Abstract
A growing body of evidence indicates that PPAR (peroxisome proliferator-activated receptor) α agonists might have therapeutic usefulness in antitumoral therapy by decreasing abnormal cell growth, and reducing tumoral angiogenesis. Most of the anti-inflammatory and antineoplastic properties of PPAR ligands are due to their inhibitory effects on transcription of a variety of genes involved in inflammation, cell growth and angiogenesis. Cyclooxygenase (COX)-2 and vascular endothelial growth factor (VEGF) are crucial agents in inflammatory and angiogenic processes. They also have been significantly associated to cell proliferation, tumor growth, and metastasis, promoting tumor-associated angiogenesis. Aberrant expression of VEGF and COX-2 has been observed in a variety of tumors, pointing to these proteins as important therapeutic targets in the treatment of pathological angiogenesis and tumor growth. This review summarizes the current understanding of the role of PPARα and its ligands in the regulation of COX-2 and VEGF gene expression in the context of tumor progression.
1. INTRODUCTION
Peroxisome proliferator-activated receptors (PPARs) are members of the nuclear receptor family of transcription factors. They modulate gene transcription in response to specific ligands by binding as heterodimers with the retinoid X receptor (RXR) to a specific peroxisome proliferator-response element (PPREs) on target genes (reviewed in [1, 2]). Three distinct isoforms of PPARs have been described PPAR α, β/δ, and γ, each encoded by a different gene and showing a distinct tissue distribution [3]. Originally found to be involved in the regulation of lipid and glucose metabolism, [4, 5] interest in these receptors has increased dramatically as a consequence of recent studies showing their involvement in tumoral cell growth and inflammation (reviewed in [6–9]). Therefore, in addition to their well-known effects in diabetes and hyperlipidemic disorders, pharmacological agents that target PPARs may have therapeutic applications in inflammatory diseases and cancer.
PPARα was the first PPAR identified [10]. It has a wide tissue distribution being expressed in liver, skeletal muscle, intestine, kidney, adipose tissue, and vascular endothelial cells, tissues in which fatty acids are predominantly catabolized [11, 12]. Several ligands have been shown to bind PPARα and to regulate transcriptional activity of target genes involved in the regulation of fatty acid metabolism as fatty acid transporters, catabolic enzymes involved in mitochondrial, and peroxisomal oxidation as well as genes necessary for the maintenance of redox balance during the oxidative catabolism of fatty acids [4, 5, 13]. PPARα-activating ligands include a number of pharmacological compounds as well as fatty acid and fatty acid-derived molecules (reviewed in [2]). Lipid-lowering fibrates as Bezafibrate, Clofibrate, Fenofibrate and Gemfibrozil as well as certain nonsteroidal anti-inflammatory drugs (NSAIDs) bind and activate PPARα [14, 15]. In addition, a variety of unsaturated and saturated fatty acids including arachidonic acid, palmitic acid, linoleic acid, linolenic acid, and oleic acid can act as natural ligands of PPARα as they can bind and activate this receptor. Some eicosanoids derived from the metabolism of arachidonic acid such as leukotrienes (LTs), hydroxyeicosatetraenoic acids (HETEs), and prostaglandins (PGs) can also be effective ligand agonists for specific PPAR isoforms [16–19]. However, it is not clear whether the concentrations at which binding of these compounds occurs are physiologically relevant.
In addition to its known role in the regulation of genes involved in fatty acid metabolism, this isoform has been shown to attenuate the inflammatory response [6, 7, 9]. Most recently, an antitumoral role of PPARα and its ligands has been proposed [7, 8]. This assumption is supported by recent experimental evidence, revealing antitumoral and anti-angiogenic properties of PPARα activators both in vitro and in vivo.
2. ANTI-INFLAMMATORY ACTIONS OF PPARα
In recent years, considerable attention has focused on the involvement of PPARs in inflammatory processes. Anti-inflammatory effects of PPAR ligands, in particular those of PPARα and PPARγ, have been ascribed to inhibition of the expression of inflammatory genes and negative interference with pro inflammatory transcription factor signaling pathways in vascular and inflammatory cells (reviewed in [1, 6, 20]. The first evidence for the involvement of PPARα in the control of inflammation came from the studies of the inflammatory response elicited by LTB4 in PPARα deficient mice. In these animals, inflammatory response to LTB4 was prolonged compared to WT mice, correlating with the ability of LTB4 to activate PPARα and regulate the expression of genes involved in its own catabolism [21]. Thus, proinflammatory lipid metabolites may serve as ligands for PPARs thereby activating PPARα responsive enzymes responsible for their clearance. Therefore, some of the anti-inflammatory actions of these receptors can occur through this autoregulatory loop in lipid homeostasis. Several lipids mediators, as the polyunsaturated fatty acids (PUFAs), can function as ligands for PPARs [2]. Arachidonic acid is a precursor of several eicosanoids that have pro inflammatory properties whereas the ω-3 PUFAs are precursors of anti-inflammatory eicosanoids as EPA (eicosapentanoid acid) and docosahexaenoic acid (DHA). These ω-3 PUFAs derivatives have been reported to decrease the production of several pro inflammatory cytokines, having beneficial effects in several inflammatory diseases as rheumatoid arthritis and inflammatory bowel disease [22, 23].
Several studies have confirmed the anti-inflammatory properties of PPARs in vitro and in vivo through the regulation of genes involved in the inflammatory response. PPAR agonists decrease plasma concentrations of interleukin (IL)-6, tumor necrosis factor (TNF)-α, and interferon (IFN)-γ in humans [24, 25]. In vascular smooth-muscle cells, PPARα ligands inhibit IL-1-induced production of IL-6, COX-2, and prostaglandins [25]. PPARα activation inhibits cytokine-induced expression of vascular cell-adhesion molecule-1 (VCAM-1) and vascular endothelial growth factor receptor-2 (VEGFR-2) in endothelial cells [26, 27]. PPARα have been also involved in the downregulation of the production of IL-2 and TNFα by T lymphocytes [28].
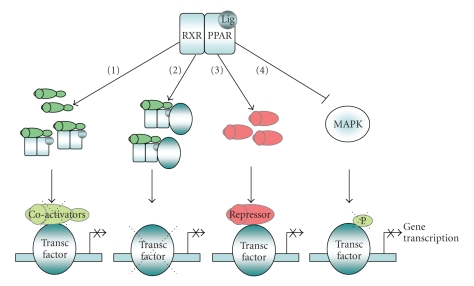
At the molecular level, most of the inhibitory actions of PPARα on gene transcription result from its ability to transrepress the activities of many activated transcription factors such as nuclear factor (NF)-κB [25, 29], activator protein-1 (AP-1) [29, 30] C/EBPβ [31, 32], signal transducers and activators of transcription (STATs) [33], and transcription factor specificity protein 1 (Sp-1) [27]. Negative regulation of gene expression by PPARα can occur by several mechanisms (Figure 1). Activated PPAR-RXR complexes may compete for limited amounts of essential coactivators shared with other transcription factors. Direct physical interactions between PPARs and specific transcription factors have been also proposed to mediate transcriptional inhibition by activated PPARα, resulting in reduced binding to their cognate response elements. Agonists-activated PPARα can effectively antagonize NF-κB and AP-1-mediated signaling pathways in a bidirectional manner by physical interaction with the Rel homology domain of NFκB-p65 and with the aminoterminal of c-Jun, respectively [34]. Physical association of the C-terminal DNA binding region of c/EBPβ with PPARα mediates inhibition of alpha1-acid glycoprotein gene expression [31]. PPARα agonists can also influence transcriptional activation by modulating the expression of transcriptional repressors such as IκBα (Kleemann, 2003 #1223; Vanden Berghe, 2003 #2170}). Finally, an additional mechanism of transrepression relies on the ability of some PPARα ligands to interfere with the activation of certain members of the mitogen-activated protein kinase (MAPK) cascade as Jun kinase (JNK) and p38 MAPK [30, 35, 36].
Figure 1.
Negative regulation of gene expression by PPARs. Different mechanisms of transrepression through interference of activated PPARs with activation of transcription factors have been described. (1) Activated PPAR-RXR complexes may sequester essential coactivators shared with other transcription factors. (2) Physical association of PPARs with specific transcription factors results in reduced binding to their cognate response elements. (3) PPARα agonists can also influence transcriptional activation by upregulating the expression of transcriptional repressors such as IκBα. (4) PPARα-mediated interference on the activation of members of the mitogen-activated protein kinase (MAPK) cascade influences transcription factor activation.
3. INVOLVEMENT OF PPARα IN CANCER
Rapidly accumulating evidence links members of the PPAR family and their agonists to cellular growth and tumor progression. The role of the PPARγ isotype in cancer has been widely studied with a large number of reports demonstrating antitumoral properties of PPARγ agonists in a variety of different malignancies [8]. Concerning to the involvement of the PPARα form and its ligands in cancer, both tumor promotion and suppression properties have been reported [37]. Sustained PPARα activation by agonists as clofibrate and Wy-14643 induce hepatocarcinogenesis in rodents [38, 39]. However, epidemiological data on long-term administration of PPARα activators in the clinic discard the occurrence of these effects in human [40–43]. Discrepancies on the effects of PPARα ligands in rodents and human liver seem to be due to several differences between species [44]. PPARα mediated signaling is less efficient in human than in mice [37, 43, 45] and expression of this receptor is 10 to 20 times higher in rodent hepatocytes compared to human liver [46].
Emerging evidence indicates that PPARα ligands are able to suppress the growth of different types of human carcinomas. PPARα is expressed in a variety of human and murine tumor cell lines [47–49]. Expression of PPARα have been also reported in clinical samples of several types of human cancers as colorectal carcinoma [50], prostate adenocarcinoma, [47, 51], testicular cancer [52], bladder carcinoma [53], and medulloblastoma [54]. PPARα ligands are able to arrest the growth of human cancer cell lines in vitro and to slow the growth of transplanted human tumor cells in nude mice. These anticancer effects have been observed in several different cancer cell types including hepatoma [55], melanoma [56], glioblastoma and fibrosarcoma [49], endometrial and ovarian cancer [57–59], as well as colon carcinoma [50, 60, 61]. Clofibric acid, a ligand for PPARα inhibits growth of ovarian cancer both in vivo and in vitro [58, 59]. Mice treated topically with the PPARα ligand Wy-14643 exhibited diminished skin tumorigenesis [62]. Moreover, Fenofibrate suppresses the metastatic potential of melanoma cells [56, 63].
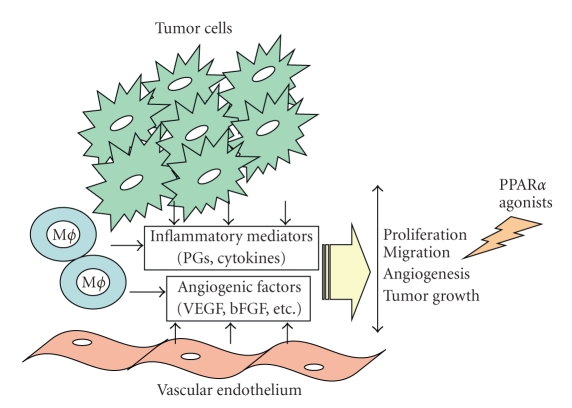
Even though accumulative evidence shows data suggesting that PPARα ligands may display antitumoral properties, the precise mechanism remains unclear. A number of reports suggest that antitumor properties of PPARα activators reside on their anti-inflammatory and anti-angiogenic effects [27, 64, 65] (Figure 2). The dependence on the presence of PPARα for the antitumorigenic and anti-angiogenic role of PPAR ligands has been determined by the analysis of their effects in PPARα null mice. Wy-14643-mediated antitumoral and anti-angiogenic responses on tumor and endothelial cells are absent in PPARα KO mice [66]. Panigrahy and coworkers [49] have shown the importance of the microenvironment in tumor progression in such a way that the activation of PPARα expressed in endothelial and inflammatory cells of the host rather than in the tumoral cells is critical for anti-inflammatory, antitumor and anti-angiogenic activity of PPARα agonists. Consistent with the anti-inflammatory role of this receptor, PPARα null mice exhibit an increase of inflammatory infiltrates in tumors. Paradoxically, in spite of the enhanced inflammatory response in the absence of PPARα, tumor growth is suppressed in these animals as a consequence of an increased production of anti-angiogenic factors TSP-1 and endostatin [67]. The immune system can have a multitude of effects on cancer development and progression, both favorable and detrimental [68, 69]. This apparent contradiction has been explained by the severity and duration of the inflammatory response associated to tumor growth. While acute inflammation is part of the defense response that may participate in the remission of preclinical cancers, chronic inflammation can promote tumor development with infiltrating innate immune cells providing proinflammatory and proangiogenic factors including cytokines, chemokines, VEGF, and prostanoids [70–72]. The association between cancer and inflammation has been also illustrated by epidemiological studies showing that the use of anti-inflammatory compounds in chronic inflammatory diseases reduces cancer risk tumor [73, 74]. In this sense, PPARα-mediated anti-inflammatory actions can be responsible for their potential chemopreventive effects in tumor progression.
Figure 2.
Antitumoral effects of PPARα ligands. Tumor progression depends on a cascade of cellular signals involving: (a) proinflammatory factors (cytokines, COX-2 derived prostaglandins (PGs), chemokines); (b) proangiogenic factors (VEGF, bFGF, and PGs) produced by endothelial and inflammatory cells, stromal fibroblasts, and tumor cells. These factors promote cell proliferation, migration, and induce new vessels that deliver nutrients and oxygen to the malignant cells and therefore allow tumor growth and metastasis. PPARα ligands may display antitumoral properties by their inhibitory effects on the transcription of genes involved in inflammation, cell growth, and angiogenesis thus leading to the inhibition of tumor growth.
An emerging area of interest is the association of anti-inflammatory actions of dietary PUFAs as potential natural agonists of PPARs with cancer risk. Increasing evidence suggests that dietary fat regulation of gene expression can play a critical role in initiation and progression of human cancer and epidemiological studies have suggested an association between dietary fat and cancer risk [75, 76]. A number of reports have shown the beneficial effects of consumption of ω-3 PUFAs, associated with anti-inflammatory effects and with protection against primary tumor development [22, 23, 75]. Although some of the effects of dietary lipids can be linked to PPARs-mediated signaling, additional research is needed to understand the potential connection between dietary fat intake and PPARs in the control of inflammation and tumor progression.
4. PPARα, COX-2, AND CANCER
4.1. COX-2: an essential role in inflammation and tumor growth
Cyclooxygenases (COX-1 and COX-2) convert arachidonic acid to prostaglandin H2(PGH2), an endoperoxide intermediate that, via specific synthases, is then transformed to prostaglandins (PGE2, PGD2, PGF2α, PGI2) and thromboxanes (TXA2). Whereas COX-1 is constitutively expressed in most tissues, COX-2 is transcriptionally upregulated in response to mitogens, tumor promoters, and pro inflammatory stimuli in a discrete number of cell types (reviewed in [77–79]). These enzymes are the target of nonsteroidal anti-inflammatory drugs (NSAIDs), one of the most widely used therapeutic for the relief of pain and inflammation (reviewed in [80–82]). The anti-inflammatory and analgesic efficacy of drugs arises essentially from inhibition of the enzymatic activity of COXs. As COX-2 is though to be the predominant isoform involved in the inflammatory response, the ability of NSAIDs to inhibit COX-2 activity may explain their therapeutic effects as anti-inflammatory drugs. Therefore, most of the new research on anti-inflammatory drugs has been aiming at targeting the COX-2 inducible production of PGs.
In addition to its essential role in inflammation, accumulating evidence links COX-2 with cancer and angiogenesis, suggesting that drugs that target COX-2 and related signaling cascades could be used as antitumoral agents [74]. Many human cancers display elevated COX-2 expression and studies in COX-2 null mice have demonstrated the role of this enzyme in tumor progression and metastasis [83–85]. Moreover, epidemiological studies have revealed a role of selective COX-2 inhibitors in decreasing the risk of developing colon cancer and in suppressing tumor formation and growth in animal models [73, 86–88]. COX-2 inhibitors can block both the production of angiogenic factors and the migration of vascular endothelial cells, and thus decrease tumor growth [89, 90]. Although some of the effects of these drugs on tumor regression might result from modulation of COX-2-independent pathways [91], it is likely that COX-2 is an important mediator of tumor growth.
4.2. Effects of PPARα ligands on COX-2 expression
The activity of COX-2 is closely linked to PPARs as COX-2 catalyzes the production of fatty acid derivates as prostanoids that are PPAR activators [2]. Modulation of COX-2 activity should influence the local availability of PPAR ligands; therefore, indirectly modulating PPAR activity. Moreover, some NSAIDs may act as PPARα and γ ligands, suggesting that, in addition to inhibit prostaglandin production, they might regulate gene expression as part of their anti-inflammatory and chemopreventive mechanisms [92, 93]. Downregulation of COX-2 expression by PPARα ligands may account for some of the anti-inflammatory, anti-angiogenic and antitumoral properties of these drugs in a variety of cell types [20] (Table 1). PPARα agonists as Wy-14643 inhibit macrophage differentiation and COX-2 gene expression [94]. In liver, COX-2 upregulation upon experimental nutritional steatohepatitis is suppressed by the PPARα agonist Wy-14,643 in wt but not in PPARα KO mice. This effect has been ascribed to the ability of activated PPARα to interfere with the NF-κB-signaling pathway [95]. Transcriptional interference of activated PPARα with NF-κB also explains the inhibition of COX-2 induction and PG production in response to IL-1 in vascular smooth muscle cells [25]. The NF-κB target genes VCAM-1 and COX-2 are also downregulated by PPARα ligands in response to cytokine activation [29]. Regarding to experimental support for anti-angiogenic and antitumoral actions of these drugs related to their effects on COX-2 expression, it has been shown that Fenofibrate inhibits bFGF-mediated angiogenesis and COX-2 mRNA expression in endothelial cells [65]. Panigrahy and cols have observed suppression of COX-2 expression in Fenofibrate and Wy-14643 treated tumors [49]. Clofibric acid suppresses the growth of tumor xenograts of ovarian cancer cell lines with decreased microvessel density, PGE2 production, and COX-2 and mPGES-1 expression [58, 59]. Diminished expression of COX-2 upon PPARα agonist treatment was parallel with reduced expression of AP-1. Similarly, in colon carcinoma cells, PPARα agonists severely diminish phorbol ester-mediated AP-1-dependent induction of COX-2 expression [30].
Table 1.
Effects of PPARα ligands on COX-2 signaling.
| PPARα ligand | Action/effect | References |
|---|---|---|
| Wy-14643 | ||
| Inhibition of IL-1-induced COX-2 expression in vascular smooth muscle cells | [25] | |
| Inhibition of LPS-induced COX-2 expression in THP-1 monocytes | [94] | |
| Inhibition of TPA-induced COX-2 expression in colon carcinoma cell lines | [30] | |
| Inhibition of COX-2 expression in B16-F10 melanoma tumor | [49] | |
| Inhibition of COX-2 up regulation by experimental steatohepatitis in liver | [95] | |
|
| ||
| Fenofibrate | ||
| Inhibition of COX-2 expression in B16-F10 melanoma tumor | [49] | |
| Inhibition of b-FGF induced COX-2 expression in endothelial cells | [65] | |
|
| ||
| Clofibric acid | ||
| Inhibition of COX-2 expression in tumor xenografts | [58] | |
| Inhibition of mPGES-1 expression in tumor xenografts | [59] | |
5. PPARα, VEGF, AND CANCER
5.1. VEGF: a therapeutic target in tumoral angiogenesis
Angiogenesis, defined as the formation of new blood vessels from preexisting vasculature, occurs under physiological conditions during embryonic development and is required for wound healing and reproduction in the adult. Indispensable for physiological processes, angiogenesis is highly regulated via fine tuning of the balance between pro- and anti-angiogenic factors [97]. Excessive angiogenesis is tightly linked to human disease, including chronic inflammatory disease, diabetic retinopathy, and cancer [98, 99]. Ample evidence shows that blockade of tumoral angiogenesis often relieves the severity of cancer [100].
Both cancer cells and cells attracted to the sites of inflammation are able to produce proangiogenic factors that cause endothelial cell recruitment and proliferation for the supply of oxygen and nutrients that favor the growth of solid tumors and facilitate metastasis. In this context, tumor-associated hypoxia plays an essential role in the regulation of angiogenesis [101]. Response to hypoxia is mediated by members of the hypoxia-inducible transcription factors (HIFs) involved in the regulation of the expression of genes participating in oxygen homeostasis [102, 103]. In addition, hypoxia has been also found to drive induction of potent angiogenic and inflammatory factors including VEGF, VEGF-R1 and -R2, angiotensin, metalloproteinases, and COX-2 [104–106]. This response of tumors to hypoxia contributes to the malignant phenotype and to more aggressive tumor progression [107].
It has been well established that VEGF signaling pathway is one of the key regulators in angiogenesis [108, 109]. Cytokines, growth factors, tumor promoters, and hypoxia modulate the expression of VEGF [110, 111]. Activated VEGF may bind to two types of tyrosine kinases receptors: VEGFR-1 and VEGFR-2. Proangiogenic actions of VEGF as vascular endothelial cell permeability, proliferation migration, and survival are mediated mainly through binding an activation of the VEGFR-2 [112, 113]. Accumulating evidence supports a key role of VEGF in cancer, contributing to tumor neovascularization and dissemination. Increased expression of this factor has been found in most tumors, and agents neutralizing VEGF expression or activity inhibit tumor growth in vivo (reviewed in [99, 100, 114]).
5.2. Inhibition of VEGF signaling by PPARα agonists
PPARα ligands can inhibit endothelial cell proliferation and migration and induce endothelial cell apoptosis in vitro, suggesting an important role of this receptor in tumor angiogenesis. Part of these effects occurs through the ability of PPARα ligands to interfere with VEGF-mediated signaling. (Table 2). At the transcriptional level, PPAR agonists have been shown to inhibit endothelial VEGFR-2 expression by repressing transactivation and binding of Sp1 to DNA [27]. Wy-14643 downregulates TPA-mediated transcriptional induction of VEGF by interference with activation of AP-1 [30]. Interestingly, lipid-lowering therapy with Fenofibrate induces a significant reduction of VEGF levels in serum [96]. Anti-angiogenic actions of PPARα agonists may explain some of their antitumoral effects. Fenofibrate reduces adventitial angiogenesis and inflammation in a porcine model of coronary angioplasty [115]. Both Fenofibrate and Wy-14643 are able to suppress VEGF secretion in glioblastoma cells and Lewis lung carcinoma cells and to inhibit angiogenesis both in vivo and in vitro [49]. Moreover, Clofibric acid inhibits VEGF expression in tumor xenografts of ovarian cancer cell lines with a reduction in angiogenesis and decreased microvessel density in solid tumors [58, 59].
Table 2.
Effects of PPARα ligands on VEGF signaling.
| PPARα ligand | Action/effect | References |
|---|---|---|
| Wy-14643 | ||
| Inhibition of VEGF-mediated endothelial cell migration | [27, 49, 64] | |
| Inhibition of VEGF production by glioblastoma U87 cells | [49] | |
| Inhibition of VEGF-induced phosphorylation of Akt | [64] | |
| Inhibition of VEGF-mediated angiogenesis in vitro | [27] | |
|
| ||
| Fenofibrate | ||
| Inhibition of VEGF production by glioblastoma U87 cells | [49] | |
| Reduction of plasma VEGF | [96] | |
| Inhibition of VEGF-induced phosphorylation of Akt | [64] | |
| Inhibition of VEGFR2 expression in endothelial cells | [27] | |
|
| ||
| Clofibric acid | ||
| Inhibition of VEGF expression in tumor xenografts | [58] | |
6. CONCLUSIONS
Taken together, findings on the effects of PPARα ligands in inflammation and cancer, suggest that PPARα activation may be beneficial against tumorigenesis through the inhibition of transcriptional activation of genes involved in inflammation and angiogenesis such as COX-2 and VEGF. Although COX-2 and VEGF are one of the many proinflammatory and proangiogenic factors that drive tumor growth and metastasis, targeting these proteins suffices to significantly impair tumor growth and angiogenesis. Inhibition of tumor inflammation and tumor angiogenesis by PPARα ligands might be responsible for their potential chemopreventive effects in a variety of experimental models of cancer. However, it must be taken into account that many of the reported effects of PPARα ligands on tumor progression have been obtained in vitro and await confirmation by additional basic and clinical research to ascertain whether they can be considered of pharmacological significance in vivo.
ACKNOWLEDGMENTS
The authors thank the financial support of Comunidad Autónoma de Madrid (S-SAL-0159-2006), Ministerio de Educación y Ciencia-FEDER (SAF 2004-05109, BFU2004-04157, and BFU2007-62659), European Commission (EICOSANOX integrated project LSH-CT-2004-005033; and MAIN network of excellence), and Laboratorios del Dr. ESTEVE S. A. We apologize that many valuable studies, especially original contributions, have not been cited due to space limitation.
References
- 1.Berger J, Moller DE. The mechanisms of action of PPARs. Annual Review of Medicine. 2002;53:409–435. doi: 10.1146/annurev.med.53.082901.104018. [DOI] [PubMed] [Google Scholar]
- 2.Corton JC, Anderson SP, Stauber A. Central role of peroxisome proliferator-activated receptors in the actions of peroxisome proliferators. Annual Review of Pharmacology and Toxicology. 2000;40:491–518. doi: 10.1146/annurev.pharmtox.40.1.491. [DOI] [PubMed] [Google Scholar]
- 3.Michalik L, Wahli W. Peroxisome proliferator-activated receptors: three isotypes for a multitude of functions. Current Opinion in Biotechnology. 1999;10(6):564–570. doi: 10.1016/s0958-1669(99)00030-0. [DOI] [PubMed] [Google Scholar]
- 4.Schoonjans K, Staels B, Auwerx J. The peroxisome proliferator activated receptors (PPARs) and their effects on lipid metabolism and adipocyte differentiation. Biochimica et Biophysica Acta. 1996;1302(2):93–109. doi: 10.1016/0005-2760(96)00066-5. [DOI] [PubMed] [Google Scholar]
- 5.Wahli W, Braissant O, Desvergne B. Peroxisome proliferator activated receptors: transcriptional regulators of adipogenesis, lipid metabolism and more. Chemistry and Biology. 1995;2(5):261–266. doi: 10.1016/1074-5521(95)90045-4. [DOI] [PubMed] [Google Scholar]
- 6.Daynes RA, Jones DC. Emerging roles of PPARs in inflammation and immunity. Nature Reviews Immunology. 2002;2(10):748–759. doi: 10.1038/nri912. [DOI] [PubMed] [Google Scholar]
- 7.Gelman L, Fruchart J-C, Auwerx J. An update on the mechanisms of action of the peroxisome proliferator-activated receptors (PPARs) and their roles in inflammation and cancer. Cellular and Molecular Life Sciences. 1999;55(6-7):932–943. doi: 10.1007/s000180050345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Michalik L, Desvergne B, Wahli W. Peroxisome-proliferator-activated receptors and cancers: complex stories. Nature Reviews Cancer. 2004;4(1):61–70. doi: 10.1038/nrc1254. [DOI] [PubMed] [Google Scholar]
- 9.Fruchart J-C, Duriez P, Staels B. Peroxisome proliferator-activated receptor-alpha activators regulate genes governing lipoprotein metabolism, vascular inflammation and atherosclerosis. Current Opinion in Lipidology. 1999;10(3):245–257. doi: 10.1097/00041433-199906000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Issemann I, Green S. Activation of a member of the steroid hormone receptor superfamily by peroxisome proliferators. Nature. 1990;347(6294):645–650. doi: 10.1038/347645a0. [DOI] [PubMed] [Google Scholar]
- 11.Auboeuf D, Rieusset J, Fajas L, et al. Tissue distribution and quantification of the expression of mRNAs of peroxisome proliferator-activated receptors and liver X receptor-α in humans: no alteration in adipose tissue of obese and NIDDM patients. Diabetes. 1997;46(8):1319–1327. doi: 10.2337/diab.46.8.1319. [DOI] [PubMed] [Google Scholar]
- 12.Inoue I, Shino K, Noji S, Awata T, Katayama S. Expression of peroxisome proliferator-activated receptor α (PPARα) in primary cultures of human vascular endothelial cells. Biochemical and Biophysical Research Communications. 1998;246(2):370–374. doi: 10.1006/bbrc.1998.8622. [DOI] [PubMed] [Google Scholar]
- 13.Leone TC, Weinheimer CJ, Kelly DP. A critical role for the peroxisome proliferator-activated receptor α (PPARα) in the cellular fasting response: the PPARα-null mouse as a model of fatty acid oxidation disorders. Proceedings of the National Academy of Sciences of the United States of America. 1999;96(13):7473–7478. doi: 10.1073/pnas.96.13.7473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Willson TM, Brown PJ, Sternbach DD, Henke BR. The PPARs: from orphan receptors to drug discovery. Journal of Medicinal Chemistry. 2000;43(4):527–550. doi: 10.1021/jm990554g. [DOI] [PubMed] [Google Scholar]
- 15.Lehmann JM, Lenhard JM, Oliver BB, Ringold GM, Kliewer SA. Peroxisome proliferator-activated receptors α and γ are activated by indomethacin and other non-steroidal anti-inflammatory drugs. The Journal of Biological Chemistry. 1997;272(6):3406–3410. doi: 10.1074/jbc.272.6.3406. [DOI] [PubMed] [Google Scholar]
- 16.Xu HE, Lambert MH, Montana VG, et al. Molecular recognition of fatty acids by peroxisome proliferator-activated receptors. Molecular Cell. 1999;3(3):397–403. doi: 10.1016/s1097-2765(00)80467-0. [DOI] [PubMed] [Google Scholar]
- 17.Forman BM, Chen J, Evans RM. Hypolipidemic drugs, polyunsaturated fatty acids, and eicosanoids are ligands for peroxisome proliferator-activated receptors α and δ . Proceedings of the National Academy of Sciences of the United States of America. 1997;94(9):4312–4317. doi: 10.1073/pnas.94.9.4312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kliewer SA, Sundseth SS, Jones SA, et al. Fatty acids and eicosanoids regulate gene expression through direct interactions with peroxisome proliferator-activated receptors α and γ . Proceedings of the National Academy of Sciences of the United States of America. 1997;94(9):4318–4323. doi: 10.1073/pnas.94.9.4318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu K, Bayona W, Kallen CB, et al. Differential activation of peroxisome proliferator-activated receptors by eicosanoids. The Journal of Biological Chemistry. 1995;270(41):23975–23983. doi: 10.1074/jbc.270.41.23975. [DOI] [PubMed] [Google Scholar]
- 20.Moraes LA, Piqueras L, Bishop-Bailey D. Peroxisome proliferator-activated receptors and inflammation. Pharmacology and Therapeutics. 2006;110(3):371–385. doi: 10.1016/j.pharmthera.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 21.Devchand PR, Keller H, Peters JM, Vazquez M, Gonzalez FJ, Wahli W. The PPARα-leukotriene B4 pathway to inflammation control. Nature. 1996;384(6604):39–43. doi: 10.1038/384039a0. [DOI] [PubMed] [Google Scholar]
- 22.Calder PC. n-3 polyunsaturated fatty acids, inflammation, and inflammatory diseases. American Journal of Clinical Nutrition. 2006;83(6):1505S–1519S. doi: 10.1093/ajcn/83.6.1505S. [DOI] [PubMed] [Google Scholar]
- 23.Calder PC. Polyunsaturated fatty acids and inflammation. Prostaglandins Leukotrienes and Essential Fatty Acids. 2006;75(3):197–202. doi: 10.1016/j.plefa.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 24.Madej A, Okopien B, Kowalski J, et al. Effects of fenofibrate on plasma cytokine concentrations in patients with atherosclerosis and hyperlipoproteinemia IIb. International Journal of Clinical Pharmacology and Therapeutics. 1998;36(6):345–349. [PubMed] [Google Scholar]
- 25.Staels B, Koenig W, Habib A, et al. Activation of human aortic smooth-muscle cells is inhibited by PPARα but not by PPARγ activators. Nature. 1998;393(6687):790–793. doi: 10.1038/31701. [DOI] [PubMed] [Google Scholar]
- 26.Marx N, Sukhova GK, Collins T, Libby P, Plutzky J. PPARα activators inhibit cytokine-induced vascular cell adhesion molecule-1 expression in human endothelial cells. Circulation. 1999;99(24):3125–3131. doi: 10.1161/01.cir.99.24.3125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meissner M, Stein M, Urbich C, et al. PPARα activators inhibit vascular endothelial growth factor receptor-2 expression by repressing Sp1-dependent DNA binding and transactivation. Circulation Research. 2004;94(3):324–332. doi: 10.1161/01.RES.0000113781.08139.81. [DOI] [PubMed] [Google Scholar]
- 28.Marx N, Kehrle B, Kohlhammer K, et al. PPAR activators as antiinflammatory mediators in human T lymphocytes: implications for atherosclerosis and transplantation-associated arteriosclerosis. Circulation Research. 2002;90(6):703–710. doi: 10.1161/01.res.0000014225.20727.8f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Delerive P, De Bosscher K, Besnard S, et al. Peroxisome proliferator-activated receptor α negatively regulates the vascular inflammatory gene response by negative cross-talk with transcription factors NF-κB and AP-1. The Journal of Biological Chemistry. 1999;274(45):32048–32054. doi: 10.1074/jbc.274.45.32048. [DOI] [PubMed] [Google Scholar]
- 30.Grau R, Punzón C, Fresno M, Iñiguez MA. Peroxisome-proliferator-activated receptor α agonists inhibit cyclo-oxygenase 2 and vascular endothelial growth factor transcriptional activation in human colorectal carcinoma cells via inhibition of activator protein-1. Biochemical Journal. 2006;395(1):81–88. doi: 10.1042/BJ20050964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mouthiers A, Baillet A, Deloménie C, Porquet D, Mejdoubi-Charef N. Peroxime proliferator-activated receptor α physically interacts with CCAAT/enhancer binding protein (C/EBPβ) to inhibit C/EBPβ-responsive α1-acid glycoprotein gene expression. Molecular Endocrinology. 2005;19(5):1135–1146. doi: 10.1210/me.2004-0188. [DOI] [PubMed] [Google Scholar]
- 32.Gervois P, Vu-Dac N, Kleemann R, et al. Negative regulation of human fibrinogen gene expression by peroxisome proliferator-activated receptor α agonists via inhibition of CCAAT box/enhancer-binding protein β . The Journal of Biological Chemistry. 2001;276(36):33471–33477. doi: 10.1074/jbc.M102839200. [DOI] [PubMed] [Google Scholar]
- 33.Shipley JM, Waxman DJ. Down-regulation of STAT5b transcriptional activity by ligand-activated peroxisome proliferator-activated receptor (PPAR) α and PPARγ . Molecular Pharmacology. 2003;64(2):355–364. doi: 10.1124/mol.64.2.355. [DOI] [PubMed] [Google Scholar]
- 34.Delerive P, Martin-Nizard F, Chinetti G, et al. Peroxisome proliferator-activated receptor activators inhibit thrombin- induced endothelin-1 production in human vascular endothelial cells by inhibiting the activator protein-1 signaling pathway. Circulation Research. 1999;85(5):394–402. doi: 10.1161/01.res.85.5.394. [DOI] [PubMed] [Google Scholar]
- 35.Desreumaux P, Dubuquoy L, Nutten S, et al. Attenuation of colon inflammation through activators of the retinoid X receptor (RXR)/peroxisome proliferator-activated receptor γ (PPARγ) heterodimer: a basis for new therapeutic strategies. Journal of Experimental Medicine. 2001;193(7):827–838. doi: 10.1084/jem.193.7.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Irukayama-Tomobe Y, Miyauchi T, Sakai S, et al. Endothelin-1-induced cardiac hyperthrophy is inhibited by activation of peroxisome proliferator-activated receptor-α partly via blockade of c-Jun NH2-terminal kinase pathway. Circulation. 2004;109(7):904–910. doi: 10.1161/01.CIR.0000112596.06954.00. [DOI] [PubMed] [Google Scholar]
- 37.Peters JM, Cheung C, Gonzalez FJ. Peroxisome proliferator-activated receptor-α and liver cancer: where do we stand? Journal of Molecular Medicine. 2005;83(10):774–785. doi: 10.1007/s00109-005-0678-9. [DOI] [PubMed] [Google Scholar]
- 38.Reddy JK, Azarnoff DL, Hignite CE. Hypolipidaemic hepatic peroxisome proliferators form a novel class of chemical carcinogens. Nature. 1980;283(5745):397–398. doi: 10.1038/283397a0. [DOI] [PubMed] [Google Scholar]
- 39.Lee SS, Pineau T, Drago J, et al. Targeted disruption of the α isoform of the peroxisome proliferator-activated receptor gene in mice results in abolishment of the pleiotropic effects of peroxisome proliferators. Molecular and Cellular Biology. 1995;15(6):3012–3022. doi: 10.1128/mcb.15.6.3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Frick MH, Elo O, Haapa K, et al. Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart disease. The New England Journal of Medicine. 1987;317(20):1237–1245. doi: 10.1056/NEJM198711123172001. [DOI] [PubMed] [Google Scholar]
- 41.Gariot P, Barrat E, Mejean L, Pointel JP, Drouin P, Debry G. Fenofibrate and human liver. Lack of proliferation of peroxisomes. Archives of Toxicology. 1983;53(2):151–163. doi: 10.1007/BF00302723. [DOI] [PubMed] [Google Scholar]
- 42.Ashby J, Brady A, Elcombe CR, et al. Mechanistically-based human hazard assessment of peroxisome proliferator-induced hepatocarcinogenesis. Human and Experimental Toxicology. 1994;13(supplement 2):S1–S117. doi: 10.1177/096032719401300201. [DOI] [PubMed] [Google Scholar]
- 43.Chevalier S, Roberts RA. Perturbation of rodent hepatocyte growth control by nongenotoxic hepatocarcinogens: mechanisms and lack of relevance for human health. Oncology Reports. 1998;5(6):1319–1327. doi: 10.3892/or.5.6.1319. [DOI] [PubMed] [Google Scholar]
- 44.Gonzalez FJ, Shah YM. PPARα: mechanism of species differences and hepatocarcinogenesis of peroxisome proliferators. Toxicology. 2008;246(1):2–8. doi: 10.1016/j.tox.2007.09.030. [DOI] [PubMed] [Google Scholar]
- 45.Lawrence JW, Li Y, Chen S, et al. Differential gene regulation in human versus rodent hepatocytes by peroxisome proliferator-activated receptor (PPAR) α. PPARα fails to induce peroxisome proliferation-associated genes in human cells independently of the level of receptor expression. The Journal of Biological Chemistry. 2001;276(34):31521–31527. doi: 10.1074/jbc.M103306200. [DOI] [PubMed] [Google Scholar]
- 46.Palmer CNA, Hsu M-H, Griffin KJ, Raucy JL, Johnson EF. Peroxisome proliferator activated receptor-α expression in human liver. Molecular Pharmacology. 1998;53(1):14–22. [PubMed] [Google Scholar]
- 47.Collett GP, Betts AM, Johnson MI, et al. Peroxisome proliferator-activated receptor α is an androgen-responsive gene in human prostate and is highly expressed in prostatic adenocarcinoma. Clinical Cancer Research. 2000;6(8):3241–3248. [PubMed] [Google Scholar]
- 48.Suchanek KM, May FJ, Robinson JA, et al. Peroxisome proliferator-activated receptor α in the human breast cancer cell lines MCF-7 and MDA-MB-231. Molecular Carcinogenesis. 2002;34(4):165–171. doi: 10.1002/mc.10061. [DOI] [PubMed] [Google Scholar]
- 49.Panigrahy D, Kaipainen A, Huang S, et al. PPARα agonist fenofibrate suppresses tumor growth through direct and indirect angiogenesis inhibition. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(3):985–990. doi: 10.1073/pnas.0711281105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jackson L, Wahli W, Michalik L, et al. Potential role for peroxisome proliferator activated receptor (PPAR) in preventing colon cancer. Gut. 2003;52(9):1317–1322. doi: 10.1136/gut.52.9.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Segawa Y, Yoshimura R, Hase T, et al. Expression of peroxisome proliferator-activated receptor (PPAR) in human prostate cancer. The Prostate. 2002;51(2):108–116. doi: 10.1002/pros.10058. [DOI] [PubMed] [Google Scholar]
- 52.Hase T, Yoshimura R, Mitsuhashi M, et al. Expression of peroxisome proliferator-activated receptors in human testicular cancer and growth inhibition by its agonists. Urology. 2002;60(3):542–547. doi: 10.1016/s0090-4295(02)01747-8. [DOI] [PubMed] [Google Scholar]
- 53.Yoshimura R, Matsuyama M, Segawa Y, et al. Expression of peroxisome proliferator-activated receptors (PPARs) in human urinary bladder carcinoma and growth inhibition by its agonists. International Journal of Cancer. 2003;104(5):597–602. doi: 10.1002/ijc.10980. [DOI] [PubMed] [Google Scholar]
- 54.Urbanska K, Pannizzo P, Grabacka M, et al. Activation of PPARα inhibits IGF-I-mediated growth and survival responses in medulloblastoma cell lines. International Journal of Cancer. 2008;123(5):1015–1024. doi: 10.1002/ijc.23588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Muzio G, Maggiora M, Trombetta A, et al. Mechanisms involved in growth inhibition induced by clofibrate in hepatoma cells. Toxicology. 2003;187(2-3):149–159. doi: 10.1016/s0300-483x(03)00055-6. [DOI] [PubMed] [Google Scholar]
- 56.Grabacka M, Plonka PM, Urbanska K, Reiss K. Peroxisome proliferator-activated receptor α activation decreases metastatic potential of melanoma cells in vitro via down-regulation of Akt. Clinical Cancer Research. 2006;12(10):3028–3036. doi: 10.1158/1078-0432.CCR-05-2556. [DOI] [PubMed] [Google Scholar]
- 57.Saidi SA, Holland CM, Charnock-Jones DS, Smith SK. In vitro and in vivo effects of the PPAR-alpha agonists fenofibrate and retinoic acid in endometrial cancer. Molecular Cancer. 2006;5, article 13:1–14. doi: 10.1186/1476-4598-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shigeto T, Yokoyama Y, Xin B, Mizunuma H. Peroxisome proliferator-activated receptor α and γ ligands inhibit the growth of human ovarian cancer. Oncology Reports. 2007;18(4):833–840. [PubMed] [Google Scholar]
- 59.Yokoyama Y, Xin B, Shigeto T, et al. Clofibric acid, a peroxisome proliferator-activated receptor α ligand, inhibits growth of human ovarian cancer. Molecular Cancer Therapeutics. 2007;6(4):1379–1386. doi: 10.1158/1535-7163.MCT-06-0722. [DOI] [PubMed] [Google Scholar]
- 60.Tanaka T, Kohno H, Yoshitani S, et al. Ligands for peroxisome proliferator-activated receptors α and γ inhibit chemically induced colitis and formation of aberrant crypt foci in rats. Cancer Research. 2001;61(6):2424–2428. [PubMed] [Google Scholar]
- 61.Maggiora M, Bologna M, Cerù MP, et al. An overview of the effect of linoleic and conjugated-linoleic acids on the growth of several human tumor cell lines. International Journal of Cancer. 2004;112(6):909–919. doi: 10.1002/ijc.20519. [DOI] [PubMed] [Google Scholar]
- 62.Thuillier P, Anchiraico GJ, Nickel KP, et al. Activators of peroxisome proliferator-activated receptor-α partially inhibit mouse skin tumor promotion. Molecular Carcinogenesis. 2000;29(3):134–142. doi: 10.1002/1098-2744(200011)29:3<134::aid-mc2>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 63.Grabacka M, Placha W, Plonka PM, et al. Inhibition of melanoma metastases by fenofibrate. Archives of Dermatological Research. 2004;296(2):54–58. doi: 10.1007/s00403-004-0479-y. [DOI] [PubMed] [Google Scholar]
- 64.Goetze S, Eilers F, Bungenstock A, et al. PPAR activators inhibit endothelial cell migration by targeting Akt. Biochemical and Biophysical Research Communications. 2002;293(5):1431–1437. doi: 10.1016/S0006-291X(02)00385-6. [DOI] [PubMed] [Google Scholar]
- 65.Varet J, Vincent L, Mirshahi P, et al. Fenofibrate inhibits angiogenesis in vitro and in vivo. Cellular and Molecular Life Sciences. 2003;60(4):810–819. doi: 10.1007/s00018-003-2322-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pozzi A, Ibanez MR, Gatica AE, et al. Peroxisomal proliferator-activated receptor-α-dependent inhibition of endothelial cell proliferation and tumorigenesis. The Journal of Biological Chemistry. 2007;282(24):17685–17695. doi: 10.1074/jbc.M701429200. [DOI] [PubMed] [Google Scholar]
- 67.Kaipainen A, Kieran MW, Huang S, et al. PPARα deficiency in inflammatory cells suppresses tumor growth. PLoS ONE. 2007;2(2):e260 pages. doi: 10.1371/journal.pone.0000260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.de Visser KE, Eichten A, Coussens LM. Paradoxical roles of the immune system during cancer development. Nature Reviews Cancer. 2006;6(1):24–37. doi: 10.1038/nrc1782. [DOI] [PubMed] [Google Scholar]
- 69.Prestwich RJ, Errington F, Hatfield P, et al. The immune system—is it relevant to cancer development, progression and treatment? Clinical Oncology. 2008;20(2):101–112. doi: 10.1016/j.clon.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 70.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mantovani A, Romero P, Palucka AK, Marincola FM. Tumour immunity: effector response to tumour and role of the microenvironment. The Lancet. 2008;371(9614):771–783. doi: 10.1016/S0140-6736(08)60241-X. [DOI] [PubMed] [Google Scholar]
- 72.Aggarwal BB, Shishodia S, Sandur SK, Pandey MK, Sethi G. Inflammation and cancer: how hot is the link? Biochemical Pharmacology. 2006;72(11):1605–1621. doi: 10.1016/j.bcp.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 73.Shiff SJ, Shivaprasad P, Santini DL. Cyclooxygenase inhibitors: drugs for cancer prevention. Current Opinion in Pharmacology. 2003;3(4):352–361. doi: 10.1016/s1471-4892(03)00087-0. [DOI] [PubMed] [Google Scholar]
- 74.Thun MJ, Henley SJ, Patrono C. Nonsteroidal anti-inflammatory drugs as anticancer agents: mechanistic, pharmacologic, and clinical issues. Journal of the National Cancer Institute. 2002;94(4):252–266. doi: 10.1093/jnci/94.4.252. [DOI] [PubMed] [Google Scholar]
- 75.Chen YQ, Edwards IJ, Kridel SJ, Thornburg T, Berquin IM. Dietary fat-gene interactions in cancer. Cancer and Metastasis Reviews. 2007;26(3-4):535–551. doi: 10.1007/s10555-007-9075-x. [DOI] [PubMed] [Google Scholar]
- 76.Escrich E, Moral R, Grau L, Costa I, Solanas M. Molecular mechanisms of the effects of olive oil and other dietary lipids on cancer. Molecular Nutrition and Food Research. 2007;51(10):1279–1292. doi: 10.1002/mnfr.200700213. [DOI] [PubMed] [Google Scholar]
- 77.Morita I. Distinct functions of COX-1 and COX-2. Prostaglandins & Other Lipid Mediators. 2002;68-69:165–175. doi: 10.1016/s0090-6980(02)00029-1. [DOI] [PubMed] [Google Scholar]
- 78.Smith WL, DeWitt DL, Garavito RM. Cyclooxygenases: structural, cellular, and molecular biology. Annual Review of Biochemistry. 2000;69:145–182. doi: 10.1146/annurev.biochem.69.1.145. [DOI] [PubMed] [Google Scholar]
- 79.Tanabe T, Tohnai N. Cyclooxygenase isozymes and their gene structures and expression. Prostaglandins & Other Lipid Mediators. 2002;68-69:95–114. doi: 10.1016/s0090-6980(02)00024-2. [DOI] [PubMed] [Google Scholar]
- 80.Simmons DL, Botting RM, Hla T. Cyclooxygenase isozymes: the biology of prostaglandin synthesis and inhibition. Pharmacological Reviews. 2004;56(3):387–437. doi: 10.1124/pr.56.3.3. [DOI] [PubMed] [Google Scholar]
- 81.Dannhardt G, Kiefer W. Cyclooxygenase inhibitors—current status and future prospects. European Journal of Medicinal Chemistry. 2001;36(2):109–126. doi: 10.1016/s0223-5234(01)01197-7. [DOI] [PubMed] [Google Scholar]
- 82.Marnett LJ. Recent developments in cyclooxygenase inhibition. Prostaglandins & Other Lipid Mediators. 2002;68-69:153–164. doi: 10.1016/s0090-6980(02)00027-8. [DOI] [PubMed] [Google Scholar]
- 83.Subbaramaiah K, Dannenberg AJ. Cyclooxygenase 2: a molecular target for cancer prevention and treatment. Trends in Pharmacological Sciences. 2003;24(2):96–102. doi: 10.1016/S0165-6147(02)00043-3. [DOI] [PubMed] [Google Scholar]
- 84.Eberhart CE, Coffey RJ, Radhika A, Giardiello FM, Ferrenbach S, Dubois RN. Up-regulation of cyclooxygenase 2 gene expression in human colorectal adenomas and adenocarcinomas. Gastroenterology. 1994;107(4):1183–1188. doi: 10.1016/0016-5085(94)90246-1. [DOI] [PubMed] [Google Scholar]
- 85.Marnett LJ, DuBois RN. COX-2: a target for colon cancer prevention. Annual Review of Pharmacology and Toxicology. 2002;42:55–80. doi: 10.1146/annurev.pharmtox.42.082301.164620. [DOI] [PubMed] [Google Scholar]
- 86.Huls G, Koornstra JJ, Kleibeuker JH. Non-steroidal anti-inflammatory drugs and molecular carcinogenesis of colorectal carcinomas. The Lancet. 2003;362(9379):230–232. doi: 10.1016/s0140-6736(03)13915-3. [DOI] [PubMed] [Google Scholar]
- 87.Gupta RA, DuBois RN. Colorectal cancer prevention and treatment by inhibition of cyclooxygenase-2. Nature Reviews Cancer. 2001;1(1):11–21. doi: 10.1038/35094017. [DOI] [PubMed] [Google Scholar]
- 88.Kawamori T, Rao CV, Seibert K, Reddy BS. Chemopreventive activity of celecoxib, a specific cyclooxygenase-2 inhibitor, against colon carcinogenesis. Cancer Research. 1998;58(3):409–412. [PubMed] [Google Scholar]
- 89.Gately S. The contributions of cyclooxygenase-2 to tumor angiogenesis. Cancer and Metastasis Reviews. 2000;19(1-2):19–27. doi: 10.1023/a:1026575610124. [DOI] [PubMed] [Google Scholar]
- 90.Iñiguez MA, Rodríguez A, Volpert OV, Fresno M, Redondo JM. Cyclooxygenase-2: a therapeutic target in angiogenesis. Trends in Molecular Medicine. 2003;9(2):73–78. doi: 10.1016/s1471-4914(02)00011-4. [DOI] [PubMed] [Google Scholar]
- 91.Tegeder I, Pfeilschifter J, Geisslinger G. Cyclooxygenase-independent actions of cyclooxygenase inhibitors. The FASEB Journal. 2001;15(12):2057–2072. doi: 10.1096/fj.01-0390rev. [DOI] [PubMed] [Google Scholar]
- 92.Jaradat MS, Wongsud B, Phornchirasilp S, et al. Activation of peroxisome proliferator-activated receptor isoforms and inhibition of prostaglandin H2 synthases by ibuprofen, naproxen, and indomethacin. Biochemical Pharmacology. 2001;62(12):1587–1595. doi: 10.1016/s0006-2952(01)00822-x. [DOI] [PubMed] [Google Scholar]
- 93.Lehmann JM, Lenhard JM, Oliver BB, Ringold GM, Kliewer SA. Peroxisome proliferator-activated receptors α and γ are activated by indomethacin and other non-steroidal anti-inflammatory drugs. The Journal of Biological Chemistry. 1997;272(6):3406–3410. doi: 10.1074/jbc.272.6.3406. [DOI] [PubMed] [Google Scholar]
- 94.Combs CK, Bates P, Karlo JC, Landreth GE. Regulation of β-amyloid stimulated proinflammatory responses by peroxisome proliferator-activated receptor α . Neurochemistry International. 2001;39(5-6):449–457. doi: 10.1016/s0197-0186(01)00052-3. [DOI] [PubMed] [Google Scholar]
- 95.Yu J, Ip E, Dela Peña A, et al. COX-2 induction in mice with experimental nutritional steatohepatitis: role as pro-inflammatory mediator. Hepatology. 2006;43(4):826–836. doi: 10.1002/hep.21108. [DOI] [PubMed] [Google Scholar]
- 96.Blann AD, Belgore FM, Constans J, Conri C, Lip GYH. Plasma vascular endothelial growth factor and its receptor Flt-1 in patients with hyperlipidemia and atherosclerosis and the effects of fluvastatin or fenofibrate. American Journal of Cardiology. 2001;87(10):1160–1163. doi: 10.1016/s0002-9149(01)01486-2. [DOI] [PubMed] [Google Scholar]
- 97.Hanahan D, Folkman J. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell. 1996;86(3):353–364. doi: 10.1016/s0092-8674(00)80108-7. [DOI] [PubMed] [Google Scholar]
- 98.Folkman J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nature Medicine. 1995;1(1):27–31. doi: 10.1038/nm0195-27. [DOI] [PubMed] [Google Scholar]
- 99.Carmeliet P, Jain RK. Angiogenesis in cancer and other diseases. Nature. 2000;407(6801):249–257. doi: 10.1038/35025220. [DOI] [PubMed] [Google Scholar]
- 100.Bergers G, Benjamin LE. Tumorigenesis and the angiogenic switch. Nature Reviews Cancer. 2003;3(6):401–410. doi: 10.1038/nrc1093. [DOI] [PubMed] [Google Scholar]
- 101.Liao D, Johnson RS. Hypoxia: a key regulator of angiogenesis in cancer. Cancer and Metastasis Reviews. 2007;26(2):281–290. doi: 10.1007/s10555-007-9066-y. [DOI] [PubMed] [Google Scholar]
- 102.Hickey MM, Simon MC. Regulation of angiogenesis by hypoxia and hypoxia-inducible factors. Current Topics in Developmental Biology. 2006;76:217–257. doi: 10.1016/S0070-2153(06)76007-0. [DOI] [PubMed] [Google Scholar]
- 103.Weidemann A, Johnson RS. Biology of HIF-1α . Cell Death and Differentiation. 2008;15(4):621–627. doi: 10.1038/cdd.2008.12. [DOI] [PubMed] [Google Scholar]
- 104.Kaidi A, Qualtrough D, Williams AC, Paraskeva C. Direct transcriptional up-regulation of cyclooxygenase-2 by hypoxia-inducible factor (HIF)-1 promotes colorectal tumor cell survival and enhances HIF-1 transcriptional activity during hypoxia. Cancer Research. 2006;66(13):6683–6691. doi: 10.1158/0008-5472.CAN-06-0425. [DOI] [PubMed] [Google Scholar]
- 105.Simiantonaki N, Jayasinghe C, Michel-Schmidt R, Peters K, Hermanns MI, Kirkpatrick CJ. Hypoxia-induced epithelial VEGF-C/VEGFR-3 upregulation in carcinoma cell lines. International Journal of Oncology. 2008;32(3):585–592. [PubMed] [Google Scholar]
- 106.Pichiule P, Chavez JC, LaManna JC. Hypoxic regulation of angiopoietin-2 expression in endothelial cells. The Journal of Biological Chemistry. 2004;279(13):12171–12180. doi: 10.1074/jbc.M305146200. [DOI] [PubMed] [Google Scholar]
- 107.Rankin EB, Giaccia AJ. The role of hypoxia-inducible factors in tumorigenesis. Cell Death and Differentiation. 2008;15(4):678–685. doi: 10.1038/cdd.2008.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ferrara N. VEGF: an update on biological and therapeutic aspects. Current Opinion in Biotechnology. 2000;11(6):617–624. doi: 10.1016/s0958-1669(00)00153-1. [DOI] [PubMed] [Google Scholar]
- 109.Cross MJ, Claesson-Welsh L. FGF and VEGF function in angiogenesis: signalling pathways, biological responses and therapeutic inhibition. Trends in Pharmacological Sciences. 2001;22(4):201–207. doi: 10.1016/s0165-6147(00)01676-x. [DOI] [PubMed] [Google Scholar]
- 110.Ho QT, Kuo CJ. Vascular endothelial growth factor: biology and therapeutic applications. International Journal of Biochemistry and Cell Biology. 2007;39(7-8):1349–1357. doi: 10.1016/j.biocel.2007.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ferrara N, Gerber H-P, LeCouter J. The biology of VEGF and its receptors. Nature Medicine. 2003;9(6):669–676. doi: 10.1038/nm0603-669. [DOI] [PubMed] [Google Scholar]
- 112.Shibuya M, Claesson-Welsh L. Signal transduction by VEGF receptors in regulation of angiogenesis and lymphangiogenesis. Experimental Cell Research. 2006;312(5):549–560. doi: 10.1016/j.yexcr.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 113.Shibuya M, Ito N, Claesson-Welsh L. Structure and function of vascular endothelial growth factor receptor-1 and -2. Current Topics in Microbiology and Immunology. 1999;237:59–83. doi: 10.1007/978-3-642-59953-8_4. [DOI] [PubMed] [Google Scholar]
- 114.Griffioen AW, Molema G. Angiogenesis: potentials for pharmacologic intervention in the treatment of cancer, cardiovascular diseases, and chronic inflammation. Pharmacological Reviews. 2000;52(2):237–268. [PubMed] [Google Scholar]
- 115.Kasai T, Miyauchi K, Yokoyama T, Aihara K, Daida H. Efficacy of peroxisome proliferative activated receptor (PPAR)-α ligands, fenofibrate, on intimal hyperplasia and constrictive remodeling after coronary angioplasty in porcine models. Atherosclerosis. 2006;188(2):274–280. doi: 10.1016/j.atherosclerosis.2005.10.047. [DOI] [PubMed] [Google Scholar]