calf vein often propagate proximally into the popliteal and femoral veins, increasing the risk of developing fatal pulmonary emboli [5, 9, 15, 29, 52, 53]. Therefore, deep venous thrombosis formation is a potentially serious risk factor in total knee arthroplasty.
Without prophylaxis, the incidence of deep venous thrombi following total knee arthroplasty has been reported at rates up to 88% [27, 53]. Up to 28% of such thrombi may further propagate to proximal veins [2, 9, 26, 35, 36, 50–53]. Venography and Doppler ultrasound are commonly used to detect thromboemboli; however, these imaging techniques are fallible and often unreliable [55, 61]. Common forms of prophylaxis include aspirin, warfarin, low molecular weight heparins, and mechanical pneumatic compression devices [1–8, 10–27, 29–54]. These modalities are also inconsistent; patients periodically develop deep venous thrombosis despite a careful prophylaxis regimen. Clearly, prevention of deep venous thrombi remains the safest course of action to remove the risk of pulmonary emboli.
As described by Virchow in 1856, three factors contribute to deep venous thrombosis formation: hypercoagulability, endothelial injury, and venous stasis. All three factors are initiated during total knee arthroplasty. Extreme flexion and dislocation of the knee during total knee arthroplasty may play a significant role in the development of deep venous thrombosis formation by theoretically causing direct trauma to the popliteal vasculature and increasing platelet adhesion in accordance with Virchow's triad. The surgeon uses both dislocation and extreme flexion to expose the knee, to perform osteotomies, and to insert the prosthesis; the dislocation and flexion are controlled and maintained throughout the duration of the arthroplasty. This study was conducted to investigate whether a reduction in the total amount of time the knee was dislocated and hyperflexed led to a decrease in deep venous thrombosis. The relationship between venous thrombosis and the extreme flexion and dislocation utilized during total knee arthroplasty has not yet been documented.
Methods
One hundred seventy-one total knee arthroplasties in 118 patients were randomized into two groups. All procedures were performed by the senior author. The average age of the patient population was 68.1 years (range 40–84 years; standard deviation 8.7 years). There were 122 knees in 83 female patients with an average age of 68.6 years (range 40–84 years; standard deviation 8.9 years) and 49 knees in 35 male patients with an average age of 66.8 years (range 46–81 years; standard deviation 7.8 years). The control or “nonmodified” group underwent the procedure according to normal protocol, which maintained the dislocation and flexion throughout the arthroplasty, whereas the variable or “modified” group underwent the procedure modified to minimize the total amount of time the knee was in extreme flexion. Intraoperative extreme flexion was defined as greater than 135° of flexion, whereas tibia-femoral dislocation was defined as 100% anterior translation of the tibia with respect to the femur. Limits were set at 4 min for the flexion and 2 min for the dislocation in the modified procedure.
One hundred eighteen consecutive patients undergoing primary total knee arthroplasty were divided into two groups using random numbers. Because of the patient randomization process, the patient population undergoing simultaneous bilateral total knee arthroplasties often had one knee assigned to the modified arm of the study and the other knee to the control arm; thus, these patients served as their own control group. Listing the number of patients in each group would have resulted in redundancy, and thus, much of the data are presented in terms of the number of knees in each group. Appropriate recognition was given to patients who underwent bilateral procedures to allow for the variable rates of deep venous thrombosis in unilateral versus bilateral total knee arthroplasty. We excluded patients with a history of previous thromboembolism, patients undergoing revision arthroplasty, and patients taking coumadin preoperatively for other medical reasons. The nonmodified group had 92 knees in 63 patients, whereas the modified group included 79 knees in 55 patients.
The following exceptions were noted. Two bilateral total knee arthroplasty patients refused to have venography performed bilaterally. The data derived from venography of each of the patients' one leg was included among the bilateral patient population. Two patients underwent staged bilateral total knee arthroplasties that occurred at a 12- and 14-day interval, respectively. These patients, totaling four knees, were included among the unilateral patient population; they served as their own control.
All patients received epidural anesthesia. Both groups of patients had a tourniquet pressurized to 350 mm Hg after the leg had been exsanguinated. A midline skin incision and a deep medial parapatellar approach were used to expose the knee. All patients had either an Insall-Burnstein II or Johnson & Johnson posterior stabilized cemented arthroplasty. Patellar preparation was performed on all patients.
The nonmodified protocol was performed with the knee in extreme flexion for the duration of the exposure as in a standard knee replacement, i.e., extended only after the trial components were inserted and the patella to be cut. The knee joint was dislocated, and osteotomies of the tibia, femur, and patella were performed. The components were then cemented and followed by closure.
The total knee arthroplasty protocol for the modified group was based on a technique described by Rabinov and Paulin (1972) and is discussed as follows. The knee was extended during preparation of the femoral and tibial sides not to allow the knee to be in the flexed state for more than 4 min. The knee was then placed into extreme flexion, after which the tibia was translated 100% anterior to the femur to perform the tibial osteotomy. The positioning and tibial osteotomy were timed by the anesthesiologist to be no longer than 4 min. The knee was then immediately placed in extension for patellar preparation. For the femoral osteotomy, the knee was positioned in no greater than 90° of flexion for a period of less than 4 min. When the 4-min interval was reached, the leg was immediately placed into extension for a period of 2 min. After 2 min of extension, the knee was reflexed to 90°, again for a time period of no longer than 4 min. During cementation of the tibial component, the knee was maintained in extreme flexion and tibia-femoral dislocation, which was also timed and limited to less than 4 min.
Postoperatively, all patients were placed on 325 mg of aspirin twice a day for deep vein thrombosis prophylaxis. Venography was performed from 2 to 17 days postoperatively, averaging 5.7 days. Because venography has been the gold standard at our institution and was used routinely until we switched to ultrasonography, we assume that the sensitivity, specificity, and accuracy approach 100%. One patient underwent staged, bilateral knee replacements (12 days apart), but venography was performed bilaterally on 17 days after the first knee and 7 days after the second knee.
Thrombi were classified according to their location. The popliteal, femoral, and iliac thrombi were considered as evidence of proximal deep vein thrombosis. If a venogram in the calf was positive, the patient was placed on warfarin for 6 weeks. Patients with positive proximal venograms were treated by an initial prescription of heparin followed by placing the patient on warfarin to maintain an international normalized ratio between 1.3 and 2.0. The drains were removed 24 h after the operation. All patients received continuous passive motion beginning on postoperative day 1.
For statistical analysis, a chi-squared test was performed to evaluate the significance of the incidence of deep vein thrombosis.
Results
The two groups were evaluated in terms of age, gender, percentage of unilateral and bilateral knees, and the arthritic nature of their disease. The patients were found to be relatively similar in regards to each basis. The average tourniquet time for the whole patient population was 56 min. The average tourniquet time was 52.7 min for the modified group and 59.3 min for the nonmodified group (p > 0.05). The modified knees spent an average of 7.9 min in extreme flexion with tibia-femoral dislocation, whereas the nonmodified knees spent an average of 34 min in extreme flexion with tibia-femoral dislocation.
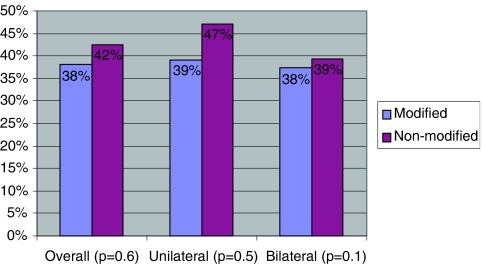
The modified group included 79 total knee arthroplasties (55 patients), whereas the nonmodified group included 92 total knee arthroplasties (63 patients). Thrombi were found in 38% (30/79) of the modified group and 42% (39/92) of the nonmodified group (p = 0.6; Fig. 1 and Table 1). The incidence of proximal deep venous thrombosis was 16% (13/79) in the modified group and 13% (11/92) in the nonmodified group (p = 0.4).
Fig 1.
Number of knees developing deep venous thrombosis in percentages by study groups. Total number of modified knees = 79; total number of nonmodified knees = 92.
Table 1.
Overall and proximal deep venous thrombosis rates as seen in the different study groups
| Modified | Nonmodified | ||
|---|---|---|---|
| 79 Knees | 92 Knees | ||
| 38% (30/79) DVT rate (p = 0.6) | 42% (39/92) DVT rate (p = 0.6) | ||
| 16% (13/79) proximal DVT rate (p = 0.4) | 12% (11/92) proximal DVT rate (p = 0.4) | ||
| Unilateral | Bilateral | Unilateral | Bilateral |
| 31 Knees | 48 Knees | 36 Knees | 56 Knees |
| 39% (12/31) DVT rate (p = 0.5) | 38% (18/48) DVT rate (p = 0.1) | 47% (17/36) DVT rate (p = 0.5) | 39% (22/56) DVT rate (p = 0.1) |
| 23% (7/31) proximal DVT rate (p = 0.1) | 13% (6/48) proximal DVT rate (p = 0.8) | 14% (5/36) proximal DVT rate (p = 0.4) | 11% (6/56) proximal DVT rate (p = 0.8) |
DVT = Deep venous thrombosis.
Sixty-nine knees in 67 patients were done unilaterally, which included two patients who underwent bilateral knee arthroplasty in a staged fashion. Venography was positive in 39% (12/31) of the modified unilateral knees and 47% (17/36) of the nonmodified, unilateral knees (p = 0.5). Thrombi were proximal in 23% (7/31) of the modified unilateral knees and 14% (5/36) of the nonmodified unilateral knees (p = 0.4).
One hundred two total knee arthroplasties in 51 patients were done bilaterally and simultaneously. Venography was positive in 38% (18/48) of the modified bilateral knees and 39% (22/56) of the nonmodified bilateral knees (p = 0.1). Thrombi were proximal in 13% (6/48) of the modified bilateral knees and 11% (6/56) of the nonmodified unilateral knees (p = 0.8).
Bilateral patients with one leg included in the modified group and the other leg in the nonmodified group demonstrated uniform results with respect to deep venous thrombosis rates (Table 2). Eighty percent (41/51) of the bilateral patients had identical findings on both of their legs: 29.4% (15/51) had positive findings on both of their legs, whereas 51.0% (26/51) had negative findings on both their legs. Twenty percent (10/51) of the bilateral patients had a positive finding on one leg and a negative finding on their other leg (10/56 knees; p < 0.0001).
Table 2.
Venography results for patients with knees performed bilaterally
| Patients with knees performed bilaterally | |||
|---|---|---|---|
| 51 Patients (102 knees) | |||
| Venography results for each of patient's knees | (−) for DVT/(+) for DVT | (−) for DVT/(−) for DVT | (+) for DVT/(+) for DVT |
| Number of patients | 10 | 26 | 15 |
| Number of patients with one of their knees undergoing surgery modified and the other knee undergoing surgery according to normal protocol | 8 | 23 | 14 |
Many of the patients in the bilateral group had one of their knees performed by the modified technique and the other knee performed by nonmodified technique.
DVT = Deep venous thrombosis.
Discussion
Deep venous thrombosis is common following total knee arthroplasty. Incidence of deep venous thrombosis after total knee replacement has been reported at rates of up to 88% [27, 53]. Thrombi commonly occur in the calf and often propagate proximally into the popliteal and femoral veins [5, 9, 15, 29, 52, 53]. Pulmonary emboli have been shown to originate from this propagation [5, 9, 15, 29, 52, 53]. Thrombi can be significantly reduced through the use of anticoagulant prophylaxis. Prophylaxis modalities include aspirin, warfarin, low molecular weight heparin, and mechanical pneumatic compression devices [1–8, 10–27, 29–54]. Despite prophylaxis, many total knee arthroplasty patients still develop deep venous thrombosis. For example, approximately 40% of the patients in this study developed thrombi while on a prophylactic regimen.
Virchow postulated that three mechanisms factor into the development of thrombosis: venous stasis, hypercoagulability, and endothelium damage. Each of these factors is present during total knee arthroplasty. During bone surgery, hypercoagulability activates clotting factors by producing the release of thromboplastins, decreasing antithrombin III levels, and changing platelet activity [18]. Kinking of the veins produces venous stasis. Damage to the vessel wall and endothelium can lead to the adhesion and aggregation of platelets. The level of damage is dependent on the amount and type of force inflicted on the vessel and the presence of any preexisting vascular pathology [18]. The severity of vascular compression, however, is unpredictable, especially if there is preexisting calcification and arteriosclerosis of the vessels. The use of tourniquet or postoperative immobilization inhibits normal venous return in the lower extremity, which may lead to venous stasis and further promoting the formation of deep venous thrombi [56–58]. Several reports have implicated tourniquet use in increasing endothelial damage [28, 59]. The tourniquet acts as a source of mechanical trauma by causing direct vascular injury.
Extreme flexion and controlled and maintained dislocation are the standard methods of exposure during the arthroplasty. The routine use of knee dislocation and prolonged extreme flexion during total knee arthroplasty may also act as another source of mechanical trauma in accordance to Virchow's theorem. Traumatic knee dislocation has been shown to cause endothelial injury [60]. Controlled dislocation may cause a rather large manipulation of vessels that can be nonpliable and fragile because of calcification and atherosclerotic plaques.
This study was conducted to investigate whether this controlled and maintained dislocation together with extreme flexion leads to an increased incidence of deep vein thrombosis. Both sets of patients in the study had knee dislocations. The nonmodified, or control, group averaged 34 min in extreme flexion and tibia-femoral dislocation. The modified group averaged 7.9 min in extreme flexion and dislocation. Deep venous thrombosis rates were 42% for the nonmodified group and 38% for the modified group (p = 0.6). Because the difference was essentially unchanged in the two groups, a power calculation was run, and it was determined that there would have to be 5000 patients in the study to see a statistically significant difference. Thus, despite the difference in time between the modified and nonmodified group (34 versus 7.9 min), deep venous thrombosis rates were not significantly different.
The present study did not find an association between the length of time the knee was in extreme flexion and the incidence of deep venous thrombosis. This study hypothesizes that dislocation itself may be the factor that leads to endothelial injury. Although the length of time the knee was in flexion and dislocation was minimized, the fact that flexion and dislocation occurred at all may be the more important factor. Duration may not be a determinant in regards to endothelial injury; any amount of dislocation and flexion could create endothelial injury. This hypothesis is supported by trends seen in the bilateral patient population. Eighty percent of the bilateral patients were either positive or negative for deep venous thrombosis on both knees despite the fact that one knee was done by the modified procedure and the other knee by the nonmodified procedure (Table 2). These results suggest that the length of dislocation was not a factor in thrombosis rates; the patients themselves appeared to be the more important factor. If, in fact, minimizing the length of time the knee spent in flexion and dislocation affected the incidence of deep venous thrombosis, thrombi should have been detected in relationship to the individual knee and not the patient.
Studies dealing with the use of a tourniquet during total knee arthroplasties may also support the current study's hypothesis. As discussed previously, using a tourniquet may damage the endothelial vessels and create venous stasis much like extreme flexion and dislocation. Abdel-Salam and Eyres [56] reported an increased incidence of deep venous thrombosis in patients that had a tourniquet, again suggesting that endothelial damage may induce thrombi formation. By kinking the veins, flexion acts much like a tourniquet. Again, time may not be a factor; the act of flexion kinks the vein causing damage to the endothelial wall regardless of how long the kinking occurs.
In conclusion, altering surgical technique to minimize the amount of time the knee spends dislocated and in extreme flexion during total knee arthroplasty does not appear to reduce the incidence of deep venous thrombosis.
References
- 1.Antiplatelet Trialists' Collaboration (1994) Collaborative overview of randomized trials of antiplatelet therapy—III: reduction in venous thrombosis and pulmonary embolism by antiplatelet prophylaxis among surgical and medical patients. Br Med J 308:235–246 [PMC free article] [PubMed]
- 2.Borow M, Goldson HJ (1983) Prevention of postoperative deep venous thrombosis and pulmonary emboli with combined modalities. Am Surgeon 49:599–605 [PubMed]
- 3.Bradley JG, Krugener GH, Jager HJ (1993) The effectiveness of intermittent plantar venous compression in prevention of deep venous thrombosis after total hip arthroplasty. J Arthroplast 8:57–61 [DOI] [PubMed]
- 4.Cohen SH, Ehrlick GE, Kauffman MS, Cope C (1973) Thrombophlebitis following knee surgery. J Bone Jt Surg 55-A:106–112 [PubMed]
- 5.Colwell CW Jr, Spiro TE, Trowbridge AA, Stephens JW, Gardiner GA Jr, Ritter MA (1995) Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep venous thrombosis after elective knee arthroplasty. Enoxaparin Clinical Trial Group. Clin Orthop Relat Res 321:19–27 [PubMed]
- 6.Comerota AJ, Katz ML, White JV (1992) Why does prophylaxis with external pneumatic compression for deep vein thrombosis fail? Am J Surg 164:265–268 [DOI] [PubMed]
- 7.Coventry MB, Nolan DR, Beckenbaugh RD (1973) “Delayed” prophylactic anticoagulation: a study of results and complications in 2,012 total hip arthroplasties. J Bone Jt Surg 55:1487–1492 [PubMed]
- 8.DeLee JC, Rockwood CA Jr (1980) The use of aspirin in thromboembolic disease. J Bone Jt Surg 62-A:149–152 [PubMed]
- 9.Doouss T (1976) The clinical significance of venous thrombosis of the calf. Br J Surg 63:377–378 [DOI] [PubMed]
- 10.Evarts CM (1992) Prevention of venous thromboembolism. Clin Ortop 222:98–104 [PubMed]
- 11.Fitzgerald RH, Spiro TE, Trowbridge AA, Gardiner GA, Whitsett TL, O'Connell MB, Ohar JA, Young TR (2001) Prevention of venous thromboembolic disease following primary total knee arthroplasty. J Bone Jt Surg 83-A(6):900–906 [PubMed]
- 12.Fordyce MJF, Ling RSM (1992) A venous foot pump reduces thrombosis after total hip replacement. J Bone Jt Surg 74-B:45–49 [DOI] [PubMed]
- 13.Gianchino A (1988) Relationship between deep-vein thrombosis in the calf and fatal pulmonary embolism. Can J Surg 31:129–130 [PubMed]
- 14.Gold EW (1988) Prophylaxis of deep venous thromboembolism. Orthopedics 11:1197–1201 [DOI] [PubMed]
- 15.Grady-Benson JC, Oishi CS, Hannson PB, Colwell CW Jr, Otis SM, Walker RJ (1994) Postoperative surveillance for deep venous thrombosis with duplex ultrasound after total knee arthroplasty. J Bone Jt Surg 76-A(11):1649–1657 [DOI] [PubMed]
- 16.Guyer RD, Booth RE Jr, Rothman RH (1982) The detection and prevention of pulmonary embolism in total hip replacement. A study comparing aspirin and low-dose warfarin. J Bone Jt Surg 64-A:1040–1044 [PubMed]
- 17.Haas SB, Insall JN, Scuderi GR, Windsor RE, Ghelman B (1990) Pneumatic sequential-compression boots compared with aspirin prophylaxis of deep-vein thrombosis after total knee arthroplasty. J Bone Jt Surg 72-A:27–31 [PubMed]
- 18.Haas SB (1999) Postoperative complications of deep vein thrombosis: prevention and treatment. In: Lotke PA, Garino J (eds) Revision total knee arthroplasty. Lippincott-Raven, Philadelphia, pp 437–446
- 19.Harris WH, Salzman EW, Athanasoulis CA, Waltman AC, Baum S, DeSanctis RW (1974) Comparison of warfarin, low-molecular-weight dextran, aspirin, and subcutaneous heparin in prevention of venous thromboembolism following total hip replacement. J Bone Jt Surg 56-A:1552–1562 [PubMed]
- 20.Harris WH, Athanasoulis C, Waltman AC, Salzman EW (1976) Cuff-impedance phlebotomy and 1251fibrinogen scanning versus roentgenographic phlebotomy for diagnosis of thromboembolism following hip surgery: a preliminary report. J Bone Jt Surg 58-A:939–944 [PubMed]
- 21.Harris WH, Athanasoulis CA, Waltman AC, Salzman EW (1982) High and low-dose aspirin prophylaxis against venous thromboembolic disease in total hip replacement. J Bone Jt Surg 64-A:63–66 [PubMed]
- 22.Harris WH, McKusick K, Athanasoulis CA, Waltman AC, Strauss HW (1984) Detection of pulmonary emboli after total hip replacement using serial C15O2 pulmonary scans. J Bone Jt Surg 66-A:1388–1393 [PubMed]
- 23.Harris WH, Athanasoulis CA, Waltman AC, Salzman EW (1985) Prophylaxis of deep-vein thrombosis after total hip replacement. Dextran and external pneumatic compression compared with 1.2 or 0.3 gram of aspirin daily. J Bone Jt Surg 67-A:57–62 [PubMed]
- 24.Hartman JT, Pugh JL, Smith RD, Robertson WW Jr, Yost RP, Janssen HF (1982) Cyclic sequential compression of the lower limb in prevention of deep venous thrombosis. J Bone Jt Surg 64-A:1059–1062 [PubMed]
- 25.Hull R, Delmore TJ, Hirsh J, Gent M, Armstrong P, Lofthouse R et al (1979) Effectiveness of intermittent pulsatile elastic stockings for the prevention of calf and thigh vein thrombosis in patients undergoing elective knee surgery. Thromb Res 16:37–45 [DOI] [PubMed]
- 26.Hull RD, Raskob GE (1986) Current concepts review. Prophylaxis of venous thromboembolic disease following hip and knee surgery. J Bone Jt Surg 68-A:146–150 [PubMed]
- 27.Insall JN, Haas SB (1993) Complications of total knee arthroplasty. In: Insall JN (ed) Surgery of the knee. Churchill Livingstone, New York, pp 891–894
- 28.Irving GA, Noakes TD (1985) The protective role of local hypothermia in tourniquet-induced ischaemia of muscle. J Bone Jt Surg Br 67(2):297–301 [DOI] [PubMed]
- 29.Kakkar VV, Howe CT, Flanc C, Clarke MB (1969) Natural history of postoperative deep-vein thrombosis. Lancet 2:230–232 [DOI] [PubMed]
- 30.Lotke PA (1989) Thromboembolic disease: a critical review. Bull Am Acad Orthop Surg 37:20–21
- 31.Lotke PA, Ecker ML, Alavi A, Berkowitz H (1984) Indications for the treatment of deep venous thrombosis following total knee replacement. J Bone Jt Surg 66-A:202–208 [PubMed]
- 32.Lotke PA, Wong RY, Ecker ML (1986) Asymptomatic pulmonary embolism after total knee replacement. Orthop Trans 10:490
- 33.Lotke PA, Palevsky H, Keenan AM, Meranze S, Steinberg ME, Ecker ML et al (1996) Aspirin and warfarin for thromboembolic disease after total joint arthroplasty. Clin Ortop 324:251–258 [DOI] [PubMed]
- 34.McCardel BR, Lachiewicz PF, Jones K (1990) Aspirin prophylaxis and surveillance of pulmonary embolism and deep vein thrombosis in total hip arthroplasty. J Arthroplast 5:181–185 [DOI] [PubMed]
- 35.McKenna R, Bachmann F, Kaushal SP, Galante JO (1976) Thromboembolic disease in patients undergoing total knee replacement. J Bone Jt Surg 58-A:928–932 [PubMed]
- 36.McKenna R, Galante J, Bachmann F, Wallace DL, Kaushal SP, Meredith P (1980) Prevention of venous thromboembolism after total knee replacement by high-dose aspirin or intermittent calf and thigh compression. Br Med J 280:514–517 [DOI] [PMC free article] [PubMed]
- 37.Modig J, Borg T, Karlström G, Maripuu K, Sahlstedt B (1983) Thromboembolism after total hip replacement: role of epidural and general anesthesia. Anesth Analg 62:174–180 [DOI] [PubMed]
- 38.Morrey BF, Adams RA, Ilsrtup DM, Bryan RS (1987) Complications and mortality associated with bilateral or unilateral total knee arthroplasty. J Bone Jt Surg 69-A:484–488 [PubMed]
- 39.Moser KM, Le Moine JR (1981) Is embolic risk conditioned by location of deep venous thrombosis? Ann Intern Med 94:574–580 [DOI] [PubMed]
- 40.Paiement G, Wessinger SJ, Waltman AC, Harris WH (1987) Low-dose warfarin versus external pneumatic compression for prophylaxis against venous thromboembolism following total hip replacement. J Arthroplast 2:23–26 [DOI] [PubMed]
- 41.Paiement GD, Bell D, Wessinger SJ et al (1987) New advances in prevention, diagnosis, and cost effectiveness of venous thromboembolic disease in patients with total hip replacement. The hip, proceedings of the fourteenth open scientific meeting of the Hip Society. C.V. Mosby, St. Louis, pp 94–119 [PubMed]
- 42.Paiement GD, Beisaw NE, Lotke PA, Elia E, Wessinger S, Harris W (1989) Advances in the prevention of venous thromboembolic disease after hip and knee surgery. Orthop Rev 18:1–20
- 43.Paiement GD, Beisaw NE, Harris WH, Wessinger SJ, Wyman EM (1990) Advances in prevention of venous thromboembolic disease after elective hip surgery. Instr Course Lect 39:413–421 [PubMed]
- 44.Roberts TS, Nelson CL, Barnes CL et al (1989) Low dose dextran 40 in reconstructive hip surgery patients. Orthopedics 12:789–801 [DOI] [PubMed]
- 45.Santori FS, Vitullo A, Stopponi M, Santori N, Ghera S (1994) Prophylaxis against deep-vein thrombosis in total hip replacement. Comparison of heparin and foot impulse pump. J Bone Jt Surg 76-B:579–583 [PubMed]
- 46.Sharrock NE, Brien WW, Salvati EA, Mineo R, Garvin K, Sculco TP (1990) The effect of intravenous fixed-dose heparin during total hip arthroplasty on the incidence of deep-vein thrombosis. A randomized double-blind trial in patients operated on with epidural anesthesia and controlled hypotension. J Bone Jt Surg 72-A:1456–1461 [PubMed]
- 47.Sharrock NE, Haas SB, Hargett MJ, Urquhart B, Insall JN, Scuderi G (1991) Effects of epidural anesthesia on the incidence deep-vein thrombosis after total knee arthroplasty. J Bone Jt Surg 73-A:502–506 [PubMed]
- 48.Sikorski JM, Hampson WG, Staddon GE (1981) The natural history and aetiology of deep vein thrombosis after total hip replacement. J Bone Jt Surg 63-B:171–177 [DOI] [PubMed]
- 49.Stranks GJ, MacKenzie NA, Grover ML, Fail T (1992) The A-V impulse system reduces deep-vein thrombosis and swelling after hemiarthroplasty for hip fractures. J Bone Jt Surg 74-B:775–778 [DOI] [PubMed]
- 50.Stringer MD, Steadman CA, Hedges AR, Thomas EM, Morley TR, Kakkar VV (1989) Deep vein thrombosis after elective knee surgery: an incidence study in 312 patients. J Bone Jt Surg 71-B:492–497 [DOI] [PubMed]
- 51.Stulberg BN, Dorr LD, Ranawat CS, Schneider R (1982) Aspirin prophylaxis for pulmonary embolism following total hip arthroplasty: an incidence study. Clin Ortop 168:119–123 [PubMed]
- 52.Westrich GH, Sculco TP (1996) Prophylaxis against deep vein thrombosis after total knee arthroplasty. Pneumatic plantar compression and aspirin compared to aspirin alone. J Bone Jt Surg 78-A(6):826 [DOI] [PubMed]
- 53.Westrich GH, Menezes A, Sharrock N, Sculco TP (1999) Thromboembolic disease prophylaxis in total knee arthroplasty using intraoperative heparin and postoperative pneumatic foot compression. J Arthroplast 14(6):651–656 [DOI] [PubMed]
- 54.Wilson NV, Das SK, Kakkar VV, Maurice HD, Smibert JG, Thomas EM et al (1992) Thrombo-embolic prophylaxis in total knee replacement. Evaluation of the A-V impulse system. J Bone Jt Surg 74–78 [DOI] [PubMed]
- 55.Westrich GH, Allen ML, Tarantino SJ, Ghelman B, Schneider R, Laskin RS et al (1998) Ultrasound screening for deep venous thrombosis after total knee arthroplasty. 2-year reassessment. Clin Orthop Relat Res 356:125–133 [DOI] [PubMed]
- 56.Abdel-Salam A, Eyres KS (1995) Effects of tourniquet during total knee arthroplasty. A prospective randomised study. J Bone Jt Surg Br 77(2):250–253 [PubMed]
- 57.Harvey EJ, Leclerc J, Brooks CE, Burke DL, Anders MJ, Lifeso RM et al (1997) Effect of tourniquet use on blood loss and incidence of deep vein thrombosis in total knee arthroplasty. J Arthroplast 12:291–296 [DOI] [PubMed]
- 58.Wakankar HM, Nicholl JE, Koka R, D'Arcy JC (1999) The tourniquet in total knee arthroplasty. A prospective, randomised study [see comments]. J Bone Jt Surg Br 81(1):30–33 [DOI] [PubMed]
- 59.Irvine GB, Chan RN (1986) Arterial calcification and tourniquets. Lancet 2(8517):1217 [DOI] [PubMed]
- 60.Wascher DC, Dvirnak PC, DeCoster TA (1997) Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma 11(7):525–529 [DOI] [PubMed]
- 61.Westrich GW, Allen ML, Tarantino S, Ghelman B, Schneider R, Laskin RS, Haas SB, Sculco TP (1998) Ultrasound screening for deep venous thrombosis after total knee arthroplasty. Clin Orthop Relat Res 336:125–133 [DOI] [PubMed]