Abstract
Variations in definitions and methodologies have created differences in the results and conclusions obtained from studies of football (soccer) injuries, making interstudy comparisons difficult. Therefore an Injury Consensus Group was established under the auspices of Fédération Internationale de Football Association Medical Assessment and Research Centre. A nominal group consensus model approach was used. A working document on definitions, methodology, and implementation was discussed by the group. Iterative draft statements were prepared and circulated to members of the group for comment before the final consensus statement was produced. Definitions of injury, recurrent injury, severity, and training and match exposures in football together with criteria for classifying injuries in terms of location, type, diagnosis, and causation are proposed. Proforma for recording players' baseline information, injuries, and training and match exposures are presented. Recommendations are made on how the incidence of match and training injuries should be reported and a checklist of issues and information that should be included in published reports of studies of football injuries is presented.
Keywords: injury, football, soccer, definitions, data collection
It has been well documented that variations in definitions and methodologies create significant differences in the results and conclusions obtained from studies of sports injuries.1,2,3,4,5,6,7,8,9,10,11 Medical journals have developed strategies, such as the CONSORT statement12 for randomised controlled trials, to address these problems and to improve the quality of published studies. However, despite continuing calls for common methodologies to be adopted, fundamental differences in definitions and implementation strategies have persisted in published studies of football injuries. This consensus statement aims to establish definitions and methodology, implementation, and reporting standards that should be adopted for studies of injuries in football and to provide the basis for studies of injuries in other team sports.
Method
After informal discussions during the 1st World Congress on Sports Injury Prevention in Oslo in June 2005, the Fédération Internationale de Football Association Medical Assessment and Research Centre (F‐MARC) agreed to host an Injury Consensus Group comprising a range of experts involved in the study of football injuries. A nominal group consensus model approach13 was adopted for producing a consensus statement on definitions and methodological issues related to studies of football injuries. A working document identifying key issues associated with data collection and reporting in surveillance, risk factor, and intervention studies was produced to structure discussions at a two day meeting in Zurich. After this meeting, iterative draft consensus statements were prepared and circulated to members of the group for comment before this final statement was produced.
Definitions
Injury
An injury is defined as:
Any physical complaint sustained by a player that results from a football match or football training, irrespective of the need for medical attention or time loss from football activities. An injury that results in a player receiving medical attention is referred to as a “medical attention” injury, and an injury that results in a player being unable to take a full part in future football training or match play as a “time loss” injury.
“Medical attention” refers to an assessment of a player's medical condition by a qualified medical practitioner. “A player being unable to take a full part in future football training or match play” is independent of whether a training session actually takes place on the day after the injury or whether a player is selected to play in the next match. The term “future” refers to any time after the onset of injury, including the day of injury. It is important to recognise that variations in medical support and practice and in an individual player's tolerance to pain may create differences in the incidence of injury reported in studies. Multiple injuries sustained by a player in a single event should be recorded as one injury with multiple diagnoses. Injuries that are unrelated to football competition or training should not be recorded in studies of football injuries. Players may also experience problems other than physical complaints, such as illnesses, diseases, and mental complaints, and it may be appropriate in specific studies to record these problems; however, their incidence should be reported separately from the incidence of physical complaints.
Recurrent injury
A recurrent injury is defined as:
An injury of the same type and at the same site as an index injury and which occurs after a player's return to full participation from the index injury. A recurrent injury occurring within two months of a player's return to full participation is referred to as an “early recurrence”, one occurring 2–12 months after a player's return to full participation as a “late recurrence”, and one occurring more than 12 months after a player's return to full participation as a “delayed recurrence”.
It is essential to adopt the same recording regimen for recurrent injuries as that adopted for index injuries—that is, “all”, “medical attention”, or “time loss” injuries—because the recording regimen affects the reported incidences of both index and recurrent injuries. When recurrent injuries are recorded, the site of the injury, such as the specific muscle or ligament, rather than the general location of the injury, such as the thigh or knee, should be considered. Index injuries sustained before the start of a study should also be considered when identifying an injury as a recurrence. Injuries such as contusions, lacerations, and concussions and sequelae resulting from an index injury should not be recorded as recurrences. Recall bias6 is less likely to affect the recording of early recurrent injuries than it is for late and delayed recurrent injuries because of the shorter time period between the two injuries.
Injury severity
Injury severity is defined as:
The number of days that have elapsed from the date of injury to the date of the player's return to full participation in team training and availability for match selection.
The day on which an injury occurs is day zero and is not counted when determining the severity of an injury. Therefore, if a player cannot participate fully on the day of an injury but is available for full participation the next day, the incident should be recorded as a time loss injury with a severity of zero days. If an injured player leaves a study or a study finishes before a player's injury has resolved, the attending clinician should estimate the total number of days that would have elapsed before the player returned to full participation if the player had remained in the study or the study had continued. If a player retires from play as a direct consequence of an injury sustained during a study before returning to full participation, the injury should be reported separately as a “career ending injury”. Occasionally, an injury may have multiple diagnoses; in these cases, it is important to distinguish between the overall severity of the injury event and the severities of the individual diagnoses. The purpose of some studies may dictate that injury outcome measures other than days of absence, such as individual or team performances, costs associated with rehabilitation, insured and uninsured costs, or the long term impact on a player's quality of life, should be recorded.
Match exposure
Match exposure is defined as:
Play between teams from different clubs.
Match exposure between teams from the same club should be regarded as training exposure. Any match activity that forms a part of a player's rehabilitation from injury should not be recorded as match exposure.
Training exposure
Training exposure is defined as:
Team based and individual physical activities under the control or guidance of the team's coaching or fitness staff that are aimed at maintaining or improving players' football skills or physical condition.
Pre‐match warm up and post‐match cool down sessions should be recorded as training exposure. Motivational team talks, classroom discussions about tactics, and sessions with sports psychologists, nutritionists, etc should not be recorded as training exposure. Personal training activities undertaken by players away from their team and which are not planned by the team's coaching or fitness staff should not be recorded as training exposure. Any training activity forming a part of a player's rehabilitation from injury should not be recorded as training exposure.
Methodological issues
Studies should be of a prospective, cohort design to minimise the occurrence of errors associated with recall, which is a problem with retrospective study designs. Cohort studies that record players' exposures enable relations between the incidence of injury and risk factors in the study population to be explored.
Interpretation of injury definition
Most studies will record medical attention and/or time loss injuries. Table 1 presents examples of how specific incidents should be recorded under these recording regimens.
Table 1 Examples of how to record injuries under different recording regimens.
| Example | Injury recording regimen | |
|---|---|---|
| Medical attention | Time loss | |
| 1. A defender sustained a hamstring injury during a match that required 30 days of rehabilitation before he could return to full training. The player sustained another hamstring injury to the same muscle (same leg) 3 weeks later and required a further 50 days of rehabilitation before he could return to full training. | First incident should be recorded as an injury (severity: 30 days); second incident as a recurrence (severity: 50 days). | First incident should be recorded as an injury (severity: 30 days); second incident as a recurrence (severity: 50 days). |
| 2. A goalkeeper developed shoulder instability and sought medical attention; the condition did not prevent him from taking a full part in team training or competition even though it caused him some pain. The team physiotherapist recommended an individual training programme for the goalkeeper to avoid aggravating the condition. | Episode should be recorded as an injury (severity: 0 days). | Episode should not be recorded as long as he remained able to take a full part in team training. |
| 3. A defender sustained a groin injury, which the team doctor decided did not warrant immediate treatment; the player continued to take a full part in team training and competition. The player underwent elective surgery 2 months later and required 90 days rehabilitation. | Incident should be recorded as an injury (severity: 0 days); when the player underwent elective surgery, the severity should be reclassified to 90 days. | Incident should be recorded as an injury at the time of the player's elective surgery (severity: 90 days). |
| 4. A defender suffered groin pain that did not result in time loss; this incident was followed by a 1 month pain‐free period; he then suffered a further period of groin pain, which prevented him from training and which required 21 days of rehabilitation. | First episode should be recorded as an injury (severity: 0 days); second episode should be recorded as a recurrence (severity: 21 days). | First episode should not be recorded; second episode should be recorded as an injury (severity: 21 days). |
| 5. A forward sustained an ankle sprain during a match but continued to play; he received medical attention after the match. He completed full team training using ankle taping (with some pain) for 6 days but aggravated the injury during the next match; he then required 15 days of rehabilitation. | First incident should be recorded as an injury (severity: 0 days) and when the second incident occurred the severity of the index injury should be reclassified to 15 days. | First incident should not be recorded and the second incident should be recorded as an injury (15 days). |
| 6. A midfield player sustained a laceration to the face during a morning training session; the doctor sutured the cut but the player missed the afternoon training session. The player was able to take a full part in training on the following day. | Incident should be recorded as an injury (severity: 0 days). | Incident should be recorded as an injury (severity: 0 days). |
Injury classification
Injuries should be classified by location, type, body side, and mechanism of injury (traumatic or overuse) and whether the injury was a recurrence. In this context, a traumatic injury refers to an injury resulting from a specific, identifiable event, and an overuse injury to one caused by repeated micro‐trauma without a single, identifiable event responsible for the injury. In some studies, diagnoses of injuries may be required; in these cases, a qualified medical practitioner should provide a specific written diagnosis or use a sport specific injury coding system, such as the Orchard14 system.
Location of injury
The location of injuries should be recorded using the categories listed in table 2. The location of injuries should be recorded using the individual categories indicated but where the number of injuries in a study is small, it may be necessary to combine individual location categories into the main groupings for analysis purposes.
Table 2 Main groupings and categories for classifying injury location.
| Main grouping | Category | Equivalent OSICS body area character |
|---|---|---|
| Head and neck | Head/face | H |
| Neck/cervical spine | N | |
| Upper limbs | Shoulder/clavicula | S |
| Upper arm | U | |
| Elbow | E | |
| Forearm | R | |
| Wrist | W | |
| Hand/finger/thumb | P | |
| Trunk | Sternum/ribs/upper back | C, D |
| Abdomen | O | |
| Lower back/pelvis/sacrum | B, L | |
| Lower limbs | Hip/groin | G |
| Thigh | T | |
| Knee | K | |
| Lower leg/Achilles tendon | Q, A | |
| Ankle | A | |
| Foot/toe | F |
OSICS, Orchard sports injury classification system.14
Type of injury
The type of injury should be recorded using the categories listed in table 3. The type of injuries should be recorded using the individual categories indicated, but where the number of injuries in a study is small, it may be necessary to combine individual type categories into the main groupings for analysis purposes. If the purpose of a study is to investigate other problems, such as illnesses, diseases, or mental complaints, these should be recorded under separate headings from those listed in table 3.
Table 3 Main groupings and categories for classifying type of injury.
| Main grouping | Category | Equivalent OSICS pathology character |
|---|---|---|
| Fractures and bone stress | Fracture | F |
| Other bone injuries | G, Q, S | |
| Joint (non‐bone) and ligament | Dislocation/subluxationSprain/ligament injury | D, UJ, L |
| Lesion of meniscus or cartilage | C | |
| Muscle and tendon | Muscle rupture/tear/strain/cramps | M, Y |
| Tendon injury/rupture/tendinosis/bursitis | T, R | |
| Contusions | Haematoma/contusion/bruise | H |
| Laceration and skin lesion | Abrasion | K |
| Laceration | K | |
| Central/peripheral nervous system | Concussion (with or without loss of consciousness)Nerve injury | NN |
| Other | Dental injuries | G |
| Other injuries |
OSICS, Orchard sports injury classification system.14
Other injury classification issues
Injuries should also be classified as to whether they occurred during a match or training session and whether they were the result of contact with another player or other object. It may also be appropriate to record whether the action causing the injury was a violation of the laws of football.
Study population
The study population should normally consist of more than one team of players and the study should last for a minimum period of one season (including preseason), 12 months, or the duration of a tournament. Players joining/leaving the cohort—for example, through transfer into/out of a team—should be included/excluded from the date of joining/leaving. Injuries and exposures should be documented for every player within the cohort throughout the study period. Players who have an existing injury at the start of a study should not be excluded from the study, but their existing injuries should not be included as part of the study. For intervention and risk factor studies and for studies where the objective is to compare injury rates between groups, power calculations should be used to determine the population size required to identify significant differences in the effects being investigated.15
Implementation issues
Standardised data collection forms, which can be in electronic or paper format, should be used consistently throughout a study. Table 4 presents an overview of the forms that are normally required for a study of injuries in football.
Table 4 Standard forms required for a study of injuries in football.
| Form | Information required | Who should provide the information? | When should the information be provided? |
|---|---|---|---|
| Player's baseline information | Player's characteristics | Each player | When a player enters the study |
| Injury report | Classification and circumstances of injury | Medical professionals | After each recordable injury |
| Match and training exposure | Player's match and training exposure time | Coaches | Every match and training session |
Player's baseline information form
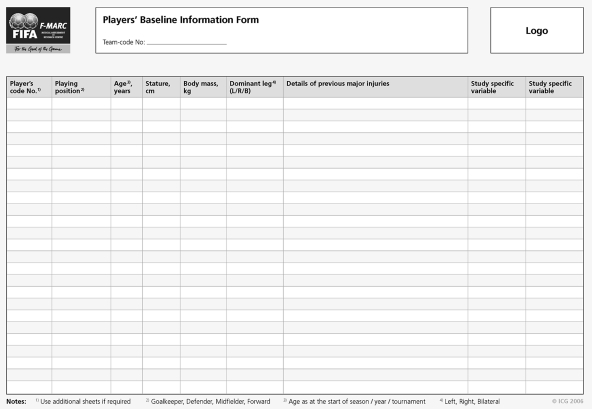
The exact nature of the baseline information required will depend on the purpose of the study; however, for surveillance studies, basic information, such as the player's age, sex, playing position, stature, and body mass should be recorded, as these parameters define the study population. For other studies, such as interventions and investigations of relations between risk factors and the incidence of injury, more detailed baseline information may be required. Appendix A provides an example of a form for collecting a player's baseline information.
Injury form
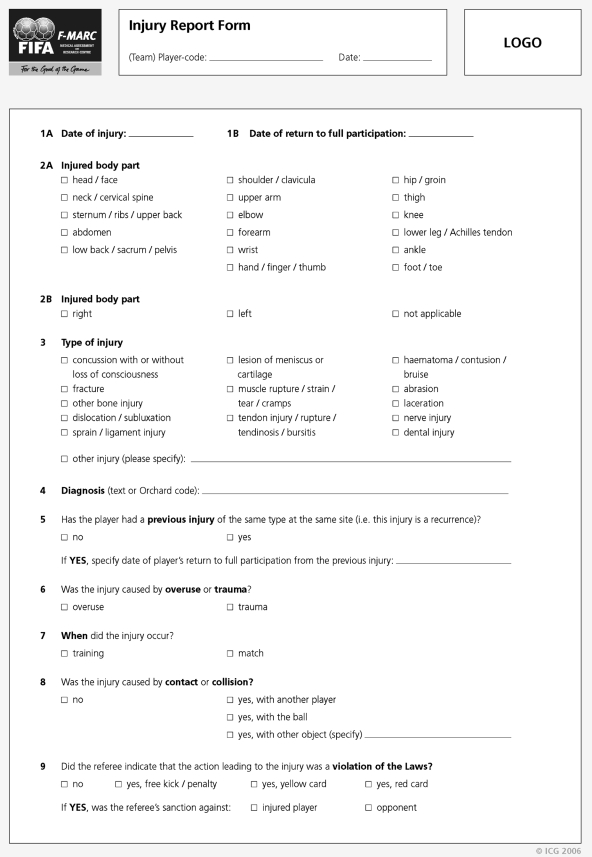
The injury form should include the team's and player's study reference numbers, date of injury, whether the injury was sustained during a match or training exposure, description of the circumstances surrounding the injury, and the date of the player's return to full participation. The nature of the injury (location, type, side injured, recurrence) and the main mechanism (traumatic or overuse) should also be recorded. One free text section should be provided to enable a specific injury diagnosis or an injury classification code to be recorded. A second free text section may be required for some studies if additional study specific information is required. Injury report forms should be completed as soon as possible after the injury was sustained to avoid inaccuracies associated with recording information retrospectively. However, injury information should be revised/updated if further information is obtained at a later date—for example, from diagnostic tests. Appendix B provides an example of a form for recording injury information.
Match and training exposure form
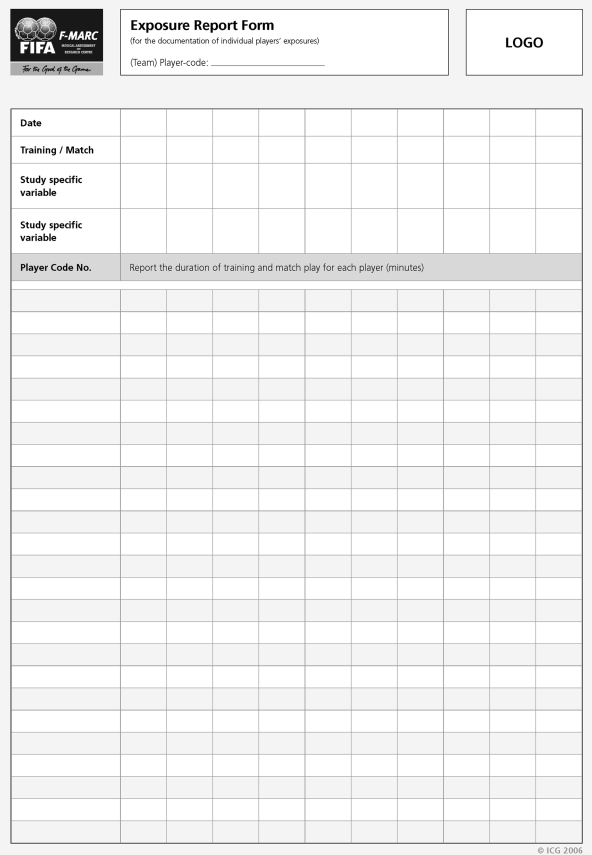
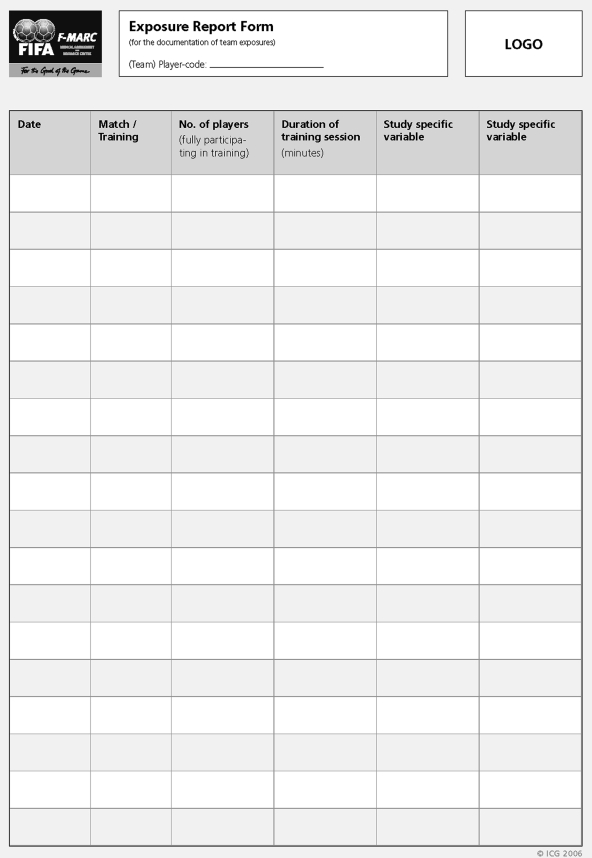
The form should record the date, type, and duration (minutes) of each exposure. Exposures can either be collected on an individual player basis or for a group of players. Collecting individual player exposures, especially for training sessions, is very time consuming, and this level of detail should only be recorded if the information is specifically required to meet the aims of the study. However, for studies where players are exposed in a range of situations, such as club and country, or where the intention is to investigate relations between the incidence of injuries and individual risk factors, the actual exposure times for each player must be recorded. If data are collected on a group basis, the number of matches and training sessions, duration of each training session, and number of players attending each training session must be recorded. Training exposure data should preferably be collected for each training session, but, as a minimum, the information should be collected on a weekly basis. It may also be appropriate, depending on the purpose of the study, to record other variables, such as the playing surface or type of training undertaken.
For studies recording team match exposure, the total player‐match exposure time in hours for a team is given by (NMPMDM)/60 where NM is the number of team matches played, PM is the number of players in the team (normally 11), and DM is the duration of the match in minutes (normally 90). Collecting match exposure data on a team basis rather than for individual players does not take into account exposure time lost because players are temporarily or permanently absent during a match through, for example, treatment or receipt of a red card. For studies recording team training exposure, the total training exposure time in hours is given by the sum of the values for (PTDT)/60 for every training session throughout the study, where PT is the number of players attending a training session and DT is the duration of the training session in minutes. Collecting team based training data rather than individual data does not take into account training exposure time lost when a player does not complete a full training session. Appendix C provides an example of a form for collecting match and training exposures for individual players, and appendix D provides an example for collecting team training and match exposures.
Other implementation issues
The purpose and setting of individual studies determine whether all, medical attention, or time loss injuries are recorded. Whichever injury recording regimen is adopted, it is essential that it is used consistently for all aspects of the study. Although collecting information on injuries without time loss may be important for investigating wider health issues, it must be recognised that this injury recording regimen places higher time demands on the medical personnel involved with the study. Although the exact format of the documentation required will depend on the specific aims and objectives of a study, the forms presented in appendices A–D provide a format for collecting the minimum amount of information that would normally be required. When new procedures are implemented, they should always be subjected to a pilot study before the main investigation is started.
The format and content of each study should be approved by and follow the protocols defined by an appropriate institutional ethics committee. Players should be assigned individual reference codes that are known only to the personnel recording information in order to maintain players' confidentiality when the data are analysed. Players taking part in a study should have the purpose and format of the study explained to them using face to face presentations or a detailed information sheet. Individual players must always retain the right not to take part and to withdraw from a study at any time. To maximise the level of compliance, a number of supporting initiatives can be implemented, such as providing written instructions for all personnel completing the forms and providing examples of completed forms. It is beneficial to identify a recognised contact person at each team, who does not have to be the person completing the forms. Regular contact should be maintained with each team, and feedback should be provided at appropriate points in time throughout the study.
Reporting data
The cohort should be clearly defined by reporting the numbers of participants and teams taking part at the beginning of the study, the numbers of participants and teams dropping out and joining during the study, together with the age range and sex of the participants, the standard of play, and the duration of the study. Numbers of injuries occurring during matches and training should be reported separately, together with the corresponding match and training exposures so that the incidences of both match and training injuries can be calculated. The incidence of injuries should normally be reported as the number of injuries per 1000 player‐hours; in studies reporting the incidence of match injuries, it may also be appropriate to report the number of injuries per match. Where possible, the incidences of all, medical attention, and time loss injuries should be reported separately, as this enables interstudy comparisons of results. The incidence of injury expressed as a function of total exposure time (match plus training) should only be reported if the incidences of match and training injuries are also reported separately. The incidence of injury should not be reported as a function of athlete exposures because the duration of individual exposures will vary. If the aim of a study is to measure the incidence of injury associated with specific training activities, then the incidence of training injuries should be reported as a function of the players' exposure to the specific training activities, such as the number of injuries during weight training per 1000 player‐hours of weight training.
The average and median severity of injuries should be reported in days together with the distribution of injuries grouped according to their severity: slight (0 days); minimal (1–3 days); mild (4–7 days); moderate (8–28 days); severe (>28 days); career ending. The severity of injuries reported will be influenced by the recording regimen adopted in a study. The locations and types of injuries should be reported as numbers and percentages for both match and training injuries. It is also beneficial to cross tabulate the injury locations (table 3) with the types of injury (table 4), as this provides an understanding of the overall nature of the injuries recorded in a study.
If the times of match injuries are recorded, the injuries should be grouped into defined periods of the game (0–15, 16–30, 31–45 (+injury time), 46–60, 61–75, 76–90 (+injury time) minutes) and reported as percentages of injuries occurring in each of these periods; injuries sustained during extra time should be reported in a separate “extra time” period. Other results reported will depend on the specific purpose of the study but may include, for example, comparisons of the incidence and severity of injuries within subgroups of the study population, such as age, sex, skill level, or training programme. In each case, the data should be presented to an equivalent standard to the examples described above.
Finally, table 5 provides a checklist of issues that should be included in reports of studies on football injuries. The checklist is intended to describe the minimum information that should be included in a report; the aims and objectives of specific studies will dictate whether other information should also be presented. In principle, reports of studies should include sufficient information for readers to understand how a study was performed, to judge the quality of the information collected, and to assess the reliability of the findings presented.
Table 5 Checklist of issues that should be included in reports of studies of football injuries.
| Section | Issues | Reported on page |
|---|---|---|
| Title | Identify the type and purpose of the study, for example, injury surveillance to measure or intervention to reduce the incidence of injuries. | |
| Abstract | Present a structured summary of the study, including Aims, Methods, Results, Discussion, and Conclusions. | |
| Introduction | Discuss background to and aims, objectives, and hypotheses for the study. | |
| Methods | Design of study, for example, prospective cohort, randomised controlled trial. | |
| Study population, including the organisational setting and geographic location, the numbers of players and teams involved, age range and sex of participants, level of play, and the duration of the study. | ||
| Describe medical personnel involved and the frequency of recording injury and exposure data. | ||
| Definitions of injury and exposure used in study. | ||
| Planned interventions and the criteria used for selecting the intervention and control groups. | ||
| Primary and secondary outcome measures, such as the number of medical attention/time loss injuries, cost of treatment, and the incidence and severity of injuries and recurrences. | ||
| Methods used to define the study size in risk factor and intervention studies, for example, power calculations. | ||
| Methods, such as training, used to improve the quality of data collection. | ||
| Statistical methods used to compare groups and subgroups. | ||
| Results | Report for the study population and each subgroup assessed: | |
| numbers of match and training injuries, | ||
| numbers of match and training recurrences, | ||
| match and training exposures. | ||
| Present with appropriate statistical information for the study population and each subgroup: | ||
| baseline data on the study population, | ||
| incidences of match and training injuries, | ||
| incidence of recurrences, | ||
| severities of match and training injuries, | ||
| distributions of injury locations and types for match and training, | ||
| cross tabulations of injury locations and types for match and training. | ||
| Present, together with inferential statistics, other summary data that are appropriate to the aims and objectives of the study. | ||
| Discussion | Interpretation of study results, taking into account the study aims, objectives, and hypotheses and the existing evidence in the literature. | |
| Comment on generalisations that can be reached from the study results. |
APPENDIX A
APPENDIX B
APPENDIX C
APPENDIX D
Footnotes
Competing interests: none declared
References
- 1.van Mechelen W, Hlobil H, Kemper H C G. Incidence, severity, aetiology and prevention of sports injuries: a review of concepts. Sports Med 19921482–99. [DOI] [PubMed] [Google Scholar]
- 2.Meeuwisse W H. Assessing causation in sport injury: a multifactorial model. Clin J Sport Med 19944166–170. [Google Scholar]
- 3.Caine D J, Caine C G, Lindner K J. The epidemiologic approach to sports injuries. In: Caine DJ, Caine CJ, Lindner KJ, eds. Epidemiology of sports injuries. Champaign, IL: Human Kinetics, 19961–13.
- 4.de Loes M. Exposure data. Why are they needed? Sports Med 199724172–175. [DOI] [PubMed] [Google Scholar]
- 5.Finch C F. An overview of some definitional issues for sports injury surveillance. Sports Med 199724157–163. [DOI] [PubMed] [Google Scholar]
- 6.Junge A, Dvorak J. Influence of definition and data collection on the incidence of injuries in football. Am J Sports Med 200028S40–S46. [DOI] [PubMed] [Google Scholar]
- 7.Ekstrand J, Karlsson J. The risk for injury in football. There is a need for consensus about definition of the injury and the design of studies. Scand J Med Science Sports 200313147–149. [Google Scholar]
- 8.Fuller C W, Drawer S D. The application of risk management in sport. Sports Med 200434349–356. [DOI] [PubMed] [Google Scholar]
- 9.Junge A, Dvorak J, Graf‐Baumann T.et al Football injuries during FIFA tournaments and the Olympic Games, 1998–2001. Am J Sports Med 200432S80–S89. [DOI] [PubMed] [Google Scholar]
- 10.Hägglund M, Waldén M, Bahr R.et al Methods for epidemiological study of injuries to professional football players: developing the UEFA model. Br J Sports Med 200539340–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brooks J H M, Fuller C W. The influence of methodological issues on the results and conclusions from epidemiological studies of sports injuries: illustrative examples. Sports Med 200636 in press [DOI] [PubMed] [Google Scholar]
- 12.Altman D G. Better reporting of randomised controlled trials: the CONSORT statement. BMJ 1996313570–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fink A, Kosecoff J, Chassin M.et al Consensus methods: characteristics and guidelines for use. Am J Public Health 198474979–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orchard J. Orchard Sports Injury Classification System (OSICS). Sport Health 19951139–41. [Google Scholar]
- 15.Bahr R, Holme I. Risk factors for sports injuries: a methodological approach. Br J Sports Med 200337384–392. [DOI] [PMC free article] [PubMed] [Google Scholar]