Abstract
Summary
We examined the rate of clinical vertebral fractures, and the circumstances associated with the fractures, in a cohort of 5,995 US older men. Fractures were more common in the most elderly men, and were usually associated with falls and other low-energy trauma.
Introduction
Little is known about clinical vertebral fractures in older men. We postulated that clinical vertebral fractures occur with falls, affect men with osteoporosis, and are more common as age increases.
Methods
Five thousand nine hundred and ninety-five men aged ≥65 years were followed prospectively for an average of 4.7 years. Men with incident clinical vertebral fractures were compared to controls.
Results
One percent (n=61) sustained incident clinical vertebral fractures (2.2/1,000 person-years). The rate of fracture rose with age (0.7% in men 65–69 years and 5% ≥85 years). Fractured men were more likely frail (8.2% vs. 2.2%), more often fell (36.1% vs. 21%) and had lower total hip and lumbar spine BMD (all p values ≤0.002). In 73.8% of cases fractures were precipitated by no known trauma or by low-energy trauma, including falls in 57.3% Fractures were thoracic in 33% and lumbar in 56%. Men with an incident vertebral fracture were more likely to be osteoporotic (13% vs. 2%, p<0.0001), but most men with incident fractures did not have osteoporosis.
Conclusions
Incident clinical vertebral fractures were relatively common in older men and the rate increased after age 80 years. Fractures were usually associated with minimal trauma, most commonly a fall.
Keywords: BMD, Epidemiology, Men, Osteoporosis, Vertebral fractures
Introduction
Vertebral fractures are the most common type of osteoporotic fractures. Data from the European Vertebral Osteoporosis Study (EVOS) suggest that 12% of both men and women aged 50–80 years have a radiographic vertebral deformity, and the prevalence of deformity increases with age in both sexes [1]. Vertebral deformities are associated with adverse outcomes including back pain, physical impairment [2, 3], an increased risk of future osteoporotic fractures [4–6] and an increased risk of mortality [4, 7]. It is estimated that a minority (from 22% to 33%) of vertebral fractures come to medical attention [3, 8–10]; these “clinical” vertebral fractures are associated with a higher morbidity [11, 12] and mortality [13–15].
There is little information concerning clinical vertebral fractures in women or men. Previous studies have been cross-sectional or retrospective and most have included young patients who are likely to sustain fractures from more severe trauma [8, 11]. For instance, we found no prospective data about patient characteristics or BMD associated with clinical vertebral fractures in older men. It has been assumed that most vertebral fractures are the result of skeletal fragility rather than trauma [16, 17], but littl information is available concerning this issue.
The Osteoporotic Fractures in Men (MrOS) study is a large prospective cohort study of fractures in older men. We investigated the incidence of clinical vertebral fractures in MrOS, the circumstances associated with their occurrence and the clinical characteristics of men who sustained these fractures.
Materials and methods
Study population
The MrOS Study enrolled 5,995 men at six U.S. clinical centers (Birmingham AL, Minneapolis MN, Palo Alto CA, Pittsburgh PA, Portland OR and San Diego CA) from March 2000 through April 2002. Eligible participants were at least 65 years of age, were able to walk without assistance from another person, and had not had bilateral hip replacement surgery. All MrOS participants completed the baseline self-administered questionnaire and attended the baseline visit during which skeletal, anthropometric and other measures were obtained. Details of the MrOS recruitment and study design have been published elsewhere [18, 19]. The institutional review board at each site approved the study protocol and written informed consent was obtained from all participants.
Baseline characteristics and measurements
Information obtained by self-administered questionnaire included demographic factors, tobacco and alcohol history, medications, history of falls (within the 12 months prior to baseline) and fracture history. Age was computed from date of birth. Participants were classified into mutually exclusive categories of race/ethnicity as white, black, Asian, Hispanic or other based on self-report. Cigarette smoking was classified as current, past or never. Current alcohol consumption was computed as average number of drinks per week. Height (cm) was measured using a Harpenden stadiometer. Participants were weighed (Kg) on balance beam or digital scales while wearing indoor clothing except shoes. Body mass index (BMI) was calculated as weight divided by the square of height in meters (Kg/m2). Frailty was accessed using the Fried index [20] slightly modified for the MrOS Study [21]. A man was considered frail if he had three or more of the following criteria: sarcopenia, low activity, weakness, slowness or low energy. Men with one or two criteria were considered prefrail, and those with no criteria present were considered robust. Lateral lumbar and thoracic radiographs were obtained at baseline and were available for a comparison with radiographs obtained at the time of possible incident clinical vertebral fracture. Bone mineral density (BMD) was measured in the proximal femur and lumbar spine using DXA measured by Hologic QDR 4500 densitometers.
Follow-up and ascertainment of clinical vertebral fractures
Every four months study participants completed a one-page mailed questionnaire asking about the occurrence of incident falls and fractures in the previous 4-month period. If a participant reported a fracture, study staff conducted a follow-up interview to determine the date/time of the fracture and a description of how the fracture occurred. An incident “clinical” vertebral fracture was defined by the presence of both symptoms suggestive of vertebral fracture, such as neck or back pain, that prompted the participant to seek medical attention and by a clinical radiograph that documented the presence of a new vertebral deformity. Verification of a new vertebral deformity was obtained in all cases by comparing the clinical radiograph (including any X-rays, CT and MRI studies) obtained from the participant's physician. The baseline study thoracic and lumber radiographs were examined to verify that a fracture was not present at the start of observation. Cervical radiographs were not obtained at baseline because cervical fractures are uncommon. In this study, all the clinical cervical fractures were associated with severe deformity and high levels of trauma, and thus it's unlikely that they did not represent incident fracture events. Semiquantitative (SQ) methods [22] were used to determine incident fracture, defined as a distinct alteration in morphology of vertebral body resulting in a higher grade (grade 1–3) when the clinical radiograph was compared to the same vertebrae on the baseline study radiograph. The SQ criteria was also used to determine the severity of vertebral fractures (mild, moderate or severe) based on the descriptions in the radiological reports obtained from participants' medical records. A fracture was considered mild if the radiology report described it as mild or as having a 20–25% reduction in vertebral anterior, middle and/or posterior height; moderate if described as moderate or with a >25–40% reduction in height and severe if described as severe or with a reduction >40% in height.
There were a total of 142 possible vertebral fractures reported on mailed questionnaires by 108 MrOS participants during the follow-up. Of these, 62 possible vertebral fractures (in 44 participants) were not confirmed by the study radiologist and were excluded from further analyses. 64 MrOS participants were found to have at least one confirmed incident vertebral fracture. Three of these cases (5%) were excluded because the discovery of a fracture was not linked to the presence of skeletal symptoms (e.g., a fracture was incidentally noted at the time of chest X-ray for cardiopulmonary disease). Thus, 61 participants with fracture linked to symptoms were included in this report. None of the fractures reported were pathological (i.e., related to local vertebral neoplasia, infection, etc.).
Circumstances of incident clinical vertebral fractures
Based on the participants' descriptions, fractures were assigned to one of seven categories of trauma: fall from standing height or less; fall on stairs, steps or curb; fall from more than standing height; minimal trauma other than a fall; moderate trauma other than a fall; severe trauma other then a fall; circumstances unknown (Table 1). It was assumed that in most cases in which the circumstances were unknown there was no obvious trauma.
Table 1.
Degree of trauma categories
| Degree of trauma | Description |
|---|---|
| Fall from standing height or less | This includes most injuries due to tripping over something, slipping in the shower or bathtub, or falling out of a chair (unless standing on it), in which the participant lands on the surface at the same height as the surface he has been standing on |
| Fall on stairs, steps or curb | This includes all falls during change of level, such as stepping up or downstairs, steps or curbs |
| Fall from more than standing height, but not on stairs |
This includes falls from heights such as off a ladder or while standing on a table or chair, off a porch, out of a window, etc. |
| Minimal trauma other than a fall | This includes vertebral fractures associated with coughing, stepping down a step, turning over in bed, etc. |
| Moderate trauma other than a fall | This includes collisions with objects during normal activities (e.g., stub toe, hit hand against doorframe, walking into door) |
| Severe trauma other than a fall | This includes motor vehicle accidents, struck by a car, hit by rapidly moving projectile (golf ball or golf club), assault |
| Circumstance unknown | This includes situations where respondent cannot remember how the fracture occurred |
Statistical analysis
Distributions of baseline characteristics among men with and without incident clinical vertebral fracture were compared using chi-square tests for categorical variables and t tests for continuous variables. Clinical vertebral fracture rates were calculated by five-year age groups. Rates were expressed as numbers of fractures per 1,000 person-years of follow-up and the 95% confidence intervals (CIs) were calculated using the exact Poisson formula. Femoral BMD T-scores using both male and female reference ranges were used to classify fractures by baseline BMD category (osteoporosis: T-score ≥−2,5, low bone mass: T-score between −1 and −2.5 or normal BMD: T-score ≤−1.0) [23]. Multivariate Cox proportional hazards model was used to assess the increase in fracture risk of potential contributors, with time-to-first clinical vertebral fracture as the outcome. All analyses were performed with Statistical Analysis Systems, version 9.1 (SAS Institute Inc., Cary, NC, USA, 2003).
Results
Seventy-five incident clinical vertebral fractures occurred in 61 subjects (1% of the cohort) during a follow-up of 4.7± 0.9 years. Baseline characteristics of the MrOS participants with or without at least one incident clinical vertebral fracture are presented in Table 2. Men who sustained an incident clinical vertebral fracture, when compared to those who did not, were older (77.5 vs. 73.6 years, respectively, p< 0.0001), were more likely to be frail (8.2% vs. 2.2%, p= 0.002) and had lower total hip BMD (0.863 vs. 0.959 g/cm2, p<0.0001) and lumbar spine BMD (1.030 vs. 1.179 g/cm2, p<0.0001). A higher proportion of men with fractures reported a history of falls in the 12 months prior to baseline (36.1% vs. 21%, p<0.0001). Other characteristics at enrollment (race, anthropometric measurements, use of glucocorticoids, smoking and alcohol habits and prior history of fractures) were similar between the groups.
Table 2.
Baseline characteristics of men with and without incident clinical vertebral fractures in the MrOS study
| Men with clinical vertebral fracturesa (N=61) |
Men without clinical vertebral fracturesa (N=5934) |
P value | ||
|---|---|---|---|---|
| Age (yr) | 77.5±6.9 | 73.6±5.8 | <0.001 | |
| Caucasian race | 95.10% | 89.40% | 0.2 | |
| Weight (Kg) | 80.2±13.1 | 83.2±13.3 | 0.08 | |
| Height (cm) | 173.5±6.5 | 174.2±6.8 | 0.5 | |
| BMI (Kg/m2) | 26.6±4.1 | 27.4±3.8 | 0.1 | |
| Glucocorticoid useb | 8.20% | 5.60% | 0.4 | |
| Smoking | ||||
| Current | 6.60% | 3.40% | 0.3 | |
| Past | 62.30% | 59% | ||
| Never smoked | 31.10% | 37.60% | ||
| Alcohol use (drinks/week) | 3.7±5.2 | 4.3±6.8 | 0.4 | |
| Frailtyc | 8.20% | 2.20% | 0.002 | |
| Prior fractures | 60.70% | 55.30% | 0.4 | |
| History of falls at baseline | 36.10% | 21% | 0.004 | |
| Total hip BMD (g/cm2) | 0.863±0.1 | 0.959±0.1 | <0.0001 | |
| Lumbar spine BMD (g/cm2) | 1.030±0.2 | 1.179±0.2 | <0.0001 | |
Categorical variables were expressed as percentage of occurrence and continuous variables as mean±1 SD
Current or past use
Presence of at least three components of frailty
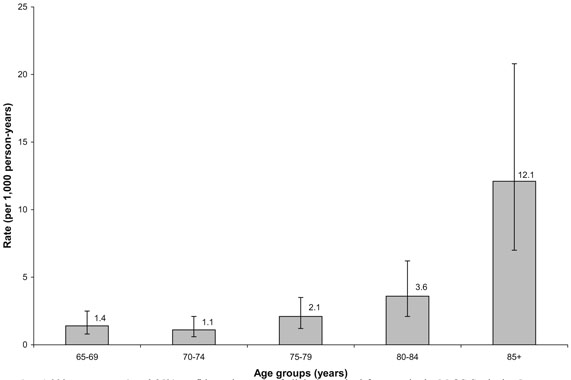
The overall rate of clinical vertebral fractures was 2.2 per 1,000 person-years (95% CI 1.7–2.8) and when cervical fractures were not considered (only thoracic and lumber fractures were considered) the incidence was 1.9 per 1,000 person-years (95% CI 1.46, 2.50). The rates of clinically diagnosed vertebral fractures by five-year age categories are shown in Fig. 1. The proportion of men that experienced a fracture in each five-year category during follow-up rose with age (0.7% in 65–69 yr; 0.5% in 70–74 yr; 1.0% in 75–79 yr; 1.6% in 80–84 yr and 5% in ≥85 yr). Compared to men aged 65–69 years, the risk of fracture was higher in those aged 80–84 years and 85 years and older (hazard ratios 2.6, 95% CI 1.2–5.7, and 8.9, 95% CI 4.1–19.5, respectively). When only thoracic and lumber fractures were considered the pattern was similar.
Fig. 1.
Rates (per 1,000 person-years) and 95% confidence intervals of clinical vertebral fractures in the MrOS Study, by 5-year age categories
The circumstances associated with incident clinical vertebral fractures are shown in Table 3. Fractures were most commonly associated with a fall from standing height or less (41%). A fall of any type was associated with incident clinical vertebral fractures in 57.3% of subjects. Fewer fractures (21.4%) occurred as a result of unknown trauma (for example, were discovered in association with back pain but without a history of an inciting event). In 73.8% of cases the fractures were attributed to low-energy (fall from standing height or less, or minimal trauma other than a fall) or unknown trauma; only 14.8% of men reported severe trauma (fall from more than standing height or severe trauma other than a fall) at the time of fracture.
Table 3.
Circumstances of incident clinical vertebral fractures in MrOS participants
| Circumstances of fractures | Participants with clinical vertebral fracturesa |
|---|---|
| Fall from standing height or less | 41% |
| Fall on stairs, steps or curbs | 8.1% |
| Fall from more than standing height | 8.2% |
| Minimal trauma other then a fall | 11.4% |
| Moderate trauma other than a fall | 3.3% |
| Severe trauma other than a fall | 6.6% |
| Circumstance unknown | 21.4% |
Results were expressed as percentage of the total number of subjects with fractures (n=61). Ten subjects had more than one incident clinical vertebral fracture (six had two fractures and four had three fractures). In the case of multiple fractures, all fractures were reported on the same date.
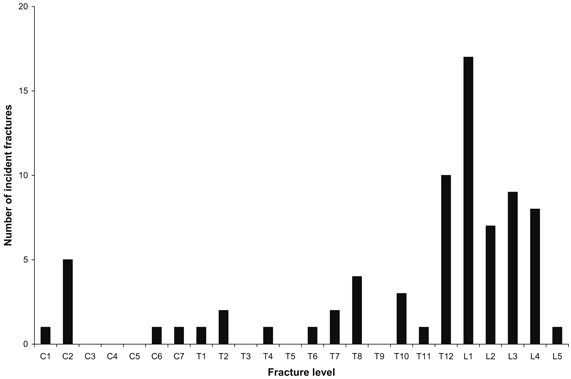
Cervical fractures occurred in eight (10.7%) men, and most (five fractures) occurred at C2. These cervical fractures were complex (none were compression or wedge) and were associated with severe trauma. Thoracic (n=25; 33.3%) or lumbar (n=42; 56%) fractures were most frequently in the thoracolumbar transition zone (13.3% T12 and 22.7% L1; Fig. 2). Among thoracic and lumbar fractures, 18 (26.9%) were classified as mild, 14 (20.9%) as moderate and 13(19.4%) as severe. Information from the remaining fracture reports (N=30, 40% of cases) was insufficient (“compression” or “wedge”) to classify the remaining fractures by severity. Of fractured men, 16.4% (n=10) had more than one incident clinical vertebral fracture (six had two fractures and four had three fractures); in each subject all of these multiple fractures were reported on the same date.
Fig. 2.
Number of incident clinical vertebral fractures by vertebral level
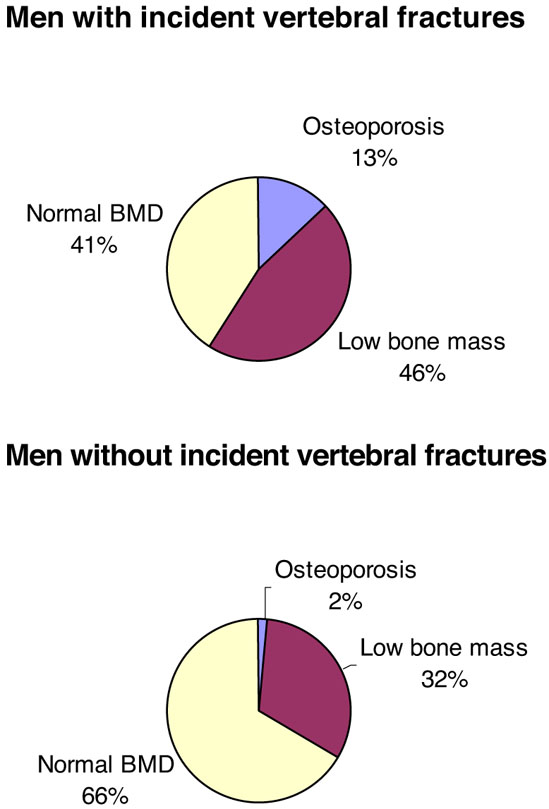
Clinical vertebral fractures were more common in men with lower BMD at the total hip (age-adjusted hazard ratio per 1 SD decrease: 1.9, 95% CI: 1.4–2.5, p<0.0001) and lumbar spine (age-adjusted hazard ratio: 2.3, 95% CI: 1.6–3.2, p<0.0001). Men who suffered an incident vertebral fracture were more likely to be osteoporotic than men who did not (13% vs. 2%, p<0.0001). Figure 3 shows the proportions of clinical vertebral fractures that occurred in men with osteoporosis (13%), low bone mass (46%) and normal BMD (41%) using male total hip T-scores reference ranges. When BMD was measured at the femoral neck, 16% of men with clinical vertebral fractures were osteoporotic, 61% had low bone mass and 23% had normal BMD. When female reference ranges were used, the proportion of men with osteoporosis, low bone mass and normal total hip BMD were 5%, 33% and 62%, respectively. Regardless of site and reference range used, more than 80% of men with incident vertebral fractures did not have osteoporotic T-scores. In men with osteoporosis, 75% (6 of 8) of fractures were associated with low-energy or unknown trauma and in men with normal BMD 68% (17 of 25) were associated with low-energy or unknown trauma.
Fig. 3.
Distribution of BMD categories in men with and without incident clinical vertebral fractures using male T-scores at total hip
When the relationship of fracture risk to baseline age, total hip BMD, frailty status (yes or no) and history of falls was examined in a multivariate analysis, total hip BMD (X2=18.8, p<0.0001) age >85 years (X2=15.1, p=0.0001), and falls history (X2=,3.9 p=0.04) were independent predictors, and frailty status (X2=3.2, p=0.07) was of borderline significance.
Discussion
This is the first large prospective study of clinical vertebral fractures in older men. We found that clinical vertebral fractures were relatively common, particularly in the oldest age groups. For instance, 1% of all participants and 5% of those aged ≥85 years experienced one or more clinical vertebral fractures during the 4.7 years of follow-up. Most fractures occurred as a result of falls and other low-energy trauma and few were the result of severe trauma. Fractures occurred most frequently at the thoracolumbar junction and were associated with lower bone mineral density. However, most fractures occurred in men with BMD T-scores >−2.5.
Clinical vertebral fractures were particularly common in the oldest men. Since clinical vertebral fractures in men are associated with important reductions in quality of life and other morbidities [11, 12], and may be associated with increased mortality [13–15], these fractures represent an important health problem. The relationship between age and fractures described here is consistent with previous retrospective reports. Our rates were somewhat lower than those reported in similarly aged men in England and Wales [24], but similar to those in Rochester (US) [25], southern Victoria (Australia) [26] and Malmö (Sweden) [27]. Our fracture rates were also about one-third those reported for incident radiographic vertebral deformities in older men [28, 29], and this supports the estimate that only about one-fourth to one-third of all vertebral fractures are clinically diagnosed [3, 8–10].
There are few studies describing the circumstances associated with clinical vertebral fractures. Most (>70%) clinical vertebral fractures in our cohort were associated with low-energy trauma or no known injury and it was uncommon that clinical vertebral fractures were the result of severe trauma (e.g., motor vehicle accidents). Overall, about one in five incident fracture patients presented with back pain but without known injury. The only published study reporting the degree of trauma in incident clinical vertebral fractures was a retrospective review of men and women residents in Rochester, Minnesota [8] that found 83% of all fractures were related to moderate or minimal trauma (defined as less than or equal to a fall from standing height), and only 14% were caused by severe trauma (traffic accidents and falls from greater than standing height). In the subgroup of older men (aged 65 years and older), the proportion of fractures caused by moderate or severe trauma was also low (18%) - similar to our finding of 26.2%.
A fall was associated with almost 60% of the fractures we observed, and men who reported a history of falling experienced more fractures. Falls are common in the elderly [30, 31] and are associated with increased risk of hip and other osteoporotic fractures [8, 32]. However, there is a general impression that falls are not important in the pathogenesis of vertebral fractures and that most of these fractures are precipitated by routine everyday activities, like lifting and bending [33]. Our results indicate that falls are an important cause of clinical vertebral fractures in older men.
Our results corroborate previous observations about the association between lower BMD and vertebral fractures [29, 34–37]. BMD values were lower for men who fractured than for those who did not, and each 1SD decrease in lumbar spine or femoral BMD was associated with an approximated twofold increased risk of incident clinical vertebral fractures. However, most men fractured with normal BMD or low bone mass. Our data are in agreement with studies in women [38, 39] and demonstrate that BMD is important, but not sufficient, for prediction of fractures in older men. The addition of other parameters that affect bone strength may improve the prediction of fractures [40, 41]. Moreover, non-skeletal factors are probably important in the determination of fracture risk. The ability of the spine to resist fracture depends not only on the structural capacity of the vertebrae but also on the loading conditions that arise from activities of daily living or trauma [42]. Our results suggest that a combination of increases in fall risk and reductions in bone density are important factors in the age-related increase in clinical vertebral fractures.
Frailty increases with age and is a risk factor for falls, disability, hospitalization and death [20]. Older women with hip fractures are more likely to have markers of frailty than those without fractures [43], and frailty predicts the risk of hip fractures in women [44]. Our study adds new information regarding frailty and clinical vertebral fractures, demonstrating that these two entities can be associated in older men. Although we did not find that other risk factors, such as smoking, alcohol intake and glucocorticoids use, were significantly more common in men who reported a clinical vertebral fracture, the number of participants with fractures reported here is relatively low, and our ability to detect effects of these factors may be limited.
The most frequent site of fractures was in the thoracolumbar region (T12 to L4), and these data are consistent with previous reports based on the location of all vertebral deformities [29] and clinical vertebral fractures [8] in men. However, we observed a lower frequency of fractures in the midthoracic region than expected. Several studies in men and women have reported that vertebral deformities cluster at the midthoracic and thoracolumbar regions of the spine, potentially as a result of the biomechanical forces exerted at these sites [8, 29, 45]. The distribution of clinical vertebral fractures noted here (more often in the lower spine) may reflect a different causation of clinical vertebral fractures that do not come to clinical attention.
To our knowledge, this is the first prospective study of the circumstances associated with incident clinical vertebral fractures in older men. Our study has several strengths, including the large, community dwelling cohort and the standardized methods for detecting, characterizing and adjudicating fractures. However, it also has limitations. Despite the large number of men followed for ~5 years, there were relatively few clinical vertebral fractures. The study was of US men who were primarily Caucasian, and our results may not be generalizable to other racial groups or geographies. Although it is likely that participant recall of fracture events was accurate via the tri-annual questionnaires, the possibility exists that some clinical vertebral fractures were not reported or accurately described. Our study is intended to provide a clinical characterization of men who suffer clinical vertebral fracture, but we have not undertaken a comprehensive analysis of the factors that may increase clinical vertebral fracture risk. These relevance of these findings to clinically undetected vertebral fractures is uncertain.
In summary, clinical vertebral fractures were relatively common in older men, particularly the most elderly (>80 years) and those who were frail. Although bone mineral density was lower in men who sustained fractures, most fractures occurred in men with BMD T-scores >−2.5. Fractures were most commonly the result of falls and other low-energy trauma.
Acknowledgments
The Osteoporotic Fractures in Men (MrOS) study is supported by the National institutes of Health. The following Institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), and the National Cancer Institute (NCI) through grants U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197 and M01 RR000334.
We thank all the participants in the Osteoporotic Fractures in Men Study for their continued participation.
Footnotes
Conflict of interest statement Dr. Orwoll receives research, consulting or speaking support from Aventis, Pfizer, Eli Lilly & Co., Novartis, Merck & Co., Procter & Gamble, GlaxoSmithKline, Zelos Therapeutics Inc., Imaging Therapeutics Ind., Solvay Pharmaceuticals. All other authors have no conflicts of interest.
References
- 1.O'Neill TW, Felsenberg D, Varlow J, et al. The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res. 1996;11:1010–1018. doi: 10.1002/jbmr.5650110719. [DOI] [PubMed] [Google Scholar]
- 2.Ettinger B, Black DM, Nevitt MC, et al. Contribution of vertebral deformities to chronic back pain and disability. The Study of Osteoporotic Fractures Research Group. J Bone Min Res. 1992;7:449–456. doi: 10.1002/jbmr.5650070413. [DOI] [PubMed] [Google Scholar]
- 3.Nevitt MC, Ettinger B, Black DM, et al. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med. 1998;128:793–800. doi: 10.7326/0003-4819-128-10-199805150-00001. [DOI] [PubMed] [Google Scholar]
- 4.Hasserius R, Karlsson MK, Nilsson BE, et al. Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int. 2003;14:61–68. doi: 10.1007/s00198-002-1316-9. [DOI] [PubMed] [Google Scholar]
- 5.Lindsay R, Silverman SL, Cooper C, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285:320–323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- 6.Pongchaiyakul C, Nguyen ND, Jones G, et al. Asymptomatic vertebral deformity as a major risk factor for subsequent fractures and mortality: a long-term prospective study. J Bone Min Res. 2005;20:1349–1355. doi: 10.1359/JBMR.050317. [DOI] [PubMed] [Google Scholar]
- 7.Ismail AA, O'Neill TW, Cooper C, et al. Mortality associated with vertebral deformity in men and women: results from the European Prospective Osteoporosis Study (EPOS) Osteoporos Int. 1998;8:291–297. doi: 10.1007/s001980050067. [DOI] [PubMed] [Google Scholar]
- 8.Cooper C, Atkinson EJ, O'Fallon WM, et al. Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res. 1992;7:221–227. doi: 10.1002/jbmr.5650070214. [DOI] [PubMed] [Google Scholar]
- 9.Fink HA, Milavetz DL, Palermo L, et al. What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Min Res. 2005;20:1216–1222. doi: 10.1359/JBMR.050314. [DOI] [PubMed] [Google Scholar]
- 10.Ettinger B, Black DM, Mitlak BH, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results froma 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA. 1999;282:637–645. doi: 10.1001/jama.282.7.637. [DOI] [PubMed] [Google Scholar]
- 11.Scane AC, Francis RM, Sutcliffe AM, et al. Case-control study of the pathogenesis and sequelae of symptomatic vertebral fractures in men. Osteoporos Int. 1999;9:91–97. doi: 10.1007/s001980050120. [DOI] [PubMed] [Google Scholar]
- 12.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–1733. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 13.Hasserius R, Karlsson MK, Jonsson B, et al. Long-term morbidity and mortality after a clinically diagnosed vertebral fracture in the elderly-a 12- and 22-year follow-up of 257 patients. Calcif Tissue Int. 2005;76:235–242. doi: 10.1007/s00223-004-2222-2. [DOI] [PubMed] [Google Scholar]
- 14.Cooper C, Atkinson EJ, Jacobsen SJ, et al. Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993;137:1001–1005. doi: 10.1093/oxfordjournals.aje.a116756. [DOI] [PubMed] [Google Scholar]
- 15.Center JR, Nguyen TV, Schneider D, et al. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–888. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 16.Papaioannou A, Joseph L, Ioannidis G, et al. Risk factors associated with incident clinical vertebral and nonvertebral fractures in postmenopausal women: the Canadian Multicentre Osteoporosis Study (CaMos) Osteoporos Int. 2005;16:568–739. doi: 10.1007/s00198-004-1735-x. [DOI] [PubMed] [Google Scholar]
- 17.Klotzbuecher CM, Ross PD, Landsman PB, et al. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Min Res. 2000;15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 18.Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the Osteoporotic Fractures in Men (MrOS) study - a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26:569–585. doi: 10.1016/j.cct.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 19.Blank JB, Cawthon PM, Carrion-Petersen ML, et al. Overview of recruitment for the Osteoporotic Fractures in Men Study (MrOS) Contemp Clin Trials. 2005;26:557–568. doi: 10.1016/j.cct.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 20.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 21.Cawthon PM, Marshall LM, Michael Y, et al. Frailty in Older Men: Prevalence, Progression and Relation to Mortality. Journal of the American Geriatrics Society. doi: 10.1111/j.1532-5415.2007.01259.x. In Press. [DOI] [PubMed] [Google Scholar]
- 22.Genant HK, Wu CY, Van Kuijk C, et al. Vertebral fracture assessment using a semiquantitative technique. J Bone Min Res. 1993;8:1137–1148. doi: 10.1002/jbmr.5650080915. [DOI] [PubMed] [Google Scholar]
- 23.Looker AC, Wahner HW, Dunn WL, et al. Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int. 1998;8:468–489. doi: 10.1007/s001980050093. [DOI] [PubMed] [Google Scholar]
- 24.Van Staa TP, Dennison EM, Leufkens HGM, et al. Epidemiology of fractures in England and Wales. Bone. 2001;29:517–522. doi: 10.1016/s8756-3282(01)00614-7. [DOI] [PubMed] [Google Scholar]
- 25.Melton LJ, 3rd, Atkinson EJ, Cooper C, et al. Vertebral fractures predict subsequent fractures. Osteoporos Int. 1999;10:214–221. doi: 10.1007/s001980050218. [DOI] [PubMed] [Google Scholar]
- 26.Sanders KM, Seeman E, Ugoni AM, et al. Age- and genderspecific rate of fractures in Australia: a population-based study. Osteoporos Int. 1999;10:240–247. doi: 10.1007/s001980050222. [DOI] [PubMed] [Google Scholar]
- 27.Kanis JA, Johnell O, Oden A, et al. Long-term risk of osteoporotic fracture in Malmo. Osteoporos Int. 2000;11:669–674. doi: 10.1007/s001980070064. [DOI] [PubMed] [Google Scholar]
- 28.The European Prospective Osteoporosis Study (EPOS) Group The relationship between bone density and incident vertebral fracture in men and women. J Bone Min Res. 2002;17:2214–2221. doi: 10.1359/jbmr.2002.17.12.2214. [DOI] [PubMed] [Google Scholar]
- 29.Van der Klift M, de Laet CEDH, McCloskey EV, et al. The incidence of vertebral fractures in men and women: the Rotterdam Study. J Bone Min Res. 2002;17:1051–1056. doi: 10.1359/jbmr.2002.17.6.1051. [DOI] [PubMed] [Google Scholar]
- 30.Kennedy RL, Grant PT, Blackwell D. Low-impact falls: demands on a system of trauma management, prediction of outcome, and influence of comorbities. J Trauma. 2001;51:717–724. doi: 10.1097/00005373-200110000-00016. [DOI] [PubMed] [Google Scholar]
- 31.Orwoll ES, Lambert LC, Marshall LM, et al. Endogenous testosterone levels, physical performance, and fall risk in older men. Arch Intern Med. 2006;166:2124–2131. doi: 10.1001/archinte.166.19.2124. [DOI] [PubMed] [Google Scholar]
- 32.Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. N Engl J Med. 1995;332:767–773. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 33.Cummings SR, Melton LJ., 3rd Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 34.Szulc P, Munoz F, Duboeuf F, et al. Bone mineral density predicts osteoporotic fractures in elderly men - the MINOS Study. Osteoporos Int. 2005;16:1184–1192. doi: 10.1007/s00198-005-1970-9. [DOI] [PubMed] [Google Scholar]
- 35.Cauley JA, Zmuda JM, Wisniewski SR, et al. Bone mineral density and prevalent vertebral fractures in men and women. Osteoporos Int. 2004;15:32–37. doi: 10.1007/s00198-003-1462-8. [DOI] [PubMed] [Google Scholar]
- 36.Nguyen TV, Eisman JA, Kelly PJ, et al. Risk factors for osteoporotic fractures in elderly men. Am J Epidemiol. 1996;144:255–263. doi: 10.1093/oxfordjournals.aje.a008920. [DOI] [PubMed] [Google Scholar]
- 37.Cummings SR, Cawthon PM, Ensrud KE, et al. BMD and risk of hip and nonvertebral fractures in older men: a prospective study and comparison with older women. J Bone Min Res. 2006;21:1550–1555. doi: 10.1359/jbmr.060708. [DOI] [PubMed] [Google Scholar]
- 38.Siris ES, Miller PD, Barrett-Connor E, et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women. Results from the National Osteoporosis Risk Assessment. JAMA. 2001;286:2815–2822. doi: 10.1001/jama.286.22.2815. [DOI] [PubMed] [Google Scholar]
- 39.Schuit SCE, van der Klift M, Weel AEAM, et al. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone. 2004;34:195–202. doi: 10.1016/j.bone.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 40.Szulc P, Munoz F, Duboeuf F, et al. Low width of tubular bones is associated with increased risk of fragility fracture in elderly men - the MINOS Study. Bone. 2006;38:595–602. doi: 10.1016/j.bone.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 41.Riggs BL, Melton LJ, 3rd, Robb RA, et al. Population-based analysis of the relationship of whole bone strength indices and fall-related loads to age- and sex-specific patterns of hip and wrist fractures. J Bone Min Res. 2006;21:315–323. doi: 10.1359/JBMR.051022. [DOI] [PubMed] [Google Scholar]
- 42.Myers ER, Wilson SE. Biomechanics of osteoporosis and vertebral fractures. Spine. 1997;22:25S–31S. doi: 10.1097/00007632-199712151-00005. [DOI] [PubMed] [Google Scholar]
- 43.Kado DM, Duong T, Stone KL, et al. Incident vertebral fractures and mortality in older women: a prospective study. Osteoporos Int. 2003;14:589–594. doi: 10.1007/s00198-003-1412-5. [DOI] [PubMed] [Google Scholar]
- 44.Woods NF, LaCroix AZ, Gray SL, et al. Frailty: emergence and consequences in women aged 65 and older in the Women's Health Initiative Observational Study. J Am Geriatr Soc. 2005;53:1321–1330. doi: 10.1111/j.1532-5415.2005.53405.x. [DOI] [PubMed] [Google Scholar]
- 45.Samelson EJ, Hannan MT, Zhang Y, et al. Incidence and risk factors for vertebral fracture in women and men: 25-year follow-up results from the population-based Framingham Study. J Bone Min Res. 2006;21:1207–1214. doi: 10.1359/jbmr.060513. [DOI] [PubMed] [Google Scholar]