Abstract
Spontaneous rupture of membranes (ROM) is a normal component of labor and delivery. Premature ROM (PROM) refers to rupture of the fetal membranes prior to the onset of labor irrespective of gestational age. Once the membranes rupture, delivery is recommended when the risk of ascending infection outweighs the risk of prematurity. When PROM occurs at term, labor typically ensues spontaneously or is induced within 12 to 24 hours. The management of pregnancies complicated by preterm PROM (defined as PROM occurring prior to 37 weeks of gestation) is more challenging. Preterm PROM complicates 2% to 20% of all deliveries and is associated with 18% to 20% of perinatal deaths. Management options include admission to hospital, amniocentesis to exclude intra-amniotic infection, and administration of antenatal corticosteroids and broad-spectrum antibiotics, if indicated. This article reviews in detail the contemporary diagnosis and management of preterm PROM.
Key words: Premature rupture of membranes, Preterm premature rupture of membranes, Preterm birth, Antibiotics, Antenatal corticosteroids
Premature rupture of membranes (PROM) refers to rupture of the fetal membranes prior to the onset of labor,1,2 and can occur at any gestational age-even at 42 weeks’ gestation. For this reason, it is also referred to as prelabor ROM. PROM can occur either at term or preterm (< 37 weeks). Prolonged PROM refers to PROM greater than 24 hours, and is associated with an increased risk of ascending infection.1,2
Scope of the Problem
Approximately 8% to 10% of term pregnancies will experience spontaneous ROM prior to the onset of uterine activity.1–4 Preterm PROM-defined as PROM prior to 37 weeks of gestation-complicates 2% to 4% of all singleton and 7% to 20% of twin pregnancies.1,2,5,6 It is the leading identifiable cause of premature birth and accounts for approximately 18% to 20% of perinatal deaths in the United States.1,2,5–9
Etiology and Risk Factors
Histologic studies of the site of membrane rupture at term have demonstrated a zone of altered morphology characterized by thickening of the connective tissue components of the membranes, thinning of the cytotrophoblast layer and decidua, and disruption of the connections between amnion and chorion. These normal physiologic changes accompany cervical ripening in preparation for labor at term, and result in focal weakening of the fetal membranes in the region of the internal cervical os that predisposes to rupture at that site. At a cellular level, these changes result from the release of phospholipases, eicosanoids (especially prostaglandin E2), cytokines, elastases, matrix metalloproteinases, and/or other proteases in response to a physiologic or pathologic stimulus.1,2,10 Although the downstream cellular changes may be similar, the inciting etiologies in preterm PROM are likely different from term PROM.
A number of risk factors for spontaneous preterm PROM have been identified (Table 1).1,2,11 Intra-amniotic infection and decidual hemorrhage (placental abruption) occurring remote from term, for example, may release proteases into the choriodecidual tissues and amniotic fluid, leading to rupture of membranes. Indeed, placental abruption is seen in 4% to 12% of pregnancies complicated by preterm PROM, and is more common in pregnancies complicated by preterm PROM prior to 28 weeks of gestation.2,12,13 However, whether it is the cause of PROM or a consequence of acute uterine decompression is not known. Invasive uterine procedures performed during pregnancy (such as amniocentesis, chorionic villus sampling, fetoscopy, and cervical cerclage) can damage the membranes, causing them to leak, but these are rare causes of preterm PROM.
Table 1.
Risk Factors for Spontaneous Preterm Premature Rupture of Membranes
| Maternal Factors |
|
| Uteroplacental Factors |
|
| Fetal Factors |
|
Data from ACOG Committee on Practice Bulletins-Obstetrics.2
The risk of recurrence of preterm PROM is 16% to 32%, as compared with approximately 4% in women with a prior uncomplicated term delivery.14–16 This percentage may be increased if there is evidence of cervical shortening or uterine contractions in the second trimester.16 However, most cases of preterm PROM occur in otherwise healthy women without identifiable risk factors.2 Epidemiologic and historic factors that are known not to be associated with preterm PROM include sexual intercourse, speculum examinations, maternal exercise, and parity.
Natural History of Pregnancies Complicated by Preterm PROM
Latency refers to the interval between rupture of the membranes and the onset of labor. A number of factors are known to affect the latency period, including:
Gestational age. An inverse relationship exists between gestational age at the time of ROM and latency. At term, 50% of pregnancies complicated by PROM will go into labor spontaneously within 12 hours, 70% within 24 hours, 85% within 48 hours, and 95% within 72 hours in the absence of obstetric intervention.1,2,4,17 In women with preterm PROM remote from term, 50% will go into labor within 24 to 48 hours and 70% to 90% within 7 days.1,2,18,19 Furthermore, women with preterm PROM at 24 to 28 weeks of gestation are likely to have a longer latency period than those with preterm PROM closer to term.
Degree of oligohydramnios. The more severe the degree of oligohydramnios, the shorter the latency period.20,21 Severe oligohydramnios may represent a larger hole in the membranes or evidence of early fetal compromise with diminished urine output.21
Sonographic myometrial thickness. Evidence of excessive thinning of the myometrium in nonlaboring women with preterm PROM (< 12 mm) as measured by transabdominal ultrasound has been associated with a shorter latency interval.22
Number of fetuses. In general, twin pregnancies complicated by preterm PROM have a shorter latency period than singleton pregnancies.23,24
Pregnancy complications. Evidence of pregnancy complications (such as intra-amniotic infection, placental abruption, or active labor) or nonreassuring fetal testing (previously referred to as fetal distress) will lead to early delivery and a shortened latency interval.
Complications
The fetal membranes serve as a barrier to ascending infection. Once the membranes rupture, both the mother and fetus are at risk of infection and of other complications.
Neonatal complications relate primarily to the gestational age at rupture of membranes. Preterm PROM is associated with a 4-fold increase in perinatal mortality and a 3-fold increase in neonatal morbidity, including respiratory distress syndrome (RDS), which occurs in 10% to 40% of women with preterm PROM and is responsible for 40% to 70% of neonatal deaths; polymicrobial intraamniotic infection, which occurs in 15% to 30% of women with preterm PROM and accounts for 3% to 20% of neonatal deaths; and intraventricular hemorrhage (IVH).1,2,18,19 Despite initial suggestions, the weight of evidence in the literature suggests that preterm PROM is not associated with an acceleration in pulmonary maturation.25 Other neonatal complications include fetal pulmonary hypoplasia, which develops in 26% of preterm PROM prior to 22 weeks; skeletal deformities, which complicate 12% of preterm PROM, related to severity and duration of preterm PROM; cord prolapse, especially in pregnancies with a nonvertex presentation; and increased cesarean delivery for malpresentation.1,2 Severe oligohydramnios in the setting of preterm PROM results in an increased incidence of cord compression and nonreassuring fetal testing (fetal distress) in labor, leading to a further increase in the risk of cesarean delivery. In this setting, amnioinfusion with saline may decrease the risk of cesarean delivery, but whether such an approach improves perinatal outcome is not clear.26 Preterm PROM and exposure to intrauterine inflammation/infection have been associated with an increased risk of neurodevelopmental impairment.2,27,28 Infection, cord accident, and other factors contribute to the 1% to 2% risk of intrauterine fetal demise (stillbirth) after preterm PROM.2,29
Maternal complications include clinically evident intra-amniotic infection, which occurs in 13% to 60% of women with preterm PROM as compared with 1% at term, and postpartum endometritis, which occurs in 2% to 13% of women with preterm PROM.1,2,30 Chorioamnionitis is seen more commonly in women with prolonged preterm PROM, severe oligohydramnios, multiple vaginal examinations, and preterm PROM at an early gestational age. Additionally, because more fetuses with preterm PROM present with malpresentation (eg, breech), the risk of cesarean delivery with its attendant surgical risks to the parturient is higher in preterm PROM as compared with term deliveries.
Differential Diagnosis
Rupture of the membranes typically presents as a large gush of clear vaginal fluid or as a steady trickle. The differential diagnosis includes leakage of urine (urinary incontinence); excessive vaginal discharge, such as physiologic discharge or bacterial vaginosis; and cervical mucus (show) as a sign of impending labor.
Diagnosis
Preterm PROM is largely a clinical diagnosis. It is typically suggested by a history of watery vaginal discharge and confirmed on sterile speculum examination. The traditional minimally invasive gold standard for the diagnosis of ROM relies on clinician ability to document 3 clinical signs on sterile speculum examination: (1) visual pooling of clear fluid in the posterior fornix of the vagina or leakage of fluid from the cervical os; (2) an alkaline pH of the cervicovaginal discharge, which is typically demonstrated by seeing whether the discharge turns yellow nitrazine paper to blue (nitrazine test); and/or (3) microscopic ferning of the cervicovaginal discharge on drying. Evidence of diminished amniotic fluid volume (by Leopold’s examination or ultrasound) alone cannot confirm the diagnosis,2 but may help to suggest it in the appropriate clinical setting.
With the possible exception of direct visualization of amniotic fluid spurting from the cervical os, all of these clinical signs have limitations in terms of diagnostic accuracy, cost, and technical ease. Moreover, such tests become progressively less accurate when more than 1 hour has elapsed after the membranes have ruptured. As such, reliance on clinical assessment alone leads to both false-positive and false-negative results. For example, the nitrazine test is designed only to confirm an alkaline pH in the cervicovaginal secretions (the pH of the vaginal secretions is generally 4.5–6.0, whereas amniotic fluid usually has a pH of 7.1–7.3), and yet it is the most common test used to diagnose PROM. It is associated with high false-positive rates related to cervicitis, vaginitis (bacterial vaginosis), and contamination with blood, urine, semen, or antiseptic agents.2,31–33 As such, the sensitivity and specificity of this test in diagnosing ROM ranges from 90% to 97% and 16% to 70%, respectively.34,35 The fern test refers to microscopic crystallization of amniotic fluid on drying, and may give false-positive results due to fingerprints or contamination with semen and cervical mucus as well as false-negative results due to technical error (using a dry swab to collect the sample) or contamination with blood.32,36,37 Reported sensitivity and specificity for the fern test are 51% and 70%, respectively, in patients without labor and 98% and 88%, respectively, in patients in labor.38
The Importance of Confirming the Diagnosis
Early and accurate diagnosis of preterm PROM would allow for gestational age-specific obstetric interventions designed to optimize perinatal outcome and minimize serious complications, such as cord prolapse and infectious morbidity (chorioamnionitis, neonatal sepsis).1,6,7 Conversely, a false-positive diagnosis of preterm PROM may lead to unnecessary obstetric interventions, including hospitalization, administration of antibiotics and corticosteroids, and even induction of labor.1,39,40 A timely and accurate diagnosis of PROM is therefore critical to optimize pregnancy outcome-so critical, in fact, that an amnio-dye test (tampon test) may be recommended if conventional tests for preterm PROM are equivocal and if the pregnancy is remote from term. This test involves amniocentesis and instillation of dye into the amniotic cavity. Indigo carmine is preferred because of the association between methylene blue dye and fetal methemoglobinemia.41 Leakage of blue-stained fluid into the vagina within 20 to 30 minutes as evidenced by staining of a tampon is regarded as a definitive diagnosis of preterm PROM. Although considered by many investigators as the gold standard for the diagnosis of preterm PROM, the amnio-dye test is an invasive procedure with inherent risks that include bleeding (placental abruption), infection, iatrogenic PROM, and miscarriage. For these reasons, a rapid, accurate, inexpensive, and noninvasive test for the diagnosis of PROM is urgently needed.
Because of the limitations with the current gold standard for the diagnosis of preterm PROM (namely, clinical assessment of pooling, nitrazine, and/or ferning), investigators have long been searching for an alternative and more objective test. Such tests are based primarily on the identification in the cervicovaginal discharge of one or more biochemical markers that are present in the setting of ROM, but absent in women with intact membranes. Several such markers have been studied, including alpha-fetoprotein (AFP),42–44 fetal fibronectin (fFN),45 insulinlike growth factor binding protein 1 (IGFBP-1),34,35,46,47 prolactin,44,48,49 beta-subunit of human chorionic gonadotropin (β-hCG),43,44,50,51 creatinine,43,52 urea,52 lactate,53 and placental alpha-microglobulin 1 (PAMG-1).54–57 However, results using such tests have been variable (Table 2). Although proteomic technology has recently been used to identify novel protein biomarkers in the cervicovaginal discharge of women who have intra-amniotic infection58 or who subsequently deliver preterm,59,60 this technology has not been applied to the problem of preterm PROM.
Table 2.
Performance of Noninvasive Tests to Diagnose Rupture of the Fetal Membranes
| Sensitivity | Specificity | PPV | NPV | |||
|---|---|---|---|---|---|---|
| Test/Reference | Name of Test | Cutoff | (%) | (%) | (%) | (%) |
| Nitrazine (pH)31,34,35 | — | Positive/negative | 90–97 | 16–70 | 63–75 | 80–93 |
| Ferning and/or pooling31,33,36,37 | — | Positive/negative | 51–98 | 70–88 | 84–93 | 97–97 |
| AFP42–44 | ROM Check® (Adeza | > 30 µg/L | 90–94 | 95–100 | 94–100 | 91–94 |
| Biomedical Corp., | ||||||
| Sunnyvale, CA) | ||||||
| Fetal fibronectin45 | — | > 50 ng/mL | 97–98 | 70–97 | 74–93 | 98–100 |
| IGFBP-134,35,46,47 | PROM-TEST® (Medix | > 3µg/L | 74–97 | 74–97 | 73–92 | 56–87 |
| Biochimica, Kauinianen, | ||||||
| Finland), AMNI Check® | ||||||
| (MAST Diagnostica, | ||||||
| Reinfield, Germany) | ||||||
| Prolactin44,48,49 | — | > 30–50 µIU/mL | 70–95 | 76–78 | 72–84 | 75–93 |
| β-hCG43,44,50,51 | — | > 40–65 µIU/mL | 68–95 | 70–95 | 73–91 | 78–97 |
| Urea and creatinine43,52 | — | > 0.12–0.6 mg/dL | 90–100 | 87–100 | 94–100 | 91–100 |
| Lactate53 | Lac test® | ≥ 4.5 mmol/L | 79–86 | 88–92 | 88–92 | 78–87 |
| PAMG-154–57 | AmniSure® ROM test | > 5.0 ng/mL | 98–99 | 88–100 | 98–100 | 91–99 |
| (AmniSure® International | ||||||
| LLC, Cambridge, MA) |
AFP, alpha-fetoprotein; β-hCG, beta-subunit of human chorionic gonadotropin; IGFBP-1, insulinlike growth factor binding protein 1; NPV, negative predictive value; PAMG-1, placental alpha-microglobulin 1; PPV, positive predictive value.
Emerging Test for the Diagnosis of Preterm PROM
One diagnostic test that is being used increasingly often both in the United States and abroad-and which has recently been approved in the United States by the Food and Drug Administration (FDA) for the diagnosis of PROM-is the AmniSure® ROM test (AmniSure® International LLC, Cambridge, MA).54–57 This bedside immunoassay is simple, easy to perform, rapid (5–10 minutes), and minimally invasive (it does not require a speculum examination). The test identifies trace amounts of PAMG-1, a 34-kDa placental glycoprotein that is abundant in amniotic fluid (2000–25,000 ng/mL) but is present in far lower concentrations in maternal blood (5–25 ng/mL). The protein is in even lower concentrations in cervicovaginal secretions in the absence of ruptured membranes (0.05–0.2 ng/mL).54–56 This 1000- to 10,000-fold difference in concentration between amniotic fluid and cervicovaginal secretions makes PAMG-1 a very attractive marker for preterm PROM. The minimum detection threshold of the AmniSure immunoassay is 5 ng/mL, which should be sufficiently sensitive to detect preterm PROM with an accuracy of approximately 99%.55 Figure 1 briefly describes the technique for performing this test. Preliminary data from studies in Moscow and California, which included about 300 patients evaluated for preterm PROM, suggest that the test has a sensitivity of 99% and a specificity of 100%, can be used at any time in gestation (15–42 weeks), and is highly specific without interference by semen, urine, blood, or vaginal infections.54–56 In the presence of vaginal infection or nonsignificant admixture of blood, for example, levels of PAMG-1 in cervicovaginal secretions do not appear to exceed 3 ng/mL and, as such, would not be expected to interfere with the test, which has a sensitivity threshold of 5 ng/mL.55 In a more recent prospective observational study of 184 consecutive patients presenting with symptoms of PROM, Lee and colleagues57 demonstrated that the PAMG-1 immunoassay confirmed rupture of membranes at initial presentation with a sensitivity of 99%, specificity of 88%, positive predictive value of 98%, and negative predictive value of 91%. Moreover, the PAMG-1 immunoassay test was reliable across a wide gestational age range (11–42 weeks) and performed better than both the conventional combined clinical tests (pooling, nitrazine, ferning) and the nitrazine test alone in confirming the diagnosis of PROM.57 In time, such noninvasive tests may replace the need for traditional clinical assessment and amnio-dye testing for the diagnosis of PROM.55
Figure 1.

AmniSure® ROM test for the diagnosis of ruptured fetal membranes. The AmniSure ROM test (AmniSure® International LLC, Cambridge, MA) is designed to measure the presence of placental alpha microglobulin 1 (PAMG-1), which is abundant in amniotic fluid but almost absent in cervicovaginal fluid in the absence of ruptured membranes. A sample of cervicovaginal fluid is collected using a sterile swab (no speculum) and eluted into a vial containing solvent for 1 minute. The test strip is then placed in a solvent, allowing the sample in the vial to move through the membrane by capillary reaction. The pad region of the test strip has 2 zones, 1 containing anti-PAMG-1 antibodies (test zone) and the other containing anti-IgG (positive control zone). If PAMG-1 is present in the sample, it will interact with the capture antibody forming antigen-conjugate complexes that can be seen as a visible line. In the absence of antigen, no visible line will form. +ve, positive; ROM, rupture of membranes.
Management
The fetal membranes serve as a barrier to ascending infection. Once the membranes rupture, delivery is recommended when the risk of ascending infection outweighs the risk of prematurity. When PROM occurs at term, labor typically ensues spontaneously or is induced within 12 to 24 hours. The management of pregnancies complicated by preterm PROM, however, is more challenging. Although the management of such pregnancies should be individualized, a proposed management algorithm for preterm PROM is summarized in Figure 2.
Figure 2.
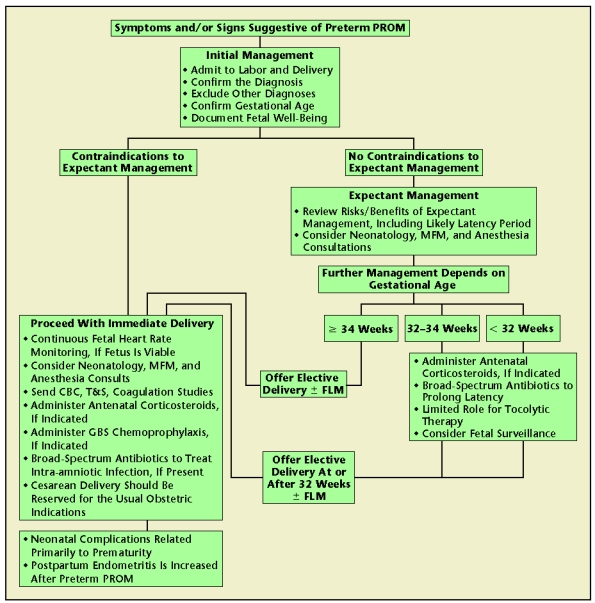
Proposed management algorithm for preterm premature rupture of membranes. CBC, complete blood count; FLM, fetal lung maturity test; GBS, group B beta-hemolytic Streptococcus; MFM, maternal-fetal medicine; PROM, premature rupture of membranes; T&S, type and screen test.
The initial management of a woman presenting with suspected preterm PROM should focus on confirming the diagnosis, validating gestational age, documenting fetal wellbeing, and deciding on the mode of delivery (which, in turn, depends on gestational age, fetal presentation, and cervical examination).1,2,61,62 Every effort should be taken to exclude contraindications to expectant management. Absolute contraindications include intra-amniotic infection (chorio-amnionitis), nonreassuring fetal testing, and active labor. The diagnosis of chorioamnionitis remains primarily a clinical one, with evidence of fetal tachycardia, maternal tachycardia, maternal fever (defined as (≥ 100.4°F), and/or uterine tenderness. Evidence of pus leaking from the cervix on sterile speculum examination can also confirm the diagnosis. Amniocentesis may be able to suggest the diagnosis (with evidence of an elevated amniotic fluid white cell count, elevated lactate dehydrogenase level, and decreased glucose concentration) or even definitely confirm the presence of intra-amniotic infection (with a positive Gram stain or amniotic fluid culture), but is not regarded as standard of care in all women presenting with preterm PROM. A favorable gestational age (defined as > 34 weeks) can also be regarded as a relative contraindication to continued expectant management in the setting of preterm PROM,2 because of the high risk of ascending infection, the low risk of complications of prematurity, and the lack of proven efficacy of antenatal corticosteroids in improving perinatal outcome.
Several areas of controversy in the management of preterm PROM still exist.
Is There a Place for Outpatient Management of Preterm PROM?
As a general rule, expectant management of pregnancies complicated by preterm PROM should be undertaken in hospital because it is not possible to accurately predict which pregnancies will develop complications such as infection, cord prolapse, umbilical cord compression, or placental abruption.2 Modified bed rest is generally recommended (in an attempt to enhance reaccumulation of amniotic fluid and to improve uteroplacental perfusion and thereby fetal growth) as is pelvic rest (no tampons, douching, or intercourse). In select circumstances (eg, compliant women who have been stable in-house for 72 hours, who live near a hospital, are able to maintain bed rest and pelvic rest at home, and who are willing to check their temperature twice daily and be seen in the office weekly), outpatient management can be considered. However, few patients fulfill all of these requirements, the approach has potential risks to both the mother and fetus, and it is not clear whether such an approach would be cost-effective.2,63
Can the Fetal Membranes Reseal?
When leakage of amniotic fluid occurs after amniocentesis, the outcome is better than after spontaneous preterm PROM. Overall, the risk of preterm PROM following second trimester genetic amniocentesis is 1.0% to 1.2%, and the procedure-related pregnancy loss rate is estimated as 0.06% to 0.2% (or 1 in 400 procedures).2,64 In most patients with preterm PROM following amniocentesis, the membranes reseal with restoration of normal amniotic fluid volume.2,65,66 This situation should be distinguished from spontaneous preterm PROM in which apparent resealing of the membranes and reaccumulation of normal amniotic fluid volume is far less common (estimated at 2.8%–13%2,30,67), especially if it has not occurred within 72 hours of presentation. If resealing of the membranes is suspected because of cessation of fluid leakage and reaccumulation of amniotic fluid on ultrasound and if the pregnancy is remote from term, an amnio-dye test is traditionally recommended to confirm this diagnosis before the patient is sent home. Newer tests such as the AmniSure ROM test may in time replace the use of amnio-dye testing in this setting.
Several techniques have been developed in an attempt to artificially reseal the fetal membranes and prevent leakage of amniotic fluid including, among others, intra-amniotic injection of platelets and cryoprecipitate (amniopatch), sealing the cervical canal, and fetoscopic laser coagulation. 68–72 However, there is as yet no effective and safe technique to achieve this goal.
Antenatal Corticosteroids
Administration of antenatal glucocorticoids (betamethasone, 12 mg IMI q 24 hourly × 2 doses or dexamethasone, 6 mg IMI q 12 hourly × 4 doses) has been shown to decrease the incidence of RDS, IVH, and necrotizing enterocolitis (NEC) by approximately 50% if given to women with intact membranes threatening to deliver prior to 34 weeks of gestation.2,73,74 Although the maximum beneficial effect is achieved 24 to 48 hours after the first dose and this effect lasts for at least 7 days, there is evidence that some clinical benefit can be achieved within 4 to 6 hours of administration. A similar beneficial effect has been confirmed in pregnancies complicated by preterm PROM prior to 32 weeks.2,73,74 However, there is insufficient evidence to demonstrate a similar beneficial response in pregnancies complicated by preterm PROM between 32 and 34 weeks of gestation.2,75 There is also no proven benefit to routine antenatal corticosteroids after 34 weeks of gestation, although some high-risk subgroups may benefit.76,77 Multiple courses of steroids are not routinely recommended because of a lack of consistent evidence showing additional benefit and because of concern about adverse effects on fetal growth and, possibly, long-term neurodevelopment. However, a repeat (salvage) dose or course should be considered if the initial course was completed prior to 28 to 32 weeks of gestation.78–80
Tocolysis
Preterm PROM is a relative contraindication to the use of tocolytic agents. Although such agents may be able to delay delivery by 24 to 28 hours, there is no convincing evidence that they can delay delivery beyond this time period and no consistent evidence that they can improve long-term perinatal morbidity or mortality.2,81–85 As such, the benefits of tocolysis in the setting of preterm PROM appear to be limited, and should be used only to allow the first course of antenatal corticosteroids to be completed and/or to transfer the patient to a tertiary care center.
Group B Beta-Hemolytic Streptococcus Chemoprophylaxis
Intrapartum-but not antepartum-Group B beta-hemolytic Streptococcus (GBS) chemoprophylaxis has been shown to significantly decrease the incidence of early-onset neonatal GBS sepsis and mortality.86,87 It is therefore indicated for all women threatening to deliver preterm, unless a negative perineal culture for GBS has been documented within the previous 5 weeks.86,87 Intravenous penicillin is the treatment of choice, and a minimum of 4 hours of antibiotics is recommended prior to delivery. A perineal and perianal (not cervical) culture for GBS should be taken from all women who present with preterm PROM with an unknown GBS carrier status.
The decision of whether to start antibiotics should be individualized depending on the likelihood that the patient will deliver within the next few days. If antibiotics are started and the decision is later taken to continue expectant management, the antibiotics can be discontinued and restarted once the patient is in labor if the GBS culture returns positive. No chemoprophylaxis is indicated if the culture returns negative, even if the delivery is preterm. If the patient subsequently develops ascending infection (chorioamnionitis), she should be treated for such with broad-spectrum intravenous antibiotics. Such protocols (which commonly include ampicillin) will adequately cover GBS. There is yet no documented GBS resistance to penicillin, although resistance to erythromycin and clindamycin may be as high as 15% to 20% in some institutions.
Prophylactic Broad-Spectrum Antibiotics to Prolong Latency
There is now substantial evidence to suggest that adjunctive prophylactic (empiric) broad-spectrum antibiotics can significantly prolong latency in the setting of preterm PROM remote from term.2,88–90 In one meta-analysis, delivery within 48 hours was reduced by 30% (relative risk [RR] 0.71; 95% confidence interval [CI], 0.58–0.87) and delivery within 7 days was reduced by 20% (RR 0.80; 95% CI, 0.71–0.90) with a concomitant increase in birth weight.90 More importantly, this approach appears to translate into an improvement in maternal and neonatal infectious morbidity with a significant reduction in chorioamnionitis (RR 0.57; 95% CI, 0.37–0.86), neonatal infection (RR 0.67; 95% CI, 0.52–0.85), and blood culture-proven neonatal sepsis (RR 0.75, 95% CI, 0.60–0.93).90 Other benefits include a reduction in oxygen requirement (RR 0.88; 95% CI, 0.81–0.96), surfactant therapy (RR 0.83; 95% CI, 0.72–0.96), RDS (RR 0.91; 95% CI, 0.83–1.00), and major cerebral abnormalities (RR 0.82; 95% CI, 0.68–0.99).90 Although there is a suggestion that overall perinatal mortality is similarly improved, not all studies have confirmed this observation.
A number of different broad-spectrum antibiotics regimens have been examined, and there is currently no evidence to recommend one regimen over another. Perhaps the most common regimen used in the United States is that from the National Institute of Child Health and Human Development (NICHD) trial, which used an initial 48 hours of intravenous therapy with ampicillin and erythromycin, followed by 5 days of oral therapy with amoxicillin and an enteric-coated erythromycin base.2,88 The use of oral amoxicillin-clavulanic acid is perhaps best avoided because of the increased risk of NEC (1.9% vs 0.5%; P = .001) documented in one study,91 although it should be noted that the NICHD trial using ampicillin and erythromycin found a decreased risk of NEC.87 Several recent studies have attempted to determine whether a shorter duration of antibiotic therapy is adequate after preterm PROM, but these are of inadequate size and power to reach any definitive recommendations. 2
Fetal Surveillance
Fetuses in pregnancies complicated by preterm PROM are at risk of ascending infection, cord accident, placental abruption, and (possibly) uteroplacental insufficiency. Although it is generally accepted that some form of fetal surveillance is necessary, there is no clear consensus about the type and frequency of this monitoring.1,2 Contraction stress testing is contraindicated in women with preterm PROM, and umbilical cord Doppler velocimetry has not been validated in this setting.2,92 Reasonable options include weekly, twice weekly, or daily non-stress testing and/or biophysical profile, but neither has been shown to be superior to fetal kick charts alone.2 Indeed, complications such as placental abruption, cord accident, and intra-amniotic infection cannot be predicted or reliably detected by such antenatal fetal testing.
Timing of Elective Delivery
Induction of labor in pregnancies complicated by preterm PROM is recommended once a favorable gestational age is reached (> 34 weeks) because of the high risk of ascending infection, the low risk of complications of prematurity, and the lack of proven efficacy of antenatal corticosteroids in improving perinatal outcome. Although most authorities regard a favorable gestational age in pregnancies complicated by preterm PROM as greater than 34 weeks,2 this definition varies from institution to institution.93 Routine induction of labor can also be safely recommended between 32 and 34 weeks’ gestation if fetal pulmonary maturity has been confirmed.94
If a Cervical Cerclage Is Present at the Time of Preterm PROM, Should It Be Removed?
The presence of a cerclage does not appear to increase the incidence of preterm PROM remote from placement. However, on occasion, preterm PROM will occur with a cerclage in place. The decision of whether or not to remove the cerclage in such patients remains controversial. Retention of the cerclage may prolong latency, thereby allowing for a more favorable gestational age at delivery. Alternatively, a retained cerclage may provide a nidus for infection. Initial studies suggested that retention of the cerclage following preterm PROM was associated with a 7-fold increase in infectious morbidity and neonatal mortality.95 However, after controlling for infection as a cause of the preterm PROM, recent studies have found no difference in perinatal outcome between cases in which the cerclage was removed or retained.96 As such, the decision of whether or not to remove the cerclage following preterm PROM should be individualized. In general, the cerclage should be removed if there is evidence of intrauterine infection, labor, unexplained vaginal bleeding, or a favorable gestational age (> 34 weeks). If not, it is reasonable to leave the cerclage in place in an attempt to prolong latency.
Conclusions
Preterm PROM is a major cause of perinatal morbidity and mortality. It is associated with 20% to 30% of all preterm births, and prognosis is related primarily to gestational age at presentation and delivery. A timely and accurate diagnosis of PROM is critical to optimize pregnancy outcome. Recent data suggest that newer noninvasive tests such as the AmniSure ROM test may replace traditional clinical tests (nitrazine, pooling, and ferning) and amnio-dye tests in the diagnosis of preterm PROM. Once the diagnosis is confirmed, management options include admission to hospital, amniocentesis to exclude intra-amniotic infection, neonatology and maternal-fetal medicine consultation, administration of antenatal corticosteroids and broad-spectrum antibiotics, if indicated, and delivery once a favorable gestation age is reached. A better understanding of the diagnosis and management of preterm PROM will allow obstetric care providers to optimize perinatal outcome and minimize neonatal morbidity.
Main Points.
Preterm premature rupture of membranes (PROM) complicates 2% to 20% of all deliveries and is associated with 18% to 20% of perinatal deaths. Management options include admission to hospital, amniocentesis to exclude intra-amniotic infection, and administration of antenatal corticosteroids and broad-spectrum antibiotics, if indicated.
The fetal membranes serve as a barrier to ascending infection. Once the membranes rupture, both the mother and fetus are at risk of infection and of other complications.
Three clinical signs of preterm PROM documented on sterile speculum examination are visual pooling of fluid in the vagina or leakage of fluid from the cervical os, an alkaline pH of cervicovaginal discharge, and/or microscoping ferning of the cervicovaginal discharge on drying.
The clinical signs of preterm PROM become progressively less accurate when more than 1 hour has elapsed after membrane rupture.
Investigators search for a test based primarily on the identification in the cervicovaginal discharge of 1 or more biochemical markers that are present with ROM, but absent in women with intact membranes.
The initial management of a woman presenting with suspected preterm PROM should focus on confirming the diagnosis, validating gestational age, documenting fetal well-being, and deciding on the mode of delivery.
Footnotes
Effective April 1, 2008, the Healthcare Common Procedure Coding System code S3628 has been assigned by Centers for Medicare & Medicaid Services to secure reimbursement for the AmniSure ROM test.
References
- 1.American College of Obstetricians and Gynecologists, authors. Premature Rupture of Membranes. Washington, DC: American College of Obstetricians and Gynecologists; 1998. (ACOG Practice Bulletin No. 1). [Google Scholar]
- 2.ACOG Committee on Practice Bulletins-Obstetrics, authors. Clinical management guidelines for obstetrician-gynecologists. (ACOG Practice Bulletin No. 80: premature rupture of membranes).Obstet Gynecol. 2007;109:1007–1019. doi: 10.1097/01.AOG.0000263888.69178.1f. [DOI] [PubMed] [Google Scholar]
- 3.Alexander JM, Cox SM. Clinical course of premature rupture of the membranes. Semin Perinatol. 1996;20:369–374. doi: 10.1016/s0146-0005(96)80003-6. [DOI] [PubMed] [Google Scholar]
- 4.Duff P. Premature rupture of the membranes in term patients. Semin Perinatol. 1996;20:401–408. doi: 10.1016/s0146-0005(96)80007-3. [DOI] [PubMed] [Google Scholar]
- 5.Ohlsson A. Treatments of preterm premature rupture of the membranes: a meta-analysis. Am J Obstet Gynecol. 1989;160:890–906. doi: 10.1016/0002-9378(89)90306-2. [DOI] [PubMed] [Google Scholar]
- 6.Mercer BM, Goldenberg RL, Meis PJ, et al. The NICHD Maternal-Fetal Medicine Units Network, authors. The Preterm Prediction Study: prediction of preterm premature rupture of membranes through clinical findings and ancillary testing. Am J Obstet Gynecol. 2000;183:738–745. doi: 10.1067/mob.2000.106766. [DOI] [PubMed] [Google Scholar]
- 7.Garite TJ. Management of premature rupture of membranes. Clin Perinatol. 2001;28:837–847. doi: 10.1016/s0095-5108(03)00081-2. [DOI] [PubMed] [Google Scholar]
- 8.Berkowitz GS, Papiernik E. Epidemiology of preterm birth. Epidemiol Rev. 1993;15:414–418. doi: 10.1093/oxfordjournals.epirev.a036128. [DOI] [PubMed] [Google Scholar]
- 9.Spinillo A, Montanari L, Sanpaolo P, et al. Fetal growth and infant neuro-developmental outcome after preterm premature rupture of membranes. Obstet Gynecol. 2004;103:1286–1293. doi: 10.1097/01.AOG.0000127706.78192.95. [DOI] [PubMed] [Google Scholar]
- 10.Parry S, Strauss JF., 3rd Preterm premature rupture of the fetal membranes. N Engl J Med. 1998;338:663–670. doi: 10.1056/NEJM199803053381006. [DOI] [PubMed] [Google Scholar]
- 11.Harger JH, Hsing AW, Tuomala RE, et al. Risk factors for preterm premature rupture of fetal membranes: a multicenter case-control study. Am J Obstet Gynecol. 1990;163:130–137. doi: 10.1016/s0002-9378(11)90686-3. [DOI] [PubMed] [Google Scholar]
- 12.Gonen R, Hannah ME, Milligan JE. Does prolonged preterm premature rupture of the membranes predispose to abruptio placentae? Obstet Gynecol. 1989;74:347–350. [PubMed] [Google Scholar]
- 13.Ananth CV, Savitz DA, Williams MA. Placental abruption and its association with hypertension and prolonged rupture of membranes: a methodologic review and meta-analysis. Obstet Gynecol. 1996;88:309–318. doi: 10.1016/0029-7844(96)00088-9. [DOI] [PubMed] [Google Scholar]
- 14.Lee T, Carpenter M, Heber WW, Silver HM. Preterm premature rupture of membranes: risks of recurrent complications in the next pregnancy among a population-based sample of gravid women. Am J Obstet Gynecol. 2003;188:209–213. doi: 10.1067/mob.2003.115. [DOI] [PubMed] [Google Scholar]
- 15.Asrat T, Lewis DF, Garite TJ, et al. Rate of recurrence of preterm premature rupture of membranes in consecutive pregnancies. Am J Obstet Gynecol. 1991;165:1111–1115. doi: 10.1016/0002-9378(91)90481-6. [DOI] [PubMed] [Google Scholar]
- 16.Guinn DA, Goldenberg RL, Hauth JC, et al. Risk factors for the development of preterm premature rupture of membranes after arrest of preterm labor. Am J Obstet Gynecol. 1995;173:1310–1315. doi: 10.1016/0002-9378(95)91377-7. [DOI] [PubMed] [Google Scholar]
- 17.Hannah ME, Ohlsson A, Farine D, et al. TERMPROM Study Group, authors. Induction of labor compared with expectant management for prelabor rupture of the membranes at term. N Engl J Med. 1996;334:1005–1010. doi: 10.1056/NEJM199604183341601. [DOI] [PubMed] [Google Scholar]
- 18.Dale PO, Tanbo T, Bendvold E, Moe N. Duration of the latency period in preterm premature rupture of the membranes. Maternal and neonatal consequences of expectant management. Eur J Obstet Gynecol Reprod Biol. 1989;30:257–262. doi: 10.1016/0028-2243(89)90010-5. [DOI] [PubMed] [Google Scholar]
- 19.Bengtson JM, Van Marter, Barss VA, et al. Pregnancy outcome after premature rupture of membranes at or before 26 weeks’ gestation. Obstet Gynecol. 1989;73:921–927. doi: 10.1097/00006250-198906000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Hadi HA, Hodson CA, Strickland D. Premature rupture of the membranes between 20 and 25 weeks’ gestation: role of amniotic fluid volume in perinatal outcome. Am J Obstet Gynecol. 1994;170:1139–1144. doi: 10.1016/s0002-9378(94)70109-1. [DOI] [PubMed] [Google Scholar]
- 21.Park JS, Yoon BH, Romero R, et al. The relationship between oligohydramnios and the onset of preterm labor in preterm premature rupture of membranes. Am J Obstet Gynecol. 2001;184:459–462. doi: 10.1067/mob.2001.109398. [DOI] [PubMed] [Google Scholar]
- 22.Buhimschi CS, Buhimschi IA, Norwitz ER, et al. Sonographic myometrial thickness predicts the latency interval of women with preterm premature rupture of the membranes and oligohydramnios. Am J Obstet Gynecol. 2005;193:762–770. doi: 10.1016/j.ajog.2005.01.053. [DOI] [PubMed] [Google Scholar]
- 23.Bianco AT, Stone J, Lapinski R, et al. The clinical outcome of preterm premature rupture of membranes in twin versus singleton pregnancies. Am J Perinatol. 1996;13:135–138. doi: 10.1055/s-2007-994310. [DOI] [PubMed] [Google Scholar]
- 24.Myles TD, Espinoza R, Meyer W, Bieniarz A. Preterm premature rupture of membranes: comparison between twin and singleton gestations. J Matern Fetal Med. 1997;6:159–163. doi: 10.1002/(SICI)1520-6661(199705/06)6:3<159::AID-MFM8>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 25.Hallak M, Bottoms S. Accelerated pulmonary maturation from preterm premature rupture of membranes: a myth. Am J Obstet Gynecol. 1993;169:1045–1049. doi: 10.1016/0002-9378(93)90051-j. [DOI] [PubMed] [Google Scholar]
- 26.Amin AF, Mohammed MS, Sayed GH, Abdel-Razik S. Prophylactic transcervical amnioinfusion in laboring women with oligohydramnios. Int J Gynaecol Obstet. 2003;81:183–189. doi: 10.1016/s0020-7292(03)00041-9. [DOI] [PubMed] [Google Scholar]
- 27.Yoon BH, Romero R, Park JS, et al. Fetal exposure to an intra-amniotic inflammation and the development of cerebral palsy at the age of three years. Am J Obstet Gynecol. 2000;182:675–681. doi: 10.1067/mob.2000.104207. [DOI] [PubMed] [Google Scholar]
- 28.Spinillo A, Capuzzo E, Stronati M, et al. Effect of preterm premature rupture of membranes on neurodevelopmental outcome: follow up at two years of age. Br J Obstet Gynaecol. 1995;102:882–887. doi: 10.1111/j.1471-0528.1995.tb10875.x. [DOI] [PubMed] [Google Scholar]
- 29.Mercer BM, Arheart KL. Antimicrobial therapy in expectant management of preterm premature rupture of membranes. Lancet. 1995;346:1271–1279. doi: 10.1016/s0140-6736(95)91868-x. [DOI] [PubMed] [Google Scholar]
- 30.Mercer BM. Management of premature rupture of the membranes before 26 weeks’ gestation. Obstet Gynecol Clin North Am. 1992;19:339–351. [PubMed] [Google Scholar]
- 31.Gorodeski IG, Haimovitz L, Bahari CM. Reevaluation of the pH, ferning and Nile blue sulphate staining methods in pregnant women with premature rupture of the fetal membranes. J Perinat Med. 1982;10:286–292. doi: 10.1515/jpme.1982.10.6.286. [DOI] [PubMed] [Google Scholar]
- 32.Friedman ML, McElin TW. Diagnosis of ruptured fetal membranes. Am J Obstet Gynecol. 1969;104:544–550. doi: 10.1016/s0002-9378(16)34244-2. [DOI] [PubMed] [Google Scholar]
- 33.de Haan HH, Offermans PM, Smits F, et al. Value of the fern test to confirm or reject the diagnosis of ruptured membranes in modest in nonlaboring women presenting with nonspecific vaginal fluid loss. Am J Perinatol. 1994;11:46–50. doi: 10.1055/s-2007-994535. [DOI] [PubMed] [Google Scholar]
- 34.Gaucherand P, Salle B, Sergeant P, et al. Comparative study of three vaginal markers of the premature rupture of membranes. Insulin like growth factor binding protein, 1 diamineoxidase, and pH. Acta Obstet Gynecol Scand. 1997;76:536–540. doi: 10.3109/00016349709024579. [DOI] [PubMed] [Google Scholar]
- 35.Erdemoglu E, Mungan T. Significance of detecting insulin-like growth factor binding protein-1 in cervicovaginal secretions: comparison with nitrazine test and amniotic fluid volume assessment. Acta Obstet Gynecol Scand. 2004;83:622–626. doi: 10.1111/j.0001-6349.2004.00343.x. [DOI] [PubMed] [Google Scholar]
- 36.Reece EA, Chervenak FA, Moya FR, Hobbins JC. Amniotic fluid arborization: effect of blood, meconium, and pH alterations. Obstet Gynecol. 1984;64:248–250. [PubMed] [Google Scholar]
- 37.Rosemond RL, Lombardi SJ, Boehm FH. Ferning of amniotic fluid contaminated with blood. Obstet Gynecol. 1990;75:338–340. [PubMed] [Google Scholar]
- 38.Smith RP. A technique for the detection of rupture of the membranes: a review and preliminary report. Obstet Gynecol. 1976;48:172–176. [PubMed] [Google Scholar]
- 39.Hannah ME, Hodnett ED, Willan A, et al. The Term PROM Study Group, authors. Prelabor rupture of the membranes at term: expectant management at home or in hospital? Obstet Gynecol. 2000;96:533–538. doi: 10.1016/s0029-7844(00)00971-6. [DOI] [PubMed] [Google Scholar]
- 40.Healy AJ, Veille JC, Sciscione A, et al. The timing of elective delivery in preterm premature rupture of the membranes: a survey of members of the Society of Maternal-Fetal Medicine. Am J Obstet Gynecol. 2004;190:1479–1481. doi: 10.1016/j.ajog.2004.02.036. [DOI] [PubMed] [Google Scholar]
- 41.Spahr RC, Salsburey DJ, Krissberg A, Prin W. Intraamniotic injection of methylene blue leading to methemoglobinemia in one of twins. Int J Gynaecol Obstet. 1980;17:477–478. doi: 10.1002/j.1879-3479.1980.tb00192.x. [DOI] [PubMed] [Google Scholar]
- 42.Kishida T, Yamada H, Negishi H, et al. Diagnosis of premature rupture of the membranes in preterm patients, using an improved AFP kit: comparison with ROM-check and/or Nitrazine test. Eur J Obstet Gynecol Reprod Biol. 1996;69:77–82. doi: 10.1016/0301-2115(95)02519-7. [DOI] [PubMed] [Google Scholar]
- 43.Li HY, Chang TS. Vaginal fluid creatinine, human chorionic gonadotropin and alpha-fetoprotein levels for detecting premature rupture of membranes. Zhonghua Yi Xue Za Zhi (Taipei) 2000;63:686–690. [PubMed] [Google Scholar]
- 44.Shahin M, Raslan H. Comparative study of three amniotic fluid markers in premature rupture of membranes: prolactin, beta subunit of human chorionic gonadotropin, and alpha-fetoprotein. Gynecol Obstet Invest. 2006;63:195–199. doi: 10.1159/000097844. [DOI] [PubMed] [Google Scholar]
- 45.Lockwood CJ, Senyei AE, Dische MR, et al. Fetal fibronectin in cervical and vaginal secretions defines a patient population at high risk for preterm delivery. N Engl J Med. 1991;325:669–674. doi: 10.1056/NEJM199109053251001. [DOI] [PubMed] [Google Scholar]
- 46.Jeurgens-Borst AJ, Bekkers RL, Sporken JM, van der Berg PP. Use of insulin like growth factor binding protein-1 in the diagnosis of ruptured fetal membranes. Eur J Obstet Gynecol Reprod Biol. 2002;102:11–14. doi: 10.1016/s0301-2115(01)00560-7. [DOI] [PubMed] [Google Scholar]
- 47.Lockwood CJ, Wein R, Chien D, et al. Fetal membrane rupture is associated with the presence of insulin-like growth factor-binding protein-1 in vaginal secretions. Am J Obstet Gynecol. 1994;171:146–150. doi: 10.1016/0002-9378(94)90461-8. [DOI] [PubMed] [Google Scholar]
- 48.Buyukbayrak EE, Turan C, Unal O, et al. Diagnostic power of the vaginal washing-fluid prolactin assay as an alternative method for the diagnosis of premature rupture of membranes. J Matern Fetal Neonatal Med. 2004;15:120–125. doi: 10.1080/14767050410001659842. [DOI] [PubMed] [Google Scholar]
- 49.Koninckx PR, Trappeniers H, van Assche FA. Prolactin concentration in vaginal fluid: a new method for diagnosing ruptured membranes. Br J Obstet Gynaecol. 1981;88:607–610. doi: 10.1111/j.1471-0528.1981.tb01216.x. [DOI] [PubMed] [Google Scholar]
- 50.Esim E, Turan C, Unal O, et al. Diagnosis of premature rupture of membranes by identification of beta-hCG in vaginal washing fluid. J Obstet Gynecol Reprod Biol. 2003;107:37–40. doi: 10.1016/s0301-2115(02)00277-4. [DOI] [PubMed] [Google Scholar]
- 51.Kim YH, Park YW, Kwon HS, et al. Vaginal fluid beta-human chorionic gonadotropin level in the diagnosis of premature rupture of membranes. Acta Obstet Gynecol Scand. 2005;84:802–805. doi: 10.1111/j.0001-6349.2005.00712.x. [DOI] [PubMed] [Google Scholar]
- 52.Kafali H, Oksuzler C. Vaginal fluid urea and creatinine in diagnosis of premature rupture of membranes. Arch Gynecol Obstet. 2007;275:157–160. doi: 10.1007/s00404-006-0240-1. [DOI] [PubMed] [Google Scholar]
- 53.Wiberg-Itzel E, Cnattingius S, Nordstrom L. Lactate determination in vaginal fluids: a new method in the diagnosis of prelabour rupture of membranes. Br J Obstet Gynaecol. 2005;112:754–758. doi: 10.1111/j.1471-0528.2004.00521.x. [DOI] [PubMed] [Google Scholar]
- 54.Petrunin DD. Immunochemical identification of organ specific human placental alphaglobulin and its concentration in amniotic fluid. Akush Ginekol. 1977;1:64–65. [PubMed] [Google Scholar]
- 55.Cousins LM, Smok DP, Lovett SM, Poeltler DM. Amnisure placental alpha macroglobulin-1 rapid immunoassay versus standard diagnostic methods for detection of rupture of membranes. Am J Perinatol. 2005;22:317–320. doi: 10.1055/s-2005-870896. [DOI] [PubMed] [Google Scholar]
- 56.Boltovskaia MN, Zaraiskii EI, Fuks BB, et al. Histochemical and clinical-diagnostic study of placental alpha 1-microglobulin using monoclonal antibodies. Bull Eksp Biol Med. 1991;112:397–400. [PubMed] [Google Scholar]
- 57.Lee SE, Park JS, Norwitz ER, et al. Measurement of placental alpha-microglobulin-1 in cervicovaginal discharge to diagnose rupture of membranes. Obstet Gynecol. 2007;109:634–640. doi: 10.1097/01.AOG.0000252706.46734.0a. [DOI] [PubMed] [Google Scholar]
- 58.Gravett MG, Thomas A, Schneider KA, et al. Proteomic analysis of cervical-vaginal fluid: identification of novel biomarkers for detection of intra-amniotic infection. J Proteome Res. 2007;6:89–96. doi: 10.1021/pr060149v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pepeira L, Lapidus J, Lu XF, et al. Comprehensive proteomic analysis of human cervical-vaginal fluid and identification of novel biomarkers for prediction of spontaneous preterm birth [abstract 4]. Presented at: 27th Annual Clinical Meeting of the Society for Maternal-Fetal Medicine; February 5–10, 2007; San Francisco, CA. [Google Scholar]
- 60.Leite RS, Brown AG, Parry S. Proteomic profiling detects calgranulin B in cervicovaginal fluid from women who deliver preterm [abstract 296]. Presented at: 54th Annual Meeting of the Society for Gynecologic Investigation; March 14–17, 2007; Reno, NV. [Google Scholar]
- 61.Mercer BM. Preterm premature rupture of the membranes: current approaches to evaluation and management. Obstet Gynecol Clin North Am. 2005;32:411–428. doi: 10.1016/j.ogc.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 62.Di Renzo GC, Roura LC the European Association of Perinatal Medicine-Study Group on Preterm Birth, authors. Guidelines for the management of spontaneous preterm labor. J Perinat Med. 2006;34:359–366. doi: 10.1515/JPM.2006.073. [DOI] [PubMed] [Google Scholar]
- 63.Carlan SJ, O’Brien WF, Parsons MT, Lense JJ. Preterm premature rupture of membranes: a randomized study of home versus hospital management. Obstet Gynecol. 1993;81:61–64. [PubMed] [Google Scholar]
- 64.Eddleman KA, Malone FD, Sullivan L, et al. Pregnancy loss rates after midtrimester amniocentesis. Obstet Gynecol. 2006;108:1067–1072. doi: 10.1097/01.AOG.0000240135.13594.07. [DOI] [PubMed] [Google Scholar]
- 65.Gold RB, Goyert GL, Schwartz DB, et al. Conservative management of second-trimester postamniocentesis fluid leakage. Obstet Gynecol. 1989;74:745–747. [PubMed] [Google Scholar]
- 66.Borgida AF, Mills AA, Feldman DM, et al. Outcome of pregnancies complicated by ruptured membranes after genetic amniocentesis. Am J Obstet Gynecol. 2000;183:937–939. doi: 10.1067/mob.2000.108872. [DOI] [PubMed] [Google Scholar]
- 67.Johnson JW, Egerman RS, Moorhead J. Cases with ruptured membranes that “reseal.”. Am J Obstet Gynecol. 1990;163:1024–1030. doi: 10.1016/0002-9378(90)91117-u. [DOI] [PubMed] [Google Scholar]
- 68.Sciscione AC, Manley JS, Pollock M, et al. Intracervical fibrin sealants: a potential treatment for early preterm premature rupture of the membranes. Am J Obstet Gynecol. 2001;184:368–373. doi: 10.1067/mob.2001.111796. [DOI] [PubMed] [Google Scholar]
- 69.Reddy UM, Shah SS, Nemiroff RL, et al. In vitro sealing of punctured fetal membranes: potential treatment for midtrimester premature rupture of membranes. Am J Obstet Gynecol. 2001;185:1090–1093. doi: 10.1067/mob.2001.117685. [DOI] [PubMed] [Google Scholar]
- 70.Lewi L, Van Schoubroeck D, Van Ranst M, et al. Successful patching of iatrogenic rupture of the fetal membranes. Placenta. 2004;25:352–356. doi: 10.1016/j.placenta.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 71.Quintero RA, Morales WJ, Allen M, et al. Treatment of iatrogenic previable premature rupture of membranes with intra-amniotic injection of platelets and cryoprecipitate (amniopatch): preliminary experience. Am J Obstet Gynecol. 1999;181:744–749. doi: 10.1016/s0002-9378(99)70522-3. [DOI] [PubMed] [Google Scholar]
- 72.Locatelli A, Andreani M, Ghidini A, et al. Amnioinfusion in preterm PROM: effects on amnion and cord histology. J Perinatol. 2008;28:97–101. doi: 10.1038/sj.jp.7211876. [DOI] [PubMed] [Google Scholar]
- 73.The effect of antenatal steroids for fetal maturation on perinatal outcomes-interim draft statement. NIH Consens Statement Online. 1994 Feb–Mar;12(2):1–24. [PubMed] [Google Scholar]
- 74.Crowley P. Prophylactic corticosteroids for preterm birth. Cochrane Database Syst Rev. 2000;2 doi: 10.1002/14651858.CD000065. CD000065. [DOI] [PubMed] [Google Scholar]
- 75.Rand L, Soto E, Norwitz ER, et al. The efficacy of antenatal corticosteroids between 32 and 34 weeks in patients with preterm premature rupture of membranes [abstract 343]. Presented at: 53rd Annual Meeting of the Society for Gynecologic Investigation; March 22–25, 2006; Toronto, Ontario, Canada. [Google Scholar]
- 76.Stutchfield P, Whitaker R, Russell I, et al. Antenatal Steroids for Term Elective Caesarean Section (ASTECS) Research Team, authors. Antenatal betamethasone and incidence of neonatal respiratory distress after elective caesarean section: pragmatic randomised trial. BMJ. 2005;331:645–646. doi: 10.1136/bmj.38547.416493.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Peranteau WH, Wilson RD, Liechty KW, et al. Effect of maternal betamethasone administration on prenatal congenital cystic adenomatoid malformation growth and fetal survival. Fetal Diagn Ther. 2007;22:365–371. doi: 10.1159/000103298. [DOI] [PubMed] [Google Scholar]
- 78.Wapner RJ, Sorokin Y, Thom EA, et al. National Institute of Child Health and Human Development Maternal Fetal Medicine Units Network. Single versus weekly courses of antenatal corticosteroids: evaluation of safety and efficacy. Am J Obstet Gynecol. 2006;195:633–642. doi: 10.1016/j.ajog.2006.03.087. [DOI] [PubMed] [Google Scholar]
- 79.Crowther CA, Haslam RR, Hiller JE, et al. Australasian Collaborative Trial of Repeat Doses of Steroids (ACTORDS) Study Group, authors. Neonatal respiratory distress syndrome after repeat exposure to antenatal corticosteroids: a randomised controlled trial. Lancet. 2006;367:1913–1919. doi: 10.1016/S0140-6736(06)68846-6. [DOI] [PubMed] [Google Scholar]
- 80.Bonanno C, Fuchs K, Wapner RJ. Single versus repeat courses of antenatal steroids to improve neonatal outcomes: risks and benefits. Obstet Gynecol Surv. 2007;62:261–271. doi: 10.1097/01.ogx.0000259226.62431.78. [DOI] [PubMed] [Google Scholar]
- 81.Garite TJ, Keegan KA, Freeman RK, Nageotte MP. A randomized trial of ritodrine tocolysis versus expectant management in patients with premature rupture of membranes at 25 to 30 weeks of gestation. Am J Obstet Gynecol. 1987;157:388–393. doi: 10.1016/s0002-9378(87)80179-5. [DOI] [PubMed] [Google Scholar]
- 82.Norwitz ER, Robinson JN, Challis JRG. The control of labor. N Engl J Med. 1999;341:660–666. doi: 10.1056/NEJM199908263410906. [DOI] [PubMed] [Google Scholar]
- 83.Mercer BM. Is there a role for tocolytic therapy during conservative management of preterm premature rupture of the membranes? Clin Obstet Gynecol. 2007;50:487–496. doi: 10.1097/GRF.0b013e31804c977d. [DOI] [PubMed] [Google Scholar]
- 84.Coombs CA, McCune M, Clark R, Fishman A. Aggressive tocolysis does not prolong pregnancy or reduce neonatal morbidity after preterm premature rupture of the membranes. Am J Obstet Gynecol. 2004;190:1723–1728. doi: 10.1016/j.ajog.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 85.Wolfensberger A, Zimmermann R, von Mandach U. Neonatal mortality and morbidity after aggressive long-term tocolysis for preterm premature rupture of the membranes. Fetal Diagn Ther. 2006;21:366–373. doi: 10.1159/000092467. [DOI] [PubMed] [Google Scholar]
- 86.Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A. Prevention of perinatal group B streptococcal disease. MMWR Recomm Rep. 2002;51:1–22. Revised guidelines from CDC. [PubMed] [Google Scholar]
- 87.American College of Obstetricians and Gynecologists, authors. Prevention of early-onset group B streptococcal disease in newborns. (ACOG Committee Opinion: number 279, December 2002).Obstet Gynecol. 2002;100:1405–1412. doi: 10.1016/s0029-7844(02)02629-7. [DOI] [PubMed] [Google Scholar]
- 88.Mercer BM, Miodovnik M, Thurnau GR, et al. the National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network, authors. Antibiotic therapy for reduction of infant morbidity after preterm premature rupture of the membranes. A randomized controlled trial. JAMA. 1997;278:989–995. [PubMed] [Google Scholar]
- 89.Kenyon SL, Taylor DJ, Tarnow-Mordi W the ORACLE Collaborative Group, authors. Broad-spectrum antibiotics for preterm, prelabor rupture of fetal membranes: the ORACLE I randomized trial. Lancet. 2001;357:979–988. doi: 10.1016/s0140-6736(00)04233-1. [DOI] [PubMed] [Google Scholar]
- 90.Kenyon S, Boulvain M, Neilson J. Antibiotics for preterm rupture of the membranes: a systematic review. Obstet Gynecol. 2004;104:1051–1057. doi: 10.1097/01.AOG.0000143268.36682.21. [DOI] [PubMed] [Google Scholar]
- 91.Kenyon S, Boulvain M, Neilson J. Antibiotics for preterm rupture of membranes. Cochrane Database Syst Rev. 2003;2 doi: 10.1002/14651858.CD001058. CD001058. [DOI] [PubMed] [Google Scholar]
- 92.Clinical management guidelines for obstetriciangynecologists. (ACOG practice bulletin).Int J Gynaecol Obstet. 2000;68:175–185. Antepartum fetal surveillance. Number 9, October 1999 (replaces Technical Bulletin Number 188, January 1994) [PubMed] [Google Scholar]
- 93.Cox SM, Leveno KJ. Intentional delivery versus expectant management with preterm ruptured membranes at 30–34 weeks’ gestation. Obstet Gynecol. 1995;86:875–879. doi: 10.1016/0029-7844(95)00303-9. [DOI] [PubMed] [Google Scholar]
- 94.Mercer BM, Crocker LG, Boe NM, Sibai BM. Induction versus expectant management in premature rupture of the membranes with mature amniotic fluid at 32–36 weeks: a randomized trial. Am J Obstet Gynecol. 1993;169:775–782. doi: 10.1016/0002-9378(93)90004-3. [DOI] [PubMed] [Google Scholar]
- 95.Ludmir J, Bader T, Chen L, et al. Poor perinatal outcome associated with retained cerclage in patients with premature rupture of membranes. Obstet Gynecol. 1994;84:823–826. [PubMed] [Google Scholar]
- 96.McElrath TF, Norwitz ER, Lieberman ES, Heffner LJ. Management of cervical cerclage and preterm premature rupture of the membranes: should the stitch be removed? Am J Obstet Gynecol. 2000;183:840–846. doi: 10.1067/mob.2000.108870. [DOI] [PubMed] [Google Scholar]


