Abstract
Background
Concussions are potentially serious injuries. The few investigations of prevalence or incidence in youth ice hockey have typically relied on prospective reports from physicians or trainers and did not survey players, despite the knowledge that many athletes do not report probable concussions.
Objective
This study sought to compare concussion rates in youth ice hockey that were estimated from a variety of reporting strategies.
Methods
Rates were calculated from British Columbia Amateur Hockey Association (BCAHA) official injury reports, from direct game observation by minor hockey volunteers (such as coaches and managers), as well as from retrospective surveys of both elite and non‐elite youth players. All research was conducted within the BCAHA.
Results
Estimates from official injury reports for male players were between 0.25 and 0.61 concussions per 1000 player game hours (PGH). Concussion estimates from volunteer reports were between 4.44 and 7.94 per 1000 PGH. Player survey estimates were between 6.65 and 8.32 per 1000 PGH, and 9.72 and 24.30 per 1000 PGH for elite and non‐elite male youth hockey, respectively.
Conclusion
It was found that concussions are considerably under‐reported to the BCAHA by youth hockey players and team personnel.
Keywords: Concussion, injury surveillance, incidence, ice hockey
Concussions are typically generated by rapid acceleration, deceleration, or rotation of the head, leading to compressive, tensile, and shearing forces on the brain.1 The deleterious effects associated with the injury may include neuropsychological deficits, temporary impairments in information processing and cognition, and a variety of symptoms associated with postconcussion syndrome (PCS).1,2,3,4,5,6 There is also emerging evidence supporting the cumulative detrimental effects of multiple concussions, the lingering of PCS for periods of a year or longer, and the risk of coma or death following concussive injuries.1,3,4,5,7,8,9,10 Clearly, concussions can become serious injuries for those victims who experience severe outcomes or suffer from the effects for long durations.
The occurrence of concussion in minor (youth) ice hockey is well established and perhaps not surprising given the speeds at which players travel, the enclosed environment in which they compete, and the collisions, including bodychecks, that are frequently used as an elemental tactic in game play.11,12,13,14,15,16,17,18,19,20,21,22 Epidemiological assessment of concussion is critical to determine the need for prevention and control measures, and various professional and semiprofessional hockey leagues (such as the National Hockey League and Ontario Hockey League) now have surveillance systems in place. However, the incidence of concussion in youth hockey is not firmly established. While a small number of risk estimates have been calculated,14,19,22 most studies are confined to reporting prevalence,11,12,13,15,16,17,20,21,22 which offers some insight into the occurrence of concussion, but does not provide such a clear picture of the risk posed to exposed populations.
Of those investigations that have reported incidence, estimates are often obtained from very different data sources and based on very different methods of surveillance, making comparison difficult. Moreover, epidemiological studies of concussion in youth ice hockey typically only use prospective injury reporting by athletic trainers or sports medicine physicians to establish the frequency of injury.11,12,14,15,16,19,21,22,23,24 While this is may be the preferred methodological approach for clinical diagnosis of concussions, it relies almost entirely on hockey players reporting their injuries to team personnel. In circumstances when a concussion presents with loss of consciousness, noticeable post‐traumatic amnesia, or severe disorientation, this may not be an issue, but the vast majority of concussive injuries are considered mild (no loss of consciousness, or post‐traumatic amnesia) and difficult to diagnose.1,25 In these instances, players would need to recognise and report their symptoms to team personnel before the incident is going to be appropriately recognised and managed. Only a limited number of studies have incorporated player reports of concussive injuries into the prospective study design,12,20,26,27 and the degree to which prospective studies under‐report the occurrence of concussions is unknown.
Given the large numbers of North American and European youth players currently participating in ice hockey, it is important that we obtain an accurate estimate of the concussion rate so that players and parents can begin to make informed decisions about participation and administrators can be guided to control parameters that may affect this rate. In this study, we present evidence to suggest that there is considerable under‐reporting of concussions in youth ice hockey and that rate estimates calculated from official injury reports data woefully underestimate the true incidence. We compared rate estimates of concussion and incidents of concern calculated from a Canadian provincial league's official injury forms, reports from minor hockey team volunteers, and retrospective surveys of youth hockey players.
MATERIALS AND METHODS
Three different strategies were used in four different projects to assess the rate of concussion in youth hockey: official injury reports, direct observation, and retrospective player surveys. All data were collected from teams and games in the British Columbia Amateur Hockey Association (BCAHA), a provincial governing branch of Hockey Canada. Body checking is permitted in male hockey from 11 years of age onward. Informed written consent was obtained in all projects when there was direct contact with participants. The research ethics board of Simon Fraser University approved these projects.
Official injury reports
The BCAHA provided injury reports from the pee wee (11 and 12 years), bantam (13 and 14 years), and midget (15–17 years) age divisions for male hockey players, and also reports from female hockey divisions (12–19 years). Injury reports are filed by team personnel and collected by the BCAHA and Hockey Canada on an ongoing basis for insurance purposes and have been used for tracking injuries (see www.hockeycanada.ca/e/develop/insurance/downloads/safety_net_e.pdf). According to Hockey Canada, they are to be completed
“for each case where an injury is sustained by a player … at a sanctioned hockey activity.”
Official injury reports include descriptive information about the injured player (such as name and home association), the details of the event, and the nature of the injury. For the purposes of this study, copies of all forms submitted to the BCAHA during the 2003–2004 season were screened for explicit reports of concussions.
Direct observation
During the 2002–2003 hockey season, minor hockey team volunteers (coaches, managers, or safety personnel) in a district of the BCAHA were asked to record and report the details of “head incidents of concern” sustained by their team's players during games. A head incident of concern, or incident, was defined as a physician diagnosed concussion or an episode considered seriously indicative of a concussion based on observed signs or symptoms. Most coaches and all safety personnel have passed the Canadian Hockey Safety Program, which includes information addressing concussion symptoms and assessment. Although the signs and symptoms associated with concussion can be associated with other conditions, when presenting after rapid acceleration or deceleration of the head they are considered indicative of concussion, and diagnosis with symptoms has been an integral element of other investigations.4,13,24,28,29,30
In total, 44 team volunteers represented 44 teams and 792 players from three hockey age divisions: pee wee, bantam, and midget. Participants were phoned or e‐mailed with project updates twice monthly. Reports of head incidents of concern were completed using a standardised form submitted by mail, fax, drop box, or an online web page.
Retrospective player surveys
A self reporting retrospective questionnaire was developed to gather information about the concussion histories of youth hockey players. Participants were asked to report if they had ever suffered a significant hockey induced hit to the head that presented signs and symptoms of concussion. Participants who reported sustaining such an injury (a head incident of concern) then reported the details of the event and the associated symptoms. Players could report any head injuries sustained in their hockey careers, but only injuries incurred in the current or prior season were included in the analysis to improve the accuracy of the injury recall.31
Elite players
Participants in 12 BCAHA elite hockey tournaments occurring between 2001 and 2003 (three tournaments each year) completed the questionnaire. The two annual male tournaments included players aged in the under‐16 and under‐17 year age groups, respectively, while the female annual tournament included players <18 years. Histories of players who participated in two or more years of competition and who reported suffering a concussion were reviewed to ensure each incident was counted only once.
Non‐elite (recreational) players
Non‐elite hockey players completed a similar self report retrospective concussion history questionnaire. Testing included players aged 11–17 years (pee wee, bantam, and midget) from a single BCAHA minor hockey association in January 2004.
Calculation of incidence
Recent sport surveillance literature has expressed incidence in terms of injuries per 1000 athlete exposures (AE) and injuries per 1000 player game hours (PGH), so we present both calculations here. Previous research has indicated the vast majority of concussions and other hockey induced injuries occur during games.17,26,29,32,33,34 For this reason, all concussions or incidents were assumed to have transpired during games and the number of concussions that occurred during practices was assumed to be negligible.
Because time at risk (AE and PGH) for individual players was not tracked during these investigations, exact player exposure during games could not be calculated. Thus, player game time at risk was estimated for an 18 member team playing an entire game at full strength (no penalties) with five skaters and a goalie on the ice. A typical BCAHA sanctioned game is 45 minutes of stopped time played within 1–1¼ hours. PGH at risk is equal to six skaters/team × 0.75 hours per game, or 4.50 hours/game/team. Each player on an 18 member team is therefore at risk for 0.25 hours per game. Similar methods have been used in prior investigations.16,19,25,26
Athlete exposures
For the purposes of this investigation, an AE was considered participation in a game where the player is exposed to the possibility of injury. The incidence of concussions or incidents of concern per 1000 AE was calculated as the number of concussions reported during the observation period/the total number of AE among all players during observation period × 1000 AE. The number of games (AE) that occurred during the observation period of each study cohort varied depending on the age and skill groups involved, so minimum and maximum estimates of the total number of games played during each study period were determined based on a sample of schedules from each cohort's category of competition. The minimum total AE among all players during each observation period was calculated as number of players × minimum number of games for a specific cohort, and maximum total AE among all players during each observation period was number of players × maximum number of games for a specific cohort. Minimum and maximum estimates of incidence were then calculated using the maximum and minimum total AE, respectively.
Player game hours
The incidence of concussion or incidents of concern per 1000 PGH was calculated as (number of concussions reported during observation period/total PGH at risk during observation period) × 1000 PGH. Minimum and maximum total PGH at risk during each observation period were calculated as minimum total games played by all players (AE) × 0.25 hours/player/game and maximum total games played by all players (AE) × 0.25 hours/player/game, respectively. Minimum and maximum estimates of incidence were then calculated using the maximum and minimum total PGH at risk, respectively.
RESULTS
The details and results of the investigations as well as estimates of the rates of concussions or incidents of concern in terms of both AE and PGH are presented in table 1. The duration of observation for each project is reported as the time period. In considering the retrospective survey results, between 2001 and 2004, 178 (of 497) male and 112 (of 326) female elite players reported sustaining at least one hockey induced concussion. Based on the reported age when the concussion occurred and player birth dates, 79 elite male and 69 elite female athletes reported at least one hockey induced concussion in the current or prior season. Of 107 non‐elite athletes, 26 reported sustaining at least one concussion during the current or prior season.
Table 1 Measured parameters and minimum and maximum incidence estimates across different observation strategies.
| Parameter | BCAHA official injury reports | Direct observation | Retrospective survey | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male (PW, B, M) | Female (all levels) | Volunteer reports | Elite (male) | Elite (female) | Non‐elite | |||||||
| Time period | 1 season | 1 season | 3.5 months | 2 seasons | 2 seasons | 2 Seasons | ||||||
| No. of players at risk | 19548 | 5017 | 792 | 475 | 309 | 107 | ||||||
| No. of CX or IOC* | 60 | 7 | 22 | 79 | 69 | 26 | ||||||
| AE | ||||||||||||
| Minimum no. | 20 | 20 | 14 | 80 | 80 | 40 | ||||||
| Maximum no. | 50 | 50 | 25 | 100 | 100 | 100 | ||||||
| Minimum incidence* | 0.06 | 0.03 | 1.11 | 1.66 | 2.23 | 2.43 | ||||||
| Maximum incidence* | 0.15 | 0.07 | 1.98 | 2.08 | 2.79 | 6.07 | ||||||
| PGH | ||||||||||||
| Minimum no. | 97 740 | 25 085 | 2772 | 9500 | 6180 | 1070 | ||||||
| Maximum no. | 244 350 | 62 713 | 4950 | 11 875 | 7725 | 2675 | ||||||
| Minimum incidence* | 0.25 | 0.09 | 4.44 | 6.65 | 8.93 | 9.72 | ||||||
| Maximum incidence* | 0.61 | 0.28 | 7.94 | 8.32 | 11.17 | 24.30 | ||||||
PW, Pee wee; B, Bantam; M, Midget; CX, concussion; IOC, incident of concern. *Per 1000 PGH.
DISCUSSION
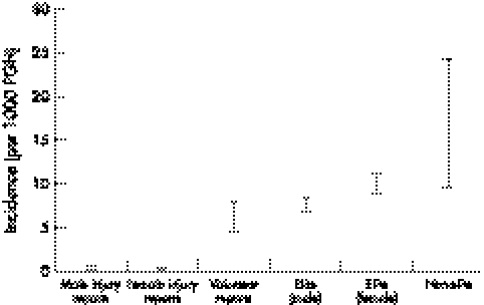
The range of incidences per 1000 PGH calculated from each observation strategy is shown in fig 1. There are considerable differences between the incidences of concussion based on official injury reports and those calculated from the other observation strategies (>30 fold difference between official injury reports and non‐elite retrospective surveys for male players). Indeed, even using very conservative estimates of the number of games in each study cohort, our data suggest considerable under‐reporting of concussions to the BCAHA. A similar figure is observed if the results are calculated in units of 1000 AE.
Figure 1 Range of incidence estimates per 1000 PGH across different observation strategies.
The prevalence of self reported incidents suggests that many players (elite and non‐elite alike) recognise when they have sustained a significant hit to the head that presents signs and symptoms of concussion. Unfortunately, many of these incidents do not appear to be reported (or perhaps even recognised) by team volunteers and fewer still are reported to the BCAHA. This is despite Hockey Canada's Coach and Safety Person Protocol, which recommends that all players demonstrating signs of concussion be removed from play and not permitted to return until advised by a physician (www.hockeycanada.ca/e/develop/safety/concussion.html). The under‐reporting of concussions also appears to occur in female hockey.
Table 2 compares median rate estimates from this study with those calculated using reported data from previous investigations of injury incidence in youth male ice hockey. With the exception of Gerberich et al,13 the cited studies used a prospective surveillance system requiring injury diagnosis by an athletic trainer or a physician. Roberts et al18,19 report rates similar to or exceeding those reported by the athletes in our investigation, perhaps because these studies included all injuries evaluated by a team physician or trainer, regardless of severity, and did not necessitate referral to a physician due to injury,21,22 24 hours' absence from participation due to injury,21,22 or loss of consciousness or post‐traumatic amnesia.13
Table 2 Investigation of male youth ice hockey incidence and calculated estimates from the literature .
| Study | Period | Type | Country | Age (years) | No. of players | No of concussions | Exposure (PGH) | Incidence (/1000 PGH) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Official reports | 2003–2004 | Retro | Canada | 12 to 17 | 19548 | 60 | 17 1045 | 0.35 | ||||||||
| Volunteer reports | 2002–2003 | Pro | Canada | 12 to 17 | 792 | 22 | 3861 | 5.70 | ||||||||
| Elite | 2001–2003 | Retro | Canada | 15 to 17 | 475 | 79 | 10 688 | 7.39 | ||||||||
| Non‐elite | 2004 | Retro | Canada | 11 to 17 | 107 | 26 | 1605 | 16.20 | ||||||||
| Gerberich13 | 1982–1983 | Retro | USA | 16.1‡ | 251 | 22 | 4141.5* | 4.35 | ||||||||
| Roberts19 | 1993–1994 | Pro | USA | 12 to 13 | 132 | 2 | 86.4 | 23.15 | ||||||||
| 14 to 15 | 127 | 1 | 93.6 | 10.68 | ||||||||||||
| 12 to 15 | 163 | 2 | 108 | 18.52 | ||||||||||||
| Roberts18 | 1994 | Pro | USA | <20 | 273 | 4 | 213.9 | 18.70 | ||||||||
| Smith21 | 1994–1995 | Pro | USA | NR | 86 | 1† | 639‡ | 1.56 | ||||||||
| Stuart22 | 1993–1994 | Pro | USA | 16 to 21 | 66 | 0 | 4707 | 0 |
The first four rows of the table are from the present study. Results are calculated from: *mean number of game hours per player × number of players; †number of injuries × proportion of injuries that were concussions; ‡number of injuries ÷ incidence of injury per player game hour. ‡Median; all other numerical values in this column are range. Retro, retrospective; P, prospective; NR, not reported.
The variability in estimates from this investigation and across past studies reiterates a call for standardisation of surveillance measures and methods in ice hockey.35 Table 2 supports the notion that the surveillance methods used may dramatically influence estimates of injury and, in turn, the conclusions of an investigation. Our findings suggest that future studies must continue to make clear the possible limitations of their methods.
This study is subject to some important limitations. Firstly, it was assumed that team volunteers and players are capable of appropriately identifying the signs and symptoms consistent with a concussive injury. Although many coaches and all safety personnel have passed the Canadian Hockey Safety Program, we did not confirm if our volunteers had completed the course. Secondly, a definitive diagnosis criterion for concussions remains elusive, so we were limited to using concussion symptoms. Thirdly, selection bias may be a limitation in this study; team volunteers who had prior experience in dealing with concussions or had an attitudinal bias may have been more willing to volunteer for the programme or report incidents than were the general population of team volunteers. Fourthly, the questionnaire may not have captured all possible concussions; surveyed players who had unwittingly sustained a previous concussion because they were unable to recognise the associated symptoms, or who sustained a potential concussion by way of an indirect mechanism may not have answered affirmatively. We believe, however, that both these questionnaire limitations lend further evidence to support the under‐reporting of concussion in youth ice hockey. It should also be noted that the use of this tool may have introduced recall bias. Finally, the means by which we calculated time at risk for each study cohort were based on educated assumptions of the number of games played and time at risk during each game. This was necessary in order to utilise several data sources in a comparison using measures consistent with the literature (AE and PGH).
It should be noted that these estimates are not intended to be conclusive measures of the rate of concussion in youth hockey, but rather to demonstrate the considerable differences in rates of concussion or incidents as calculated from reports to the hockey governing bodies, from volunteers, and by the players who suffer injuries seriously indicative of concussions. We feel they are strong evidence to indicate a considerable under‐reporting of concussive injuries in youth hockey, both to the hockey governing bodies and to team personnel. In addition, we feel these results suggest studies relying exclusively on prospective injury reports by team personnel—that is, studies that do not regularly consult with players, are likely to under‐report the true rate of concussion.
CONCLUSION
Based on the converging evidence cited above, the under‐reporting of concussions to the hockey governing bodies, both by players and by bench staff, remains a major problem in youth hockey in British Columbia. There is no reason to believe that this is not also the case in other Canadian provinces, which operate under the same principles of Hockey Canada. The under‐reporting of these injuries to the hockey governing bodies has important implications for decision makers and parents who rely on these data to make informed decisions about the risk of concussion in the game of hockey. Of particular concern to us is the under‐reporting of concussions by players to team staff. Players who do not report incidents indicative of concussions and return to play while still symptomatic may be placing themselves at risk of further injury, thereby increasing the risk of the cumulative detrimental effects of multiple concussions and the risk of further injury.7,8,9,36
What is already known on this topic
Goodman et al25 found 50% of junior hockey players, when surveyed retrospectively, did not report injuries they recognised as concussions during prospective investigation.
Researchers appear to acknowledge this under‐reporting, but no efforts have been made to quantify it.
What this study adds
It is the first to demonstrate there is a substantial under‐reporting of concussion at several levels within youth hockey organisations.
It also demonstrates methods dependent on prospective player reports alone likely underestimate the true risk.
Hockey Canada has recently indicated a desire to expand the use of injury reports to create an injury tracking system in minor hockey (see website given above). Unless appropriate steps are taken to address the under‐reporting of concussions and other injuries, results obtained from this data source may be inaccurate. We feel our findings indicate the importance of surveying athletes engaged in a prospective study of sport induced injury. Studies based solely on administrative records (such as official injury reports or hospital records) or reports from team staff (such as athletic therapists, physicians, and volunteers) may not account for all concussions.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the assistance of Dr D Voaklander in the preparation of this manuscript and thank Dr W Roberts for encouraging the inclusion of previous incidence research. We also thank the anonymous reviewers for their insight and advice and are grateful to the BCAHA and Hockey Canada for their ongoing cooperation in our research. This study was funded by a grant from the Canadian Institutes of Health Research.
Abbreviations
AE - athlete exposures
BCAHA - British Columbia Amateur Hockey Association
PCS - postconcussion syndrome
PGH - player game hours
Footnotes
Competing interests: none
References
- 1.Cantu R C. Cerebral concussion in sport: Management and prevention. Sports Med 19921464–74. [DOI] [PubMed] [Google Scholar]
- 2.Grindel S H. Epidemiology and pathophysiology of minor traumatic brain injury. Curr Sports Med Rep 2003218–23. [DOI] [PubMed] [Google Scholar]
- 3.Gronwall D, Wrightson P. Delayed recovery of intellectual function after minor head injury. Lancet 19742605–609. [DOI] [PubMed] [Google Scholar]
- 4.Macciocchi S N, Barth J T, Alves W M.et al Neuropsychological functioning and recovery after mild head injury in college athletes. Neurosurgery 199639510–514. [PubMed] [Google Scholar]
- 5.Macciocchi S N, Barth J T, Littlefield L M. Outcome after mild head injury. Neurol Athletic Head Neck Inj 19981727–36. [DOI] [PubMed] [Google Scholar]
- 6.McCrea M, Kelly J P, Randolph C.et al Immediate neurocognitive effects of concussion. Neurosurgery 2002501032–1042. [DOI] [PubMed] [Google Scholar]
- 7.Cantu R C. Second‐impact syndrome. Clin Sports Med 19981737–44. [DOI] [PubMed] [Google Scholar]
- 8.Collins M W, Lovell M R, Iverson G L.et al Cumulative effects of concussion in high school athletes. Neurosurgery 2002511175–1179. [DOI] [PubMed] [Google Scholar]
- 9.Gaetz M, Goodman D, Weinberg H. Electrophysiological evidence for the cumulative effects of concussion. Brain Inj 2000141077–1088. [DOI] [PubMed] [Google Scholar]
- 10.Gennerelli T A, Thibault L E, Graham D I. Diffuse axonal injury: an important form of traumatic brain damage. Neuroscientist 19984202–215. [Google Scholar]
- 11.Brust J D, Leonard B J, Phely A.et al Children's ice hockey injuries. Am J Dis Child . 1992;146741–747. [DOI] [PubMed]
- 12.Dryden D M, Francescutti L H, Rowe B H.et al Epidemiology of women's recreational ice hockey injuries. Med Sci Sports Exerc 2000321378–1383. [DOI] [PubMed] [Google Scholar]
- 13.Gerberich S G, Finke R, Madden M.et al An epidemiological study of high school ice hockey injuries. Childs Nerv Syst 1987359–64. [DOI] [PubMed] [Google Scholar]
- 14.Gröger A. Ten years of ice hockey‐related‐injuries in the German Ice Hockey Federation. Sportverl Sportschad 20011582–86. [DOI] [PubMed] [Google Scholar]
- 15.McFaull S. Contact injuries in minor hockey: a review of the CHIRPP database for the 1998/1999 hockey season. CHIRPP News 2001191–9. [Google Scholar]
- 16.Pinto M, Kuhn J E, Greenfield M V H.et al Prospective analysis of ice hockey injuries at the junior A level over the course of one season. Clin J Sports Med 1999970–74. [DOI] [PubMed] [Google Scholar]
- 17.Reid S R, Losek J D. Factors associated with significant injuries in youth ice hockey players. Pediatr Emerg Care 199915310–313. [DOI] [PubMed] [Google Scholar]
- 18.Roberts W O, Brust J D, Leonard B.et al Fair‐play rules and injury reduction in ice hockey. Arch Pediatr Adolesc Med 1966150140–145. [DOI] [PubMed] [Google Scholar]
- 19.Roberts W O, Brust J D, Leonard B. Youth ice hockey tournament injuries: rates and patterns compared to season play. Med Sci Sports Exerc 19993146–51. [DOI] [PubMed] [Google Scholar]
- 20.Roy M A, Bernard D, Benoît R.et al Body checking in pee wee hockey. Phys Sportsmed 198917119–126. [DOI] [PubMed] [Google Scholar]
- 21.Smith A M, Stuart M J, Weise‐Bjornstal D M.et al Predictors of injury in ice hockey players: a multivariate, multidisciplinary approach. Am J Sports Med 199725500–507. [DOI] [PubMed] [Google Scholar]
- 22.Stuart M J, Smith A M, Nieva J J.et al Injuries in youth ice hockey: a pilot surveillance strategy. Mayo Clin Proc 199570350–356. [DOI] [PubMed] [Google Scholar]
- 23.Sutherland G W. Fire on ice. Am J Sports Med 19764264–269. [DOI] [PubMed] [Google Scholar]
- 24.Daffner R H. Injuries in amateur ice hockey: a two‐year analysis. J Family Pract 19774225–227. [PubMed] [Google Scholar]
- 25.Guskiewicz K M, Weaver N L, Padua D A.et al Epidemiology of concussion in collegiate and high school football players. Am J Sports Med 200028643–650. [DOI] [PubMed] [Google Scholar]
- 26.Goodman D, Gaetz M, Meichenbaum D. Concussions in hockey: there is cause for concern. Med Sci Sports Exerc 2001332004–2009. [DOI] [PubMed] [Google Scholar]
- 27.Tegner Y, Lorentzon R. Ice hockey injuries: incidence, nature and causes. Br J Sp Med 19912587–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alves W, Macciocchi S N, Barth J T. Postconcussive symptoms after uncomplicated mild head injury. J Head Trauma Rehabil 1993348–59. [Google Scholar]
- 29.Covassin T, Swanik C B, Sachs M L. Epidemiological considerations of concussions among intercollegiate athletes. Appl Neuropsycol 20031012–21. [DOI] [PubMed] [Google Scholar]
- 30.Schulz M R, Marshall S W, Mueller F O.et al Incidence and risk factors for concussion in high school athletes, North Carolina, 1996–1999. Am J Epidemiol 2004160937–944. [DOI] [PubMed] [Google Scholar]
- 31.Gabbe B J, Finch C F, Bennell K L.et al How valid is a self reported 12 month sports injury history? Br J Sp Med 200337545–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mölsä J, Kujala U, Näsman O.et al Injury profile in ice hockey from the 1970s through the 1990s in Finland. Am J Sports Med 200028322–326. [DOI] [PubMed] [Google Scholar]
- 33.Pettersson M, Lorentzon R. Ice hockey injuries: a 4‐year prospective study of a Swedish elite ice hockey team. Br J Sp Med 199327251–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tegner Y, Lorentzon R. Ice hocky injuries: incidence, nature and causes. Br J Sp Med 19912587–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pelletier R L, Montelpare W J, Stark R M. Intercollegiate ice hockey injuries. A case for uniform definitions and reports. Am J Sports Med 19932178–81. [DOI] [PubMed] [Google Scholar]
- 36.Tysvaer A T, Storli O V, Bachen N I. Soccer injuries to the brain: A neurologic and electroencephalographic study of former players. Acta Neruol Scand 198980151–156. [DOI] [PubMed] [Google Scholar]