Abstract
Background
The development of symptomatic hyponatraemia consequent on participation in marathon and ultraendurance races has led to questions about its aetiology and prevention.
Objectives
To evaluate: (a) the assertion that sweat sodium losses cannot contribute to the development of hyponatraemia during endurance exercise; (b) the adequacy of fluid replacement recommendations issued by the International Marathon Medical Directors Association (IMMDA) for races of 42 km or longer; (c) the effectiveness of commercial sports drinks, compared with water, for attenuating plasma sodium reductions.
Methods
A mathematical model was used to predict the effects of different drinking behaviours on hydration status and plasma sodium concentration when body mass, body composition, running speed, weather conditions, and sweat sodium concentration were systematically varied.
Results
Fluid intake at rates that exceed sweating rate is predicted to be the primary cause of hyponatraemia. However, the model predicts that runners secreting relatively salty sweat can finish ultraendurance exercise both dehydrated and hyponatraemic. Electrolyte‐containing beverages are predicted to delay the development of hyponatraemia. The predictions suggest that the IMMDA fluid intake recommendations adequately sustain hydration over the 42 km distance if qualifiers—for example, running pace, body size—are followed.
Conclusions
Actions to prevent hyponatraemia should focus on minimising overdrinking relative to sweating rate and attenuating salt depletion in those who excrete salty sweat. This simulation demonstrates the complexity of defining fluid and electrolyte consumption rates during athletic competition.
Keywords: water intoxication, fluid balance, dehydration, overhydration, prolonged exercise
Symptomatic hyponatraemia associated with athletic competition was first described in 1985,1 and more than 100 cases have been documented.2,3,4 Although most cases develop during participation in endurance events lasting eight hours or more, this syndrome also develops in slower runners participating in marathon (42 km) races. Most cases are associated with excessive fluid intake and weight gain.2,5 However, there is evidence that some athletes finish ultraendurance competition with plasma sodium concentrations below 130 mEq/l and have body mass losses greater than or equal to the weight loss expected from cellular respiration and respiratory water loss.6,7 The latter suggests that, in certain situations, hyponatraemia can occur without excessive fluid consumption. As sweat sodium concentrations can be high,8,9 it has been proposed that excessive fluid consumption and sweat sodium losses can contribute to symptomatic hyponatraemia.5 Noakes and colleagues have discounted the idea that sweat sodium losses contribute to the development of symptomatic hyponatraemia10,11 and argue that all cases would be prevented if athletes refrained from drinking excessively large volumes during endurance events.10,11
In response to the symptomatic hyponatraemia cases during marathon competitions, the International Marathon Medical Directors Association (IMMDA) of the Association of International Marathons published a position stand recommending that marathon runners drink ad libitum 400–800 ml/h, with the higher rates for the faster, heavier runners competing in warm environmental conditions and the lower rates for the slower runners/walkers completing marathon races in cooler environmental conditions.12 IMMDA has not made any recommendations about sodium intake. The adequacy of the IMMDA recommendation for preventing excessive dehydration or the development of symptomatic hyponatraemia has not been systematically evaluated. Excessive dehydration was not defined and probably refers more to minimising its contributions to heat exhaustion rather than to sustaining race pace. The IMMDA fluid consumption rates were stated as being “applicable to other distance running races”, so perhaps including ultraendurance events, such as Ironman distance triathlons. The effect of using the IMMDA recommendation for races longer than a marathon has also not been systematically evaluated.
This study uses a mathematical model to simulate the effects of different drinking behaviours on hydration status and plasma sodium concentration when body mass, body composition, running speed, weather conditions, and sweat sodium concentration are systematically varied. This mathematical analysis evaluates: (a) the assertion that unreplaced sweat sodium cannot contribute to the development of hyponatraemia during endurance exercise; (b) the applicability of IMMDA fluid replacement recommendations for running events longer than or equal to 42 km; (c) the effectiveness of commercial sports drinks, compared with water, for attenuating plasma sodium reductions. For the analyses, a fluid intake rate was considered effective for sustaining performance if predicted loss of body mass (attributable to dehydration) did not exceed 3% of the initial body mass and/or predicted plasma sodium concentrations did not fall below 130 mEq/l by the end of the estimated race time. A priori, we hypothesised that, under most circumstances, hyponatraemia would be primarily attributable to excessive fluid intake (relative to sweating rate), that high sweat sodium concentration would minimise the amount of overdrinking needed to produce sodium dilution, and the combination of hydration and unreplaced sweat sodium losses could, under specific circumstances, produce both dehydration and hyponatraemia. This simulation demonstrates the complexity of defining fluid and electrolyte consumption needs during athletic competition.
Methods
Body water and sodium loss (gain) were modelled for subjects of various body masses (50, 70 and 90 kg) and body compositions (total body water equal to 63% and 50% of body mass),13 performing prolonged sustained exercise equivalent to the energy cost of running 8.5, 10, 12.5, and 15 km/h in cool/temperate (∼ 18°C) and warm (∼ 28°C) weather, with various water consumption rates (400, 600 and 800 ml/h) and sweat sodium concentrations (25, 50 and 75 mEq/l).
Changes in body mass (due to water loss/gain) and plasma sodium concentration were calculated from the following equations:
SR = (BM × V)/732 × (1 − ((R + C)/H))
FB = FI − SR × t
%BML = FB/BMi × 100
ΔNa+e = (FI × Na+FI × t) − (SR × Na+sweat × t)
ΔK+e = (FI × K+FI × t) − (SR × K+sweat × t)
[Na+]p2 = ((([Na+]p1 + 23.8) × TBWi + 1.03Δ(Na+e + K+e))/(TBWi + FB)) − 23.8
where SR is sweating rate (litres/h), BM is body mass (kg), V is velocity (km/h), R + C is radiative and convective heat loss (W/m2), H is heat production (W/m2), FB is fluid balance (litres), FI is fluid intake (litres/h), t is time (hours), %BML is percentage body mass loss, BMi is initial body mass (kg), ΔNa+e is the change in exchangeable sodium (mEq), Na+FI is the sodium concentration of the fluids consumed (mEq/l), Na+sweat is the sweat sodium concentration (mEq/l), ΔK+e is the change in exchangeable potassium (mEq), K+FI is the potassium concentration of the fluids consumed (mEq/l), K+sweat is the sweat potassium concentration (mEq/l),[Na+]p2 is the predicted plasma sodium concentration (mEq/l), [Na+]p1 is the initial plasma sodium concentration (mEq/l), and TBWi is initial total body water (litres).
Sweating rate was calculated from energy cost of locomotion and expected heat production14 with adjustment for heat loss from radiation and convection.15 For the latter, it was assumed that the skin to ambient temperature gradient was 10°C and 4°C for cool/temperate and warm weather conditions respectively. The sweating rate equation assumes that sweating and sweat evaporation are 100% efficient. Plasma sodium concentration was calculated using the equation of Kurtz and Nguyen,16 which predicts changes in plasma sodium concentration from changes in the mass balance of sodium, potassium, and water. Details on the derivation of the equation and the significance of the constants are presented elsewhere,16,17 but they account for the unequal distribution of univalent cations between the plasma and interstitial fluid, the osmotic coefficient of sodium salts, the contribution of osmotically inactive exchangeable sodium and potassium, plasma potassium concentration, and osmotically active non‐sodium and non‐potassium osmoles. For this analysis, initial plasma sodium concentration was assumed to be 140 mEq/l. Potassium losses in sweat were assumed to be 4.5 mEq/l.9,18 For simplicity, BMLs due to respiratory water loss and oxidative metabolism were ignored. This omission should have limited effect on body water status, as the rate of respiratory water loss is typically negated by the water produced during cellular respiration. However, it will produce less BML than what would be expected to occur. Similarly, no attempt was made to adjust water gained from the breakdown of muscle glycogen or protein. However, the model also assumed that there was no change in the quantity of osmotic particles in the intracellular fluid and no water or electrolytes were lost in urine. On the basis of reported urine production rates during Ironman triathlons19 and estimated water released from glycogen oxidation, these omissions probably underestimated fluid balance by 50–300 ml over such a triathlon.
Data were analysed by evaluating the changes in body mass and sodium concentration over time. The rate of fluid intake was considered effective for sustaining performance if dehydration did not produce a BML in excess of 3% initial body mass and/or plasma sodium concentrations did not fall below 130 mEq/l by the end of the estimated race time. These values were chosen because dehydration in excess of 2% body mass is associated with the onset of impaired endurance performance,13,20 and plasma sodium concentrations below 130 mEq/l are associated with the development of symptomatic hyponatraemia.5 For this paper, hyponatraemia is defined as plasma sodium <130 mEq/l.
Results
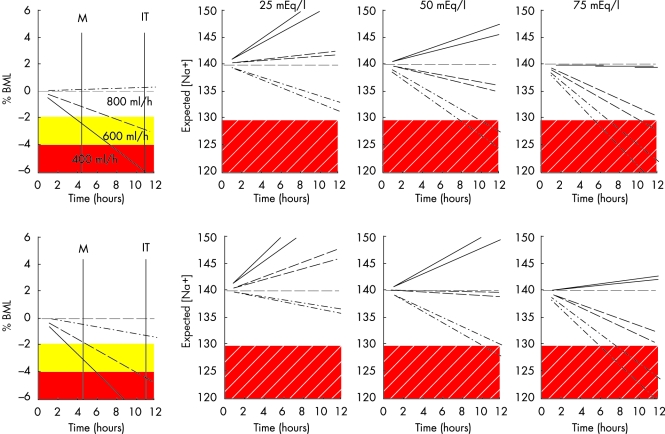
Table 1 presents the predicted sweating rates for 50–90 kg subjects running at 8.5–15 km/h in cool/temperate and warm weather conditions. Figure 1 presents the predicted BML (attributable to water deficit) and predicted plasma sodium associated with three rates of fluid replacement for a 70 kg person, running at a velocity approximating the average time of mass participant marathons. During cool/temperate weather (upper panels), 400 ml/h water or electrolyte‐free fluid is predicted to produce ∼2% BML by the end of a 42 km marathon and ∼6% BML by the end of an Ironman length triathlon. Consumption of 400 ml/h water is not predicted to produce hyponatraemia over the range of sweat sodium concentrations evaluated. Drinking at 600 ml/h would lead to moderate dehydration (2–5% BML) over time. Interestingly, despite modest dehydration, when sweat sodium is 75 mEq/l, drinking at this rate would be sufficient to induce hyponatraemia by the end of an Ironman length competition. Drinking water at a rate of 800 ml/h is predicted to prevent dehydration, but hyponatraemia would occur after five to six and eight to nine hours when sweat sodium concentrations are 75 and 50 mEq/l respectively. In the warm environment, 800 ml/h water consumption is also predicted to produce a modest dehydration (1–2% BML) and hyponatraemia during an Ironman length competition when sweat sodium concentrations are 50 mEq/l and higher.
Table 1 Predicted sweating rates (litres/h) for running 8.5–15 km/h in cool/temperate (18°C) and warm (28°C) weather.
| Body mass (kg) | Climate | 8.5 km/h | 10 km/h | 12.5 km/h | 15 km/h |
|---|---|---|---|---|---|
| 50 | Cool/temperate | 0.43 | 0.53 | 0.69 | 0.86 |
| Warm | 0.52 | 0.62 | 0.79 | 0.96 | |
| 70 | Cool/temperate | 0.65 | 0.79 | 1.02 | 1.25 |
| Warm | 0.75 | 0.89 | 1.12 | 1.36 | |
| 90 | Cool/temperate | 0.86 | 1.04 | 1.34 | 1.64 |
| Warm | 0.97 | 1.15 | 1.46 | 1.76 |
Figure 1 Predicted percentage body mass loss due to water deficit (%BML) and plasma sodium concentration (mEq/l) under three levels of sweat sodium loss for 70 kg subjects of varying body composition drinking 400–800 ml water/hour while running at 10 km/h in cool (18°C; upper panels) and warm (28°C; lower panels) weather. The solid shaded areas demark when water loss would be sufficient to modestly (yellow) and substantially (red) diminish performance. The hatched shaded area demarks the presence of hyponatraemia. The two lines sharing the same line style in the sodium figures are the predicted outcomes for each fluid replacement rate (400 ml/h = solid line, 600 ml/h = dashed line, 800 ml/h = dash‐dot line) when total body water accounts for 50% and 63% of body mass. M indicates the finishing time for the marathon run. IT indicates the approximate finishing time for the Ironman distance triathlon based on literature values for participants running a marathon portion at 10 km/h.
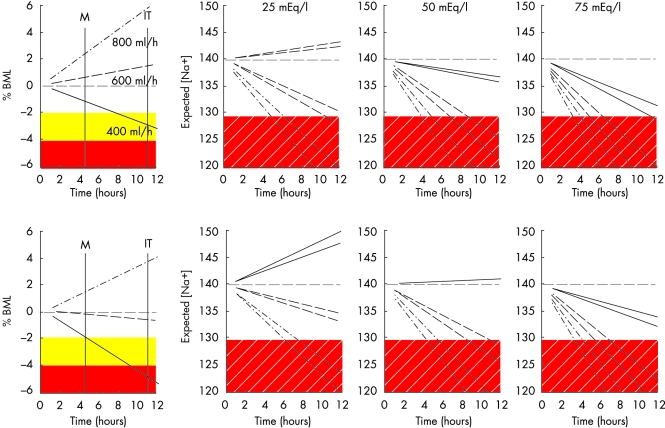
Figure 2 presents the predicted outcomes for the smaller 50 kg person running at 10 km/h. In cool/temperate weather, 400 ml/h consumption of water would sustain adequate hydration and prevent hyponatraemia, whereas 600–800 ml/h water is predicted to be in excess of sweat loss and would dilute plasma sodium over time. Consuming 800 ml/h would produce hyponatraemia before the finish of a 42 km marathon if sweat sodium concentration is 50 mEq/l and higher. In warm weather, 400 ml/h consumption of water is predicted to produce 2% BML and 5% BML by the end of a 42 km marathon and Ironman length triathlon respectively. Consuming 600 ml/h water is predicted to sustain hydration through an Ironman length triathlon, but induce hyponatraemia before the end if sweat sodium concentrations are 50 mEq/l or higher. Drinking 800 ml/h would be in excess of sweating rate and produce hyponatraemia by the end of a marathon if sweat sodium is 75 mEq/l.
Figure 2 Predicted percentage body mass loss due to water deficit (%BML) and plasma sodium concentration (mEq/l) under three levels of sweat sodium loss for 50 kg subjects of varying body composition drinking 400–800 ml water/hour while running at 10 km/h in cool (18°C; upper panels) and warm (28°C; lower panels) weather. The solid shaded areas demark when water loss would be sufficient to modestly (yellow) and substantially (red) diminish performance. The hatched shaded area demarks the presence of hyponatraemia. The two lines sharing the same line style in the sodium figures are the predicted outcomes for each fluid replacement rate (400 ml/h = solid line, 600 ml/h = dashed line, 800 ml/h = dash‐dot line) when total body water accounts for 50% and 63% of body mass. M indicates the finishing time for the marathon run. IT indicates the approximate finishing time for the Ironman distance triathlon based on literature values for participants running a marathon portion at 10 km/h.
Figure 3 presents the predicted outcomes for a larger 90 kg person running at 10 km/h. Progressive dehydration is predicted over the range of fluid intakes examined. Hyponatraemia was produced only when 800 ml/h was consumed with 75 mEq/l sweat sodium concentration.
Figure 3 Predicted percentage body mass loss due to water deficit (%BML) and plasma sodium concentration (mEq/l ) under three levels of sweat sodium loss for 90 kg subjects of varying body composition drinking 400–800 ml water/hour while running at 10 km/h in cool (18°C; upper panels) and warm (28°C; lower panels) weather. The solid shaded areas demark when water loss would be sufficient to modestly (yellow) and substantially (red) diminish performance. The hatched shaded area demarks the presence of hyponatraemia. The two lines sharing the same line style in the sodium figures are the predicted outcomes for each fluid replacement rate (400 ml/h = solid line, 600 ml/h = dashed line, 800 ml/h = dash‐dot line) when total body water accounts for 50% and 63% of body mass. M indicates the finishing time for the marathon run. IT indicates the approximate finishing time for the Ironman distance triathlon based on literature values for participants running a marathon portion at 10 km/h.
Slower (8.5 km/h) marathon runners have been reported to be at higher risk of developing exercise associated hyponatraemia.4,21 When this pace was used in the simulation, a 70 kg person consuming 400–600 ml/h water was not predicted to develop hyponatraemia, except if consuming 600 ml/h and sweat sodium was 75 mEq/l. Hyponatraemia would occur after eight to nine hours and 9–11 hours in cool and warm weather respectively. In cool/temperate weather, drinking 800 ml/h would produce overhydration and development of hyponatraemia after six to seven hours and 8.5–10 hours when sweat sodium was 50 and 25 mEq/l respectively. In warm weather, this drinking rate would produce less overhydration, and hyponatraemia would not develop until seven to nine hours at 50 mEq/l sweat sodium. For a 50 kg person, the slower speed would produce a similar pattern of changes, with 800 ml/h inducing dilutional hyponatraemia within a 42 km marathon independent of sweat sodium concentration. Drinking 400 ml/h would sustain adequate hydration and prevent hyponatraemia over an Ironman length triathlon when sweat sodium is 50 mEq/l or less.
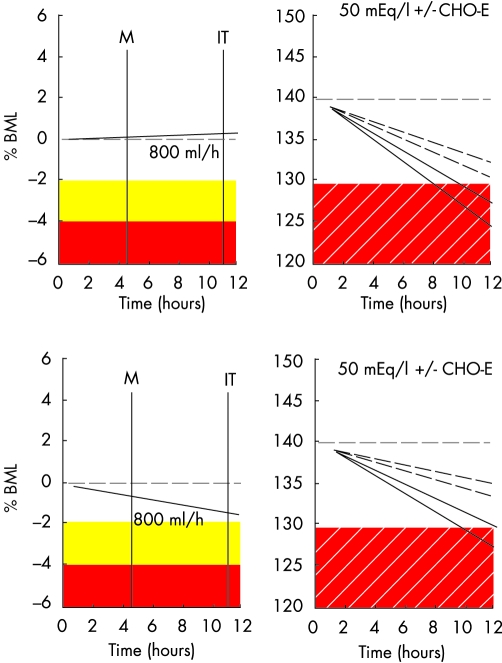
Figure 4 illustrates the influence of consuming a sports drink (containing 20 mEq/l sodium and 3 mEq potassium) in delaying hyponatraemia. In both cool/temperate and warm condition simulations, the sports drink is predicted to slow the rate of plasma sodium reduction (0.44 and 0.55 mEq/l/h when total body water is 63% and 50% of body mass respectively). Therefore, in these situations, sports drink consumption would prevent hyponatraemia.
Figure 4 Predicted effectiveness of a carbohydrate‐electrolyte sports drink (CHO‐E) containing 17 mEq/l sodium and 5 mEq/l potassium for attenuating the decline in plasma sodium concentration (mEq/l) expected for a 70 kg person drinking water at 800 ml/h when running 10 km/h in cool (18°C; upper panel) and warm (28°C; lower panel) weather. The solid shaded areas demark when water loss would be sufficient to modestly (yellow) and (red) substantially diminish performance. The hatched shaded area demarks the presence of hyponatraemia. M indicates the finishing time for the marathon run. IT indicates the approximate finishing time for the Ironman distance triathlon based on literature values for participants running a marathon portion at 10 km/h. For the sodium figures, the solid lines reflect the effect of drinking water only, and hatched lines illustrate the effect of consuming the same volume of a sports drink. The pair of lines of similar type represent the predicted outcomes when total body water accounts for 50% and 63% of body mass. BML, Body mass loss.
The effectiveness of drinking at 400–800 ml/h to sustain hydration over a 42 km run depends on body mass, race speed, and weather. Table 2 provides the predicted BML changes attributable to dehydration in cool/temperate weather. As illustrated in table 2, a 50 kg person consuming 400 ml/h fluid would sustain hydration across the running speeds examined. Consuming 600 ml/h would be predicted to induce overhydration at running speeds below 10 km/h, as would consuming 800 ml/h at 12.5 km/h. Consuming 400–600 ml/h would sustain hydration of a 70 kg runner, except that 400 ml/h at 15 km/h is predicted to produce excessive dehydration. At the other extreme, 800 ml/h is predicted to induce overhydration at running speeds below 10 km/h. For a 90 kg person, consuming 400–800 ml/h would adequately sustain hydration at running speeds of 8.5–10 km/h. At a 12.5 km/h and higher pace, consuming 400 ml/h would be insufficient to prevent excessive dehydration (⩾3% BML), and 800 ml/h would sustain adequate hydration.
Table 2 Predicted percentage body mass loss due to dehydration at end of 42 km marathon held in cool/temperate (18°C) weather for runners of various body mass drinking 400–800 ml/h while running at 8.5–15 km/h.
| Body mass (kg) | Fluid intake (ml/h) | 8.5 km/h | 10 km/h | 12.5 km/h | 15 km/h |
|---|---|---|---|---|---|
| 50 | 400 | −0.4 | −1.1 | −2.0 | −2.6 |
| 600 | 1.6 | 0.6 | −0.6 | −1.5 | |
| 800 | 3.6 | 2.2 | 0.7 | −0.3 | |
| 70 | 400 | −1.8 | −2.3 | −3.0 | −3.4 |
| 600 | −0.4 | −1.1 | −2.0 | −2.6 | |
| 800 | 1.1 | 0.1 | −1.0 | −1.8 | |
| 90 | 400 | −2.6 | −3.0 | −3.5 | −3.9 |
| 600 | −1.5 | −2.1 | −2.8 | −3.2 | |
| 800 | −0.4 | −1.1 | −2.0 | −2.6 |
Underlined type illustrates overdrinking relative to sweating rate. Bold type illustrates sufficient dehydration to compromise performance.
Table 3 provides the predicted body mass changes attributable to dehydration for a warm weather 42 km marathon. Consuming 400 ml/h would be adequate to sustain hydration for a 50 kg person except at the ∼15 km/h pace, at which dehydration is predicted to reach 3.2% BML. Drinking at a rate of 600 ml/h or higher while running at 8.5 km/h or drinking at a rate of 800 ml/h at 10 km/h would produce overhydration. For a 70 kg runner, a 10 km/h pace and consumption at 400 ml/h would result in dehydration, with 2.9% BML before completion of the race. Drinking 800 ml/h is predicted to induce modest overhydration at 8.5 km/h, otherwise consuming 600–800 ml/h seems appropriate to sustain hydration. For a 90 kg person, 400 ml/h would produce dehydration in excess of 3% BML at all running speeds, and 600 ml/h would be adequate until running pace reached ∼12.5 km/h, and thereafter consumption of 800 ml/h would be needed to sustain hydration.
Table 3 Predicted percentage body mass loss due to dehydration at the end of a 42 km marathon held in warm (28°C) weather for runners of various body mass drinking 400–800 ml/h while running at 8.5–15 km/h.
| Body mass (kg) | Fluid intake (ml/h) | 8.5 km/h | 10 km/h | 12.5 km/h | 15 km/h |
|---|---|---|---|---|---|
| 50 | 400 | −1.2 | −1.9 | −2.6 | −3.2 |
| 600 | 0.8 | −0.2 | −1.3 | −2.0 | |
| 800 | 2.7 | 1.5 | 0.1 | −0.9 | |
| 70 | 400 | −2.5 | −2.9 | −3.5 | −3.9 |
| 600 | −1.0 | −1.7 | −2.5 | −3.1 | |
| 800 | 0.4 | −0.5 | −1.6 | −2.3 | |
| 90 | 400 | −3.1 | −3.5 | −4.0 | −4.3 |
| 600 | −2.0 | −2.6 | −3.2 | −3.6 | |
| 800 | −0.9 | −1.7 | −2.5 | −3.0 |
Underlined type illustrates overdrinking relative to sweating rate. Bold type illustrates sufficient dehydration to compromise performance.
Discussion
This paper provides a quantitative approach to assessing the contribution of fluid intake and sweat sodium losses to the plasma sodium dilution during prolonged exercise. We were interested in evaluating whether hyponatraemia could occur without overdrinking relative to sweating rate. The sweat sodium concentrations used for the simulation represent the average and range observed in laboratory and field studies.9,18,22 The fluid intake rates were selected to cover the range recently recommended for curtailing overdrinking during marathon running.12
Central to acceptance of the outcomes of these simulations is the validity of the assumptions used in producing the model. Specifically, it was assumed that sweat rates and sweat electrolyte composition would remain constant over time. We further assumed that running velocity would remain constant for the duration of the modelled scenario. It is likely that running pace and sweat rate and composition would vary during a race. The body water estimates represent the average values for men and women, covering a broad range of expected values. The sweating rate estimate used an accepted estimate of energy expenditure. We minimised the likelihood of overpredicting sweating rate by adjusting for the increasing convective heat transfer as running speed increases. Plasma sodium concentrations were predicted using a validated equation. Most importantly, the model produced sweating rate estimates similar to those measured in marathon participants running at 10–15 km/h23,24,25 and accurately modelled plasma sodium changes measured consequent on prolonged exercise under different rates of fluid replacement and when fluids of various compositions were consumed.26,27,28,29 That said, it is known that sweat rates and composition will vary considerably between individuals, so the predictions are only a “reasonable” average response, and actual sweating rates and plasma sodium estimates are probably normally distributed around the predicted values.13
The simulations predict that overdrinking is the cause of exertional hyponatraemia during ∼42 km marathon events. Across the scenarios evaluated for marathon distances, the magnitude of sweat sodium loss was insufficient to produce enough reduction in plasma sodium for symptomatic hyponatraemia without overdrinking relative to sweating rate. This agrees with the observations that hyponatraemic marathon runners have greater self reported fluid intakes than expected sweating rates.3,4,21
For longer duration events, such as Ironman triathlon, overdrinking relative to sweating rate is the major cause of symptomatic hyponatraemia.2 However, the simulation predicts that it is not a prerequisite condition for hyponatraemia. As illustrated in figs 1–3, when sweat sodium concentrations are above average, but within the normal range, a sufficient sweat sodium deficit can accrue for ultraendurance athletes to finish both dehydrated and hyponatraemic. This is supported by the finding that some triathletes with >2% BML during a triathlon competition have plasma sodium concentrations after the race of 130 mEq/l or below.6,7 Whether the magnitude of hyponatraemia is sufficient to produce symptoms, however, is uncertain, as in most cases of symptomatic hyponatraemia plasma sodium concentrations are less than 125 mEq/l.2,5 In our simulations, this level of hyponatraemia was only reached when sweat sodium was well above average.8,13,18
The risk of developing symptomatic hyponatraemia depends on both the magnitude of sodium dilution and the rate at which the water/electrolyte imbalance occurs.30 As figs 1–3 illustrate, salty sweat reduces the amount of overdrinking necessary to produce hyponatraemia and accelerates the reduction in plasma sodium. In the situations where both dehydration and hyponatraemia are present, aggressive rehydration during recovery from the race with water or electrolyte‐poor drinks could produce rapid dilution of plasma sodium to concentrations associated with symptomatic hyponatraemia. This scenario may explain why many runners with hyponatraemia present with symptoms several hours after completing a race.3
The use of sports drinks instead of water or electrolyte‐free drinks is one strategy for slowing down the development of hyponatraemia. This approach is recommended by the American College of Sports Medicine for ultraendurance races31 and the Institute of Medicine for prolonged physical labour in hot environments.32 As illustrated in fig 4, under conditions in which sweat sodium concentrations are high, fluid replacement with electrolyte sports drink slows down the dilution of plasma sodium, and reduces the likelihood of hyponatraemia development. In the cool/temperate weather conditions, consuming sports drink instead of water delayed the development of hyponatraemia for four to five hours. Thus there is merit in consuming electrolyte‐containing drinks or food during ultraendurance competition, and this should be considered as part of a preventive strategy, particularly if there is a suspicion that the athlete secretes relatively salty sweat.
Electrolyte replacement should be considered only as part of the preventive process; most important is the avoidance of excessive fluid intake. Electrolyte replacement will slow but not prevent the development of hyponatraemia if fluid intake is in gross excess of sweating rate. There is no physiological advantage of drinking above sweating rate.33 Furthermore, as dehydration levels to ∼2% of body mass do not adversely affect exercise performance,13,20 there is a range of dehydration that is acceptable during competition. In addition, the magnitude of water deficit before performance deteriorates probably has individual and event/environment variability. For our simulation, we used 3% BML as the threshold of drinking too little during exercise and replacement above sweating rate as too much. We chose 3% BML because enough time would have accrued since attainment of 2% BML for performance time to be significantly compromised. We then evaluated the efficacy of the IMMDA position stand for sustaining hydration during marathon and longer ultradistance events.
As illustrated in tables 2 and 3, within the boundaries of consuming 400–800 ml/h fluid, there was a rehydration rate that was appropriate for sustaining hydration. Within that fluid intake range, the optimal rate depended on body mass, race pace, and weather. Whereas drinking 600 ml/h was appropriate for a 70–90 kg person in the cool/temperate weather simulation, the same rate of fluid replacement would produce overhydration in a 50 kg person running at pace of 10 km/h or slower. Furthermore, this rate of fluid intake, for a 50 kg person running at a 10 km/h pace with sweat sodium of 50 mEq/l, is predicted to lower plasma sodium concentrations to 123–126 mEq/l by the end of the race. In contrast, a 90 kg person would have developed excessive dehydration. Thus, if athletes implement the range of fluid intakes and qualifiers provided in the IMMDA guidelines, the simulation predicts that excessive dehydration and hyponatraemia would be prevented in a 42 km marathon. However, like the fluid replacement recommendations of other professional organisations,31,34 the IMMDA recommendations need to be sensibly implemented, as arbitrary use of the fluid intake range provided without consideration of the parameters that influence sweating rate will lead to excessive dehydration in some athletes and overhydration in others. Athletes should be encouraged to evaluate their individual fluid losses during practice sessions and develop personal rehydration programmes.
It is important to recognise that the body mass changes predicted by the model reflect only those attributable to changes in total body water. Oxidation of carbohydrate, fat, and protein leads to a loss of mass independent of total body water. Similarly, ventilation leads to respiratory water loss and BML. However, the respiratory water loss typically does not affect total body water, as approximately the same amount of water is produced during cell respiration. These weight losses can be estimated: 0.12 g/kcal and 0.11 g/kcal respectively.24 For a 70 kg participant in a 42 km marathon, they could produce 1% BML without affecting fluid balance.
In summary, fluid intake in excess of sweating rate is the primary cause of hyponatraemia associated with prolonged exercise. Thus preventive strategies to limit overhydration are warranted. The contribution of sweat sodium losses, however, should not be ignored. People who secrete relatively salty sweat can tolerate less overdrinking before developing hyponatraemia. Furthermore, if they rely solely on water or weak electrolyte solutions for fluid replacement and consume only electrolyte‐poor foods, it is possible for them to become both dehydrated and hyponatraemic. Sports beverages can help to delay the development of hyponatraemia in these situations. Fluid replacement strategies designed to prevent symptomatic hyponatraemia should target both fluid and electrolyte intake. Finally, athletes should be encouraged to develop customised fluid replacement programmes, through trial and error, that ensure that enough fluid is consumed to prevent excessive dehydration without risking hyperhydration.
What is already known on this topic
Exercise associated hyponatraemia, although rare, can compromise performance and health
It most often afflicts athletes performing prolonged exercise lasting four hours or longer and who drink over‐aggressively; female and slower participants are also at higher risk of developing the condition
What this study adds
A mathematical model is used to illustrate the complex interactions between exercise intensity, climatic conditions, sweat composition, total body water, drinking rate, and drink composition for sustaining fluid balance and normal natraemia
Strategies to prevent exercise associated hyponatraemia should target fluid intake but also consider solute losses
Acknowledgements
The opinions an assertions contained herein are the private views of the author(s) and are not to be construed as official or as reflecting the views of the Army or Department of Defense. Approved for public release; distribution unlimited.
Footnotes
Competing interests: none declared
References
- 1.Noakes T D, Goodwin N, Rayner B L.et al Water intoxication: a possible complication during endurance exercise. Med Sci Sports Exerc 198517370–375. [PubMed] [Google Scholar]
- 2.Speedy D B, Noakes T D, Schneider C. Exercise‐associated hyponatremia: a review. Emerg Med (Fremantle) 20011317–27. [DOI] [PubMed] [Google Scholar]
- 3.Davis D P, Videen J S, Marino A.et al Exercise‐associated hyponatremia in marathon runners: a two‐year experience. J Emerg Med 20012147–57. [DOI] [PubMed] [Google Scholar]
- 4.Hew T D, Chorley J N, Cianca J C.et al The incidence, risk factors, and clinical manifestations of hyponatremia in marathon runners. Clin J Sport Med 20031341–47. [DOI] [PubMed] [Google Scholar]
- 5.Montain S J, Sawka M N, Wenger C B. Hyponatremia associated with exercise: risk factors and pathogenesis. Exerc Sport Sci Rev 200129113–117. [DOI] [PubMed] [Google Scholar]
- 6.O'Toole M L, Douglas P S, Laird R H.et al Fluid and electrolyte status in athletes receiving medical care at an ultadistance triathlon. Clin J Sport Med 19955116–122. [DOI] [PubMed] [Google Scholar]
- 7.Speedy D B, Noakes T D, Rogers I R.et al Hyponatremia in ultradistance triathletes. Med Sci Sports Exerc 199931809–815. [DOI] [PubMed] [Google Scholar]
- 8.Verde T, Shephard R J, Corey P.et al Sweat composition in exercise and in heat. J Appl Physiol 1982531540–1545. [DOI] [PubMed] [Google Scholar]
- 9.Shirreffs S M, Maughan R J. Whole body sweat collection in humans: an improved method with preliminary data on electrolyte content. J Appl Physiol 199782336–341. [DOI] [PubMed] [Google Scholar]
- 10.Noakes T D, Sharwood K, Collins M.et al The dispsomania of great distance: water intoxication in an Ironman triathlete. Br J Sports Med 200438e16–e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noakes T. Hyponatremia in distance runners: fluid and sodium balance during exercise. Curr Sports Med Rep 20024197–207. [DOI] [PubMed] [Google Scholar]
- 12.Noakes T. Fluid replacement during marathon running. Clin J Sport Med 200313309–318. [DOI] [PubMed] [Google Scholar]
- 13.Food and Nutrition Board of the Institute of Medicine Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington, DC: The National Academies Press, 2005
- 14.Barr S I, Costill D L. Water: can the endurance athlete get too much of a good thing? J Am Diet Assoc 1989891629–1635. [PubMed] [Google Scholar]
- 15.Gagge A P, Gonzalez R R. Mechanisms of heat exchange: biophysics and physiology. In: Fregley MJ, Blatteis CM, eds. Section 4. Environmental physiology. New York: Oxford University Press, 199645–83.
- 16.Kurtz I, Nguyen M K. A simple quantitative approach to analyzing the generation of the dysnatremias. Clin Exp Nephrol 20037138–143. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen M K, Kurtz I. Determinants of plasma water sodium concentration as reflected in the Edelman equation: role of osmotic and Gibbs‐Donnan equilibrium. Am J Physiol 2004286F828–F837. [DOI] [PubMed] [Google Scholar]
- 18.Patterson M J, Galloway S D R, Nimmo M A. Variations in regional sweat composition in normal human males. Exp Physiol 200085869–875. [DOI] [PubMed] [Google Scholar]
- 19.Rogers G, Goodman C, Rosen C. Water budget during ultra‐endurance exercise. Med Sci Sports Exerc 1997291482–1490. [DOI] [PubMed] [Google Scholar]
- 20.Cheuvront S N, Carter R I, Sawka M N. Fluid balance and endurance exercise performance. Curr Sports Med Rep 20032202–208. [DOI] [PubMed] [Google Scholar]
- 21.Almond C S D, Shin A Y, Fortescue E B.et al Hyponatremia among runners in the Boston Marathon. N Engl J Med 20053521550–1556. [DOI] [PubMed] [Google Scholar]
- 22.Maughan R J, Merson S J, Broad N P.et al Fluid and electrolyte intake and loss in elite soccer players during training. Int J Sport Nutr Exerc Metab 200414333–346. [DOI] [PubMed] [Google Scholar]
- 23.Adams W C, Fox R H, Fry A J.et al Thermoregulation during marathon running in cool, moderate, and hot environments. J Appl Physiol 1975381030–1037. [DOI] [PubMed] [Google Scholar]
- 24.Pugh L G C E, Corbett J L, Johnson R H. Rectal temperatures, weight losses, and sweat rates in marathon running. J Appl Physiol 196723347–352. [DOI] [PubMed] [Google Scholar]
- 25.Noakes T D, Adams B A, Myburgh K H.et al The danger of an inadequate water intake during prolonged exercise. Eur J Appl Physiol 198857210–219. [DOI] [PubMed] [Google Scholar]
- 26.Twerenbold R, knechtle B, Kakebeeke T H.et al Effects of different sodium concentrations in replacement fluids during prolonged exercise in women. Br J Sports Med 200337300–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vrijens D M J, Rehrer N J. Sodium‐free fluid ingestion decreases plasma sodium during exercise in the heat. J Appl Physiol 1999861847–1851. [DOI] [PubMed] [Google Scholar]
- 28.Speedy D B, Noakes T D, Rogers I R.et al A prospective study of exercise‐associated hyponatremia in two ultradistance triathletes. Clin J Sport Med 200010136–141. [DOI] [PubMed] [Google Scholar]
- 29.Montain S J, Coyle E F. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J Appl Physiol 1992731340–1350. [DOI] [PubMed] [Google Scholar]
- 30.Adrogué H J, Madias N E. Hyponatremia. N Engl J Med 20003421581–1589. [DOI] [PubMed] [Google Scholar]
- 31.American College of Sports Medicine Position stand on exercise and fluid replacement. Med Sci Sports Exerc. 1996;28: i–vii, [DOI] [PubMed]
- 32.Food and Nutrition Board of the Institute of Medicine Fluid replacement and heat stress. Washington, DC: National Academies Press, 1994 [PubMed]
- 33.Sawka M N, Coyle E F. Influence of body water and blood volume on thermoregulation and exercise performance in the heat. Exerc Sport Sci Rev 199927167–218. [PubMed] [Google Scholar]
- 34.Casa D J, Armstrong L E, Hillman S K.et al National Athletic Trainers' Association position statement: fluid replacement for athletes. J Athl Train 200035212–224. [PMC free article] [PubMed] [Google Scholar]