Abstract
Background
Cellular redox state is important to cell growth and death. The growth of tumor cells may be modulated by intracellular reduced glutathione/oxidized glutathione (GSH/GSSG). The present study aims to investigate the effects of ginsenosides Re and Rg3 on cellular redox state and cell proliferation in C6 glioma cells.
Methods
Cultured C6 glioma cells were exposed to various concentrations of either Rg3 or Re for 24 hours. Cell growth and death were measured by the BrdU incorporation assay and the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay respectively. Cellular redox state was determined by free radical production using flow cytometry and GSH/GSSG using spectrofluorometry.
Results
At a sub-lethal concentration, Re suppressed cell proliferation with a significant decrease in BrdU incorporation. Re did not increase reactive oxygen species (ROS) production but increased GSH/GSSG via increased activity of gamma glutamylcystenyl synthase (γ-GCS). In contrast, Rg3 increased free radical production and reduced GSH/GSSG. The effects of Rg3 were probably due to increased activity of glutathione peroxidase (GPx).
Conclusion
Re and Rg3 alter cellular redox state of C6 glioma cells in opposite directions. Changes in cellular redox state induced by Re and Rg3 are correlated with the proliferation rates of C6 glioma cells.
Background
Cellular redox state can be monitored by intracellular thiol levels, among which the ratio of reduced glutathione (GSH) and oxidized glutathione (GSSG) is the most useful [1,2]. In the presence of free radicals, mainly H2O2, GSH acts as electron donor and is oxidized into GSSG by glutathione peroxidase (GPx). The GSSG generated is later converted back to GSH by glutathione reductase (GR) in which reduced nicotinamide adenine dinucleotide phosphate (NADPH) is the hydrogen donor. In living tissues, the level of glutathione is ranged 5–10 mM. In cultured cells, the level of intracellular glutathione is several folds higher than the level of total adenosine nucleotides [3]. Under stable conditions, cells maintain a constant ratio of GSH/GSSG [1,4,5]. Excessive reactive oxygen species (ROS) decreases the GSH/GSSG ratio [6]. The GSH/GSSG ratio is increased by the addition of N-acetylcysteine (NAC, a cysteine analogue) [7] or by improved enzymes for glutathione synthesis [8]. Antioxidants or molecules that increase the GSH/GSSG ratio suppress cell proliferation [9-14], while oxidative stress increases cell proliferation and leads to cell death [2,15-19]. Cellular redox state also affects cellular signaling pathways, gene expression and enzymes associated with cell cycle progression [2,6,11,12,15,16,18,19]. Conour et al. identified 92 candidate proteins involved in cell cycle progression that are redox sensitive [20]. Growth and metastasis of tumor cells may also be regulated by intracellular redox state [2,17,21,22].
Ginseng (Panax ginseng, Renshen) is a popular Chinese herbal medicine known for its wide spectrum of pharmacological actions [23]. Ginseng is composed of a series of saponins known as ginsenosides which are derivatives of triterpene dammarane. There are two categories of ginsenosides, namely protopanaxadiol (PPD, e.g. Ra, Rb, Rc, Rd, Rg3, Rh2) and protopanaxatriol (PPT, e.g. Re, Rf, Rg1, Rg2, Rh1). Each gensenoside is characteristic in its sugar moiety position on dammarane. Some ginsenosides modulate cardiovascular and neurological functions [24], whereas others act as antioxidants [25-29] to prevent cancer [30-32], protect against chemically induced tissues damage [33-36] and delay ageing [25]. Ginsenoside Re has anti-oxidative abilities apart from its immunomodulatory, antihyperlipidemic and neuroprotective activities. In cardiomyocytes, pretreatment with Re significantly attenuates H2O2 induced free radical production and protect cell death [37]. Rg3 acts as a prooxidant to accelerate 2,2'-azobis (2-amidinopropane) hydrochloride (AAPH) induced haemolysis in human erythrocytes [26]. Rg3 is anti-angiogenic and anticancer through inducing apoptosis [30,38].
Ginsenosides are active components in ginseng which has anticancer properties [23,32,39-41]. The present study investigates how Re and Rg3 suppress the growth of C6 glioma cells. The C6 glioma cell is a model for studying a form of malignant brain tumor glioblastoma multiform [42]. The study also investigates the mechanisms through which ginsenosides Re and Rg3 modulate the levels of oxidized and reduced glutathione, and ROS production
Methods
Materials
Cell culture media and all reagents for biochemical assays were purchased from Sigma Chemical (MO, USA). Perchloric acid (PCA) and potassium hydroxide were purchased from Fisher Scientific (NJ, USA). Antibiotics were purchased from Life Technologies (NY, USA). Fetal bovine serum (FBS) and 6-carboxy-2,7-dichlorodihydrofluorescein diacetate (H2DCFDA) were purchased from Invitrogen (Scotland, UK) and Molecular Probes (NJ, USA) respectively.
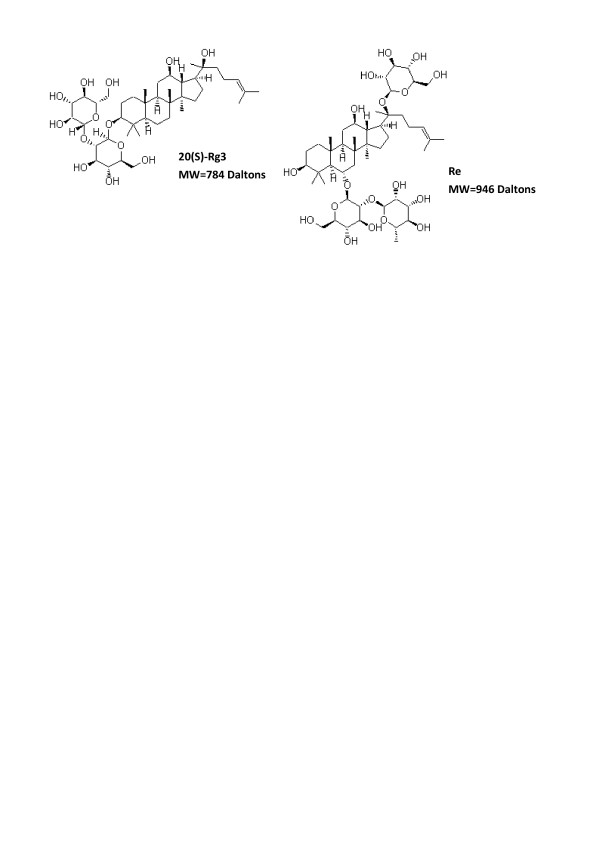
Ginsenosides Re and Rg3 (purity>99%) were obtained from International laboratory (USA). The identities of ginsenosdies were confirmed by high-performance liquid chromatography (HPLC) and electrospray ionization – mass spectrometry (ESI-MS). The Rg3, a 20(S) isoform, and the Re were 784 Daltons and 946 Daltons of molecular weight respectively (Figure 1). In this study, the concentration of ginsenosides was based on nominal weight. The ginsenosides were dissolved in dimethyl sulfoxide (DMSO), filtered (0.2 μm membrane) and added to the culture media to achieve various final concentrations.
Figure 1.
Chemical structures of ginsenosides Re and Rg3 (adapted from chemBlink http://www.chemblink.com/).
Buthionine-(S, R)-sulfoximine (BSO), an inhibitor of gamma glutamylcystenyl synthase (γ-GCS), was dissolved in phosphate buffered saline (PBS) and sterilized through a 0.2 μm membrane. Cultured C6 glioma cells (ATCC no CCL-107) were purchased from the American Type Culture Collection (USA).
Cell culture
The cells were maintained in the F-12 medium supplemented with 10% FBS (tested for lipopolysaccharide) and 0.5% antibiotics (amphotericin B and penicillin-streptomycin) in a humidifier under 95% air and 5% CO2 at 37°C.
Treatment of cells
Cells were sub-cultured into 6-well plates until confluence. The incubation media were then removed and replaced with those containing the required concentration of Rg3 or Re. The concentration of DMSO in each well was kept at 0.5%, which did not affect intracellular glutathione level and GSH/GSSG. Cells were treated with 100 μM BSO for 24 hours for the study of cell response in the absence of GSH.
Analysis of cell viability
The viability of C6 glioma cells treated with Re and Rg3 was determined by the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. Briefly, cells were cultured in 96-well plates and treated with various concentrations (0–800 μg/ml) of Re or Rg3. After incubation, cells were washed twice with PBS. A medium (100 μl) containing 500 μg/ml MTT was added to each well. The medium was removed after 3 hours of incubation and DMSO (100 μl) was added to dissolve the formazan crystals. Light absorbance at 595 nm was measured with a microplate reader (Tecan Infinite F200, Germany). Cell viability was the optical density ratio of a treated culture over an untreated control.
Cell proliferation assay
The effects of either Re or Rg3 on cell proliferation were determined by the BrdU cell proliferation kit (Calbiochem, Germany). Cells were cultured in 96-well plates. Upon confluence, they were incubated with either Re or Rg3 of various concentrations for 24 hours. BrdU was added to the medium 20 hours before the end of incubation. The amount of BrdU incorporated into cells was determined by binding BrdU to mouse anti-BrdU antibody conjugated with horseradish peroxidase. Tetra-methylbenzidine, the substrate of horseradish peroxidase, was later added. The color product of the enzymatic reaction was measured in a microplate reader (Tecan Infinite F200, Germany) at 450–540 nm.
Analysis of intracellular glutathione metabolism
Intracellular glutathione metabolism is reflected by the interplay of GSH, GSSG, GPx, GR and γ-GCS. Cells were incubated for 24 hours before intracellular metabolites were extracted by 0.3 M PCA containing 1 mM ethylenediamine-tetraacetic acid (EDTA) with a previously described method [43]. The levels of GSH and GSSG were determined with spectrofluorometry [3]. For enzyme assays, cells were washed twice with pre-warmed PBS and extracted with a protein extraction kit (EMB Biosciences, Calbiochem, USA) with a previously described method [8].
Analysis of ROS production by flow cytometry
Intracellular production of ROS was evaluated with H2DCFDA which is converted to a fluorescence product dichlorodihydrofluoroscine (DCF) when treated with H2O2. Cells were treated for 24 hours with either 100 μg/ml of BSO or 200 μg/ml of Re. Thirty minutes before the end of experiment, H2DCFDA was added (final concentration 10 μM). The cells were then trypsinized, centrifuged, re-suspended in PBS and passed through the FACScan flow cytometer (Becton Dickinson, U.S.A.). Fluorescence intensities of DCF were measured by excitation wavelength of 488 nm and emission wavelength of 620 nm. In each sample, approximately 10000 cells were analyzed by the CellQuest software (Becton Dickinson, U.S.A.).
Data analysis
Cellular redox state was determined by the ratio of GSH/GSSG. Each experiment was repeated 3–8 times. The means and standard deviations were calculated. The differences between samples were evaluated by the one way analysis of variance (ANOVA), followed by tests for differences between groups by a post-hoc method (Dunnett C) without an assumption of equal variance between groups (SPSS version 14). The differences with P < 0.05 were considered statistically significant.
Results
Selection of concentrations of Re and Rg3 for the study of cell proliferation
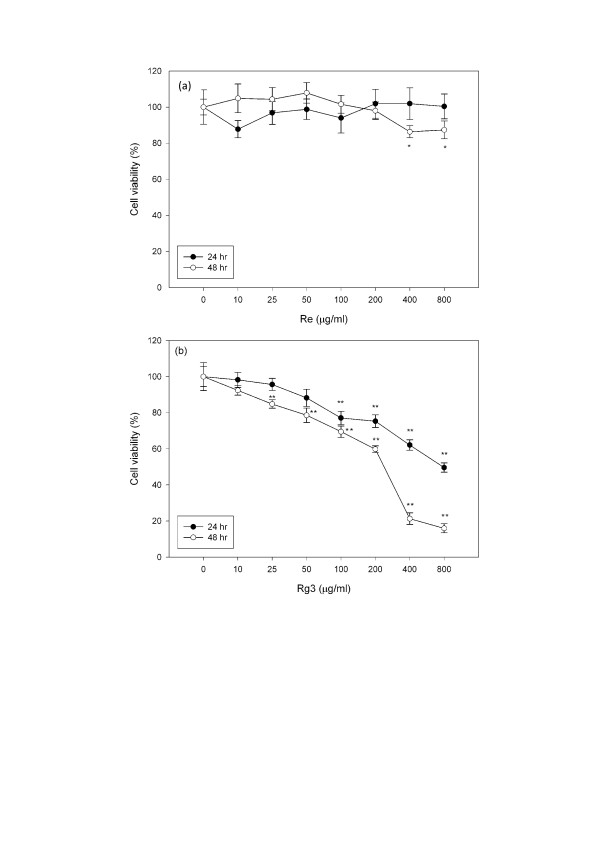
A 24 and 48 hour dose-response study was conducted. Cells were treated with various concentrations (0–800 μg/ml) of Re and Rg3. There was a significant reduction (P < 0.01) in cell viability upon treatment with 100 μg/ml of Rg3 for 24 hours (Figure 2). At 48 hours, a significant difference (P < 0.01) in cell viability was observed when Rg3 concentration was 50 μg/ml. In contrast, there was no significant change in cell viability after treatment with Re for 24 hours. At high concentrations (400 and 800 μg/ml), cell viability decreased 20% after 48 hours.
Figure 2.
Changes in cell viability of cells treated with (a) Re or (b) Rg3 for 24 and 48 hours. Each value represents the mean and standard deviation of 8 replicates. **: statistically significant (P < 0.01)
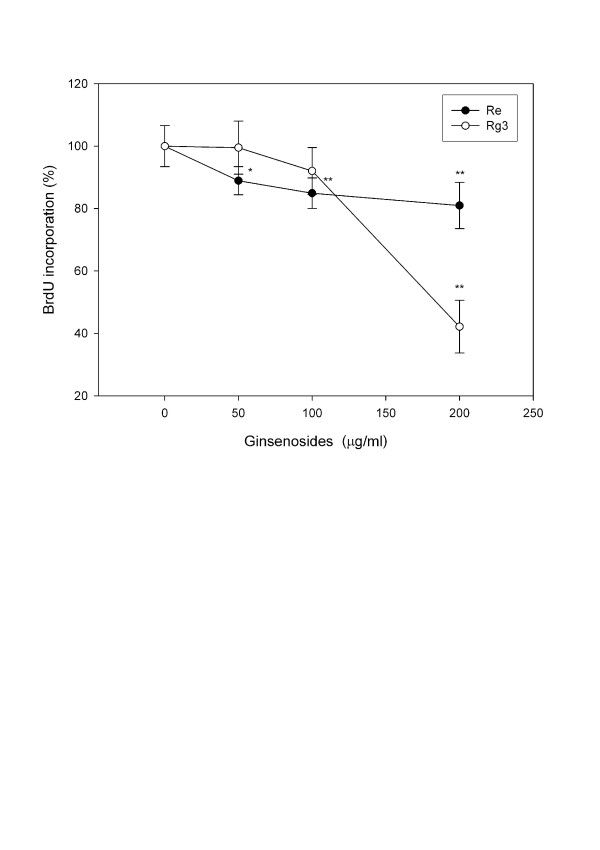
A decrease in cell proliferation was also demonstrated by decreased BrdU incorporation. While cell viability did not decrease (Figure 2a) after treatment with low concentrations of Re (50–200 μg/ml), BrdU incorporation (Figure 3) decreased 20% (P < 0.01). In contrast, Rg3 did not decrease BrdU incorporation at concentrations below 200 μg/ml at which cell viability significantly decreased (P < 0.05).
Figure 3.
BrdU incorporation assay in C6 glioma cells treated with various concentrations of Re and Rg3 for 24 hours. Each value represents the mean and standard deviation of 8 replicates. *: statistically significant (P < 0.05). **: statistically significant (P < 0.01).
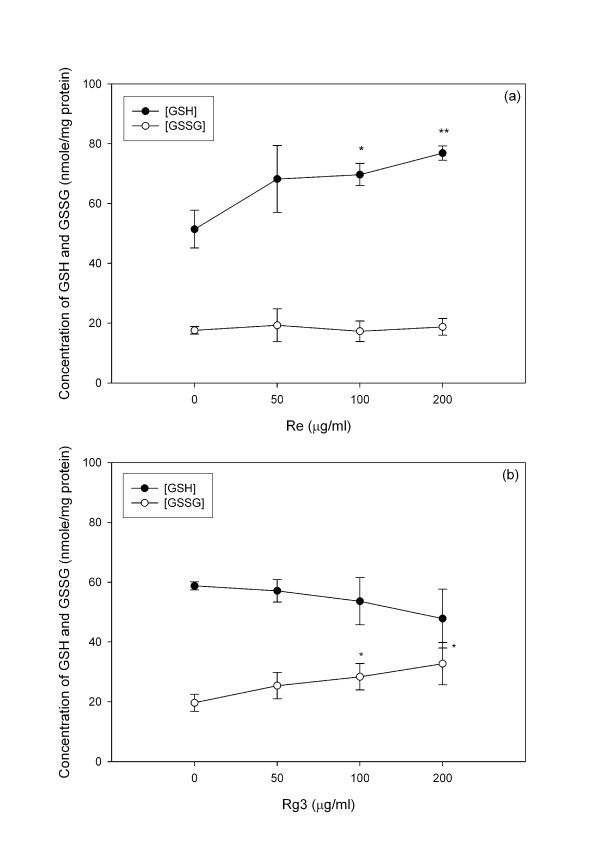
Glutathione metabolism
The resting level of GSH is three folds higher than that of GSSG. The GSH/GSSG ratio ranges from 2 (in tumor cells) to >40 (in normal cells) [44]. The GSH/GSSG ratio may be altered by either toxicants [3] or antioxidants [45]. Re treatment increased GSH but not GSSG (Figure 4a), while Rg3 increased GSSG (Figure 4b) but not GSH. Rg3 treatment decreased the GSH/GSSG ratio, while Re treatment increased it (Figure 5). A decrease in the GSH/GSSG ratio after treatment with Rg3 indicated oxidative stress. ROS production was increased after treatment with Rg3 (Figure 6). Rg3, which decreased the GSH/GSSG ratio at 200 μg/ml, also significantly increased ROS generation (Figure 6). The results show that Rg3 and Re treatments changed the intracellular GSH/GSSG ratio in opposite directions.
Figure 4.
Changes in the GSH and GSSG levels upon treatment with (a) Re or (b) Rg3 for 24 hours. Each value represents the mean and standard deviation of 4 replicates. *: statistically significant (P < 0.05). **: statistically significant (P < 0.01).
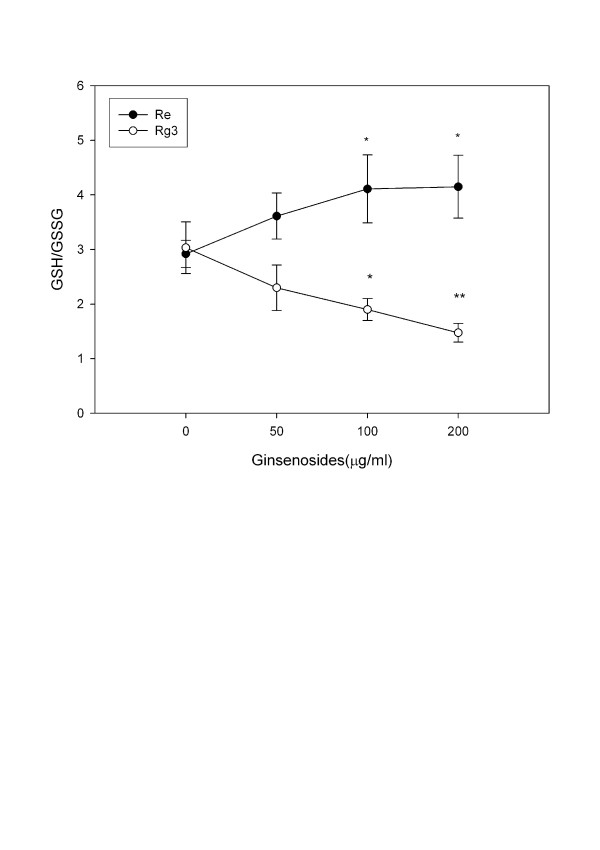
Figure 5.
Change in the GSH/GSSH ratio of C6 glioma cells treated with Re and Rg3 for 24 hours. Each value represents the mean and standard deviation of 4 replicates. *: statistically significant (P < 0.05). **: statistically significant (P < 0.01).
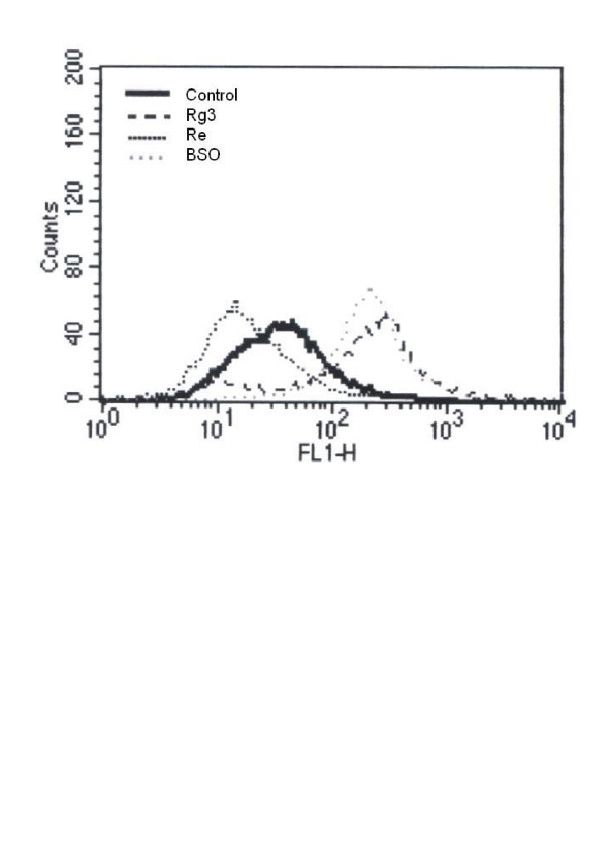
Figure 6.
Changes in the intracellular ROS level indicated by the fluorescence intensity (FLH-1) in C6 glioma cells treated with Re (200 μg/ml), Rg3 (200 μg/ml) or BSO (100 μM) for 24 hours. The cytogram represents three independent experiments. The x-axis and y-axis denote fluorescence intensity and cell count respectively.
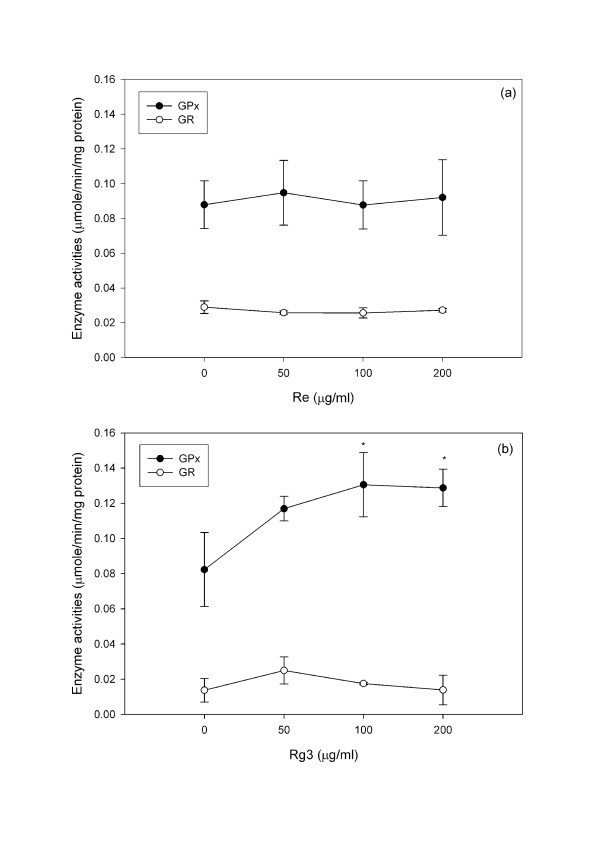
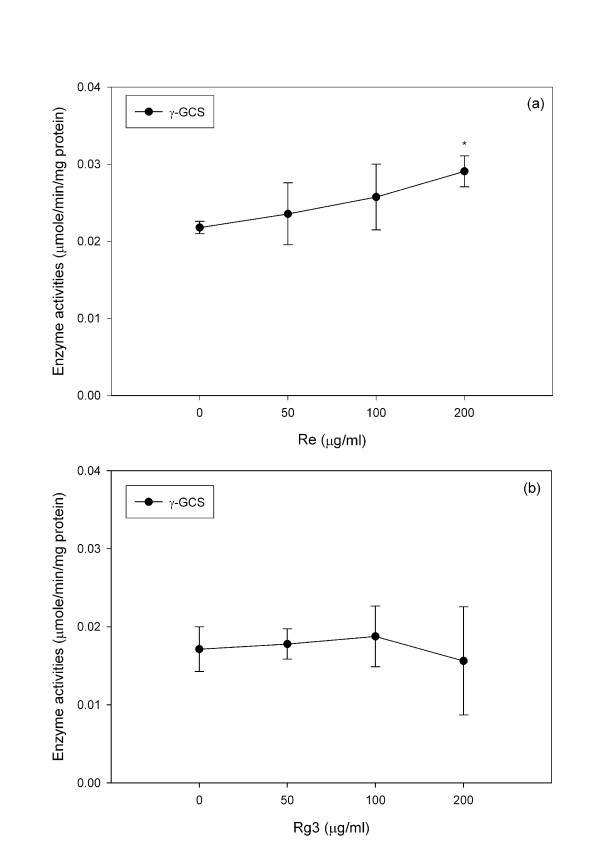
Re treatment did not significantly change the activity of either GPx or GR (Figure 7a) but increased (P < 0.05) the activity of γ-GCS, which is the rate limiting enzyme for GSH synthesis (Figure 8). Rg3 significantly increased (P < 0.05) GPx without changing GR (Figure 7b) or γ-GCS (Figure 8).
Figure 7.
Changes in the GR and GPx activities of C6 glioma cells treated with (a) Re and (b) Rg3 for 24 hours. Each value represents the mean and standard deviation of 4 replicates. *: statistically significant (P < 0.05).
Figure 8.
Changes in the γ-GCS activity of C6 glioma cells treated with Re and Rg3 for 24 hours. Each value represents the mean and standard deviation of 4 replicates. *: statistically significant (P < 0.05).
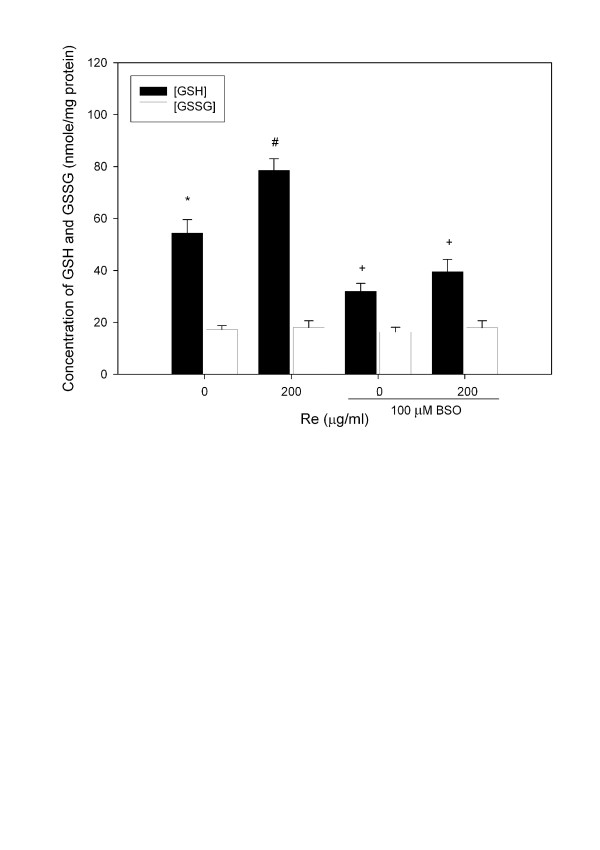
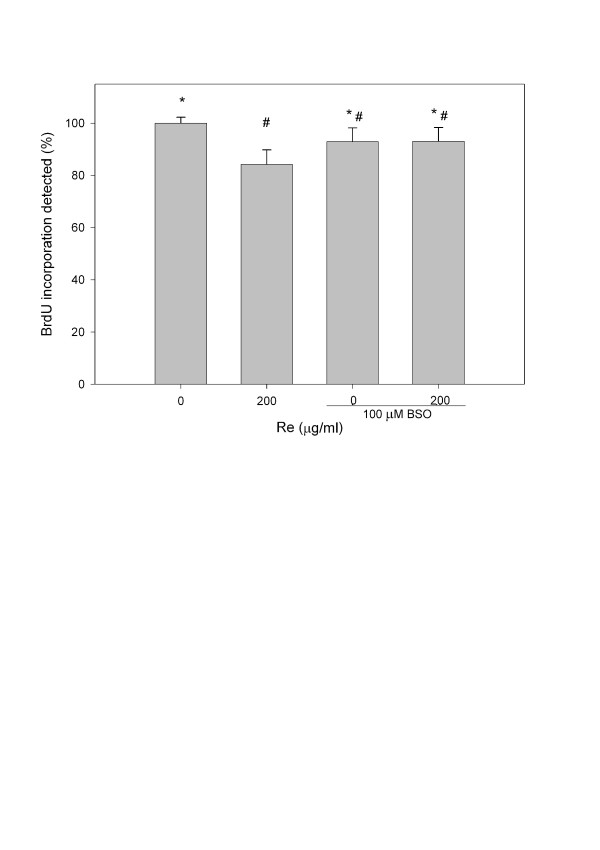
Suppreession of γ-GCS activity by BSO reverses Re induced changes
To further confirm that Re acts by changing γ-GCS activity, treatment of cells with BSO, an inhibitor of γ-GCS which could significantly lowered (P<0.01) the GSH/GSSG ratio (Figure 9) and increased (P<0.05) cellular ROS production (Figure 6), was able to reverse the Re induced change in both GSH/GSSG (Figure 9) and BrdU incorporation (Figure 10).
Figure 9.
Changes in the GSH and GSSG levels upon treatment with Re and/or BSO for 24 hours. Each value represents the mean and standard deviation of 4 replicates. Symbols indicate that the treatment groups are significantly different (P < 0.05) from each other.
Figure 10.
BrdU incorporation assay in C6 glioma cells treated with Re and BSO for 24 hours. Each value represents the mean and standard deviation of 4 replicates. Symbols indicate that the treatment groups are significantly different (P < 0.05) from each other.
Discussion
The present study showed that both Re and Rg3 affected the survival of C6 glioma cells. While Re suppressed the growth of C6 glioma cells at low concentrations, Rg3 caused death of C6 glioma cells via oxidative stress. Furthermore, we demonstrated that the action of Re was correlated with an increase in the intracellular GSH level, thereby raising the GSH/GSSG ratio. BSO (an inhibitor of γ-GCS) treatment reversed the GSH/GSSG rise induced by Re (Figure 9) and decreased BrdU incorporation in the presence of Re (Figure 10).
γ-GCS is the rate limiting enzyme in glutathione synthesis. The enzyme and its gene expression may be modulated by a number of factors. For example, an increase in the γ-GCS activity may be stimulated by oxidative metabolites. Shi et al. showed that the heavy subunit mRNA level and subsequent enzyme activity increased in response to 2,3-dimethoxy-1,4-napthoquinone (DMNQ) through transcriptional activation of γ-GCS [46]. Our previous studies showed that the production of quinone metabolite of benzo [a]pyrene activated γ-GCS [8]. However, no such quinone metabolites were detected in the metabolism of Re in biological tissues. Furthermore, the present study showed that Re treatment suppressed free radical production (Figure 6), which did not support the free radical production hypothesis in γ-GCS activation. Another study showed that PC12 cells' tolerance of 7-hydroxycholesterol and 15-deoxy-12,13- prostaglandin J2 was achieved via up-regulation of cellular glutathione by γ-GCS transcription [47]. Such feedback activation may be an underlying cause of cellular adaptation to oxidative stress. Therefore, similar adaptive response may take place in C6 glioma cells following Re treatment.
A number of factors must be considered before using Re to treat brain tumor. Firstly, Re suppresses cell proliferation at a low rate. At a low concentration of 50 μg/ml, Re was effective in suppressing cell proliferation (Figure 3). However, there was only a 10% decrease in BrdU uptake after 24 hours (Figure 2a), and only a 20% decrease in cell viability after 48 hours. Secondly, Re is metabolized by intestinal flora via deglycosylation and fatty acid esterification [48], which may limit the application of Re given per oral. Finally, it is not clear whether normal astrocytes respond similarly to Re. In current anticancer strategies, both normal and tumor cells are affected. Menon et al. demonstrated that exposure of both nonmalignant human breast epithelial (MCF-10A) and breast cancer cells (MCF-7 and MDA-MB-231) to NAC decreased the oxidation of a prooxidant-sensitive dye in MCF-10A cells, but not in MCF-7 and MDA-MB-231 cells, suggesting that malignant and non-malignant cells may have different responses to oxidative stress [17]. We will further investigate whether C6 glioma cells and normal astrocytes respond differently to Re treatment.
Conclusion
Re suppresses the growth and proliferation of C6 glioma cells and increases the cellular GSH/GSSG ratio by enhancing the γ-GCS activity, suppressing ROS generation and reducing cell proliferation rate. Rg3 causes cell death via oxidative stress. While both Re and Rg3 eliminate the growth and proliferation of C6 glioma cells, they modulate cellular redox state in opposite directions. Yue et al. suggest that ginseng or selected ginsenosides modulate cellular function via specific intracellular receptors in a way that may reflect the Ying/Yang actions of ginseng [49]. The opposite actions in modulating cellular redox state by Re and Rg3 may be another example of the Ying/Yang actions of ginseng.
Abbreviations
γ-GCS: gamma glutamylcystenyl synthase; AAPH: 2,2'-azobis (2-amidinopropane) hydrochloride; BSO: buthionine-(S, R)-sulfoximine; DMNQ: 2,3-dimethoxy-1,4-napthoquinone; DMSO: dimethyl sulfoxide; EDTA: ethylenediamine-tetraacetic acid; ESI-MS: electrospray ionization – mass spectrometry; Fetal bovine serum (FBS); GPx: glutathione peroxidase; GR: glutathione reductase; GSH: reduced glutathione; GSSG: oxidized glutathione; H2DCFDA: 6-carboxy-2,7-dichlorodihydrofluorescein diacetate; HPLC: high-performance liquid chromatography; MTT: 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide; NAC: N-acetylcysteine; NADPH: nicotinamide adenine dinucleotide phosphate; -PBS: phosphate buffered saline; Perchloric acid (PCA); PPD: protopanaxadiol; PPT: protopanaxatriol; -ROS: reactive oxygen species
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
WN is an MPhil student who carried out the experiments and helped draft the manuscript. MY supervised the study and drafted the manuscript. Both authors read and approved the final version of the manuscript.
Acknowledgments
Acknowledgements
The authors wish to thank Prof ZH Jiang, School of Chinese Medicine, Hong Kong Baptist University for the HPLC and ESI-MS analyses to confirm the ginsenosides Re and Rg3 used in this study. This study was supported by the Hong Kong Baptist University Faculty Research Grant.
Contributor Information
Wai Yee Ng, Email: 06458815@hkbu.edu.hk.
Mildred S Yang, Email: msyang@hkbu.edu.hk.
References
- Jones DP. Redox potential of GSH/GSSG couple: assay and biological significance . Methods Enzymol. 2002;348:93–112. doi: 10.1016/s0076-6879(02)48630-2. [DOI] [PubMed] [Google Scholar]
- Jonas CR, Ziegler TR, Gu LH, Jones DP. Extracellular thiol/disulfide redox state affects proliferation rate in a human colon carcinoma (Caco2) cell line . Free Radic Biol Med. 2002;33:1499–1506. doi: 10.1016/s0891-5849(02)01081-x. [DOI] [PubMed] [Google Scholar]
- Yang MS, Yu LC, Gupta RC. Analysis of changes in energy and redox states in HepG2 hepatoma and C6 glioma cells upon exposure to cadmium. Toxicology. 2004;201:105–113. doi: 10.1016/j.tox.2004.04.007. [DOI] [PubMed] [Google Scholar]
- Andersson A, Lindgren A, Arnadottir M, Prytz H, Hultberg B. Thiols as a measure of plasma redox status in healthy subjects and in patients with renal or liver failure . Clin Chem. 1999;45:1084–1086. [PubMed] [Google Scholar]
- Hultberg B, Andersson A, Isaksson A. Thiol and redox reactive agents exert different effects on glutathione metabolism in HeLa cell cultures . Clin Chim Acta. 1999;283:21–32. doi: 10.1016/s0009-8981(99)00028-5. [DOI] [PubMed] [Google Scholar]
- Menon SG, Goswami PC. A redox cycle within the cell cycle: ring in the old with the new . Oncogene. 2007;26:1101–1109. doi: 10.1038/sj.onc.1209895. [DOI] [PubMed] [Google Scholar]
- De Flora S, Izzotti A, D'Agostini F, Balansky RM. Mechanisms of N-acetylcysteine in the prevention of DNA damage and cancer, with special reference to smoking-related end-points. Carcinogenesis. 2001;22:999–1013. doi: 10.1093/carcin/22.7.999. [DOI] [PubMed] [Google Scholar]
- Lin T, Yang MS. Benzo[a]pyrene-induced elevation of GSH level protects against oxidative stress and enhances xenobiotic detoxification in human HepG2 cells . Toxicology. 2007;235:1–10. doi: 10.1016/j.tox.2007.03.002. [DOI] [PubMed] [Google Scholar]
- Fisher JC, Kling DE, Kinane TB, Schnitzer JJ. Oxidation-reduction (redox) controls fetal hypoplastic lung growth. J Surg Res. 2002;106:287–291. doi: 10.1006/jsre.2002.6461. [DOI] [PubMed] [Google Scholar]
- Hoffman A, Spetner LM, Burke M. Cessation of cell proliferation by adjustment of cell redox potential. J Theor Biol. 2001;211:403–407. doi: 10.1006/jtbi.2001.2356. [DOI] [PubMed] [Google Scholar]
- Kim KY, Rhim T, Choi I, Kim SS. N-acetylcysteine induces cell cycle arrest in hepatic stellate cells through its reducing activity . J Biol Chem. 2001;276:40591–40598. doi: 10.1074/jbc.M100975200. [DOI] [PubMed] [Google Scholar]
- Menon SG, Sarsour EH, Spitz DR, Higashikubo R, Sturm M, Zhang H, Goswami PC. Redox regulation of the G1 to S phase transition in the mouse embryo fibroblast cell cycle . Cancer Res. 2003;63:2109–2117. [PubMed] [Google Scholar]
- Nkabyo YS, Ziegler TR, Gu LH, Watson WH, Jones DP. Glutathione and thioredoxin redox during differentiation in human colon epithelial (Caco-2) cells . Am J Physiol Gastrointest Liver Physiol. 2002;283:G1352–G1359. doi: 10.1152/ajpgi.00183.2002. [DOI] [PubMed] [Google Scholar]
- Sekharam M, Trotti A, Cunnick JM, Wu J. Suppression of fibroblast cell cycle progression in G1 phase by N-acetylcysteine. Toxicol Appl Pharmacol. 1998;149:210–216. doi: 10.1006/taap.1997.8361. [DOI] [PubMed] [Google Scholar]
- Burdon RH, Gill V, Rice-Evans C. Oxidative stress and tumour cell proliferation . Free Radic Res Commun. 1990;11:65–76. doi: 10.3109/10715769009109669. [DOI] [PubMed] [Google Scholar]
- Kusano C, Takao S, Noma H, Yoh H, Aikou T, Okumura H, Akiyama S, Kawamura M, Makino M, Baba M. N-acetyl cysteine inhibits cell cycle progression in pancreatic carcinoma cells. Hum Cell. 2000;13:213–220. [PubMed] [Google Scholar]
- Menon SG, Coleman MC, Walsh SA, Spitz DR, Goswami PC. Differential susceptibility of nonmalignant human breast epithelial cells and breast cancer cells to thiol antioxidant-induced G(1)-delay . Antioxid Redox Signal. 2005;7:711–718. doi: 10.1089/ars.2005.7.711. [DOI] [PubMed] [Google Scholar]
- Burdon RH, Rice-Evans C. Free radicals and the regulation of mammalian cell proliferation . Free Radic Res Commun. 1989;6:345–358. doi: 10.3109/10715768909087918. [DOI] [PubMed] [Google Scholar]
- Burdon RH, Gill V, Rice-Evans C. Cell proliferation and oxidative stress . Free Radic Res Commun. 1989;7:149–159. doi: 10.3109/10715768909087937. [DOI] [PubMed] [Google Scholar]
- Conour JE, Graham WV, Gaskins HR. A combined in vitro/bioinformatic investigation of redox regulatory mechanisms governing cell cycle progression . Physiol Genomics. 2004;18:196–205. doi: 10.1152/physiolgenomics.00058.2004. [DOI] [PubMed] [Google Scholar]
- Futakuchi M, Ogawa K, Tamano S, Takahashi S, Shirai T. Suppression of metastasis by nuclear factor kappaB inhibitors in an in vivo lung metastasis model of chemically induced hepatocellular carcinoma . Cancer Sci. 2004;95:18–24. doi: 10.1111/j.1349-7006.2004.tb03165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin V, Herrera F, Carrera-Gonzalez P, Garcia-Santos G, Antolin I, Rodriguez-Blanco J, Rodriguez C. Intracellular signaling pathways involved in the cell growth inhibition of glioma cells by melatonin . Cancer Res. 2006;66:1081–1088. doi: 10.1158/0008-5472.CAN-05-2354. [DOI] [PubMed] [Google Scholar]
- Attele AS, Wu JA, Yuan CS. Ginseng pharmacology: multiple constituents and multiple actions. Biochem Pharmacol. 1999;58:1685–1693. doi: 10.1016/s0006-2952(99)00212-9. [DOI] [PubMed] [Google Scholar]
- Attele AS, Zhou YP, Xie JT, Wu JA, Zhang L, Dey L, Pugh W, Rue PA, Polonsky KS, Yuan CS. Antidiabetic effects of Panax ginseng berry extract and the identification of an effective component. Diabetes. 2002;51:1851–1858. doi: 10.2337/diabetes.51.6.1851. [DOI] [PubMed] [Google Scholar]
- Yokozawa T, Satoh A, Cho EJ. Ginsenoside-Rd attenuates oxidative damage related to aging in senescence-accelerated mice. J Pharm Pharmacol. 2004;56:107–113. doi: 10.1211/0022357022449. [DOI] [PubMed] [Google Scholar]
- Liu ZQ, Luo XY, Sun YX, Chen YP, Wang ZC. Can ginsenosides protect human erythrocytes against free-radical-induced hemolysis? Biochim Biophys Acta. 2002;1572:58–66. doi: 10.1016/s0304-4165(02)00281-7. [DOI] [PubMed] [Google Scholar]
- Liu ZQ, Luo XY, Liu GZ, Chen YP, Wang ZC, Sun YX. In vitro study of the relationship between the structure of ginsenoside and its antioxidative or prooxidative activity in free radical induced hemolysis of human erythrocytes. J Agric Food Chem. 2003;51:2555–2558. doi: 10.1021/jf026228i. [DOI] [PubMed] [Google Scholar]
- Deng HL, Zhang JT. Anti-lipid peroxilative effect of ginsenoside Rb1 and Rg1. Chin Med J (Engl ) 1991;104:395–398. [PubMed] [Google Scholar]
- Chen XC, Zhou YC, Chen Y, Zhu YG, Fang F, Chen LM. Ginsenoside Rg1 reduces MPTP-induced substantia nigra neuron loss by suppressing oxidative stress. Acta Pharmacol Sin. 2005;26:56–62. doi: 10.1111/j.1745-7254.2005.00019.x. [DOI] [PubMed] [Google Scholar]
- Zhang Q, Kang X, Zhao W. Antiangiogenic effect of low-dose cyclophosphamide combined with ginsenoside Rg3 on Lewis lung carcinoma. Biochem Biophys Res Commun. 2006;342:824–828. doi: 10.1016/j.bbrc.2006.02.044. [DOI] [PubMed] [Google Scholar]
- Wang W, Zhao Y, Rayburn ER, Hill DL, Wang H, Zhang R. In vitro anti-cancer activity and structure-activity relationships of natural products isolated from fruits of Panax ginseng. Cancer Chemother Pharmacol. 2007;59:589–601. doi: 10.1007/s00280-006-0300-z. [DOI] [PubMed] [Google Scholar]
- Li G, Wang Z, Sun Y, Liu K, Wang Z. Ginsenoside 20(S)-protopanaxadiol inhibits the proliferation and invasion of human fibrosarcoma HT1080 cells. Basic Clin Pharmacol Toxicol. 2006;98:588–592. doi: 10.1111/j.1742-7843.2006.pto_415.x. [DOI] [PubMed] [Google Scholar]
- Yokozawa T, Liu ZW, Dong E. A study of ginsenoside-Rd in a renal ischemia-reperfusion model. Nephron. 1998;78:201–206. doi: 10.1159/000044911. [DOI] [PubMed] [Google Scholar]
- Yokozawa T, Owada S. Effect of ginsenoside-Rd in cephaloridine-induced renal disorder. Nephron. 1999;81:200–207. doi: 10.1159/000045277. [DOI] [PubMed] [Google Scholar]
- Yokozawa T, Liu ZW. The role of ginsenoside-Rd in cisplatin-induced acute renal failure. Ren Fail. 2000;22:115–127. doi: 10.1081/jdi-100100858. [DOI] [PubMed] [Google Scholar]
- Yokozawa T, Dong E. Role of ginsenoside-Rd in cisplatin-induced renal injury: special reference to DNA fragmentation. Nephron. 2001;89:433–438. doi: 10.1159/000046116. [DOI] [PubMed] [Google Scholar]
- Xie JT, Shao ZH, Vanden Hoek TL, Chang WT, Li J, Mehendale S, Wang CZ, Hsu CW, Becker LB, Yin JJ, Yuan CS. Antioxidant effects of ginsenoside Re in cardiomyocytes . Eur J Pharmacol. 2006;532:201–207. doi: 10.1016/j.ejphar.2006.01.001. [DOI] [PubMed] [Google Scholar]
- Yue PY, Wong DY, Wu PK, Leung PY, Mak NK, Yeung HW, Liu L, Cai Z, Jiang ZH, Fan TP, Wong RN. The angiosuppressive effects of 20(R)- ginsenoside Rg3. Biochem Pharmacol. 2006;72:437–445. doi: 10.1016/j.bcp.2006.04.034. [DOI] [PubMed] [Google Scholar]
- Kumar A, Kumar M, Panwar M, Samarth RM, Park TY, Park MH, Kimura H. Evaluation of chemopreventive action of Ginsenoside Rp1. Biofactors. 2006;25:29–43. doi: 10.1002/biof.5520260104. [DOI] [PubMed] [Google Scholar]
- Popovich DG, Kitts DD. Ginsenosides 20(S)-protopanaxadiol and Rh2 reduce cell proliferation and increase sub-G1 cells in two cultured intestinal cell lines, Int-407 and Caco-2. Can J Physiol Pharmacol. 2004;82:183–190. doi: 10.1139/y04-001. [DOI] [PubMed] [Google Scholar]
- Wu G, Fang YZ, Yang S, Lupton JR, Turner ND. Glutathione metabolism and its implications for health. J Nutr. 2004;134:489–492. doi: 10.1093/jn/134.3.489. [DOI] [PubMed] [Google Scholar]
- Grobben B, De Deyn PP, Slegers H. Rat C6 glioma as experimental model system for the study of glioblastoma growth and invasion. Cell Tissue Res. 2002;310:257–270. doi: 10.1007/s00441-002-0651-7. [DOI] [PubMed] [Google Scholar]
- Yang MS, Gupta RC. Determination of energy charge potential in the C6 glioma and the HepG-2 cell culture. Toxicology Mechanisms and Methods. 2003;13:97–101. doi: 10.1080/15376510309843. [DOI] [PubMed] [Google Scholar]
- Hissin PJ, Hilf R. A fluorometric method for determination of oxidized and reduced glutathione in tissues . Anal Biochem. 1976;74:214–226. doi: 10.1016/0003-2697(76)90326-2. [DOI] [PubMed] [Google Scholar]
- Yang MS, Yu LC, S.W. P. Manipulation of energy and redox states in the C6 glioma cells by buthionine sulfoxamine and N-acetylcysteine and the effect on cell survival to cadmium toxicity. Cellular and Molecular Biology. 2007;53:56–61. [PubMed] [Google Scholar]
- Shi MM, Iwamoto T, Forman HJ. gamma-Glutamylcysteine synthetase and GSH increase in quinone-induced oxidative stress in BPAEC . Am J Physiol. 1994;267:L414–L421. doi: 10.1152/ajplung.1994.267.4.L414. [DOI] [PubMed] [Google Scholar]
- Chen ZH, Yoshida Y, Saito Y, Sekine A, Noguchi N, Niki E. Induction of adaptive response and enhancement of PC12 cell tolerance by 7-hydroxycholesterol and 15-deoxy-delta(12,14)-prostaglandin J2 through up-regulation of cellular glutathione via different mechanisms . J Biol Chem. 2006;281:14440–14445. doi: 10.1074/jbc.M600260200. [DOI] [PubMed] [Google Scholar]
- Bae EA, Shin JE, Kim DH. Metabolism of ginsenoside Re by human intestinal microflora and its estrogenic effect . Biol Pharm Bull. 2005;28:1903–1908. doi: 10.1248/bpb.28.1903. [DOI] [PubMed] [Google Scholar]
- Yue PY, Mak NK, Cheng YK, Leung KW, Ng TB, Fan DT, Yeung HW, Wong RN. Pharmacogenomics and the Yin/Yang actions of ginseng: anti-tumor, angiomodulating and steroid-like activities of ginsenosides . Chin Med. 2007;2:6. doi: 10.1186/1749-8546-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]