Abstract
Objective
Using prospective data, we tested the hypothesis that early depressed mood was associated with an increased risk for initiation of alcohol use. In addition, we examined whether these associations varied according to the youths' report that alcohol consumption occurred with or without parental permission.
Methods
The participants for these analyses were students, ages 9 to 13 years old, participating in a longitudinal study in an urban sample of public schools (n=2311). As part of the prospective annual assessments of the students, in 1990 through 1994, data on depressive mood and alcohol use were gathered. Logistic regression models were used to assess the association between the level of baseline depressed mood in 1990 and initiation of alcohol use between 1991 through 1994 in the sample of youth at risk for new onset drinking (n=1526). Other characteristics assessed in the analyses included age, sex, race-ethnicity, alcohol use by peers, neighborhood environment, and receipt of subsidized lunch.
Results
Higher level of early depressed mood was associated with an earlier and increased estimated risk of initiating alcohol use without parental permission for boys but not for girls. Depressed mood was not associated with alcohol use initiation that occurred with parental sanctions.
Conclusions
Findings from the current study support the hypothesis that among urban youth, early depressed mood influences the initiation of alcohol consumption without parental permission for boys.
Keywords: alcohol, adolescence, depression, mood, risk
1. Introduction
In cross-national surveys among adults, alcohol and depressive disorders have been reported to co-occur (Alonso et al., 2004; Andrade et al., 2002; Burns and Teesson, 2002; Helzer and Pryzbeck, 1988; Kessler et al., 1997; Grant and Harford, 1995). In addition, some prospective analyses involving adults show an association of increased risk for alcohol outcomes such as heavy drinking and alcohol dependence among individuals who are depressed (Aalto-Setälä et al, 2002; Clark et al, 2003; Dixit and Crum, 2000; Gilman and Abraham, 2001). These relationships may be particularly important among women (Gilman and Abraham, 2001; Dixit and Crum, 2000). For example, in a three-wave panel study of New York household residents, Moscato and colleagues (1997) found that depressive symptoms predicted alcohol problems for women, but not for men. In a meta-analysis of eight longitudinal studies with follow-up intervals up to 10 years, Hartka et al (1991) found that over the short term, depression tended to decrease alcohol use for both males and females; yet over the long term, depression predicted alcohol consumption only among women. Wang and Patten (2001) found that depression increased risk for heavy drinking episodes only for females.
Less information is available concerning these conditions among adolescents. Some cross-sectional school-based studies have provided evidence that associations exist between depressive symptoms and drinking behavior (e.g., Kelder et al, 2001; Rohde et al, 1996). For example, Kelder and colleagues (2001) surveyed minority middle school students and found that the strength of association for substance use, including binge drinking, increased with higher quintile of depressive symptomatology. Studies of clinical samples of adolescents also provide evidence that depressive and alcohol use disorders co-occur (Danielson et al, 2003; Deykin et al, 1992), and in longitudinal analyses depression may be associated with higher risk of subsequent problem drinking such as earlier alcohol relapse among those with treated alcohol use disorders (Cornelius et al, 2004). Yet, there is a paucity of prospective analyses which have examined the relationship of depressive symptoms with earlier drinking behavior, such as the initiation of alcohol consumption. In one such study, Kaplow et al (2001) examined a predominantly rural population, with a relatively large proportion of Native American children, and found that some dimensions of early anxiety symptoms were associated with the subsequent increased risk for the initiation of alcohol during adolescence. In that same study, early depressive symptoms were also found to be associated with higher risk for drinking onset. However, the investigators acknowledged the limited generalizability to other race and ethnic groups.
Etiologic theories to account for the comorbid relationship between depressive symptoms as a predictor of alcohol involvement often focus on the use of alcohol as a method of self-medicating, self-regulating or coping with an underlying mood disturbance. Social learning theory (Bandura, 1977) might explain the role that alcohol expectancies, coping skills, and self-efficacy play in regulation of alcohol consumption and the development of maladaptive drinking patterns (e.g., Evans and Dunn, 1995; Maisto et al, 2000; Christiansen et al, 1985). This is reinforced by evidence that tension-reduction motives are positively associated with heavy drinking (Rutledge and Sher, 2001), and alcohol expectancies and specific coping strategies are associated with consumption levels (Evans and Dunn, 1995; Read and O'Connor, 2006; Cooper et al, 1988). For example, Holahan et al (2003) found that drinking to cope among depressed individuals increased risk for both level of consumption and development of alcohol-related problems in a 10-year follow-up period. Furthermore, expectancies for negative mood regulation may increase risk for problem drinking (Kassel et al, 2000). In addition, there also may be common underlying factors which predispose to an increased risk for both alcohol and depressive conditions. These may include genetic factors as well as social or environmental characteristics (Fu et al, 2002; Chassin et al, 1999; Kendler et al, 1993; Dohrenwend et al, 1992; Clark et al, 2003).
In the current report, we aimed to extend prior findings from prospective assessments of youth to examine early depressed mood among a sample of urban predominantly African American adolescents. We hypothesized that higher level of depressed mood would be associated with greater risk for the initiation of alcohol use without permission. Because of prior evidence of gender and racial differences among population-based as well as clinical samples of adults (Gilman and Abraham, 2001; Moscato et al, 1997; Hartka et al, 1991; Wang and Patten, 2001; King et al, 2003; Maag and Irvin, 2005), we also examined these associations separately by sex as well as race-ethnicity. In addition, there is limited information regarding whether parental permission involving alcohol use is an important factor effecting this potential association. If mood symptoms increase risk for starting to drink alcohol, we hypothesized a priori that this would most likely occur without parental permission. Our goal was to assess this type of drinking behavior separately from alcohol use that parents may have condoned (for example allowing sips of wine at the dinner table). We also felt that drinking which had not been sanctioned by parents would be more likely to represent early deviance. Prior studies have indicated that drinking without parental permission may be an important alcohol use outcome (Bush and Iannotti, 1992), may increase risk for other behavioral disturbances (e.g., Johnson et al, 1995), and may be a specific target for alcohol initiation intervention programs (Spoth et al, 1999). Consequently, we examined the possible role of parental permission by assessing the association of depressed mood and alcohol use initiation with and without parental permission.
2. Methods
2.1. Study population and sample for the current analyses
Data are from a prospective study conducted within the context of a group randomized prevention trial targeting early learning and aggression during two successive school years in 1985−86 when 2311 students entered the first grade classrooms of 19 elementary schools in an urban mid-Atlantic region of the United States (1985: cohort I, n=1196; 1986: cohort II, n=1115). Further details and additional information on the intervention study and subsequent prospective data collection are available elsewhere (Kellam et al, 1991; Kellam and Anthony, 1998). Students remaining in the public school system between 1989 and 1994 were interviewed annually. Parental consent was obtained for the majority of eligible youth; only 5% of the original cohort recruited in 1985−86 declined to participate. Child assent was obtained at the time of the interview, and a Certificate of Confidentiality was used to increase protection for study participants. The face-to-face interviews were administered in private locations at each school by one member in a team of trained interviewers. The interviewers were all young male and female adults from predominately minority racial-ethnic backgrounds, similar to the ethnic composition of the student participants.
Of the original sample of 2311, a total of 785 youth were excluded because they either did not have a childhood interview subsequent to 1990 (n=526), or because they had indicated an age of onset of alcohol use without parental permission to be before their age of the baseline depressed mood assessment (n=259) and therefore were no longer at risk for new onset alcohol use initiation. The 1990 interview is considered the baseline for the current report because this was the first year that this specific information on depressed mood was gathered. The sample for the current analyses is comprised of the 1526 study participants that were at risk for first time alcohol use without parental permission at the time of the 1990 interview. Of this baseline sample, 97.0% were re-interviewed in 1991 (96.0% cohort I, 98.0% cohort II), 89.6% in 1992 (89.8% cohort I, 89.5% cohort II), 79.1% in 1993 (80.3% cohort I, 77.9% cohort II). In 1994, it was decided to focus limited resources on following up youth in cohort II so that they would be followed to a similar mean age as the first cohort (69.0% cohort II, 34.9% cohort). The handling of missing information in the data analyses is described below. The study participants who were excluded or missing from our sample when compared with those at risk for initiation of alcohol use without permission were more likely to be White (χ2=233.2, (degrees of freedom (df))=1, p<0.001) and were also more likely to have paid for lunches in first grade as opposed to having received free or reduced cost lunches (χ2=125.1, (df)=2, p<0.001).
2.2. Measures
Information on alcohol use was based on responses to the question asked each year regarding whether the student had “ever drunk beer, wine, wine coolers, or any other drink with alcohol in it, even just a sip or taste”. Starting in 1990, a separate item inquired about the age first drank alcohol without parental permission. Study participants who reported alcohol use without permission for the first time at an age greater than their age in the 1990 interview during at least one subsequent interview between 1991 and 1994 were considered incident cases of alcohol use without permission. For these analyses, the reference group included participants who had not yet used alcohol, as well as those who may have used alcohol but only with parental permission. We felt that this was a more conservative approach to the analyses and would be more generalizable than simply using as the reference only those who had never used alcohol in any setting. Our rationale is also based on the concept that those students that eventually drink with and without permission are likely to start first by drinking with permission. Approximately half of the incident cases that began drinking without permission had already indicated alcohol use with permission prior to 1990, while for the other half of the incident cases without permission, alcohol use began after the 1990 interview. We assessed separately the association of depressed mood with alcohol use initiation among individuals who reported that alcohol use occurred only with parental permission. For those analyses, our reference group was comprised of those study participants who had reported no alcohol use.
Depressed mood was assessed from questions that asked about having “been in a bad mood”, “felt sad”, “felt crabby or cranky” and “felt like crying” “all the time or almost all of the time”. Item probes queried whether each specific feeling had ever occurred “every day or almost every day” for two weeks, or for the prior two weeks if the symptoms were current. Youth were considered to have depressed mood if the specific feeling was reported as having occurred daily or almost daily for a period of two weeks or more, similar to prior analyses completed with this dataset (Wu and Anthony, 1999; Chen et al, 1999). A “high” level of depressed mood was defined if there was the report of either 1) three or more different depressive feelings at any time, or 2) at least two depressive feelings that were described as being current (within the prior two weeks), as well as having occurred for at least two weeks in the past. A “low” depressed mood level was defined if a student reported either 1) having one depressive feeling that had occurred at any time, or 2) having two depressive feelings that only occurred once (current or in the past but not both). “High” and “low” level depressed mood classifications were both referenced to students without depressive feelings at any time. Our rationale for the high and low categories was to distinguish those with many symptoms or evidence for chronicity in the “high” level group, with those individuals in the “low” level group with only one depressive feeling and little evidence for persistence of symptoms. We hypothesized that those with the greater burden of negative affect as evidenced by the larger number of depressive feelings and recurrence or persistence of these feelings would be at highest risk for onset of drinking. This measure of depressed mood has been found to have adequate internal consistency (Cronbach α=0.69), and to have strong predictive validity, in that the high level of depressive symptoms as measured in the 1990 interview, was found to be strongly associated with major depressive disorder as assessed by the Composite International Diagnostic Interview (CIDI) (WHO, 1989), completed during the 1993−94 interview: relative to those without depressed mood, Odds ratio (OR)= 3.17 (95% confidence interval (CI)=1.68, 5.95; p=<0.001), and OR=1.64 (95% CI=0.89, 3.01; p=0.11) for CIDI-defined major depressive disorder among those with high and low levels of depressive symptoms, respectively.
Additional covariates included in these analyses were age, sex, race-ethnicity (African-American, all other racial groups), and the student's report of peer alcohol use. We assessed neighborhood environment using an 18-item scale, which was adapted and modified from one initially developed for use in the National Youth Survey by Elliott and colleagues (Elliott et al, 1989). This scale is a self-report measure of neighborhood characteristics which includes specific items that address concepts such as church and religious involvement in the neighborhood, as well as whether neighbors take care of each other, as compared to those that damage or steal property (Elliott et al, 1989; Crum et al, 1996). The scale items were scored so that a higher score indicated a greater degree of neighborhood disadvantage. We also included a variable indicating the report of having subsidized lunch in first grade because this characteristic was differentially related to attrition in the sample.
2.3. Data analysis
After exploratory data analyses, we completed initial and multiple logistic regression analyses to assess the strength of the association between depressed mood level (measured at the 1990 interview) with risk for the subsequent initiation of alcohol use without parental permission (assessed at the 1991 through 1994 interviews). In addition, separate analyses to assess potential effect modification by sex and race were completed by stratifying the sample and repeating the logistic regression models separately for girls and boys, and African-Americans and the group comprised of other race-ethnicities (96% white) consistent with our a priori hypotheses. As an alternative method of assessing effect modification, we also provide findings from the analyses when interaction terms for depression levels with sex, and depression levels with race-ethnicity were included in the multivariable models. Separate analyses also addressed whether the association of depressed mood with alcohol use onset differed for those study participants who drank alcohol only with parental permission.
Potential confounding by other characteristics was constrained in these analyses via statistical adjustment. These covariates included the dichotomous variable for whether the student reported peer alcohol use (yes=1, no=0), age at baseline (included as a continuous variable) and neighborhood disadvantage (included as tertiles of score, as previously accomplished (Crum et al, 1996)). The information for these additional covariates was gathered at the time of the 1990 interview. These specific covariates were included in the model because prior analyses of this dataset have shown that these characteristics may influence the occurrence of alcohol use or problem drinking among adolescents (e.g., Crum et al, 1996, 2005; Chen et al, 1999). Because study participants may not have been interviewed each year due to school absences at the time of the annual interview, there is a proportion of students for whom follow-up alcohol use information is available, but not information on baseline characteristics. In addition, some missing information is also due to attrition, for example when study participants moved out of the urban area. In order to take into account these various occurrences of missing information, and to keep the representativeness of the original sample intact, we created categories for missing information for each of the specific characteristics where this occurred in order to stabilize the number of participants contributing information to the multiple regression analyses. Furthermore, a variant of the Huber-White sandwich estimator of variance was used to obtain robust standard errors and variance estimates in all the logistic regression analyses to accommodate the initial sample design of clustering of students within schools (STATA, 2000). Finally, we included in the multiple regression models a variable indicating the intervention status of the participants to hold constant this additional study design characteristic.
3. Results
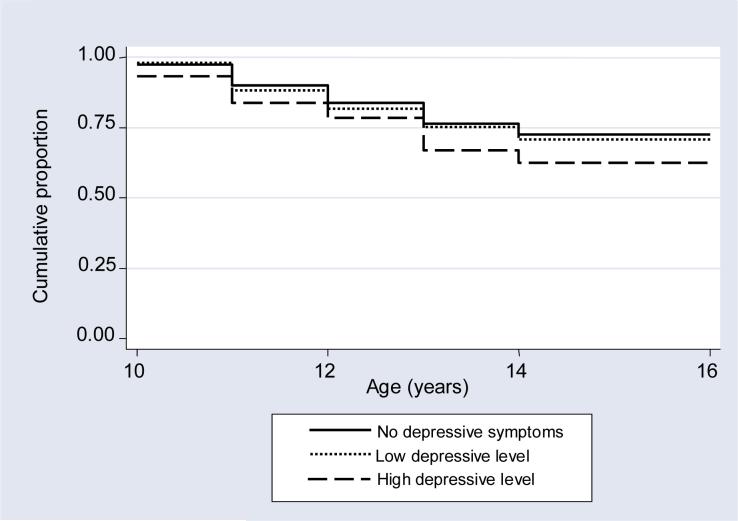
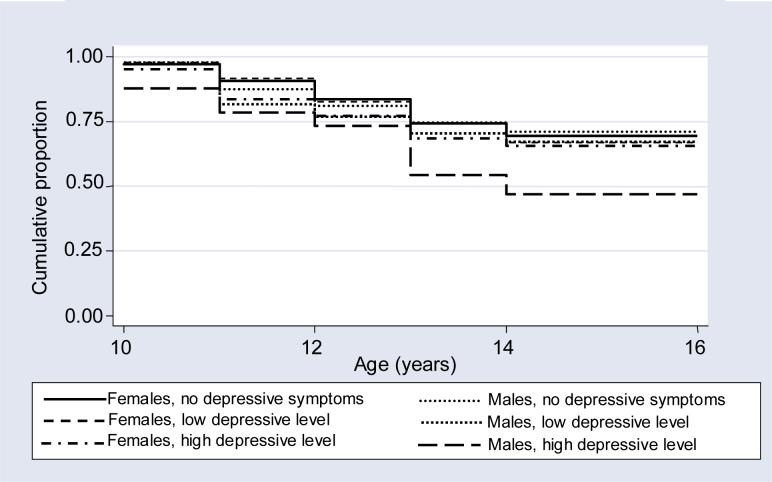
Between 1991 and 1994, a total of 477 of the 1526 study participants were identified as incident cases of new onset alcohol use without parental permission. Table 1 presents the frequency distribution of characteristics by incident alcohol use without permission during the four year follow-up interval. The only characteristic associated with new initiation of alcohol without permission in these initial analyses was depressed mood. When the frequency distributions were stratified by sex and race-ethnicity (Table 2), we also found that males and African Americans with depressed moods were more likely to be among the incident cases. Furthermore, Kaplan-Meier survival estimates for the overall sample indicated that with higher levels of depressed mood there was an earlier onset of alcohol use without parental permission (log-rank test for equality of survivor functions χ2=11.45, (df)=2, p=0.003) (Figure 1). When we completed Kaplan-Meier survival estimates by sex as well as depressed mood level, we found that boys with the highest level of depressed mood started drinking earlier than any other subgroup (log-rank test for equality of survivor functions, χ2=17.92, (df)=5, p=0.003) (Figure 2).
Table 1.
Frequency distribution of baseline characteristics in the 1990 interview by incident use of alcohol without parental permission assessed during follow-up between 1991 through 1994.
| Baseline characteristics | Incident Use of Alcohol without Parental Permission | ||||||
|---|---|---|---|---|---|---|---|
| Total (%) | No (%) | Yes (%) | χ2 (df), p-value1 | ||||
| 1526 | 1049 | (68.7) | 477 | (31.3) | |||
| Sex: Female | 785 | (51.4) | 550 | (52.4) | 235 | (49.3) | 1.31 (1), 0.25 |
| Male | 741 | (48.6) | 499 | (47.6) | 242 | (50.7) | |
| Race-ethnicity | 0.86 (1), 0.35 | ||||||
| African American | 1165 | (76.3) | 808 | (77.0) | 357 | (74.8) | |
| Non-African American2 | 361 | (23.7) | 241 | (23.0) | 120 | (25.2) | |
| Age (years): 9 | 460 | (30.1) | 327 | (31.2) | 133 | (27.9) | 1.70 (4), 0.79 |
| 10 | 700 | (45.9) | 475 | (45.3) | 225 | (47.2) | |
| 11 | 335 | (22.0) | 226 | (21.5) | 109 | (22.8) | |
| 12 | 28 | (1.8) | 19 | (1.8) | 9 | (1.9) | |
| 13 | 3 | (0.2) | 2 | (0.2) | 1 | (0.2) | |
| Peer alcohol use: Present | 915 | (60.0) | 640 | (61.0) | 275 | (57.6) | 1.83 (2), 0.40 |
| Absent | 194 | (12.7) | 127 | (12.1) | 67 | (14.0) | |
| missing | 417 | (27.3) | 282 | (26.9) | 135 | (28.3) | |
| Neighborhood disadvantage3 | 4.40 (3), 0.22 | ||||||
| Low | 383 | (25.1) | 277 | (26.4) | 106 | (22.2) | |
| Moderate | 365 | (23.9) | 250 | (23.8) | 115 | (24.1) | |
| High | 344 | (22.5) | 224 | (21.4) | 120 | (25.2) | |
| missing | 434 | (28.4) | 298 | (28.4) | 136 | (28.5) | |
| Subsidized lunch4 | 2.20 (2), 0.33 | ||||||
| Yes | 928 | (60.8) | 638 | (60.8) | 290 | (60.8) | |
| No | 597 | (39.1) | 411 | (39.2) | 186 | (39.0) | |
| missing | 1 | (0.1) | 0 | (0.0) | 1 | (0.2) | |
| Depressed mood level: | 9.89 (3), 0.02 | ||||||
| None | 638 | (41.2) | 457 | (43.6) | 181 | (38.0) | |
| Low | 290 | (19.0) | 201 | (19.2) | 89 | (18.7) | |
| High | 180 | (11.8) | 107 | (10.2) | 73 | (15.3) | |
| missing | 418 | (27.4) | 284 | (27.1) | 134 | (28.1) | |
χ2 (df), chi-square test value, degrees of freedom, p-value.
A total of 96% of the non African American group are White, 4% are Asian, American Indian or Hispanic.
The neighborhood scale items were scored so that a higher score indicated a greater degree of neighborhood disadvantage (Elliott et al, 1989; Crum et al, 1996). Score tertiles were used in these analyses.
Indicates report of receiving subsidized lunch during first grade in 1985−1986.
Table 2.
Frequency distribution by sex and race-ethnicity for baseline depressive symptom level with incident use of alcohol without parental permission.
| Depressed mood level | Incident Use of Alcohol without Parental Permission | ||||||
|---|---|---|---|---|---|---|---|
| Total (%) | No (%) | Yes (%) | χ2 (df), p-value1 | ||||
| 1526 | 1049 | (68.7) | 477 | (31.3) | |||
| Females | |||||||
| None | 332 | (42.3) | 236 | (42.9) | 96 | (40.8) | 0.75 (3), 0.86 |
| Low | 146 | (18.6) | 102 | (18.6) | 44 | (18.7) | |
| High | 105 | (13.4) | 70 | (12.7) | 35 | (14.9) | |
| missing | 202 | (25.7) | 142 | (25.8) | 60 | (25.5) | |
| Males | |||||||
| None | 306 | (41.3) | 221 | (44.3) | 85 | (35.1) | 14.76 (3), 0.002 |
| Low | 144 | (19.4) | 99 | (19.8) | 45 | (18.6) | |
| High | 75 | (10.1) | 37 | (7.4) | 38 | (15.7) | |
| missing | 216 | (29.2) | 142 | (28.5) | 74 | (30.6) | |
| African Americans | |||||||
| None | 483 | (41.5) | 353 | (43.7) | 130 | (36.4) | 9.69 (3), 0.02 |
| Low | 236 | (20.3) | 164 | (20.3) | 72 | (20.2) | |
| High | 147 | (12.6) | 88 | (10.9) | 59 | (16.5) | |
| missing | 299 | (25.7) | 203 | (25.1) | 96 | (26.9) | |
| Non-African Americans2 | |||||||
| None | 155 | (42.9) | 104 | (43.2) | 51 | (42.5) | 1.43 (3), 0.70 |
| Low | 54 | (15.0) | 37 | (15.4) | 17 | (14.2) | |
| High | 33 | (9.1) | 19 | (7.9) | 14 | (11.7) | |
| missing | 119 | (33.0) | 81 | (33.6) | 38 | (31.7) | |
χ2 (df), chi-square test value, degrees of freedom, p-value.
A total of 96% of the non African American group are White, 4% are Asian, American Indian or Hispanic.
Figure 1.
Kaplan-Meier survival estimates for the cumulative proportion that have not initiated alcohol use without permission by depressed mood level1.
Figure 2.
Kaplan-Meier survival estimates for the cumulative proportion that have not initiated alcohol use without permission by sex and depressed mood level1.
In the initial logistic regression model for the overall sample, we found that the low depressed mood level was not associated with an increased estimated risk for new onset alcohol use without parental permission (Table 3). However, the high depressed mood level group was associated with a higher risk for alcohol use initiation. The strength of the association was similar when the model was adjusted for potential confounding by age, sex, race, peer alcohol use, neighborhood disadvantage, and receipt of subsidized lunch. The logistic regression models were repeated stratifying by sex and race-ethnicity. Male, but not female youth with high depressed mood were associated with greater risk for beginning to drink alcohol without permission (OR=2.40, 95% CI=1.20, 4.79, p=0.01 for males; OR=1.20, 95% CI=0.74, 1.93, p=0.46 for females). The model for African American youth also initially indicated that those with the higher depressed mood level were associated with greater risk for alcohol use initiation without parental permission (OR=1.82, 95% CI=1.01, 3.27, p=0.04). Yet, the strength of the association was attenuated in the adjusted model (OR=1.73, 95% CI=0.96, 3.13), p=0.07). No association with alcohol use initiation was found for the classification that included all other racial groups (OR=1.35, 95% CI=0.77, 2.35, p=0.30). As an alternative method for assessing effect modification, interaction terms were included in the multiple regression models. In those analyses, the OR=2.3 (95% CI=1.04, 5.08, p=0.04) for males with the higher depressive symptom level relative to females without depression (data not shown). Using this methodology, we found no evidence for interaction by race-ethnicity.
Table 3.
Odds ratios for the association of depressive symptom level with incident use of alcohol without parental permission based on initial and multiple logistic regression models.
| Depressed mood level |
Incident Alcohol Use without Parental Permission |
|
|---|---|---|
| Crude OR (95% CI), p-value1 |
Adjusted OR (95% CI), p-value2 |
|
| Overall sample | ||
| None | 1.0 | 1.0 |
| Low | 1.18 (0.78, 1.61), 0.55 | 1.08 (0.75, 1.57), 0.62 |
| High |
1.72 (1.06, 2.79), 0.03 |
1.62 (1.00, 2.61), 0.05 |
| Females | ||
| None | 1.0 | 1.0 |
| Low | 1.06 (0.65, 1.72), 0.81 | 1.05 (0.65, 1.70), 0.84 |
| High |
1.23 (0.78, 1.94), 0.38 |
1.20 (0.74, 1.93), 0.46 |
| Males | ||
| None | 1.0 | 1.0 |
| Low | 1.18 (0.79, 1.77), 0.42 | 1.14 (0.75, 1.71), 0.54 |
| High |
2.67 (1.36, 5.23), 0.004 |
2.40 (1.20, 4.79), 0.01 |
| African Americans | ||
| None | 1.0 | 1.0 |
| Low | 1.19 (0.82, 1.74), 0.36 | 1.14 (0.77, 1.71), 0.50 |
| High |
1.82 (1.01, 3.27), 0.04 |
1.73 (0.96, 3.13), 0.07 |
| Non-African Americans3 | ||
| None | 1.0 | 1.0 |
| Low | 0.94 (0.46, 1.93), 0.86 | 0.90 (0.45, 1.79), 0.76 |
| High | 1.50 (0.95, 2.36), 0.08 | 1.35 (0.77, 2.35), 0.30 |
OR, 95% CI, odds ratio, 95% confidence interval.
The multiple logistic regression analyses were completed holding constant age, sex (for the overall and race stratified models), race-ethnicity (for the overall and sex stratified models), peer alcohol use, neighborhood disadvantage, report of receiving subsidized lunch, and intervention status. We also included categories that contained participants with missing data (specifically for depressed mood, peer alcohol use and neighborhood disadvantage).
A total of 96% of the non African American group are White, 4% are Asian, American Indian or Hispanic.
As stipulated previously, we examined whether depressed mood level with risk for alcohol use initiation was related to whether or not the alcohol consumption occurred with parental permission. As a consequence, we assessed the associations for individuals who indicated that alcohol use initiation only occurred with parental permission referenced to those students who reported no alcohol use. In these initial and adjusted logistic regression models (Table 4), depressed mood was not associated with alcohol initiation when the drinking occurred with parental permission.
Table 4.
Odds ratios for the association of depressive symptom level with incident use of alcohol only with parental permission based on initial and multiple logistic regression models.
|
Incident Alcohol Use Only with Parental Permission |
||
|---|---|---|
| |
Crude OR (95% CI), p-value1 |
Adjusted OR (95% CI), p-value1,2 |
| Depressed mood level | ||
| None | 1.0 | 1.0 |
| Low | 1.21 (0.91, 1.61), 0.19 | 1.21 (0.89, 1.65), 0.23 |
| High | 0.88 (0.58, 1.33), 0.55 | 0.93 (0.62, 1.39), 0.73 |
OR, 95% CI, odds ratio, 95% confidence interval.
The multiple logistic regression analyses were completed holding constant age, sex (for the race stratified models), race-ethnicity (for the sex stratified models), peer alcohol use, neighborhood disadvantage, report of receiving subsidized lunch, and intervention status. We also included categories that contained participants with missing data (specifically for depressed mood, peer alcohol use and neighborhood disadvantage).
4. Discussion
Consistent with our hypotheses, a higher level of depressed mood was associated with risk for alcohol use initiation without parental permission. In addition, specific stratified analyses indicated important relationships by sex, and possibly by race. Only among boys did we find an association of high depressed mood level with the onset of drinking. No appreciable association was found for girls. Although initially there appeared to be an association among African Americans with depressed mood and drinking onset, the strength of the association was attenuated once potential confounding characteristics were held constant in the multiple logistic regression models.
Although cross-sectional survey data (Alonso et al., 2004; Andrade et al., 2002; Burns and Teesson, 2002; Helzer and Pryzbeck, 1988; Kessler et al., 1997; Grant and Harford, 1995), and analyses involving clinical samples of adults and adolescents (Cornelius et al, 2004; Greenfield et al, 1998; Pettinati et al, 1997; Brown et al, 1998; Thase et al., 2001; Danielson et al, 2003; Deykin et al, 1992) have reported associations of depressive disorders or other assessments of mood symptoms with alcohol outcomes, few studies have examined the relationship prospectively among urban youth. There is a paucity of information regarding the association of depressive symptoms with the onset of drinking. Kaplow and colleagues have examined anxiety symptoms with alcohol use initiation, and in that study also reported that depressive symptoms increased risk for alcohol use initiation in their sample of predominantly rural youth (Kaplow et al, 2001). This current report extends these findings to an urban youth population. Drinking to cope with negative affect (Carpenter and Hasin, 1999; Hussong et al, 2005; Kaplan et al., 1982) and to cope with distress among patients with clinical depression (Holahan et al, 2003) have been shown to relate to drinking behavior and occurrence of alcohol dependence and may account for some of the findings here. Expectancies for negative mood regulation among some samples may predict problem drinking (Kassel et al, 2000). However, to what degree children have expectations for regulation of depressive symptoms and to what extent this might alter drinking behavior has not been adequately assessed. Furthermore, internalizing symptoms such as anxiety and depression may act as mediators in the relationship between life events, trauma or perceived stress (Hussong and Chassin, 1994) and alcohol consumption. Because prior work has not shown varying patterns by sex for other emotional symptoms such as anxiety with drinking onset (Kaplow et al, 2001), it is possible that the negative affect typical of depressive conditions predicts particular vulnerability for drinking onset. Other genetic and environmental characteristics may have important influences on this relationship. They might include parental drinking, as well as familial history of affective or alcohol use disorders (Conway et al, 2003; Warner et al, 2007; Tambs et al, 1997). Although we attempted to hold constant some environmental characteristics which might potentially confound this association such as peer use and neighborhood disadvantage (Chuang et al, 2005; Duncan et al, 2002; Chen et al, 1999; Kuntsche and Jordon, 2006; Hill et al, 1994), there are also likely to be many other familial, cultural, religious and school-based influences which predict as well as reduce the risk of early drinking initiation during adolescence (Ennett et al, 1997; Fite et al, 2006; Nash et al, 2005; Mason and Windle, 2001; Curran et al, 1997; Duncan et al, 1994).
Prior research has shown that expectations of alcohol's effects change with development, with some investigators reporting a growth in positive alcohol expectancies with age (Schell et al, 2005; Gustafson, 1992; Miller et al, 1990). An additional explanation for our findings is that mood symptoms interact with the development of alcohol expectancies or with the cognitive perceptions of drinking effects to alter drinking behavior. Alcohol expectancies have an important role in predicting both drinking patterns during adolescence as well as the development of alcohol use disorders in adulthood (Brown et al, 1987; Christiansen et al, 1989; Callas et al, 2004; Cable and Sacker, 2007; Simons-Morton et al, 1999). In addition, coping styles, the presence of stress and positive expectancies may predict drinking patterns, including the use of alcohol as a method of coping among adults (Cooper et al, 1992; Evans and Dunn, 1995) and adolescents (Laurent et al, 1997). The impact of alcohol expectations also may differ by sex (Griffin et al, 2000). Furthermore, some delinquent behaviors associated with consumption may be mediated by alcohol expectancies (Barnow et al, 2004). Because the presence of externalizing behaviors such as conduct and attention deficit disorders also relates to drinking patterns and deviance (Molina et al, 2002; Button et al, 2007; Brown et al, 1996), and also effects the relationships between expectancies and maladaptive drinking (Finn et al, 2005; Greenbaum et al, 1995), the incorporation of these additional conditions will be important to assess in future analyses.
Our results indicate important differences by sex. In some of the prior literature, stronger comorbid associations have been reported among females. However, these associations were often with depressive disorders which are more prevalent among women (Kessler et al, 1993; Eaton et al, 1997). In our study the prevalence of these early mood symptoms at baseline did not significantly differ by sex (see Table 2). In addition, when we examined the overall age of alcohol use onset without permission for boys and girls separately, we found no differences (mean age (SD)=11.58 years (0.084) for girls, 11.47 years (0.087) for boys (two-sample t test with equal variance=0.95, p=0.34)). Yet the presence of depressed mood appears to predict an earlier and stronger drinking onset for boys as opposed to girls. There are a number of possible explanations for these associations which will need to be explored further in future investigations. For example, boys may be more likely to express or cope with early depressive symptoms with behavioral disturbances, which might include initiation into earlier drinking onset.
It is possible that girls with these early mood symptoms manifest greater subsequent risk for the development of depressive disorders, whereas boys may be at greater risk for maladaptive alcohol involvement and alcohol dependence. These sex differences in possible manifestations of early mood symptoms (as with other forms of stress or adversity) have been discussed by other investigators (e.g., Klein and Corwin, 2002; Dohrenwend and Dohrenwend, 1976; Young and Ribeiro, 2006; Young, 1998). Future studies may explore these possible explanations by evaluating specific transition patterns for boys and girls with similar levels of early mood symptoms, by examining differential risk for multiple conditions simultaneously including psychopathologic, behavioral and substance use outcomes, and by assessing important potential mediators in these relationships which may include biologic factors.
In our analyses, depressed mood level was associated with new onset drinking without permission by parents. We did not find any association of depressed mood with drinking onset when the alcohol consumption occurred with parental permission. This implies that these early mood symptoms are predicting a type of deviant drinking for which boys may be particularly vulnerable. These findings may also help elucidate specific etiologic mechanisms for these associations. For example, we would not necessarily expect that if drinking as a method for coping with or regulating negative affect is the sole explanation for these findings that the associations of depressed mood level with drinking onset would differ by parental permission. How these patterns relate to other types of internalizing symptoms such as anxiety, externalizing symptoms such as conduct disorder and aggression, and whether there are associations with other deviant behaviors including other substance use will be important pathways to elucidate in future studies.
Several limitations in the current report should be mentioned. First, as discussed above, several characteristics which may be potential confounders were not included in these analyses because the information was not available, such as familial history of alcohol and depressive disorders (Conway et al, 2003; Warner et al, 2007; Tambs et al, 1997; Hill et al, 1994). These conditions would be expected to influence both the development of mood symptoms in childhood, as well the possible early use of alcohol due to genetic vulnerabilities and influences from the familial environment on modeling behavior, provision of support, and parental monitoring (Nash et al, 2005; Mason and Windle, 2001; Duncan et al, 1994; Ary et al, 1993). Yet, a number of important predictors were examined in this current report, and adjustment by these characteristics did not significantly alter the associations found. Second, our assessment of depressed mood did not include a structured psychiatric interview and so cannot be used as diagnostic of a depressive or affective disorder in these youth. However, as discussed in the Methods section, this measure of childhood depressed mood has adequate internal consistency and was found to be associated with CIDI-defined major depression in subsequent interviews of this sample, providing evidence of predictive validity. Third, the co-occurrence and effect of other psychiatric conditions such as externalizing behaviors including attention deficit hyperactivity and conduct disorders were not assessed in these analyses. Fourth, in our analyses, we did not require that depressive symptoms be temporally comorbid with alcohol use initiation. This is because we felt that risk for alcohol use initiation may occur among those with a history of depressive symptoms whether or not these symptoms are concurrent with the onset of drinking. The relationship of mood symptoms that predate and also persist, so that they are concurrent with subsequent alcohol use will need to be explored in future analyses. Fifth, conclusions regarding generalizability of these findings from our inner-city sample of school youth cannot be made without further assessments and replication of findings within other populations. However, our study does confirm some prior findings reported from a predominantly rural population with a different racial distribution (Kaplow et al, 2001).
Notwithstanding these possible limitations, the study findings may help to elucidate early predictors of alcohol use initiation in childhood and early adolescence. Because early use of alcohol has been shown to be a strong predictor of subsequent risk for the development of alcohol use disorders in adulthood (DeWit et al., 2000; Grant and Dawson, 1997; Grant et al, 2001), the identification of these early predictors may have important implications for reducing the incidence and prevalence of alcohol abuse and dependence. Future investigations will need to explore possible pathways for these associations with particular emphasis on mediating and moderating influences of other emotional symptoms such as anxiety, and co-occurring use of other substances, such as marijuana and tobacco.
Acknowledgments
The analyses for this work were supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (AA014869). Data gathering for the study was completed by grants DA04392 and DA09897, and a career development award K05DA015799 (JCA) from the National Institute on Drug Abuse.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Log-rank test for equality of survivor functions, χ2=11.45, (df)=2, p=0.003.
Log-rank test for equality of survivor functions, χ2=17.92, (df)=5, p=0.003.
References
- Aalto-Setala T, Marttunen M, Tuulio-Henriksson A, Poikolainen K, Lonnqvist J. Depressive symptoms in adolescence as predictors of early adulthood depressive disorders and maladjustment. Am J Psychiatry. 2002;159:1235–1237. doi: 10.1176/appi.ajp.159.7.1235. [DOI] [PubMed] [Google Scholar]
- Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, Girolamo G, Graaf R, Demyttenaere K, Gasquet I, Haro JM, Katz SJ, Kessler RC, Kovess V, Lepine JP, Ormel J, Polidori G, Russo LJ, Vilagut G, Almansa J, Arbabzadeh-Bouchez S, Autonell J, Bernal M, Buist-Bouwman MA, Codony M, Domingo-Salvany A, Ferrer M, Joo SS, Martinez-Alonso M, Matschinger H, Mazzi F, Morgan Z, Morosini P, Palacin C, Romera B, Taub N, Vollebergh WA, ESEMeD/MHEDEA 2000 Investigators, European Study of the Epidemiology of Mental Disorders (ESEMeD) Project 12-Month comorbidity patterns and associated factors in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;(420):28–37. doi: 10.1111/j.1600-0047.2004.00328.x. [DOI] [PubMed] [Google Scholar]
- Andrade L, Walters EE, Gentil V, Laurenti R. Prevalence of ICD-10 mental disorders in a catchment area in the city of Sao Paulo, Brazil. Soc Psychiatry Psychiatr Epidemiol. 2002;37:316–325. doi: 10.1007/s00127-002-0551-x. [DOI] [PubMed] [Google Scholar]
- Ary DV, Tildesley E, Hops H, Andrews J. The influence of parent, sibling, and peer modeling and attitudes on adolescent use of alcohol. Int J Addict. 1993;28:853–880. doi: 10.3109/10826089309039661. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social learning theory. Prentice Hall; Englewood Cliffs, N.J.: 1977. [Google Scholar]
- Barnow S, Schultz G, Lucht M, Ulrich I, Preuss UW, Freyberger HJ. Do alcohol expectancies and peer delinquency/substance use mediate the relationship between impulsivity and drinking behaviour in adolescence? Alcohol Alcoholism. 2004;39:213–219. doi: 10.1093/alcalc/agh048. [DOI] [PubMed] [Google Scholar]
- Brown SA, Christiansen BA, Goldman MS. The alcohol expectancy questionnaire: an instrument for the assessment of adolescent and adult alcohol expectancies. J Stud Alcohol. 1987;48:483–491. doi: 10.15288/jsa.1987.48.483. [DOI] [PubMed] [Google Scholar]
- Brown SA, Gleghorn A, Schuckit MA, Myers MG, Mott MA. Conduct disorder among adolescent alcohol and drug abusers. J Stud Alcohol. 1996;57(3):314–324. doi: 10.15288/jsa.1996.57.314. [DOI] [PubMed] [Google Scholar]
- Brown RA, Monti PM, Myers MG, Martin RA, Rivinus T, Dubreuil ME, Rohsenow DJ. Depression among cocaine abusers in treatment: relation to cocaine and alcohol use and treatment outcome. Am J Psychiatry. 1998;155(2):220–225. doi: 10.1176/ajp.155.2.220. [DOI] [PubMed] [Google Scholar]
- Burns L, Teesson M. Alcohol use disorders comorbid with anxiety, depression and drug use disorders. Findings from the Australian National Survey of Mental Health and Well Being. Drug Alcohol Depend. 2002;68:299–307. doi: 10.1016/s0376-8716(02)00220-x. [DOI] [PubMed] [Google Scholar]
- Bush PJ, Iannotti RJ. Elementary schoolchildren's use of alcohol, cigarettes and marijuana and classmates' attribution of socialization. Drug Alcohol Depend. 1992;30:275–287. doi: 10.1016/0376-8716(92)90062-h. [DOI] [PubMed] [Google Scholar]
- Button TM, Rhee SH, Hewitt JK, Young SE, Corley RP, Stallings MC. The role of conduct disorder in explaining the comorbidity between alcohol and illicit drug dependence in adolescence. Drug Alcohol Depend. 2007;87(1):46–53. doi: 10.1016/j.drugalcdep.2006.07.012. [DOI] [PubMed] [Google Scholar]
- Cable N, Sacker A. The role of adolescent social disinhibition expectancies in moderating the relationship between psychological distress and alcohol use and misuse. Addict Behav. 2007;32:282–295. doi: 10.1016/j.addbeh.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Callas PW, Flynn BS, Worden JK. Potentially modifiable psychosocial factors associated with alcohol use during early adolescence. Addict Behav. 2004;29:1503–1515. doi: 10.1016/j.addbeh.2004.02.028. [DOI] [PubMed] [Google Scholar]
- Carpenter KM, Hasin DS. Drinking to cope with negative affect and DSM-IV alcohol use disorders: a test of three alternative explanations. J Stud Alcohol. 1999;60(5):694–704. doi: 10.15288/jsa.1999.60.694. [DOI] [PubMed] [Google Scholar]
- Chassin L, Pitts SC, DeLucia C, Todd M. A longitudinal study of children of alcoholics: predicting young adult substance use disorders, anxiety, and depression. J Abnorm Psychol. 1999;108:106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- Chen LS, Anthony JC, Crum RM. Perceived cognitive competence, depressive symptoms and the incidence of alcohol-related problems in urban school children. Journal of Child & Adolescent Substance Abuse. 1999;8(4):37–53. [Google Scholar]
- Christiansen BA, Goldman MS, Brown SA. The differential development of adolescent alcohol expectancies may predict adult alcoholism. Addict Behav. 1985;10:299–306. doi: 10.1016/0306-4603(85)90011-5. [DOI] [PubMed] [Google Scholar]
- Christiansen BA, Smith GT, Roehling PV, Goldman MS. Using alcohol expectancies to predict adolescent drinking behavior after one year. J Consult Clin Psychol. 1989;57:93–99. doi: 10.1037//0022-006x.57.1.93. [DOI] [PubMed] [Google Scholar]
- Chuang YC, Ennett ST, Bauman KE, Foshee VA. Neighborhood influences on adolescent cigarette and alcohol use: mediating effects through parent and peer behaviors. J Health Soc Behav. 2005;46:187–204. doi: 10.1177/002214650504600205. [DOI] [PubMed] [Google Scholar]
- Clark D,B, De Bellis MD, Lynch KG, Cornelius JR, Martin CS. Physical and sexual abuse, depression and alcohol use disorders in adolescents: onsets and outcomes. Drug Alcohol Depend. 2003;69:51–60. doi: 10.1016/s0376-8716(02)00254-5. [DOI] [PubMed] [Google Scholar]
- Conway KP, Swendsen JD, Merikangas KR. Alcohol expectancies, alcohol consumption, and problem drinking: the moderating role of family history. Addict Behav. 2003;28:823–836. doi: 10.1016/s0306-4603(02)00265-4. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, George WH. Coping, expectancies, and alcohol abuse: A test of social learning formulations. Psychol. 1988;97:218–230. doi: 10.1037//0021-843x.97.2.218. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: moderating effects of gender, coping, and alcohol expectancies. J Abnorm Psychol. 1992;101:139–152. doi: 10.1037//0021-843x.101.1.139. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Maisto SA, Martin CS, Bukstein OG, Salloum IM, Daley DC, Wood DS, Clark DB. Major depression associated with earlier alcohol relapse in treated teens with AUD. Addict Behav. 2004;29:1035–1038. doi: 10.1016/j.addbeh.2004.02.056. [DOI] [PubMed] [Google Scholar]
- Crum RM, Lillie-Blanton M, Anthony JC. Neighborhood environment and opportunity to use cocaine and other drugs in late childhood and early adolescence. Drug Alcohol Depend. 1996;43:155–161. doi: 10.1016/s0376-8716(96)01298-7. [DOI] [PubMed] [Google Scholar]
- Crum RM, Storr C, Anthony JC. Are educational aspirations associated with the risk of alcohol use and alcohol-related problems among adolescents? Substance Use and Misuse. 2005;40(2):151–169. doi: 10.1081/ja-200047558. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Stice E, Chassin L. The relation between adolescent alcohol use and peer alcohol use: a longitudinal random coefficients model. J Consult Clin Psychol. 1997;65:130–140. doi: 10.1037//0022-006x.65.1.130. [DOI] [PubMed] [Google Scholar]
- Danielson CK, Overholser JC, Butt ZA. Association of substance abuse and depression among adolescent psychiatric inpatients. Can J Psychiatry. 2003;48:762–765. doi: 10.1177/070674370304801109. [DOI] [PubMed] [Google Scholar]
- DeWit DJ, Adlaf EM, Offord DR, Ogborne AC. Age at first alcohol use: a risk factor for the development of alcohol disorders. Am J Psychiatry. 2000;157:745–750. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- Deykin EY, Buka SL, Zeena TH. Depressive illness among chemically dependent adolescents. Am J Psychiatry. 1992;149:1341–1347. doi: 10.1176/ajp.149.10.1341. [DOI] [PubMed] [Google Scholar]
- Dixit AR, Crum RM. Prospective study of depression and the risk of heavy alcohol use in women. Am J Psychiatry. 2000;157:751–758. doi: 10.1176/appi.ajp.157.5.751. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Dohrenwend BS. Sex differences and psychiatric disorders. Am J Sociol. 1976;81(6):1447–1454. doi: 10.1086/226229. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Levav I, Shrout PE, Schwartz S, Naveh G, Link BG, Skodol AE, Stueve A. Socioeconomic status and psychiatric disorders: The causation-selection issue. Science. 1992;255:946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- Duncan SC, Duncan TE, Strycker LA. A multilevel analysis of neighborhood context and youth alcohol and drug problems. Prev Sci. 2002;3:125–133. doi: 10.1023/a:1015483317310. [DOI] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, Hops H. The effects of family cohesiveness and peer encouragement on the development of adolescent alcohol use: a cohort-sequential approach to the analysis of longitudinal data. J Stud Alcohol. 1994;55:588–599. doi: 10.15288/jsa.1994.55.588. [DOI] [PubMed] [Google Scholar]
- Eaton WW, Anthony JC, Gallo J, Cai G, Tien A, Romanoski A, Lyketsos C, Chen LS. Natural history of Diagnostic Interview Schedule/DSM-IV major depression. The Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry. 1997;54(11):993–999. doi: 10.1001/archpsyc.1997.01830230023003. [DOI] [PubMed] [Google Scholar]
- Elliott DS, Huizinga D, Menard S. Multiple Problem Youth: Delinquency, Substance Use, and Mental Health Problems. Springer Verlag; New York: 1989. [Google Scholar]
- Ennett ST, Flewelling RL, Lindrooth RC, Norton EC. School and neighborhood characteristics associated with school rates of alcohol, cigarette, and marijuana use. J Health Soc Behav. 1997;38:55–71. [PubMed] [Google Scholar]
- Evans DM, Dunn NJ. Alcohol expectancies, coping responses and self-efficacy judgments: a replication and extension of Copper et al.'s 1988 study in a college sample. J Stud Alcohol. 1995;56(2):186–193. doi: 10.15288/jsa.1995.56.186. [DOI] [PubMed] [Google Scholar]
- Finn PR, Bobova L, Wehner E, Fargo S, Rickert ME. Alcohol expectancies, conduct disorder and early-onset alcoholism: negative alcohol expectancies are associated with less drinking in non-impulsive versus impulsive subjects. Addiction. 2005;100(7):953–962. doi: 10.1111/j.1360-0443.2005.01105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fite PJ, Colder CR, O'Connor RM. Childhood behavior problems and peer selection and socialization: risk for adolescent alcohol use. Addict Behav. 2006;31:1454–1459. doi: 10.1016/j.addbeh.2005.09.015. [DOI] [PubMed] [Google Scholar]
- Fu Q, Health AC, Bucholz KK, Nelson E, Goldberg J, Lyons MJ, True WR, Jacob T, Tsuang MT, Eisen SA. Shared genetic risk of major depression, alcohol dependence, and marijuana dependence: contribution of antisocial personality disorder in men. Arch Gen Psychiatry. 2002;59:1125–1132. doi: 10.1001/archpsyc.59.12.1125. [DOI] [PubMed] [Google Scholar]
- Gilman SE, Abraham HD. A longitudinal study of the order of onset of alcohol dependence and major depression. Drug Alcohol Depend. 2001;63:277–286. doi: 10.1016/s0376-8716(00)00216-7. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC. Comorbidity between DSM-IV alcohol use disorders and major depression: results of a national survey. Drug Alcohol Depend. 1995;39:197–206. doi: 10.1016/0376-8716(95)01160-4. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of Substance Abuse. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Harford TC. Age at onset of alcohol use and DSM-IV alcohol abuse and dependence: a 12-year follow-up. Journal of Substance Abuse. 2001;13:493–504. doi: 10.1016/s0899-3289(01)00096-7. [DOI] [PubMed] [Google Scholar]
- Greenbaum PE, Brown EC, Friedman RM. Alcohol expectancies among adolescents with conduct disorder: prediction and mediation of drinking. Addict Behav. 1995;20(3):321–333. doi: 10.1016/0306-4603(94)00074-9. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, Michael J. The effect of depression on return to drinking: a prospective study. Arch Gen Psychiatry. 1998;55(3):259–265. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Griffin KW, Botvin GJ, Epstein JA, Doyle MM, Diaz T. Psychosocial and behavioral factors in early adolescence as predictors of heavy drinking among high school seniors. J Stud Alcohol. 2000;61:603–606. doi: 10.15288/jsa.2000.61.603. [DOI] [PubMed] [Google Scholar]
- Gustafson R. The development of alcohol-related expectancies from the age of 12 to the age of 15 for two Swedish adolescent samples. Alcohol Clin Exp Res. 1992;16:700–704. doi: 10.1111/j.1530-0277.1992.tb00664.x. [DOI] [PubMed] [Google Scholar]
- Hartka E, Johnstone B, Leino EV, Motoyoshi M, Temple MT, Fillmore KM. A meta-analysis of depressive symptomatology and alcohol consumption over time. Br J Addict. 1991;86:1283–1298. doi: 10.1111/j.1360-0443.1991.tb01704.x. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Pryzbeck TR. The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment. J Stud Alcohol. 1988;49:219–224. doi: 10.15288/jsa.1988.49.219. [DOI] [PubMed] [Google Scholar]
- Hill EM, Blow FC, Young JP, Singer KM. Family history of alcoholism and childhood adversity: joint effects on alcohol consumption and dependence. Alcohol Clin Exp Res. 1994;18:1083–1090. doi: 10.1111/j.1530-0277.1994.tb00085.x. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Drinking to cope and alcohol use and abuse in unipolar depression: a 10-year model. J Abnorm Psychol. 2003;112(1):159–65. [PubMed] [Google Scholar]
- Hussong AM, Chassin L. The stress-negative affect model of adolescent alcohol use: disaggregating negative affect. J Stud Alcohol. 1994;55(6):707–18. doi: 10.15288/jsa.1994.55.707. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Galloway CA, Feagans LA. Coping motives as a moderator of daily mood-drinking covariation. J Stud Alcohol. 2005;66(3):344–53. doi: 10.15288/jsa.2005.66.344. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Arria AM, Borges G, Ialongo N, Anthony JC. The growth of conduct problem behaviors from middle childhood to early adolescence: sex differences and the suspected influence of early alcohol use. J Stud Alcohol. 1995;56:661–671. doi: 10.15288/jsa.1995.56.661. [DOI] [PubMed] [Google Scholar]
- Kaplan HB. Martin SS. Robbins C. Application of a general theory of deviant behavior: Self-derogation and adolescent drug use. J Health Soc Behavior. 1982;23:274–294. [PubMed] [Google Scholar]
- Kaplow JB, Curran PJ, Angold A, Costello EJ. The prospective relation between dimensions of anxiety and the initiation of adolescent alcohol use. J Clin Child Psychol. 2001;30:316–326. doi: 10.1207/S15374424JCCP3003_4. [DOI] [PubMed] [Google Scholar]
- Kassel JD, Jackson SI, Unrod M. Generalized expectancies for negative mood regulation and problem drinking among college students. J Stud Alcohol. 2000;61(2):332–40. doi: 10.15288/jsa.2000.61.332. [DOI] [PubMed] [Google Scholar]
- Kelder SH, Murray NG, Orpinas P, Prokhorov A, McReynolds L, Zhang Q, Roberts R. Depression and substance use in minority middle-school students. Am J Public Health. 2001;91:761–766. doi: 10.2105/ajph.91.5.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellam SG, Anthony JC. Targeting early antecedents to prevent tobacco smoking: Findings from a epidemiologically based randomized field trial. Am J Public Health. 1998;88:1490–1495. doi: 10.2105/ajph.88.10.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellam SG, Werthamer-Larsson L, Dolan LJ, Brown CH, Mayer LS, Rebok GW, Anthony JC, Laudolff J, Edelsohn G. Developmental epidemiologically based preventive trials: Baseline modeling of early target behaviors and depressive symptoms. Am J Community Psychol. 1991;19:563–584. doi: 10.1007/BF00937992. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Health AC, Neale MC, Kessler RC, Eaves LJ. Alcoholism and major depression in women. A twin study of the causes of comorbidity. Arch Gen Psychiatry. 1993;50:690–698. doi: 10.1001/archpsyc.1993.01820210024003. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey. I: Lifetime prevalence, chronicity and recurrence. J Affect Disord. 1993;29(2−3):85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- King AC, Bernardy NC, Hauner K. Stressful events, personality, and mood disturbance: gender differences in alcoholics and problem drinkers. Addict Behav. 2003;28:171–187. doi: 10.1016/s0306-4603(01)00264-7. [DOI] [PubMed] [Google Scholar]
- Klein LC, Corwin EJ. Seeing the unexpected: how sex differences in stress responses may provide a new perspective on the manifestation of psychiatric disorders. Curr Psychiatry Rep. 2002;4(6):441–448. doi: 10.1007/s11920-002-0072-z. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Jordan MD. Adolescent alcohol and cannibis use in relation to peer and school factors. Results of multilevel analyses. Drug Alcohol Depend. 2006;84:167–174. doi: 10.1016/j.drugalcdep.2006.01.014. [DOI] [PubMed] [Google Scholar]
- Laurent J, Catanzaro SJ, Callan MK. Stress, alcohol-related expectancies and coping preferences: a replication with adolescents of the Cooper et al. (1992) model. J Stud Alcohol. 1997;58:644–651. doi: 10.15288/jsa.1997.58.644. [DOI] [PubMed] [Google Scholar]
- Maag JW, Irvin DM. Alcohol use and depression among African-American and Caucasian adolescents. Adolescence. 2005;40:87–101. [PubMed] [Google Scholar]
- Maisto SA, Connors GJ, Zywiak WH. Alcohol treatment, changes in coping skills, self-efficacy, and levels of alcohol use and related problems 1 year following treatment initiation. Psychol Addict Behav. 2000;14(3):257–266. doi: 10.1037//0893-164x.14.3.257. [DOI] [PubMed] [Google Scholar]
- Mason WA, Windle M. Family, religious, school and peer influences on adolescent alcohol use: a longitudinal study. J Stud Alcohol. 2001;62:44–53. doi: 10.15288/jsa.2001.62.44. [DOI] [PubMed] [Google Scholar]
- Miller PM, Smith GT, Goldman MS. Emergence of alcohol expectancies in childhood: a possible critical period. J Stud Alcohol. 1990;51:343–349. doi: 10.15288/jsa.1990.51.343. [DOI] [PubMed] [Google Scholar]
- Molina BS, Bukstein OG, Lynch KG. Attention-deficit/hyperactivity disorder and conduct disorder symptomatology in adolescents with alcohol use disorder. Psychol Addict Behav. 2002;16(2):161–164. doi: 10.1037//0893-164x.16.2.161. [DOI] [PubMed] [Google Scholar]
- Moscato BS, Russell M, Zielezny M, Bromet E, Egri G, Mudar P, Marshall JR. Gender differences in the relation between depressive symptoms and alcohol problems: a longitudinal perspective. Am J Epidemiol. 1997;146:966–974. doi: 10.1093/oxfordjournals.aje.a009224. [DOI] [PubMed] [Google Scholar]
- Nash SG, McQueen A, Bray JH. Pathways to adolescent alcohol use: family environment, peer influence, and parental expectations. J Adolesc Health. 2005;37(1):19–28. doi: 10.1016/j.jadohealth.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Pettinati HM, Pierce JD, Wolf AL, Rukstalis MR, O'Brien CP. Gender differences in comorbidity depressed alcohol-dependent outpatients. Alcohol Clin Exp Res. 1997;21(9):1742–1746. [PubMed] [Google Scholar]
- Read JP, O'Connor RM. High- and low-dose expectancies as mediators of personality dimensions and alcohol involvement. J Stud Alcohol. 2006;67(2):204–214. doi: 10.15288/jsa.2006.67.204. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Psychiatric comorbidity with problematic alcohol use in high school students. J Am Acad Child Adolesc Psychiatry. 1996;35:101–109. doi: 10.1097/00004583-199601000-00018. [DOI] [PubMed] [Google Scholar]
- Rutledge PC, Sher KJ. Heavy drinking from the freshman year into early young adulthood: the roles of stress, tension-reduction drinking motives, gender and personality. J Stud Alcohol. 2001;62:457–466. doi: 10.15288/jsa.2001.62.457. [DOI] [PubMed] [Google Scholar]
- Schell TL, Martino SC, Ellickson PL, Collins RL, McCaffrey D. Measuring developmental changes in alcohol expectancies. Psychol Addict Behav. 2005;19:217–220. doi: 10.1037/0893-164X.19.2.217. [DOI] [PubMed] [Google Scholar]
- Simons-Morton B, Haynie DL, Crump AD, Saylor KE, Eitel P, Yu K. Expectancies and other psychosocial factors associated with alcohol use among early adolescent boys and girls. Addict Behav. 1999;24:229–238. doi: 10.1016/s0306-4603(98)00095-1. [DOI] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Lepper H. Alcohol initiation outcomes of universal family-focused preventive interventions: one- and two-year follow-ups of a controlled study. J Stud Alcohol. 1999;(Suppl 13):103–111. doi: 10.15288/jsas.1999.s13.103. [DOI] [PubMed] [Google Scholar]
- STATA Corp. STATA Statistical Software . Reference Manual. STATA Press; Texas: 2000. Release 8.0SE. [Google Scholar]
- Tambs K, Harris JR, Magnus P. Genetic and environmental contributions to the correlation between alcohol consumption and symptoms of anxiety and depression. Results from a bivariate analysis of Norwegian twin data. Behav Genet. 1997;27:241–250. doi: 10.1023/a:1025662114352. [DOI] [PubMed] [Google Scholar]
- Thase ME, Salloum IM, Cornelius JD. Comorbid alcoholism and depression: treatment issues. J Clin Psychiatry. 2001;62(Suppl 20):32–41. [PubMed] [Google Scholar]
- Wang J, Patten SB. A prospective study of sex-specific effects of major depression on alcohol consumption. Can J Psychiatry. 2001;46:422–425. doi: 10.1177/070674370104600507. [DOI] [PubMed] [Google Scholar]
- Warner LA, White HR, Johnson V. Alcohol initiation experiences and family history of alcoholism as predictors of problem-drinking trajectories. J Stud Alcohol. 2007;68:56–65. doi: 10.15288/jsad.2007.68.56. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) Composite International Diagnostic Interview. WHO; Geneva: 1989. [Google Scholar]
- Wu LT, Anthony JC. Tobacco smoking and depressed mood in late childhood and early adolescence. Am J Public Health. 1999;89:1837–1840. doi: 10.2105/ajph.89.12.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young EA, Ribeiro SC. Sex differences in the ACTH response to 24H metyrapone in depression. Brain Res. 2006;1126(1):148–55. doi: 10.1016/j.brainres.2006.05.053. [DOI] [PubMed] [Google Scholar]
- Young EA. Sex differences and the HPA axis: implications for psychiatric disease. J Gend Specif Med. 1998;1(1):21–7. [PubMed] [Google Scholar]