Abstract
Whilst there is strong evidence that human papillomavirus (HPV) is the principal aetiological agent in cervical neoplasia, some other sexually transmitted agents may either contribute or protect against cervical carcinogenesis, such as the herpes virus family (HSV), cytomegalovirus (CMV), Epstein-Barr virus (EBV), human immunodeficiency virus (HIV) or Chlamydia trachomatis (CT). Epidemiological studies suggest that HSV may have a role in cervical neoplasia, but there is no clear supportive experimental evidence. Serological studies have also failed to reveal a difference in the prevalence of antibodies to CMV and EBV between patients with cervical cancer and controls. However, longitudinal seroepidemiological studies have provided evidence that CT is an independent risk factor for the development of cervical squamous carcinoma and this association is serotype specific. The increased risk of cervical neoplasia in patients infected with HIV has been recognised for over a decade and HIV may interact with HPV either by alternating HPV gene transcription or by immunosuppression. Finally extensive experimental and limited epidemiological evidence suggests that adeno-associated viruses (AAV) may have antioncogenic activity in man and may protect against the development of cervical cancer. At present the mechanism of this action is unclear but may relate to AAV-induced regulation of HPV gene expression and the HPV life cycle. In this review we summarize the current literature relating to the associations and mechanisms of cervical carcinogenesis by each of these infectious microorganisms.
Keywords: Human papillomavirus (HPV), cervical neoplasia, sexually transmitted infections (STI), microbiology
Introduction
Sexual activity has both life-giving and life-endangering effects. The association of cervical carcinoma and sexual activity has been known over 150 years. As any sexually transmitted infection, cervical carcinoma is more common in woman who have had multiple sexual partners or whose partner is promiscuous, and is absent in virgins. Rigoni-Stern in 1842 noticed that cervical carcinoma occurred only in married woman [1].
In the UK, about 2300 woman per year are diagnosed as having cervical cancer, 95% of cases occurring in woman over the age of 35 years [2]. However, the number of deaths from cervical cancer has decreased by more than 40% during the last 20 years, and the incidence of cervical cancer is now more than that, for example, breast cancer (41,000 new cases per year) [3–6]. This decrease is directly related to implementation of cervical screening programs. It is estimated that 471,000 new cases of cervical cancer are diagnosed every year worldwide, 80% of which occur in less developed countries [2–4, 6–12].
About 15% of human cancer can be attributed to virus infection, and viruses are second only to tobacco as a risk factor for cancer. In the future, a major proportion of these infections may be preventable by immunization, significantly reducing the worldwide cancer burden. The importance of the experimental study of tumour viruses in animals and human illustrated by the fact that oncogenes and tumour suppressor genes were first identified through their interaction with tumour virus proteins [13–26]. There are two major mechanisms by which oncogenic viruses induce tumours [16, 27–30]. In direct oncogenesis, the virus infects a progenitor of the clonal tumour cell population, and usually persists in the tumour cells. Indirect oncogenesis occurs when the virus does not necessarily infect the tumour progenitor cell, but exerts an indirect effect on cell and tissue turnover or in the immune system, predisposing to tumour development.
However, assessing an infectious aetiology can be difficult [16]. Firstly, subclinical infections are common and this may lead to misclassification bias. Secondly, complex interactions can result because many sexually transmitted infections do occur simultaneously. Thirdly, the presence of a latency period between exposure and outcome, which vary considerably, is another problem. Finally, clinical follow-up studies always remain inconclusive [16, 27, 28, 30–41].
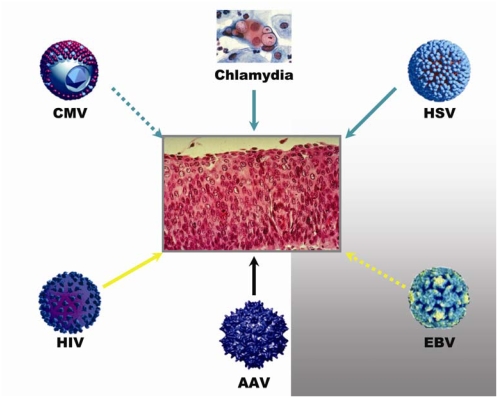
Whilst there is strong evidence that human papillomavirus (HPV) is the principle aetiological agent in cervical neoplasia [13, 27, 42–64], some other sexually transmitted organisms may either contribute to or protect against cervical carcinogenesis [65–82] (Figure 1).
Figure 1.
An illustration of the relationship between cervical neoplasia and infectious micro-organisms.
Papillomaviruses
HPV group currently comprises more than 130 distinct types [83, 84], causing lesions of the genital, upper respiratory and digestive tracts, and cutaneous lesions at various sites [85, 86]. For each virus type, the site of infection is very restricted. The lesions caused are usually benign [86–102].
Cervical neoplasia is known to be induced in different ways, such as via multiple pregnancies [103–106], radiation [107–112], smoking [113–119] and viral infection. HPV is regarded as the most significant risk factor for cervical carcinoma. Cancer of the cervix was identified as a sexually transmitted disease in 1834, and the hypothesis that HPV is involved was suggested in the mid-1970's [50, 105, 120–130]. The risk varies according to the infecting HPV subtype, for example, high risk (types 16 and 18), moderate risk (types 33 and 35) and low risk (types 6 and 11). Subsequent studies have shown that almost all cervical cancers are HPV-positive and that only certain HPV types are associated with invasive carcinoma (most commonly HPV-16, HPV-18, HPV-31, and HPV-45) [131–138]. These and other HPVs are also found in other anogenital cancers [139–142] and may cause cancers at other sites such as the head and neck [142–152], oesophagus [102, 149, 151, 153–156] and skin [87, 88, 157–166].
α-Herpesviruses
HSV-2 is the main cause of primary and genital herpes. Because of changing sexual practices, many causes of primary genital herpes are caused by HSV-1, though this virus is less likely to reactivate from the sacral ganglia than is HSV-2. Current research on genital herpes focuses on asymptomatic patients as a common course of infection.
The role of HSV in the development of cervical neoplasia has been a subject of extensive research. Patients with cervical carcinoma have consistently been shown to demonstrate the presence of higher levels of HSV-2 antibody than controls. An interaction between HSV and HPV-16/18 in the causation of cervical carcinogenesis has been suggested by several groups [167–170]. Two hypotheses have been devised to explain this: the ‘hit and run’ hypothesis and synergism between HSV and HPV [171]. Of these there is more epidemiological and experimental support of the latter. HSV is known to contain regions on its genome capable of transforming cells in vitro which could make it a candidate for oncogenic transformation in vivo. On the other hand, in a study by Vecchione et al (1994) investigating the interaction between HPV types 16 and 18, HSV-2 and p53 inactivation, none of the 41 cervical biopsies (ranging from low to high grade cervical intraepithelial neoplasm) tested positive for HSV-2. In addition, this study showed that the infection with HPV-16 and the alteration of p53 expression were the most important associations [172].
However, the potential interaction between HPV and HSV is supported with several lines of evidence [167–170, 173, 174]. First, ulcerative herpetic lesions facilitate HPV access to the basal layer. Second, the inflammatory response induced by herpes may suppress the T helper cell mediated immune response. Third, herpes infection does induce the production of nitric oxide resulting in cellular DNA damage together with direct actions by herpes viruses on host cellular DNA. Fourth, Herpes virus infection accelerates replication of HPV and increases the integration of HPV DNA sequences.
In a pooled analysis of 7 case-control studies to examine the effects of HSV-2 as an HPV cofactor, blood and exfoliated cervical cells obtained from 1263 cases of cervical cancer and 1117 age-matched controls were investigated using Western blot analysis, PCR and ELISA [170]. The odds ratio (ORs) and confidence intervals (CIs) computed from unconditional logistic regression models are summarised in Tables 1–3. ORs and CI of HSV seropositivity and cervical cancer from previous case-control studies are summarised in Table 4 [175–179].
Table 1.
Seroprevalence of HSV antibodies and HPV DNA in invasive cervical cancers and controls
| N | % HSV-2 seropositive (95% CI) | % HSV-1 seropositive (95% CI) | % HPV DNA positive (95% CI) | Median age, years (range) | |
|---|---|---|---|---|---|
| Squamous Cell Carcinoma | 1158 | 44.4 (41.5–47.3) | 80.3 (77.9–88.3) | 94.8 (93.5–96.1) | 49 (18–84) |
| Adeno- or adenosquamous carcinoma | 105 | 43.8 (34.2–53.5) | 85.7 (76.3–95.2) | 90.5 (84.4–96.2) | 48 (28–69) |
| Controls | 1117 | 25.6 (23.0–28.2) | 89.6 (87.0–92.1) | 14.7 (12.6–16.8) | 47 (21–77) |
Table 3.
Odds ratios of invasive cervical cancers and 95% confidence intervals among all cases and controls according to HSV-2 seropositivity
| Case patients HSV2+/HSV2− | Control subjects HSV2+/HSV2− | OR | 95% CI | |
|---|---|---|---|---|
| Squamous cell carcinoma | 514/644 | 286/831 | 1.72 | 1.21–2.44 |
| Adeno- or adenosquamous carcinoma | 46/59 | 241/726 | 2.43 | 1.22–4.81 |
Table 4.
HSV seropositivity and cervical cancer from previous case-control studies
Table 2.
Odds ratios of invasive cervical cancers and 95% confidence intervals among HPV positive women according to HSV-2 seropositivity
| Case patients HSV2+/HSV2− | Control subjects HSV2+/HSV2− | OR | 95% CI | |
|---|---|---|---|---|
| Squamous cell carcinoma | 497/601 | 49/115 | 2.19 | 1.41–3.40 |
| Adeno- or adenosquamous carcinoma | 43/52 | 39/100 | 3.37 | 1.47–7.74 |
Lehtinen et al in a longitudinal nested case control study in Nordic countries using 1974–1993 data showed that smoking- and HPV positive-adjusted relative risks for HSV-2 were 1.0 (95% CI 0.6) and 0.7 (95% CI o.3, 1.6) respectively for HPV seropositives. Comparing results with those of meta-analysis revealed that the relative risk for HSV-2 was 0.9 (95% CI 0.6, 1.3). In addition, HSV was shown not to play a role in cervical carcinogenesis [180]. It is important to note that conflicting seroepidemiological evidence of an interaction between HSV and HPV in cervical carcinogenesis has been shown by different authors. In addition, in vitro observations are not yet confirmed in vivo.
β-Herpesviruses
Cytomegalovirus (CMV), human herpes virus-6 and -7 (HHV-6 and HHV-7) are members of the β-herpesvirus group and are found universally throughout all geographic locations and socioeconomic groups. HHV-6 was identified in 1986 and causes roseola infantum (exanthema sabitum) in infants. HHV-6 is clearly neurotropic and has recently been suggested, but not confirmed, as an aetiological factor in multiple sclerosis [181–184]. HHV-7 was first described in 1991 and causes roseola infantum in a few patients, but seems to be less pathogenic than HHV-6.
CMV, HHV-6 and HHV-7 have all been detected in the cervix [185]. CMV spreads mainly by sexual and transfusion routes. Infection of the genital tract with CMV evidenced by inclusion bodies on the cervical smear is uncommon. CMV infection of the genital tract in immunocompetent females is generally regarded as incidental and self-limiting. In immunocompromised patients, CMV is an opportunistic infection that has been reported in the genital tract. This was reported in two patients with HIV undergoing colposcopy, in which one patient developed asymptomatic pelvic inflammatory disease and disseminated infection in the other. In paraffin embedded sections from 34 Ugandans patients with cervical carcinoma, CMV was detected in five of the 34 cases using immunohistochemistry. In all cases CMV antibody reactivity was confined to the cervical epithelial tissue. These results were interpreted as evidence for association between CMV and cervical carcinoma. However, the immune status of these patients and their HPV status were not correlated to the immunostaining findings [186]. Several studies using PCR analyses have also revealed CMV in women with cervical cancer. For example CMV was found in 67% of Taiwanese woman with cervical cancer [187], but only 4% in Australian woman.
In a PCR-based study involving 388 women attending colposcopy clinics by Chan et al [188], the association between these viruses and cervical neoplasia was analysed with respect to the HPV status. Positive rates for CMV, HHV-6 and HHV-7 were 9.5%, 3.6% and 3.4%, respectively. HPV positive patients carried a high risk of high grade cervical lesions, whereas those positive for CMV, HHV-6 and HHV-7 did not. Chan et al concluded that these viruses are bystanders rather than cofactors in oncogenesis of cervical cancer. More recently, Yang et al studied the correlation of viral factors (including CMV) with cervical cancer and concluded that CMV might not be involved in the oncogenic processes directly but might enhance the possibility of oncogenesis or infect cancer tissues opportunistically [189].
HHV-6 was found in 38% and 20% of women with cervical carcinoma using in situ hybridisation [190] and PCR [191, 192], respectively. Two groups have studied the prevalence of HHV-6 and HHV-7 in the female genital tract [185, 193–195]. Leach et al found HHV-6 in 10% of vaginal swabs of women attending Genito-Urinary Medicine (GUM) clinics [193–195], whereas Okuno et al found HHV-6 (the B variant only) in 19.4% of cervical swabs from 72 pregnant women compared to 34 non-pregnant controls, and HHV-7 in 2.7% of pregnant women and none in the non-pregnant controls. In addition, 1% of woman with abnormal smears were positive for HHV-6 [196–200]. In another study performed in Wessex, UK, HHV-6 was detected in 18% of samples examined [201]. Overall, the high incidence of HHV-6 and HHV-7 in cervical smears may indicate that these viruses are sexually transmitted. Alternatively, the presence of HHV-6 and HHV-7 in cervical samples could be due to macrophages or lymphocytes from the tissue or blood that are simultaneously collected with cervical cells or latently infected epithelial cells. In this case, detection of these viruses in the cervix may therefore represent dissemination of a systemic infection rather than sexually acquired infection. Therefore, it appears that HHV-6, HHV-7 and CMV are unlikely to have a direct role in the carcinogenesis of cervical neoplasia.
γ-Herpesviruses
Kaposi's sarcoma-associated herpesvirus (KSHV) or human herpes virus-8 (HHV-8) was first described in 1994 and has been linked to several malignancies in the human population such as Kaposi's sarcoma (KS), primary effusions lymphomas (PEL) and multicenteric Castleman's disease (MCD). It is believed that HHV-8 transforms cells through a paracrine mechanism since there is a plethora of evidence of high levels of cytokines and growth factors in lesions of KS and MCD. HHV-8 has been shown to infect but not immortalise CD19-positive B cells in vitro, perhaps due to technical difficulties in culture system. In contrast, HHV-8 can immortalise primary bone marrow derived endothelial cell; the virus induces cell proliferation, anchorage independence and survival of these cells. Interestingly, only a subset of the transformed endothelial cells contained viral DNA, suggesting that uninfected cells survived through a mechanism involving cytokines secreted by the infected cells. These observations suggest that HHV-8 transformation is highly dependent on paracrine factors as well as the cellular microenvironment, a concept gaining favour in other tumour models as well.
The relation between HHV8 and cervical carcinoma has also been investigated [188, 202–210]. Recently, Taylor et al found that the prevalence of HHV-8 DNA was 32% in saliva samples, 28% mouth swabs, 4% in cervical swabs, 2.3% in vaginal swabs, 9% in plasma samples and 18% in peripheral-blood mononuclear cell sample from HIV seropositive and seronegative Kenyan women [211]. Similar results were found in oral and genital secretions of Zimbabwean women. On the other hand, a real-time PCR study showed that no cervical secretion or leukocyte samples contained detectable HHV-8 DNA. However, the latter study detected antibodies to HHV-8 of serum samples. Lanham et al showed that there was no link with cervical intraepithelial neoplasia status and the detection of HHV-8 [212].
Epstein-Barr Virus (EBV)
EBV was the first human tumour virus discovered from biopsy tissue samples of the childhood malignancy African Burkitt lymphoma. It is one of the most efficient cellular growth-transforming viruses known, but in most infected individuals (more than 90% of the world population) it coexists with the host asymptomatically. Infected individuals become lifelong carriers. Under certain conditions, however, its potential as a tumour-causing agent is realised, and EBV is associated with a wide spectrum of clinical conditions, many of which are malignant. Three lymphoproliferative disorders have known associations with EBV: Hodgkin lymphoma, Burkitt lymphoma and lymphoma in immunocompromised individuals. Although the lymphotropism of EBV is well recognised, it is becoming increasingly clear that EBV may have epitheliotropic qualities. For example, an association with EBV was established with nasopharyngeal and gastric carcinoma. In addition, several studies suggested a possible connection between EBV and cervical neoplasia although no serological evidence of such an association has been reported.
Landers et al randomly studied selected cases of invasive cervical carcinoma as well as cases with varying degrees of cervical intraepithelial neoplasm (CIN) and normal cervices. Their results showed that neither normal cervices nor CIN 1 specimens contained EBV, but that 8% of cases of both CIN 2 and CIN 3 and 43% cases of cervical carcinoma contained EBV detected by PCR and/or in situ hybridisation [213]. However, Hilton et al tested the presence of EBV in epithelial cells and showed, using in situ hybridization, that none of 10 CIN cases or 24 cervical carcinoma cases were EBV positive [214]. Thus, the positive results of the Landers study may simply reflect EBV in stromal cervical lymphocytes. To clarify the relationship between EBV and CIN, given the conflicting results of Hilton et al and Landers et al, 30 CIN cases were evaluated of which 20 were EBV positive using PCR. The authors stated that PCR results should always be confirmed by a morphological technique [213, 215, 216]. PCR and in-situ hybridisation have also shown that the expression rates of genes such as EBNA-2, LMP-1 and EBER-1 were also significantly higher in cervical carcinoma and CIN than in the normal cervix [217–219].
Overall, these studies support a possible sexual route of transmission for EBV. However, there is no convincing evidence that EBV infection has a direct role in the pathogenesis of cervical neoplasia or even HPV-mediated carcinogenesis. However, EBV-infected tumour infiltrating lymphocytes might contribute indirectly to cervical carcinogenesis via producing viral IL-10 expressed from BCRF-1 gene, which causes a reduction in local immunity leading to suppression of the response to HPV-transformed cells.
Human Immunodeficiency Virus (HIV)
It remains debatable whether HIV infection itself increases the incidence of invasive cervical carcinoma. Cervical cancer was added to the Centre for Disease Control (CDC) classification for AIDS defining illness in 1993 despite sparse evidence for a causal relationship. Smith et al found no association between the detection of HPV and immunosuppression or CIN, but rather immunosuppressed HIV-positive females had a higher incidence regardless of the presence or absence of HPV, EBV or HSV for which subjects were tested. An odds ratio of 4.9 for an association between HIV and cervical dysplasia was found in a meta-analysis of five studies [220, 221].
The interaction between HPV and HIV in the affected cervical tissue leads to the persistence of HPV infection and cervical neoplasia by depleting Langerhans cells or their MHC class presenting ability of the host immune response. An alternative explanation is at the cellular level; HIV specific Tat protein upregulates expression of HPV E6 and E7 oncogenes and enhances their oncogenetic transformation efficacy. These two mechanisms are, however, not exclusive and a joint effect(s) most likely takes place at early stages of CIN [222–231].
Both HPV infection and CIN are common in woman with HIV infection. HIV disease may be asymptomatic, however, and therefore woman with rapidly progressive CIN should be tested for HIV. Recurrence rates are disappointingly high with standard local ablative therapy for CIN. Frequent and regular cervical smears are recommended. Woman with any degree of abnormal cytology must be referred for colposcopy. Invasive cervical carcinoma in HIV-positive woman is usually advanced, and more likely to relapse following treatment. The incidence is unchanged with highly active anti-retroviral therapy (HAART). Management is as in seronegative woman and involves chemoradiotherapy, but the prognosis is worse [222–231].
Adeno-Associated Viruses (AAV)
AAV is a ubiquitous human helper-dependent common genital parvovirus that may protect, at least, in part against HPV-associated cervical cancer. AAV may also be sexually acquired. This virus has many features of parvovirus but relies on co-infection with other viruses to replicate. AAV has not been associated with any disease in humans despite its ability to integrate in the cell genome. In fact, limited epidemiological studies indicate a negative correlation between AAV infection and the incidence of cervical cancer, although some groups reported no association with either CIN or invasive squamous cell carcinoma. AAV antibodies are detectable in 45% of the population and 60% of the adult population specifically, but antibody titres in patients with cervical carcinoma are well below those of age-matched controls. In addition, using a whole virus AAV sandwich enzyme linked immunosorbent assay, no relationship was found between AAV antibodies and the presence or grade of neoplasia in 291 cervical specimens from 291 Jamaican woman and 79 United States university students enrolled in one study. Extensive experimental evidence suggests that AAV have an anti-oncogenic activity and may protect against the development of cervical carcinoma [232]. At present the mechanism of this action is unclear but may be related to AAV induced regulation of HPV gene expression and HPV life cycle. Using a raft culture system, Mayers et al demonstrated a complex interaction between AAV, HPV and skin during dual infection [233]. As AAV has a relatively fast life cycle generating infectious progeny, Agrawal et al suggested that AAV has a significant effect upon the temporal kinetics of the HPV life cycle in natural host tissue [234]. Furthermore, AAV was shown to inhibit bovine papilloma virus 1 and HPV 16 and HPV 18 oncogenic properties in tissue culture via the rep 78 protein. It is known that the primary AAV infection usually occurs in childhood, but unstable AAV antibody response may allow lifelong reinfection or reactivation of persisting virus. Lanhham et al found AAV in similar proportions of high and low grade CIN samples in all age groups studied, indicating that reactivation of latent infection rather than reinfection would be the most likely source of AAV [212]. This suggests that many women will have latent AAV infection from an early age and hence the possible susceptibility to HPV transformation if cells in the endocervix are infected. Interestingly, Coker et al demonstrated that AAV positivity was associated with significantly reduced risk of high-grade intraepithelial lesions (HSIL) [235], but not LSIL and not associated with race, HPV status, age or sexual risk factors. In contrast, Walz et al detected AAV in 63% of samples from high grade CIN biopsies [236], and in a larger study by Strickler et al, no evidence was found of AAV infection in either CIN samples or CIN normal cervical samples [237].
It seems that the inverse association between AAV and cervical neoplasia may be due to an ability of AAV to change the role of HPV in cervical carcinogenesis in particular in late stages of carcinogenesis. This conclusion needs to be verified in additional epidemiological studies and undoubtedly merits further experimental work.
Chlamydia trachomatis (CT)
Chlamydia is an obligate intracellular bacterium, and is the most sexually transmitted micro-organism in the developed world, causing genital and ocular disease. Serovars A-C cause trachoma; serovars D-K affect primarily the genital tract. It is estimated that 3–5% of sexually active young women are infected, and up to 10% in selected groups. Chlamydial infection is associated with age under 25 years, a new sexual partner or more than one sexual partner in the recent past, lack of barrier contraception, use of oral contraceptive pill, and termination of pregnancy.
In earlier prospective studies an association between past infection with CT and cervical cancer was found, but strength of evidence was limited either due to inability to control for effects of HPV 16 or due to limited number of cases [238]. Exposure as assessed by serology has been shown that CT to be significant and independent risk factor for cervical neoplasia. For example, Bjorge et al suggested that effects of CT are specific for cervical cancer and not other anogenital cancers [239, 240]. In addition, higher rates of progression to CIN3 have been noted in females whose cervical smears had changes suggestive of CT infection, although this is a relatively insensitive method for detection.
Koskela et al found in a longitudinal study that antibodies to CT were associated with increased risk of squamous cell carcinoma (SCC) (HPV and smoking adjusted OR, 2.2; 95% CI, 1.3–3.5) and this risk increased with increasing time from serum sampling to cancer diagnosis, and the OR for metastatic disease were larger than for localised disease [241]. These results are surprising since the increased risk was specific for SCC and not adenocarcinoma, and since endocervical glandular cell are the targets for CT. This might be related to metaplastic cells being permissive to CT. Whether or not infection with CT could alter the proportion of cells permissive to the oncogenic HPV types also remains to be determined, but interaction between the two micro-organisms in cervical carcinogenesis remains possible.
In another longitudinal nested case-control study within a cohort of 530,000 women who provided samples to serum banks in Finland, Norway and Sweden, the association between exposure to different CT serotypes and subsequent development of cervical SCC was investigated. Interestingly, of specific CT serotypes, serotype G was most strongly associated with SCC (adjusted OR, 6.6; 95% CI, 1.6–27.0). Other serotypes associated with SCC are the I serotype (OR, 3.8; 95% CI, 1.3–11.0) and the D serotype (OR, 2.7; 95% CI, 1.3–5.6). Furthermore, the serum IgGs to more than one serotype increased the ORs for SCC (p<0.001 for trend) [242].
The molecular mechanisms underlying cervical carcinogenesis induced by CT are not fully understood. Genetic damage and neoplastic changes induced in vitro, release of nitric oxide and the inhibition of host cell apoptosis by blockade of mitochondrial cytochrome c release and caspase activation might account, at least, in part for such mechanisms [243].
In summary, this contribution focuses on HPV and non-HPV causes of cervical neoplasia. The role of these infectious non-HPV organisms in the prevention, diagnosis, vaccination and treatment of cervical neoplasia merits further clinico-pathological-molecular studies.
References
- 1.Rigoni-Stern D. Statistical facts relating to cancer. G Service Progr Pathol Terap Ser. 1842;2:507–517. [Google Scholar]
- 2.Giannopoulos T, Butler-Manuel S, Tailor A, Demetriou E, Daborn L. Prevalence of high-grade CIN following mild dyskaryotic smears in different age groups. Cytopathology. 2005;16:277–280. doi: 10.1111/j.1365-2303.2005.00301.x. [DOI] [PubMed] [Google Scholar]
- 3.Walker P. The English National Health Service Cervical Screening Programme–approach to new technologies and quality assurance. J Low Genit Tract Dis. 2005;9:118–123. doi: 10.1097/00128360-200504000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Grainge MJ, Seth R, Coupland C, Guo L, Rittman T, Vryenhoef P, Johnson J, Jenkins D, Neal KR. Human papillomavirus infection in women who develop high-grade cervical intraepithelial neoplasia or cervical cancer: a case-control study in the UK. Br J Cancer. 2005;92:1794–1799. doi: 10.1038/sj.bjc.6602538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pharoah P. Genetic epidemiology of cancer: relatively risky relatives. Eur J Hum Genet. 2005;13:519–520. doi: 10.1038/sj.ejhg.5201395. [DOI] [PubMed] [Google Scholar]
- 6.Comber H, Gavin A. Recent trends in cervical cancer mortality in Britain and Ireland: the case for population-based cervical cancer screening. Br J Cancer. 2004;91:1902–1904. doi: 10.1038/sj.bjc.6602236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garnett GP, Kim JJ, French K, Goldie SJ. Modelling the impact of HPV vaccines on cervical cancer and screening programmes. Vaccine. 2006;24:S178–186. doi: 10.1016/j.vaccine.2006.05.116. [DOI] [PubMed] [Google Scholar]
- 8.Tawfik El-Mansi M, Cuschieri KS, Morris RG, Williams AR. Prevalence of human papillomavirus types 16 and 18 in cervical adenocarcinoma and its precursors in Scottish patients. Int J Gynecol Cancer. 2006;16:1025–1031. doi: 10.1111/j.1525-1438.2006.00552.x. [DOI] [PubMed] [Google Scholar]
- 9.Barnabas RV, Laukkanen P, Koskela P, Kontula O, Lehtinen M, Garnett GP. Epidemiology of HPV 16 and cervical cancer in Finland and the potential impact of vaccination: mathematical modelling analyses. PLoS Med. 2006;3:e138. doi: 10.1371/journal.pmed.0030138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grainge MJ, Seth R, Guo L, Neal KR, Coupland C, Vryenhoef P, Johnson J, Jenkins D. Cervical human papillomavirus screening among older women. Emerg Infect Dis. 2005;11:1680–1685. doi: 10.3201/eid1111.050575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah S, Montgomery H, Smith C, Madge S, Walker P, Evans H, Johnson M, Sabin C. Cervical screening in HIV-positive women: characteristics of those who default and attitudes towards screening. HIV Med. 2006;7:46–52. doi: 10.1111/j.1468-1293.2005.00331.x. [DOI] [PubMed] [Google Scholar]
- 12.Peto J, Gilham C, Fletcher O, Matthews FE. The cervical cancer epidemic that screening has prevented in the UK. Lancet. 2004;364:249–256. doi: 10.1016/S0140-6736(04)16674-9. [DOI] [PubMed] [Google Scholar]
- 13.Cuschieri KS, Horne AW, Szarewski A, Cubie HA. Public awareness of human papillomavirus. J Med Screen. 2006;13:201–207. doi: 10.1177/096914130601300408. [DOI] [PubMed] [Google Scholar]
- 14.Lupberger J, Hildt E. Hepatitis B virus-induced oncogenesis. World J Gastroenterol. 2007;13:74–81. doi: 10.3748/wjg.v13.i1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Campbell K. Understanding how viruses can cause malignant disease. Nurs Times. 2006;102:30–31. [PubMed] [Google Scholar]
- 16.Campbell K. The infectious causes of cancer. Nurs Times. 2006;102:28–30. [PubMed] [Google Scholar]
- 17.Young LS, Rickinson AB. Epstein-Barr virus: 40 years on. Nat Rev Cancer. 2004;4:757–768. doi: 10.1038/nrc1452. [DOI] [PubMed] [Google Scholar]
- 18.Yu MC, Yuan JM. Environmental factors and risk for hepatocellular carcinoma. Gastroenterology. 2004;127:S72–78. doi: 10.1016/j.gastro.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 19.Ledwaba T, Dlamini Z, Naicker S, Bhoola K. Molecular genetics of human cervical cancer: role of papillomavirus and the apoptotic cascade. Biol Chem. 2004;385:671–682. doi: 10.1515/BC.2004.083. [DOI] [PubMed] [Google Scholar]
- 20.Nahar A, Azad AK. Sexually transmitted diseases (STD) / reproductive tract infections (RTI) including acquired immunodeficiency syndrome (AIDS) / human immunodeficiency virus (HIV) infections among the women of reproductive age group: a review. J Prev Soc Med. 1999;18:84–88. [PubMed] [Google Scholar]
- 21.Greenberg SB. Respiratory viral infections in adults. Curr Opin Pulm Med. 2002;8:201–208. doi: 10.1097/00063198-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Rocken C, Carl-McGrath S. Pathology and pathogenesis of hepatocellular carcinoma. Dig Dis. 2001;19:269–278. doi: 10.1159/000050693. [DOI] [PubMed] [Google Scholar]
- 23.Thomas DJ. Sexually transmitted viral infections: epidemiology and treatment. J Obstet Gynecol Neonatal Nurs. 2001;30:316–323. [PubMed] [Google Scholar]
- 24.Ohtsuru A, Yamashita S. [Viral tumor markers] Nippon Rinsho. 1996;54:1529–1535. [PubMed] [Google Scholar]
- 25.Weinreb M, Day PJ, Niggli F, Powell JE, Raafat F, Hesseling PB, Schneider JW, Hartley PS, Tzortzatou-Stathopoulou F, Khalek ER, Mangoud A, El-Safy UR, Madanat F, Al Sheyyab M, Mpofu C, Revesz T, Rafii R, Tiedemann K, Waters KD, Barrantes JC, Nyongo A, Riyat MS, Mann JR. The role of Epstein-Barr virus in Hodgkin's disease from different geographical areas. Arch Dis Child. 1996;74:27–31. doi: 10.1136/adc.74.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chow VT. Cancer and viruses. Ann Acad Med Singapore. 1993;22:163–169. [PubMed] [Google Scholar]
- 27.Kanodia S, Fahey LM, Kast WM. Mechanisms used by human papillomaviruses to escape the host immune response. Curr Cancer Drug Targets. 2007;7:79–89. doi: 10.2174/156800907780006869. [DOI] [PubMed] [Google Scholar]
- 28.Klein E, Kis LL, Takahara M. Pathogenesis of Epstein-Barr virus (EBV)-carrying lymphomas. Acta Microbiol Immunol Hung. 2006;53:441–457. doi: 10.1556/AMicr.53.2006.4.3. [DOI] [PubMed] [Google Scholar]
- 29.Negro F. Mechanisms and significance of liver steatosis in hepatitis C virus infection. World J Gastroenterol. 2006;12:6756–6765. doi: 10.3748/wjg.v12.i42.6756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moss SF, Blaser MJ. Mechanisms of disease: Inflammation and the origins of cancer. Nat Clin Pract Oncol. 2005;2:90–97. doi: 10.1038/ncponc0081. [DOI] [PubMed] [Google Scholar]
- 31.Rapp F. Current knowledge of mechanisms of viral carcinogenesis. Crit Rev Toxicol. 1984;13:197–204. doi: 10.3109/10408448409034082. [DOI] [PubMed] [Google Scholar]
- 32.Willecke K, Schafer R. Human oncogenes. Hum Genet. 1984;66:132–142. doi: 10.1007/BF00286587. [DOI] [PubMed] [Google Scholar]
- 33.Maral J, Florentin I, Soubrane C, Maral R. [Cancer and immunosuppression : experimental aspects] Bull Cancer. 1983;70:351–371. [PubMed] [Google Scholar]
- 34.Gilden RV, Rabin H. Mechanisms of viral tumorigenesis. Adv Virus Res. 1982;27:281–334. doi: 10.1016/s0065-3527(08)60437-6. [DOI] [PubMed] [Google Scholar]
- 35.Tennant RW, Rascati RJ. Mechanisms of cocarcinogenesis involving endogenous retroviruses. Carcinog Compr Surv. 1980;5:185–205. [PubMed] [Google Scholar]
- 36.Borecky L. Interactions between viral infection and immune mechanisms. Comp Immunol Microbiol Infect Dis. 1980;3:381–390. doi: 10.1016/0147-9571(80)90015-6. [DOI] [PubMed] [Google Scholar]
- 37.Wainberg MA, Phillips ER. Immunity against avian sarcomas: a review. Isr J Med Sci. 1976;12:388–406. [PubMed] [Google Scholar]
- 38.Aurelian L. The “viruses of love” and cancer. Am J Med Technol. 1974;40:496–512. [PubMed] [Google Scholar]
- 39.Poste G. Mechanisms of virus-induced cell fusion. Int Rev Cytol. 1972;33:157–252. doi: 10.1016/s0074-7696(08)61451-5. [DOI] [PubMed] [Google Scholar]
- 40.Smith RT. Tumor-specific immune mechanisms. N Engl J Med. 1968;278:1207–1214. doi: 10.1056/NEJM196805302782206. [DOI] [PubMed] [Google Scholar]
- 41.Stoker M. Mechanisms of viral carcinogenesis. Proc Can Cancer Conf. 1966;6:357–368. [PubMed] [Google Scholar]
- 42.Freitag P. [Prophylactic HPV vaccination] Ceska Gynekol. 2007;72:38–41. [PubMed] [Google Scholar]
- 43.Monk BJ, Mahdavi A. Human papillomavirus vaccine: a new chance to prevent cervical cancer. Recent Results Cancer Res. 2007;174:81–90. doi: 10.1007/978-3-540-37696-5_8. [DOI] [PubMed] [Google Scholar]
- 44.Arbyn M, Dillner J. Review of current knowledge on HPV vaccination: An Appendix to the European Guidelines for Quality Assurance in Cervical Cancer Screening. J Clin Virol. 2007;38:189–197. doi: 10.1016/j.jcv.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 45.Behtash N, Mehrdad N. Cervical cancer: screening and prevention. Asian Pac J Cancer Prev. 2006;7:683–686. [PubMed] [Google Scholar]
- 46.Dehn D, Torkko KC, Shroyer KR. Human papillomavirus testing and molecular markers of cervical dysplasia and carcinoma. Cancer. 2007;111:1–14. doi: 10.1002/cncr.22425. [DOI] [PubMed] [Google Scholar]
- 47.Hymel PA. Decreasing risk: impact of HPV vaccination on outcomes. Am J Manag Care. 2006;12:S473–483. [PubMed] [Google Scholar]
- 48.Snoeck R. Papillomavirus and treatment. Antiviral Res. 2006;71:181–191. doi: 10.1016/j.antiviral.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 49.Wiley D, Masongsong E. Human papillomavirus: the burden of infection. Obstet Gynecol Surv. 2006;61:S3–14. doi: 10.1097/01.ogx.0000221010.82943.8c. [DOI] [PubMed] [Google Scholar]
- 50.Weaver BA. Epidemiology and natural history of genital human papillomavirus infection. J Am Osteopath Assoc. 2006;106:S2–8. [PubMed] [Google Scholar]
- 51.Zheng ZM, Baker CC. Papillomavirus genome structure, expression, and post-transcriptional regulation. Front Biosci. 2006;11:2286–2302. doi: 10.2741/1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Monsonego J. [Cervical cancer prevention: the impact of HPV vaccination] Gynecol Obstet Fertil. 2006;34:189–201. doi: 10.1016/j.gyobfe.2006.01.036. [DOI] [PubMed] [Google Scholar]
- 53.Malik AI. The role of human papilloma virus (HPV) in the aetiology of cervical cancer. J Pak Med Assoc. 2005;55:553–558. [PubMed] [Google Scholar]
- 54.Trottier H, Franco EL. The epidemiology of genital human papillomavirus infection. Vaccine. 2006;24:S1–15. doi: 10.1016/j.vaccine.2005.09.054. [DOI] [PubMed] [Google Scholar]
- 55.Tristram A. HPV information needs. Best Pract Res Clin Obstet Gynaecol. 2006;20:267–277. doi: 10.1016/j.bpobgyn.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 56.zur Hausen H, de Villiers EM. Human papillomaviruses. Annu Rev Microbiol. 1994;48:427–447. doi: 10.1146/annurev.mi.48.100194.002235. [DOI] [PubMed] [Google Scholar]
- 57.Beral V, Hermon C, Munoz N, Devesa SS. Cervical cancer. Cancer Surv. 1994;19–20:265–285. [PubMed] [Google Scholar]
- 58.Brinton LA, Herrero R, Reeves WC, de Britton RC, Gaitan E, Tenorio F. Risk factors for cervical cancer by histology. Gynecol Oncol. 1993;51:301–306. doi: 10.1006/gyno.1993.1294. [DOI] [PubMed] [Google Scholar]
- 59.Moscicki AB. Human papillomavirus infections. Adv Pediatr. 1992;39:257–281. [PubMed] [Google Scholar]
- 60.Vousden KH. Human papillomaviruses and cervical carcinoma. Cancer Cells. 1989;1:43–50. [PubMed] [Google Scholar]
- 61.Crum CP, Levine RU. Human papillomavirus infection and cervical neoplasia: new perspectives. Int J Gynecol Pathol. 1984;3:376–388. [PubMed] [Google Scholar]
- 62.Roy M, Morin C, Casas-Cordero M, Meisels A. Human papillomavirus and cervical lesions. Clin Obstet Gynecol. 1983;26:949–967. doi: 10.1097/00003081-198312000-00019. [DOI] [PubMed] [Google Scholar]
- 63.Meisels A. The story of a cell. The George N. Papanicolaou Award lecture. Acta Cytol. 1983;27:584–596. [PubMed] [Google Scholar]
- 64.Meisels A, Morin C, Casas-Cordero M, Rabreau M. Human papillomavirus (HPV) venereal infections and gynecologic cancer. Pathol Annu. 1983;18(Pt 2):277–293. [PubMed] [Google Scholar]
- 65.Seidman JD, Kumar D, Cosin JA, Winter WE, 3rd, Cargill C, Boice CR. Carcinomas of the female genital tract occurring after pelvic irradiation: a report of 15 cases. Int J Gynecol Pathol. 2006;25:293–297. doi: 10.1097/01.pgp.0000189240.03780.b1. [DOI] [PubMed] [Google Scholar]
- 66.Oh KJ, Kalinina A, Park NH, Bagchi S. Deregulation of eIF4E: 4E-BP1 in differentiated human papillomavirus-containing cells leads to high levels of expression of the E7 oncoprotein. J Virol. 2006;80:7079–7088. doi: 10.1128/JVI.02380-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Divya CS, Pillai MR. Antitumor action of curcumin in human papillomavirus associated cells involves downregulation of viral oncogenes, prevention of NFkB and AP-1 translocation, and modulation of apoptosis. Mol Carcinog. 2006;45:320–332. doi: 10.1002/mc.20170. [DOI] [PubMed] [Google Scholar]
- 68.O'Neill CJ, McCluggage WG. p16 expression in the female genital tract and its value in diagnosis. Adv Anat Pathol. 2006;13:8–15. doi: 10.1097/01.pap.0000201828.92719.f3. [DOI] [PubMed] [Google Scholar]
- 69.Hellman K, Silfversward C, Nilsson B, Hellstrom AC, Frankendal B, Pettersson F. Primary carcinoma of the vagina: factors influencing the age at diagnosis. The Radiumhemmet series 1956–96. Int J Gynecol Cancer. 2004;14:491–501. doi: 10.1111/j.1048-891x.2004.014310.x. [DOI] [PubMed] [Google Scholar]
- 70.Sirimai K, Chalermchockcharoenkit A, Roongpisuthipong A, Pongprasobchai S. Associated risk factors of human papillomavirus cervical infection among human immunodificiency virus-seropositive women at Siriraj Hospital. J Med Assoc Thai. 2004;87:270–276. [PubMed] [Google Scholar]
- 71.Katiyar S, Thelma BK, Murthy NS, Hedau S, Jain N, Gopalkrishna V, Husain SA, Das BC. Polymorphism of the p53 codon 72 Arg/Pro and the risk of HPV type 16/18-associated cervical and oral cancer in India. Mol Cell Biochem. 2003;252:117–124. doi: 10.1023/a:1025546610920. [DOI] [PubMed] [Google Scholar]
- 72.Im SS, Wilczynski SP, Burger RA, Monk BJ. Early stage cervical cancers containing human papillomavirus type 18 DNA have more nodal metastasis and deeper stromal invasion. Clin Cancer Res. 2003;9:4145–4150. [PubMed] [Google Scholar]
- 73.Roteli-Martins CM, Derchain SF, Martinez EZ, Siqueira SA, Alves VA, Syrjanen KJ. Morphological diagnosis of HPV lesions and cervical intraepithelial neoplasia (CIN) is highly reproducible. Clin Exp Obstet Gynecol. 2001;28:78–80. [PubMed] [Google Scholar]
- 74.Iwamasa T, Miyagi J, Tsuhako K, Kinjo T, Kamada Y, Hirayasu T, Genka K. Prognostic implication of human papillomavirus infection in squamous cell carcinoma of the lung. Pathol Res Pract. 2000;196:209–218. doi: 10.1016/S0344-0338(00)80069-2. [DOI] [PubMed] [Google Scholar]
- 75.Zumbach K, Kisseljov F, Sacharova O, Shaichaev G, Semjonova L, Pavlova L, Pawlita M. Antibodies against oncoproteins E6 and E7 of human papillomavirus types 16 and 18 in cervical-carcinoma patients from Russia. Int J Cancer. 2000;85:313–318. doi: 10.1002/(sici)1097-0215(20000201)85:3<313::aid-ijc3>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 76.Kleine-Lowinski K, Gillitzer R, Kuhne-Heid R, Rosl F. Monocyte-chemo-attractant-protein-1 (MCP-1)-gene expression in cervical intra-epithelial neoplasias and cervical carcinomas. Int J Cancer. 1999;82:6–11. doi: 10.1002/(sici)1097-0215(19990702)82:1<6::aid-ijc2>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 77.Chen Z, Kamath P, Zhang S, St John L, Adler-Storthz K, Shillitoe EJ. Effects on tumor cells of ribozymes that cleave the RNA transcripts of human papillomavirus type 18. Cancer Gene Ther. 1996;3:18–23. [PubMed] [Google Scholar]
- 78.Prasad CJ, Sheets E, Selig AM, McArthur MC, Crum CP. The binucleate squamous cell: histologic spectrum and relationship to low-grade squamous intraepithelial lesions. Mod Pathol. 1993;6:313–317. [PubMed] [Google Scholar]
- 79.Macri CI, Cook NS, Walker JL, Berman ML, Patton TJ, Jr, Wilczynski SP. Analysis of fine-needle aspirates for HPV by PCR may be useful in diagnosis of metastatic gynecologic malignancies. Gynecol Oncol. 1992;46:372–376. doi: 10.1016/0090-8258(92)90235-b. [DOI] [PubMed] [Google Scholar]
- 80.Arends MJ, Donaldson YK, Duvall E, Wyllie AH, Bird CC. HPV in full thickness cervical biopsies: high prevalence in CIN 2 and CIN 3 detected by a sensitive PCR method. J Pathol. 1991;165:301–309. doi: 10.1002/path.1711650405. [DOI] [PubMed] [Google Scholar]
- 81.Ward BE, Burkett B, Petersen C, Nuckols ML, Brennan C, Birch LM, Crum CP. Cytologic correlates of cervical papillomavirus infection. Int J Gynecol Pathol. 1990;9:297–305. doi: 10.1097/00004347-199010000-00001. [DOI] [PubMed] [Google Scholar]
- 82.Byrne MA, Parry GC, Morse A, Taylor-Robinson D, Malcolm AD, Coleman DV. A prospective study of human papillomavirus infection of the cervix. Cytopathology. 1990;1:329–337. doi: 10.1111/j.1365-2303.1990.tb00370.x. [DOI] [PubMed] [Google Scholar]
- 83.Balakrishnan L, Clauson R, Weiland T, Bianco M, Milavetz B. Sexually transmitted Human Papillomavirus type variations resulting in high grade cervical dysplasia in North-East North Dakota and North-West Minnesota. Virol J. 2006;3:46. doi: 10.1186/1743-422X-3-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ortholan C, Francois E, Gerard JP. [Preneoplastic anal lesions and anal canal carcinoma] Bull Cancer. 2003;90:405–411. [PubMed] [Google Scholar]
- 85.Grce M, Husnjak K, Milutin N, Matovina M. [Detection of human papillomaviruses and other agents causing sexually transmitted diseases with molecular diagnosis methods] Acta Med Croatica. 2003;57:295–301. [PubMed] [Google Scholar]
- 86.Orth G, Jablonska S, Breitburd F, Favre M, Croissant O. The human papillomaviruses. Bull Cancer. 1978;65:151–164. [PubMed] [Google Scholar]
- 87.Aubin F, Laurent R. [Human papillomavirus-associated cutaneous lesions] Rev Prat. 2006;56:1905–1913. [PubMed] [Google Scholar]
- 88.Ahmed AM, Madkan V, Tyring SK. Human papillomaviruses and genital disease. Dermatol Clin. 2006;24:157–165. doi: 10.1016/j.det.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 89.Shahmahmoudi S, Mahmoodi M, Azad TM, Rad KS, Tabatabaie H, Sarijlou M, Pour YY, Yousefi M, Ghasemi M, Far KJ, Nategh R. Prevalence of mucosal types of human papillomavirus in skin lesions in north part of Iran. Cancer Lett. 2007;247:72–76. doi: 10.1016/j.canlet.2006.03.023. [DOI] [PubMed] [Google Scholar]
- 90.Majewski S, Jablonska S. Do epidermodysplasia verruciformis human papillomaviruses contribute to malignant and benign epidermal proliferations? Arch Dermatol. 2002;138:649–654. doi: 10.1001/archderm.138.5.649. [DOI] [PubMed] [Google Scholar]
- 91.Jimenez C, Correnti M, Salma N, Cavazza ME, Perrone M. Detection of human papillomavirus DNA in benign oral squamous epithelial lesions in Venezuela. J Oral Pathol Med. 2001;30:385–388. doi: 10.1034/j.1600-0714.2001.300701.x. [DOI] [PubMed] [Google Scholar]
- 92.Weber F, Fuchs PG, Pfister HJ, Hintner H, Fritsch P, Hoepfl R. Human papillomavirus infection in Netherton's syndrome. Br J Dermatol. 2001;144:1044–1049. doi: 10.1046/j.1365-2133.2001.04196.x. [DOI] [PubMed] [Google Scholar]
- 93.Manavi M, Baghestanian M, Kucera E, Berger A, Schatten C, Pischinger K, Czerwenka K. Papilloma virus and c-erbB-2 expression in diseases of the mammary nipple. Anticancer Res. 2001;21:797–801. [PubMed] [Google Scholar]
- 94.Pinto PA, Mellinger BC. HPV in the male patient. Urol Clin North Am. 1999;26:797–807. doi: 10.1016/s0094-0143(05)70220-2. [DOI] [PubMed] [Google Scholar]
- 95.Frisch M, Glimelius B, van den Brule AJ, Wohlfahrt J, Meijer CJ, Walboomers JM, Adami HO, Melbye M. Benign anal lesions, inflammatory bowel disease and risk for high-risk human papillomavirus-positive and – negative anal carcinoma. Br J Cancer. 1998;78:1534–1538. doi: 10.1038/bjc.1998.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ravakhah K, Midamba F, West BC. Esophageal papillomatosis from human papilloma virus proven by polymerase chain reaction. Am J Med Sci. 1998;316:285–288. doi: 10.1097/00000441-199810000-00010. [DOI] [PubMed] [Google Scholar]
- 97.Beutner KR, Tyring S. Human papillomavirus and human disease. Am J Med. 1997;102:9–15. doi: 10.1016/s0002-9343(97)00178-2. [DOI] [PubMed] [Google Scholar]
- 98.Ostrow RS, Faras AJ. The molecular biology of human papillomaviruses and the pathogenesis of genital papillomas and neoplasms. Cancer Metastasis Rev. 1987;6:383–395. doi: 10.1007/BF00144271. [DOI] [PubMed] [Google Scholar]
- 99.McDougall JK, Beckmann AM, Kiviat NB. Methods for diagnosing papillomavirus infection. Ciba Found Symp. 1986;120:86–103. doi: 10.1002/9780470513309.ch7. [DOI] [PubMed] [Google Scholar]
- 100.van Voorst Vader PC, Orth G, Dutronquay V, Driessen LH, Eggink HF, Kallenberg CG, The TH. Epidermodysplasia verruciformis. Skin carcinoma containing human papillomavirus type 5 DNA sequences and primary hepatocellular carcinoma associated with chronic hepatitis B virus infection in a patient. Acta Derm Venereol. 1986;66:231–236. [PubMed] [Google Scholar]
- 101.Jenson AB, Lim LY, Lancaster WD. Role of papilloma virus in proliferative squamous lesions. Surv Synth Pathol Res. 1985;4:8–13. doi: 10.1159/000156961. [DOI] [PubMed] [Google Scholar]
- 102.Winkler B, Capo V, Reumann W, Ma A, La Porta R, Reilly S, Green PM, Richart RM, Crum CP. Human papillomavirus infection of the esophagus. A clinicopathologic study with demonstration of papillomavirus antigen by the immunoperoxidase technique. Cancer. 1985;55:149–155. doi: 10.1002/1097-0142(19850101)55:1<149::aid-cncr2820550123>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 103.Evans MI, Krivchenia EL, Yaron Y. Screening. Best Pract Res Clin Obstet Gynaecol. 2002;16:645–657. doi: 10.1053/beog.2002.0330. [DOI] [PubMed] [Google Scholar]
- 104.Falkenberry SS. Cancer in pregnancy. Surg Oncol Clin N Am. 1998;7:375–397. [PubMed] [Google Scholar]
- 105.Stone KM. Avoiding sexually transmitted diseases. Obstet Gynecol Clin N Am. 1990;17:789–799. [PubMed] [Google Scholar]
- 106.Mochizuki Y, Noguchi S, Yokoyama S, Murakami N, Moriuchi A, Aisaka K, Yamashita H, Nakayama I. Cervical teratoma in a fetus and an adult. Two case reports and review of literature. Acta Pathol Jpn. 1986;36:935–943. doi: 10.1111/j.1440-1827.1986.tb03127.x. [DOI] [PubMed] [Google Scholar]
- 107.Giampieri S, Storey A. Repair of UV-induced thymine dimers is compromised in cells expressing the E6 protein from human papillomaviruses types 5 and 18. Br J Cancer. 2004;90:2203–2209. doi: 10.1038/sj.bjc.6601829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Borras C, Bares JP, Rudder D, Amer A, Millan F, Abuchaibe O. Clinical effects in a cohort of cancer patients overexposed during external beam pelvic radiotherapy. Int J Radiat Oncol Biol Phys. 2004;59:538–550. doi: 10.1016/j.ijrobp.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 109.Mut M, Cataltepe O, Soylemezoglu F, Akalan N, Ozgen T. Radiation-induced malignant triton tumor associated with severe spinal cord compression. Case report and review of the literature. J Neurosurg. 2004;100:298–302. [PubMed] [Google Scholar]
- 110.Nomayr A, Lell M, Sweeney R, Bautz W, Lukas P. MRI appearance of radiation-induced changes of normal cervical tissues. Eur Radiol. 2001;11:1807–1817. doi: 10.1007/s003300000728. [DOI] [PubMed] [Google Scholar]
- 111.Pirhonen JP, Grenman SA, Bredbacka AB, Bahado-Singh RO, Salmi TA. Effects of external radiotherapy on uterine blood flow in patients with advanced cervical carcinoma assessed by color Doppler ultrasonography. Cancer. 1995;76:67–71. doi: 10.1002/1097-0142(19950701)76:1<67::aid-cncr2820760109>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 112.Figini HA, Grosz D. [Cervical myelopathies caused by radiation. Report of 3 cases] Prensa Med Argent. 1970;57:1755–1758. [PubMed] [Google Scholar]
- 113.Munoz N, Castellsague X, de Gonzalez AB, Gissmann L. HPV in the etiology of human cancer. Vaccine. 2006;24:S1–S10. doi: 10.1016/j.vaccine.2006.05.115. [DOI] [PubMed] [Google Scholar]
- 114.Lacey JV, Jr., Frisch M, Brinton LA, Abbas FM, Barnes WA, Gravitt PE, Greenberg MD, Greene SM, Hadjimichael OC, McGowan L, Mortel R, Schwartz PE, Zaino RJ, Hildesheim A. Associations between smoking and adenocarcinomas and squamous cell carcinomas of the uterine cervix (United States) Cancer Causes Control. 2001;12:153–161. doi: 10.1023/a:1008918310055. [DOI] [PubMed] [Google Scholar]
- 115.Ponten J, Guo Z. Precancer of the human cervix. Cancer Surv. 1998;32:201–229. [PubMed] [Google Scholar]
- 116.Munk C, Svare EI, Poll P, Bock JE, Kjaer SK. History of genital warts in 10,838 women 20 to 29 years of age from the general population. Risk factors and association with Papanicolaou smear history. Sex Transm Dis. 1997;24:567–572. doi: 10.1097/00007435-199711000-00003. [DOI] [PubMed] [Google Scholar]
- 117.Hellberg D, Borendal N, Sikstrom B, Nilsson S, Mardh PA. Comparison of women with cervical human papillomavirus infection and genital warts. I. Some behavioural factors and clinical findings. Genitourin Med. 1995;71:88–91. doi: 10.1136/sti.71.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cresanta JL. Epidemiology of cancer in the United States. Prim Care. 1992;19:419–441. [PubMed] [Google Scholar]
- 119.Palan PR, Mikhail MS, Basu J, Romney SL. Plasma levels of antioxidant beta-carotene and alpha-tocopherol in uterine cervix dysplasias and cancer. Nutr Cancer. 1991;15:13–20. doi: 10.1080/01635589109514106. [DOI] [PubMed] [Google Scholar]
- 120.Moscicki AB. Cervical cytology testing in teens. Curr Opin Obstet Gynecol. 2005;17:471–475. doi: 10.1097/01.gco.0000179665.90778.f7. [DOI] [PubMed] [Google Scholar]
- 121.Guido R. Guidelines for screening and treatment of cervical disease in the adolescent. J Pediatr Adolesc Gynecol. 2004;17:303–311. doi: 10.1016/j.jpag.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 122.Gray SH, Walzer TB. New strategies for cervical cancer screening in adolescents. Curr Opin Pediatr. 2004;16:344–349. doi: 10.1097/01.mop.0000133078.40007.2b. [DOI] [PubMed] [Google Scholar]
- 123.Moscicki AB. Cervical cytology screening in teens. Curr Womens Health Rep. 2003;3:433–437. [PubMed] [Google Scholar]
- 124.Schiffman M, Kjaer SK. Natural history of anogenital human papillomavirus infection and neoplasia. J Natl Cancer Inst Monogr. 2003:14–19. doi: 10.1093/oxfordjournals.jncimonographs.a003476. [DOI] [PubMed] [Google Scholar]
- 125.Chang AR, Sewell H. Cervical cytology screening in Vietnamese asylum seekers in a Hong Kong detention center. Population demographics and historical perspectives. Acta Cytol. 2002;46:475–480. doi: 10.1159/000326864. [DOI] [PubMed] [Google Scholar]
- 126.Arends MJ, Buckley CH, Wells M. Aetiology, pathogenesis, and pathology of cervical neoplasia. J Clin Pathol. 1998;51:96–103. doi: 10.1136/jcp.51.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Economos K, Perez-Veridiano N, Mann M, Delke I, Tancer ML. Abnormal cervical cytology in adolescents. A 15-year experience. J Reprod Med. 1994;39:973–976. [PubMed] [Google Scholar]
- 128.Schiffman MH, Bauer HM, Hoover RN, Glass AG, Cadell DM, Rush BB, Scott DR, Sherman ME, Kurman RJ, Wacholder S, et al. Epidemiologic evidence showing that human papillomavirus infection causes most cervical intraepithelial neoplasia. J Natl Cancer Inst. 1993;85:958–964. doi: 10.1093/jnci/85.12.958. [DOI] [PubMed] [Google Scholar]
- 129.Schneider A, Koutsky LA. Natural history and epidemiological features of genital HPV infection. IARC; 1992. pp. 25–52. [PubMed] [Google Scholar]
- 130.Chou P. [Review on risk factors of cervical cancer] Zhonghua Yi Xue Za Zhi (Taipei) 1991;48:81–88. [PubMed] [Google Scholar]
- 131.zur Hausen H. Human genital cancer: synergism between two virus infections or synergism between a virus infection and initiating events? Lancet. 1982;2:1370–1372. doi: 10.1016/s0140-6736(82)91273-9. [DOI] [PubMed] [Google Scholar]
- 132.Zheng S, Zhang C, Li L, Han C, Jing J, Zhu Q. [The relationship of cervical cancer with pathogen infectious, cytokine and Se] Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi. 2002;16:179–183. [PubMed] [Google Scholar]
- 133.Zhan D, Santin AD, Liu Y, Parham GP, Li C, Meyers C, Hermonat PL. Binding of the human papillomavirus type 16 p97 promoter by the adeno-associated virus Rep78 major regulatory protein correlates with inhibition. J Biol Chem. 1999;274:31619–31624. doi: 10.1074/jbc.274.44.31619. [DOI] [PubMed] [Google Scholar]
- 134.Zbar AP, Fenger C, Efron J, Beer-Gabel M, Wexner SD. The pathology and molecular biology of anal intraepithelial neoplasia: comparisons with cervical and vulvar intraepithelial carcinoma. Int J Colorectal Dis. 2002;17:203–215. doi: 10.1007/s00384-001-0369-0. [DOI] [PubMed] [Google Scholar]
- 135.Zarcone R, Cardone G, Bellini P, Carfora E, Fortuna G, Raucci F. [Incidence of HPV and CIN in HIV positive women] Minerva Ginecol. 1995;47:477–480. [PubMed] [Google Scholar]
- 136.Zarcone R, Bellini P, Carfora E, Longo M, Monarca M, Tomasillo G, Lizza R. [Incidence of CIN in HIV-positive women] Minerva Ginecol. 1998;50:181–183. [PubMed] [Google Scholar]
- 137.Wilbanks GD. In vitro studies on human cervical epithelium, benign and neoplastic. Am J Obstet Gynecol. 1975;121:771–788. [PubMed] [Google Scholar]
- 138.Heard I. Cervical disease and cancer in HIV positive women. Recommendations for screening and diagnosis. Med Wieku Rozwoj. 2003;7:479–485. [PubMed] [Google Scholar]
- 139.Moscicki AB, Schiffman M, Kjaer S, Villa LL. Updating the natural history of HPV and anogenital cancer. Vaccine. 2006;24:S42–51. doi: 10.1016/j.vaccine.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 140.Fox PA, Tung MY. Human papillomavirus: burden of illness and treatment cost considerations. Am J Clin Dermatol. 2005;6:365–381. doi: 10.2165/00128071-200506060-00004. [DOI] [PubMed] [Google Scholar]
- 141.Sinclair KA, Woods CR, Kirse DJ, Sinal SH. Anogenital and respiratory tract human papillomavirus infections among children: age, gender, and potential transmission through sexual abuse. Pediatrics. 2005;116:815–825. doi: 10.1542/peds.2005-0652. [DOI] [PubMed] [Google Scholar]
- 142.Spano JP, Marcelin AG, Carcelin G. [HPV and cancer.] Bull Cancer. 2005;92:59–64. [PubMed] [Google Scholar]
- 143.Tsuchiya H, Tomita Y, Shirasawa H, Tanzawa H, Sato K, Simizu B. Detection of human papillomavirus in head and neck tumors with DNA hybridization and immunohistochemical analysis. Oral Surg Oral Med Oral Pathol. 1991;71:721–725. doi: 10.1016/0030-4220(91)90281-g. [DOI] [PubMed] [Google Scholar]
- 144.Watts SL, Brewer EE, Fry TL. Human papillomavirus DNA types in squamous cell carcinomas of the head and neck. Oral Surg Oral Med Oral Pathol. 1991;71:701–707. doi: 10.1016/0030-4220(91)90278-k. [DOI] [PubMed] [Google Scholar]
- 145.Bradford CR, Zacks SE, Androphy EJ, Gregoire L, Lancaster WD, Carey TE. Human papillomavirus DNA sequences in cell lines derived from head and neck squamous cell carcinomas. Otolaryngol Head Neck Surg. 1991;104:303–310. doi: 10.1177/019459989110400304. [DOI] [PubMed] [Google Scholar]
- 146.Ishibashi T, Matsushima S, Tsunokawa Y, Asai M, Nomura Y, Sugimura T, Terada M. Human papillomavirus DNA in squamous cell carcinoma of the upper aerodigestive tract. Arch Otolaryngol Head Neck Surg. 1990;116:294–298. doi: 10.1001/archotol.1990.01870030058009. [DOI] [PubMed] [Google Scholar]
- 147.Bradford CR, Hoffman HT, Wolf GT, Carey TE, Baker SR, McClatchey KD. Squamous carcinoma of the head and neck in organ transplant recipients: possible role of oncogenic viruses. Laryngoscope. 1990;100:190–194. doi: 10.1288/00005537-199002000-00016. [DOI] [PubMed] [Google Scholar]
- 148.Rogo KO, Nyansera PN. Congenital condylomata acuminata with meconium staining of amniotic fluid and fetal hydrocephalus: case report. East Afr Med J. 1989;66:411–413. [PubMed] [Google Scholar]
- 149.Brandsma JL, Abramson AL. Association of papillomavirus with cancers of the head and neck. Arch Otolaryngol Head Neck Surg. 1989;115:621–625. doi: 10.1001/archotol.1989.01860290079018. [DOI] [PubMed] [Google Scholar]
- 150.Milde-Langosch KM, Loning T, Meichsner M, Henke RP. [HPV infections in tumors of the upper respiratory and digestive tract. In situ hybridization and dot-blot hybridization with biotinylated DNA probes] Acta Histochem Suppl. 1989;37:103–108. [PubMed] [Google Scholar]
- 151.Lindeberg H, Fey SJ, Ottosen PD, Mose Larsen P. Human papilloma virus (HPV) and carcinomas of the head and neck. Clin Otolaryngol Allied Sci. 1988;13:447–454. doi: 10.1111/j.1365-2273.1988.tb00318.x. [DOI] [PubMed] [Google Scholar]
- 152.Lee NK, Ritter DB, Gross AE, Myssiorek DJ, Kadish AS, Burk RD. Head and neck squamous cell carcinomas associated with human papillomaviruses and an increased incidence of cervical pathology. Otolaryngol Head Neck Surg. 1988;99:296–301. doi: 10.1177/019459988809900306. [DOI] [PubMed] [Google Scholar]
- 153.Chang F, Syrjanen S, Shen Q, Ji HX, Syrjanen K. Human papillomavirus (HPV) DNA in esophageal precancer lesions and squamous cell carcinomas from China. Int J Cancer. 1990;45:21–25. doi: 10.1002/ijc.2910450106. [DOI] [PubMed] [Google Scholar]
- 154.Fekete F, Chazouilleres O, Ganthier V, Molas G, Potet F. [A case of esophageal papillomatosis in adults] Gastroenterol Clin Biol. 1988;12:66–70. [PubMed] [Google Scholar]
- 155.Syrjanen KJ. [Human papillomavirus (HPV) infections and their associations with squamous cell neoplasia] Arch Geschwulstforsch. 1987;57:417–444. [PubMed] [Google Scholar]
- 156.Hille JJ, Margolius KA, Markowitz S, Isaacson C. Human papillomavirus infection related to oesophageal carcinoma in black South Africans. A preliminary study. S Afr Med J. 1986;69:417–420. [PubMed] [Google Scholar]
- 157.Ozols RF, Herbst RS, Colson YL, Gralow J, Bonner J, Curran WJ, Jr., Eisenberg BL, Ganz PA, Kramer BS, Kris MG, Markman M, Mayer RJ, Raghavan D, Reaman GH, Sawaya R, Schilsky RL, Schuchter LM, Sweetenham JW, Vahdat LT, Winn RJ. Clinical cancer advances 2006: major research advances in cancer treatment, prevention, and screening–a report from the American Society of Clinical Oncology. J Clin Oncol. 2007;25:146–162. doi: 10.1200/JCO.2006.09.7030. [DOI] [PubMed] [Google Scholar]
- 158.Kanitakis J, Euvrard S, Chouvet B, Butnaru AC, Claudy A. Merkel cell carcinoma in organ-transplant recipients: report of two cases with unusual histological features and literature review. J Cutan Pathol. 2006;33:686–694. doi: 10.1111/j.1600-0560.2006.00529.x. [DOI] [PubMed] [Google Scholar]
- 159.Orth G. Genetics of epidermodysplasia verruciformis: Insights into host defense against papillomaviruses. Semin Immunol. 2006;18:362–374. doi: 10.1016/j.smim.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 160.Yanagi T, Shibaki A, Tsuji-Abe Y, Yokota K, Shimizu H. Epidermodysplasia verruciformis and generalized verrucosis: the same disease? Clin Exp Dermatol. 2006;31:390–393. doi: 10.1111/j.1365-2230.2006.02100.x. [DOI] [PubMed] [Google Scholar]
- 161.Bologna-Molina RE, Castaneda-Castaneira RE, Molina-Frechero N, Perez-Rodriguez E. [Human papilloma virus and its association with oral cancer] Rev Med Inst Mex Seguro Soc. 2006;44:147–153. [PubMed] [Google Scholar]
- 162.Cassarino DS, Derienzo DP, Barr RJ. Cutaneous squamous cell carcinoma: a comprehensive clinicopathologic classification–part two. J Cutan Pathol. 2006;33:261–279. doi: 10.1111/j.0303-6987.2006.00516.x. [DOI] [PubMed] [Google Scholar]
- 163.Tan HH, Goh CL. Viral infections affecting the skin in organ transplant recipients: epidemiology and current management strategies. Am J Clin Dermatol. 2006;7:13–29. doi: 10.2165/00128071-200607010-00003. [DOI] [PubMed] [Google Scholar]
- 164.Cassarino DS, Derienzo DP, Barr RJ. Cutaneous squamous cell carcinoma: a comprehensive clinicopathologic classification. Part one. J Cutan Pathol. 2006;33:191–206. doi: 10.1111/j.0303-6987.2006.00516_1.x. [DOI] [PubMed] [Google Scholar]
- 165.Akgul B, Cooke JC, Storey A. HPV-associated skin disease. J Pathol. 2006;208:165–175. doi: 10.1002/path.1893. [DOI] [PubMed] [Google Scholar]
- 166.Struijk L, ter Schegget J, Bouwes Bavinck JN, Feltkamp MC. [Human papillomavirus in the aetiology of skin cancer] Ned Tijdschr Geneeskd. 2005;149:518–522. [PubMed] [Google Scholar]
- 167.Smith JW, Torres JE, Holmquist ND. Herpes simplex virus type 2 and human cervical cancer: relationship between cellular and immune assays for the detection of previous infection. J Natl Cancer Inst. 1981;66:1031–1036. doi: 10.1093/jnci/66.6.1031. [DOI] [PubMed] [Google Scholar]
- 168.Smith JW, Torres JE, Holmquist ND. Association of Herpes simplex virus (HSV) with cervical cancer by lymphocyte reactivity with HSV-1 and HSV-2 antigens. Am J Epidemiol. 1979;110:141–147. doi: 10.1093/oxfordjournals.aje.a112798. [DOI] [PubMed] [Google Scholar]
- 169.Smith JW. Herpes simplex virus. An expanding relationship to human cancer. J Reprod Med. 1983;28:116–122. [PubMed] [Google Scholar]
- 170.Smith JS, Herrero R, Bosetti C, Munoz N, Bosch FX, Eluf-Neto J, Castellsague X, Meijer CJ, Van den Brule AJ, Franceschi S, Ashley R. Herpes simplex virus-2 as a human papillomavirus cofactor in the etiology of invasive cervical cancer. J Natl Cancer Inst. 2002;94:1604–1613. doi: 10.1093/jnci/94.21.1604. [DOI] [PubMed] [Google Scholar]
- 171.zur Hausen H. Intracellular surveillance of persisting viral infections. Human genital cancer results from deficient cellular control of papillomavirus gene expression. Lancet. 1986;2:489–491. doi: 10.1016/s0140-6736(86)90360-0. [DOI] [PubMed] [Google Scholar]
- 172.Vecchione A, Cermele C, Giovagnoli MR, Valli C, Alimandi M, Carico E, Esposito DL, Mariani-Costantini R, French D. p53 expression and genetic evidence for viral infection in intraepithelial neoplasia of the uterine cervix. Gynecol Oncol. 1994;55:343–348. doi: 10.1006/gyno.1994.1304. [DOI] [PubMed] [Google Scholar]
- 173.Jones C, Zhu F, Dhanwada KR. Analysis of a herpes simplex virus 2 fragment from the open reading frame of the large subunit of ribonucleotide reductase with transcriptional regulatory activity. DNA Cell Biol. 1993;12:127–137. doi: 10.1089/dna.1993.12.127. [DOI] [PubMed] [Google Scholar]
- 174.Dhanwada KR, Garrett L, Smith P, Thompson KD, Doster A, Jones C. Characterization of human keratinocytes transformed by high risk human papillomavirus types 16 or 18 and herpes simplex virus type 2. J Gen Virol. 1993;74:955–963. doi: 10.1099/0022-1317-74-6-955. [DOI] [PubMed] [Google Scholar]
- 175.Jha PK, Beral V, Peto J, Hack S, Hermon C, Deacon J, Mant D, Chilvers C, Vessey MP, Pike MC, et al. Antibodies to human papillomavirus and to other genital infectious agents and invasive cervical cancer risk. Lancet. 1993;341:1116–1118. doi: 10.1016/0140-6736(93)93128-n. [DOI] [PubMed] [Google Scholar]
- 176.Dillner J, Lenner P, Lehtinen M, Eklund C, Heino P, Wiklund F, Hallmans G, Stendahl U. A population-based seroepidemiological study of cervical cancer. Cancer Res. 1994;54:134–141. [PubMed] [Google Scholar]
- 177.Daling JR, Madeleine MM, McKnight B, Carter JJ, Wipf GC, Ashley R, Schwartz SM, Beckmann AM, Hagensee ME, Mandelson MT, Galloway DA. The relationship of human papillomavirus-related cervical tumors to cigarette smoking, oral contraceptive use, and prior herpes simplex virus type 2 infection. Cancer Epidemiol Biomarkers Prev. 1996;5:541–548. [PubMed] [Google Scholar]
- 178.Hildesheim A, Mann V, Brinton LA, Szklo M, Reeves WC, Rawls WE. Herpes simplex virus type 2: a possible interaction with human papillomavirus types 16/18 in the development of invasive cervical cancer. Int J Cancer. 1991;49:335–340. doi: 10.1002/ijc.2910490304. [DOI] [PubMed] [Google Scholar]
- 179.Lehtinen M, Dillner J, Knekt P, Luostarinen T, Aromaa A, Kirnbauer R, Koskela P, Paavonen J, Peto R, Schiller JT, Hakama M. Serologically diagnosed infection with human papillomavirus type 16 and risk for subsequent development of cervical carcinoma: nested case-control study. Br Med J. 1996;312:537–539. doi: 10.1136/bmj.312.7030.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Lehtinen M, Koskela P, Jellum E, Bloigu A, Anttila T, Hallmans G, Luukkaala T, Thoresen S, Youngman L, Dillner J, Hakama M. Herpes simplex virus and risk of cervical cancer: a longitudinal, nested case-control study in the nordic countries. Am J Epidemiol. 2002;156:687–692. doi: 10.1093/aje/kwf098. [DOI] [PubMed] [Google Scholar]
- 181.Szczucinski A, Losy J. [Infectious agents in the pathogenesis of multiple sclerosis] Przegl Epidemiol. 2006;60:160–165. [PubMed] [Google Scholar]
- 182.Soldan SS, Jacobson S. Role of viruses in etiology and pathogenesis of multiple sclerosis. Adv Virus Res. 2001;56:517–555. doi: 10.1016/S0065-3527(01)56037-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Enbom M. Human herpesvirus 6 in the pathogenesis of multiple sclerosis. Apmis. 2001;109:401–411. doi: 10.1034/j.1600-0463.2001.090601.x. [DOI] [PubMed] [Google Scholar]
- 184.Azoulay-Cayla A. [Is multiple sclerosis a disease of viral origin?] Pathol Biol (Paris) 2000;48:4–14. [PubMed] [Google Scholar]
- 185.Okuno T, Sao H, Asada H, Shiraki K, Takahashi M, Yamanishi K. Analysis of a glycoprotein of human herpesvirus 6 (HHV-6) using monoclonal antibodies. Virology. 1990;176:625–628. doi: 10.1016/0042-6822(90)90033-n. [DOI] [PubMed] [Google Scholar]
- 186.Chiang WT, Chen HM, Hsieh CY, Tsai WS, Wei PY, Alexander ER. Cytomegalovirus infection of the uterine cervix: local cervical infection and antibody response. Int J Gynaecol Obstet. 1981;19:177–180. doi: 10.1016/0020-7292(81)90059-x. [DOI] [PubMed] [Google Scholar]
- 187.Han CP, Tsao YP, Sun CA, Ng HT, Chen SL. Human papillomavirus, cytomegalovirus and herpes simplex virus infections for cervical cancer in Taiwan. Cancer Lett. 1997;120:217–221. doi: 10.1016/s0304-3835(97)00312-1. [DOI] [PubMed] [Google Scholar]
- 188.Chan PK, Chan MY, Li WW, Chan DP, Cheung JL, Cheng AF. Association of human beta-herpesviruses with the development of cervical cancer: bystanders or cofactors. J Clin Pathol. 2001;54:48–53. doi: 10.1136/jcp.54.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Yang YY, Koh LW, Tsai JH, Tsai CH, Wong EF, Lin SJ, Yang CC. Correlation of viral factors with cervical cancer in Taiwan. J Microbiol Immunol Infect. 2004;37:282–287. [PubMed] [Google Scholar]
- 190.Yadav M, Arivananthan M, Kumar S. HHV-6 antigen and viral DNA detected in cervical cells from archived tissue using histochemical staining and hybridization. Clin Diagn Virol. 1996;7:23–33. doi: 10.1016/s0928-0197(96)00250-4. [DOI] [PubMed] [Google Scholar]
- 191.Wang J, Jones C, Norcross M, Bohnlein E, Razzaque A. Identification and characterization of a human herpesvirus 6 gene segment capable of transactivating the human immunodeficiency virus type 1 long terminal repeat in an Sp1 binding site-dependent manner. J Virol. 1994;68:1706–1713. doi: 10.1128/jvi.68.3.1706-1713.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Wang H, Chen M, Berneman ZN, Delgado G, DiPaolo JA. Detection of human herpesvirus-6 in paraffin-embedded tissue of cervical cancer by polymerase chain reaction. J Virol Methods. 1994;47:297–305. doi: 10.1016/0166-0934(94)90026-4. [DOI] [PubMed] [Google Scholar]
- 193.Leach CT, Sumaya CV, Brown NA. Human herpesvirus-6: clinical implications of a recently discovered, ubiquitous agent. J Pediatr. 1992;121:173–181. doi: 10.1016/s0022-3476(05)81184-9. [DOI] [PubMed] [Google Scholar]
- 194.Leach CT, Pollock BH, McClain KL, Parmley RT, Murphy SB, Jenson HB. Human herpesvirus 6 and cytomegalovirus infections in children with human immunodeficiency virus infection and cancer. Pediatr Infect Dis J. 2002;21:125–132. doi: 10.1097/00006454-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 195.Leach CT, Newton ER, McParlin S, Jenson HB. Human herpesvirus 6 infection of the female genital tract. J Infect Dis. 1994;169:1281–1283. doi: 10.1093/infdis/169.6.1281. [DOI] [PubMed] [Google Scholar]
- 196.Shiraki K, Mukai T, Okuno T, Yamanishi K, Takahashi M. Physicochemical characterization of human herpesvirus 6 infectivity. J Gen Virol. 1991;72:169–172. doi: 10.1099/0022-1317-72-1-169. [DOI] [PubMed] [Google Scholar]
- 197.Okuno T, Shao H, Asada H, Shiraki K, Takahashi M, Yamanishi K. Analysis of human herpesvirus 6 glycoproteins recognized by monoclonal antibody OHV1. J Gen Virol. 1992;73:443–447. doi: 10.1099/0022-1317-73-2-443. [DOI] [PubMed] [Google Scholar]
- 198.Okuno T, Sao H, Yamanishi K. [Human herpes virus 6 (HHV-6)] Uirusu. 1991;41:65–76. doi: 10.2222/jsv.41.65. [DOI] [PubMed] [Google Scholar]
- 199.Okuno T, Oishi H, Hayashi K, Nonogaki M, Tanaka K, Yamanishi K. Human herpesviruses 6 and 7 in cervixes of pregnant women. J Clin Microbiol. 1995;33:1968–1970. doi: 10.1128/jcm.33.7.1968-1970.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Kurata T, Iwasaki T, Sata T, Wakabayashi T, Yamaguchi K, Okuno T, Yamanishi K, Takei Y. Viral pathology of human herpesvirus 6 infection. Adv Exp Med Biol. 1990;278:39–47. doi: 10.1007/978-1-4684-5853-4_5. [DOI] [PubMed] [Google Scholar]
- 201.Kapur N, Brooks DJ. Temporally-specific retrograde amnesia in two cases of discrete bilateral hippocampal pathology. Hippocampus. 1999;9:247–254. doi: 10.1002/(SICI)1098-1063(1999)9:3<247::AID-HIPO5>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 202.Tran-Thanh D, Koushik A, Provencher D, Drouin P, Dubuc-Lissoir J, Gauthier P, Allaire G, Kornegay J, Franco E, Coutlee F. Detection of human herpes virus type 6 DNA in precancerous lesions of the uterine cervix. J Med Virol. 2002;68:606–610. doi: 10.1002/jmv.10229. [DOI] [PubMed] [Google Scholar]
- 203.Santon Roldan A, De San Jose S, Gomez Sanz E, Fernandez Munoz R, Herrera P, Bellas Menendez C. [Human herpesvirus-8 detection in Kaposi's sarcoma, multiple myeloma, and lymphoproliferative syndromes occurring in immunocompetent and immunocompromised patients] Med Clin (Barc) 2002;119:241–244. doi: 10.1016/s0025-7753(02)73375-7. [DOI] [PubMed] [Google Scholar]
- 204.Romano N, Romano FM, Viviano E, Vitale F, Villafrate MR, Perna AM, Bonura F, Guttadauro R. Rare association of human herpesvirus 6 DNA with human papillomavirus DNA in cervical smears of women with normal and abnormal cytologies. J Clin Microbiol. 1996;34:1589–1591. doi: 10.1128/jcm.34.6.1589-1591.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Newton R, Ziegler J, Bourboulia D, Casabonne D, Beral V, Mbidde E, Carpenter L, Reeves G, Parkin DM, Wabinga H, Mbulaiteye S, Jaffe H, Weiss R, Boshoff C. The sero-epidemiology of Kaposi's sarcoma-associated herpesvirus (KSHV/HHV-8) in adults with cancer in Uganda. Int J Cancer. 2003;103:226–232. doi: 10.1002/ijc.10817. [DOI] [PubMed] [Google Scholar]
- 206.Enbom M, Strand A, Falk KI, Linde A. Detection of Epstein-Barr virus, but not human herpesvirus 8, DNA in cervical secretions from Swedish women by real-time polymerase chain reaction. Sex Transm Dis. 2001;28:300–306. doi: 10.1097/00007435-200105000-00013. [DOI] [PubMed] [Google Scholar]
- 207.Chen M, Wang H, Woodworth CD, Lusso P, Berneman Z, Kingma D, Delgado G, DiPaolo JA. Detection of human herpesvirus 6 and human papillomavirus 16 in cervical carcinoma. Am J Pathol. 1994;145:1509–1516. [PMC free article] [PubMed] [Google Scholar]
- 208.Berrington de Gonzalez A, Urban M, Sitas F, Blackburn N, Hale M, Patel M, Ruff P, Sur R, Newton R, Beral V. Antibodies against six human herpesviruses in relation to seven cancers in black South Africans: A case control study. Infect Agent Cancer. 2006;1:2. doi: 10.1186/1750-9378-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Beral V, Newton R. Overview of the epidemiology of immunodeficiency-associated cancers. J Natl Cancer Inst Monogr. 1998:1–6. doi: 10.1093/oxfordjournals.jncimonographs.a024164. [DOI] [PubMed] [Google Scholar]
- 210.Arivananthan M, Yadav M, Kumar S. Detection of HHV-6 genotypes by in situ hybridization with variant-specific oligonucleotide probes. J Virol Methods. 1997;66:5–14. doi: 10.1016/s0166-0934(97)02198-8. [DOI] [PubMed] [Google Scholar]
- 211.Taylor MM, Chohan B, Lavreys L, Hassan W, Huang ML, Corey L, Ashley Morrow R, Richardson BA, Mandaliya K, Ndinya-Achola J, Bwayo J, Kreiss J. Shedding of human herpesvirus 8 in oral and genital secretions from H IV-1-seropositive and -seronegative Kenyan women. J Infect Dis. 2004;190:484–488. doi: 10.1086/421466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Lanham S, Herbert A, Basarab A, Watt P. Detection of cervical infections in colposcopy clinic patients. J Clin Microbiol. 2001;39:2946–2950. doi: 10.1128/JCM.39.8.2946-2950.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Landers RJ, O'Leary JJ, Crowley M, Healy I, Annis P, Burke L, O'Brien D, Hogan J, Kealy WF, Lewis FA, et al. Epstein-Barr virus in normal, pre-malignant, and malignant lesions of the uterine cervix. J Clin Pathol. 1993;46:931–935. doi: 10.1136/jcp.46.10.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Hilton DA, Brown LJ, Pringle JH, Nandha H. Absence of Epstein-Barr virus in carcinoma of the cervix. Cancer. 1993;72:1946–1948. doi: 10.1002/1097-0142(19930915)72:6<1946::aid-cncr2820720625>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 215.Voog E, Ricksten A, Stenglein M, Jonassen F, Ternesten A, Ryd W, Lowhagen GB. Are acetowhite lesions of the cervix correlated to the presence of Epstein-Barr virus DNA? Int J STDAIDS. 1997;8:432–436. doi: 10.1258/0956462971920488. [DOI] [PubMed] [Google Scholar]
- 216.Shoji Y, Saegusa M, Takano Y, Hashimura M, Okayasu I. Detection of the Epstein-Barr virus genome in cervical neoplasia is closely related to the degree of infiltrating lymphoid cells: a polymerase chain reaction and in situ hybridization approach. Pathol Int. 1997;47:507–511. doi: 10.1111/j.1440-1827.1997.tb04532.x. [DOI] [PubMed] [Google Scholar]
- 217.Mansoor A, Stevenson MS, Li RZ, Frekko K, Weiss W, Ahmad M, Khan AH, Mushtaq S, Saleem M, Raffeld M, Kingma DW, Jaffe ES. Prevalence of Epstein-Barr viral sequences and EBV LMP1 oncogene deletions in Burkitt's lymphoma from Pakistan: epidemiological correlations. Hum Pathol. 1997;28:283–288. doi: 10.1016/s0046-8177(97)90125-8. [DOI] [PubMed] [Google Scholar]
- 218.Hamilton-Dutoit SJ, Rea D, Raphael M, Sandvej K, Delecluse HJ, Gisselbrecht C, Marelle L, van Krieken HJ, Pallesen G. Epstein-Barr virus-latent gene expression and tumor cell phenotype in acquired immunodeficiency syndrome-related non-Hodgkin's lymphoma. Correlation of lymphoma phenotype with three distinct patterns of viral latency. Am J Pathol. 1993;143:1072–1085. [PMC free article] [PubMed] [Google Scholar]
- 219.Audouin J, Prevot S, Brouland JP, Molina T, Le Tourneau A, Diebold J. [Contribution of immunohistochemistry and in situ hybridization techniques in diseases caused by or associated with Epstein-Barr virus] Arch Anat Cytol Pathol. 1992;40:95–104. [PubMed] [Google Scholar]
- 220.Smith JR, Kitchen VS, Botcherby M, Hepburn M, Wells C, Gor D, Forster SM, Harris JR, Steer P, Mason P. Is HIV infection associated with an increase in the prevalence of cervical neoplasia? Br J Obstet Gynaecol. 1993;100:149–153. doi: 10.1111/j.1471-0528.1993.tb15211.x. [DOI] [PubMed] [Google Scholar]
- 221.Smith C, Lilly S, Mann KP, Livingston E, Myers S, Lyerly HK, Miralles GD. AIDS-related malignancies. Ann Med. 1998;30:323–344. doi: 10.3109/07853899809029932. [DOI] [PubMed] [Google Scholar]
- 222.Southern SA, Herrington CS. Molecular events in uterine cervical cancer. Sex Transm Infect. 1998;74:101–109. doi: 10.1136/sti.74.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Poblet E, Alfaro L, Fernander-Segoviano P, Jimenez-Reyes J, Salido EC. Human papillomavirus-associated penile squamous cell carcinoma in HIV-positive patients. Am J Surg Pathol. 1999;23:1119–1123. doi: 10.1097/00000478-199909000-00016. [DOI] [PubMed] [Google Scholar]
- 224.Mayaud P, Gill DK, Weiss HA, Uledi E, Kopwe L, Todd J, ka-Gina G, Grosskurth H, Hayes RJ, Mabey DC, Lacey CJ. The interrelation of HIV, cervical human papillomavirus, and neoplasia among antenatal clinic attenders in Tanzania. Sex Transm Infect. 2001;77:248–254. doi: 10.1136/sti.77.4.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Mandelblatt JS, Kanetsky P, Eggert L, Gold K. Is HIV infection a cofactor for cervical squamous cell neoplasia? Cancer Epidemiol Biomarkers Prev. 1999;8:97–106. [PubMed] [Google Scholar]
- 226.Lacey CJ. Assessment of exposure to sexually transmitted agents other than human papillomavirus. IARC; 1992. pp. 93–105. [PubMed] [Google Scholar]
- 227.Harju L, Janne P, Kallio A, Laukkanen ML, Lautenschlager I, Mattinen S, Ranki A, Ranki M, Soares VR, Soderlund H, et al. Affinity-based collection of amplified viral DNA: application to the detection of human immunodeficiency virus type 1, human cytomegalovirus and human papillomavirus type 16. Mol Cell Probes. 1990;4:223–235. doi: 10.1016/0890-8508(90)90056-6. [DOI] [PubMed] [Google Scholar]
- 228.Desaintes C, Hallez S, Van Alphen P, Burny A. Transcriptional activation of several heterologous promoters by the E6 protein of human papillomavirus type 16. J Virol. 1992;66:325–333. doi: 10.1128/jvi.66.1.325-333.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Clarke B, Chetty R. Postmodern cancer: the role of human immunodeficiency virus in uterine cervical cancer. Mol Pathol. 2002;55:19–24. doi: 10.1136/mp.55.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Caussy D, Goedert JJ, Palefsky J, Gonzales J, Rabkin CS, DiGioia RA, Sanchez WC, Grossman RJ, Colclough G, Wiktor SZ, et al. Interaction of human immunodeficiency and papilloma viruses: association with anal epithelial abnormality in homosexual men. Int J Cancer. 1990;46:214–219. doi: 10.1002/ijc.2910460212. [DOI] [PubMed] [Google Scholar]
- 231.Braun L. Role of human immunodeficiency virus infection in the pathogenesis of human papillomavirus-associated cervical neoplasia. Am J Pathol. 1994;144:209–214. [PMC free article] [PubMed] [Google Scholar]
- 232.Hermonat PL, Plott RT, Santin AD, Parham GP, Flick JT. Adeno-associated virus Rep78 inhibits oncogenic transformation of primary human keratinocytes by a human papillomavirus type 16-ras chimeric. Gynecol Oncol. 1997;66:487–494. doi: 10.1006/gyno.1997.4789. [DOI] [PubMed] [Google Scholar]
- 233.Meyers C, Alam S, Mane M, Hermonat PL. Altered biology of adeno-associated virus type 2 and human papillomavirus during dual infection of natural host tissue. Virology. 2001;287:30–39. doi: 10.1006/viro.2001.0968. [DOI] [PubMed] [Google Scholar]
- 234.Agrawal N, Mane M, Chiriva-Internati M, Roman JJ, Hermonat PL. Temporal acceleration of the human papillomavirus life cycle by adeno-associated virus (AAV) type 2 superinfection in natural host tissue. Virology. 2002;297:203–210. doi: 10.1006/viro.2002.1405. [DOI] [PubMed] [Google Scholar]
- 235.Coker AL, Russell RB, Bond SM, Pirisi L, Liu Y, Mane M, Kokorina N, Gerasimova T, Hermonat PL. Adeno-associated virus is associated with a lower risk of high-grade cervical neoplasia. Exp Mol Pathol. 2001;70:83–89. doi: 10.1006/exmp.2000.2347. [DOI] [PubMed] [Google Scholar]
- 236.Walz CM, Anisi TR, Schlehofer JR, Gissmann L, Schneider A, Muller M. Detection of infectious adeno-associated virus particles in human cervical biopsies. Virology. 1998;247:97–105. doi: 10.1006/viro.1998.9226. [DOI] [PubMed] [Google Scholar]
- 237.Strickler HD, Viscidi R, Escoffery C, Rattray C, Kotloff KL, Goldberg J, Manns A, Rabkin C, Daniel R, Hanchard B, Brown C, Hutchinson M, Zanizer D, Palefsky J, Burk RD, Cranston B, Clayman B, Shah KV. Adeno-associated virus and development of cervical neoplasia. J Med Virol. 1999;59:60–65. doi: 10.1002/(sici)1096-9071(199909)59:1<60::aid-jmv10>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 238.Kalimo K, Terho P, Honkonen E, Gronroos M, Halonen P. Chlamydia trachomatis and herpes simplex virus IgA antibodies in cervical secretions of patients with cervical atypia. Br J Obstet Gynaecol. 1981;88:1130–1134. doi: 10.1111/j.1471-0528.1981.tb01767.x. [DOI] [PubMed] [Google Scholar]
- 239.Bjorge T, Gunbjorud AB, Langmark F, Skare GB, Thoresen SO. [Mass screening for cervical cancer. A one-year registration of cervical cytological tests] Tidsskr Nor Laegeforen. 1994;114:341–345. [PubMed] [Google Scholar]
- 240.Bjorge T, Gunbjorud AB, Haugen OA, Skare GB, Trope C, Thoresen SO. Mass screening for cervical cancer in Norway: evaluation of the pilot project. Cancer Causes Control. 1995;6:477–484. doi: 10.1007/BF00054154. [DOI] [PubMed] [Google Scholar]
- 241.Koskela P, Anttila T, Bjorge T, Brunsvig A, Dillner J, Hakama M, Hakulinen T, Jellum E, Lehtinen M, Lenner P, Luostarinen T, Pukkala E, Saikku P, Thoresen S, Youngman L, Paavonen J. Chlamydia trachomatis infection as a risk factor for invasive cervical cancer. Int J Cancer. 2000;85:35–39. doi: 10.1002/(sici)1097-0215(20000101)85:1<35::aid-ijc6>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 242.Anttila T, Saikku P, Koskela P, Bloigu A, Dillner J, Ikaheimo I, Jellum E, Lehtinen M, Lenner P, Hakulinen T, Narvanen A, Pukkala E, Thoresen S, Youngman L, Paavonen J. Serotypes of Chlamydia trachomatis and risk for development of cervical squamous cell carcinoma. JAMA. 2001;285:47–51. doi: 10.1001/jama.285.1.47. [DOI] [PubMed] [Google Scholar]
- 243.Gravitt PE, Castle PE. Chlamydia trachomatis and cervical squamous cell carcinoma. JAMA. 2001;285:1703–1704. [PubMed] [Google Scholar]