Abstract
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Co-proxamol is associated with excess mortality in overdose
Legislative change in 2005 has led to a phased withdrawal of co-proxamol from the UK market
WHAT THIS STUDY ADDS
Co-proxamol legislation resulted in a marked reduction in the number of prescriptions for co-proxamol within 6 months
This was followed by a major reduction in mortality associated with co-proxamol poisoning
Overall mortality from drug poisoning in Scotland has also fallen over the same period, suggesting an effect on total overdose mortality
AIM
To determine what effect the withdrawal of co-proxamol from the UK market has had on mortality from poisoning in Scotland.
METHODS
This was a retrospective, observational study of mortality relating to poisoning by single agents in Scotland for the period 2000–2006. Mortality data were obtained from the General Register Office Scotland, and primary care prescribing data from the Information and Statistics Division of the Scottish Executive Health Department.
RESULTS
A significant reduction in the proportion of poisoning deaths due to co-proxamol was observed following legislation [mean 2000–2004, 37 deaths (21.8% of total poisoning deaths); 2006, 10 (7.8%); P < 0.0001]. The most significant reduction was seen in male out-of-hospital deaths [mean 2000–2004, 17 (21.8%); 2006, two (2.9%); P < 0.0001]. This was associated with a decline in prescriptions by 60% within 6 months of legislation. The total number of poisoning deaths also fell, slightly earlier than the full impact on co-proxamol deaths (mean 2000–2004, 171.2; mean 2005–2006, 129.5; P = 0.005).
CONCLUSIONS
Legislation has resulted in a major reduction in the number of deaths associated with co-proxamol poisoning in Scotland, with no compensatory rise in mortality from poisonings from other common analgesics. We estimate from this study that a minimum of 300 lives across the UK will have been saved by the withdrawal of co-proxamol.
Keywords: co-proxamol, legislation, mortality, overdose
Introduction
Co-proxamol (paracetamol 325 mg and dextropropoxyphene 32.5 mg) was previously one of the most commonly prescribed analgesics in the UK. However, it has been associated with an increased risk of death in overdose and has not been shown to possess any analgesic advantage over paracetamol alone [1–3]. Studies have estimated that a minimum of 39 excess deaths each year in Scotland are due to co-proxamol poisoning [1]. This has been attributed to a combination of the opioid and non-opioid effects of the dextropropoxyphene. Conduction disturbances such as QRS prolongation, due to sodium channel blockade, leave patients vulnerable to fatal arrhythmias, particularly when hypoxic, and a large proportion of patients die before reaching hospital [4–6]. Restricting availability of methods of suicide is an important component in suicide prevention strategies. [7] This can be conducted in several ways, including educating doctors about the risks of co-proxamol, reducing the size of prescriptions, restricting prescribing to specialists, or complete withdrawal of the drug from the market. In view of the poorly established efficacy associated with co-proxamol and the risk of toxicity in overdose, the Committee of Safety on Medicines recommended co-proxamol undergo a phased withdrawal from the UK market in January 2005 [8]. This is a rare example in which concern over the effect of a drug in overdose contributed to its withdrawal, and a phased withdrawal period was undertaken to allow time for the significant number of patients taking co-proxamol to be converted onto an alternative analgesic. An important concern was the potential for switch to other agents for suicide. This study reports the effect of legislation on Scottish mortality from overdose.
Methods
Mortality data relating to poisoning by single agents in Scotland were obtained from the General Register Office for the period 2000–2006. Deaths due to co-proxamol poisoning alone (± alcohol) were identified. Deaths involving co-proxamol in a mixed overdose were excluded. The proportion of all poisoning deaths due to co-proxamol for the 5 years pre-legislation (2000–2004) was compared with the 2 years after legislation (2005–2006). Co-proxamol deaths were compared with those as a result of poisoning from other commonly used analgesics. Deaths are recorded by location and we compared the distribution of deaths occurring in-hospital with those occurring out-of-hospital, before the patient reaches medical care. Quarterly primary care prescribing data were obtained from the Information and Statistics Division of the Scottish Executive Health Department. Adding the mortality figures associated with co-proxamol poisoning reported in England and Wales [3] to that in Scotland allowed an estimate of the number of lives saved by legislation. Statistical analyses were undertaken using two-tailed Fisher's exact test and Student's t-test in Graphpad Software, Inc. Quickcalcs 2005 (Graphpad, San Diego, CA, USA).
Results
The data demonstrate a decline in co-proxamol deaths following legislation in 2005, with the reduction reaching statistical significance in 2006 [mean 2000–2004, 37 deaths (21.8% of total poisoning deaths); 2006, 10 (7.8%); P < 0.0001, Table 1]. The decline was predominantly seen in men [mean 2000–2004, 20 (19.4%); 2006, three (3.6%); P = 0.0001]. Female co-proxamol deaths also fell after legislation [mean 2000–2004, 17 (25.4%); 2006, seven (15.9%); P = 0.19].
Table 1.
Deaths in Scotland due to poisoning by all drugs and co-proxamol alone
| All poisoning deaths | Co-proxamol only deaths (±alcohol) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Male | Female | |||||||
| Total | Male | Female | n | (%)* | n | (%)* | n | (%)* | |
| 2000 | 160 | 103 | 57 | 37 | (23.1) | 21 | (20.4) | 16 | (28.1) |
| 2001 | 186 | 97 | 89 | 43 | (23.1) | 20 | (20.6) | 23 | (25.8) |
| 2002 | 179 | 113 | 66 | 39 | (21.8) | 20 | (17.7) | 19 | (28.9) |
| 2003 | 158 | 100 | 58 | 27 | (17.1) | 18 | (18.0) | 9 | (15.5) |
| 2004 | 173 | 103 | 70 | 41 | (23.7) | 21 | (20.4) | 20 | (28.6) |
| 2005 | 131 | 71 | 60 | 27 | (20.6) | 13 | (18.3) | 14 | (23.3) |
| 2006 | 128 | 84 | 44 | 10 | (7.8) | 3 | (3.6) | 7 | (15.9) |
Figures represent proportion of total poisoning deaths in Scotland.
The total number of poisoning deaths in Scotland also fell following co-proxamol legislation. This decline was observed from 2005, slightly earlier than the full impact on co-proxamol deaths [mean 2000–2004, 171.2; mean 2005–2006, 129.5; P = 0.005].
Analysing mortality according to location of death demonstrates that in the 5 years pre-legislation (2000–2004), there was a mean of 37 [95% confidence interval (CI) 29.7, 45.1] co-proxamol deaths per annum, of which 80.2% (mean 30, 95% CI 22.5, 37.4) occurred out of hospital. When compared with total out-of-hospital poisoning deaths in Scotland, legislation resulted in a significant reduction in the proportion due to co-proxamol, most evident in 2006 [mean 2000–2004, 30 (24.7%); 2005, 21 (22.8%); 2006, eight (8.2%); mean 2000–2004 vs. 2006, P = 0.0012]. This fall was reflected largely amongst male out-of-hospital deaths [mean 2000–2004, 17 (21.8%); 2006, two (2.9%); P < 0.0001]. Female out-of-hospital deaths also fell [mean 2000–2004, 13 (30.4%); 2006, six (20.7%); P = 0.39]. Similarly, there was a reduction in the small number of in-hospital co-proxamol deaths [mean 2000–2004, seven (14.6%); 2006, two (6.5%); P = 0.28].
When co-proxamol deaths were analysed according to age, prior to legislation (2000–2004), the average number of deaths per year by age group was: 10–34 years, 12; 35–54 years, 17; >54 years, nine. Despite the small numbers, a shift in age distribution of deaths was observed following legislation, particularly in younger patients (2006, 10–34 years, one; 35–54 years, four; >54 years, five).
Comparison of co-proxamol mortality with that of other common analgesics (Figure 1) illustrates both the excess mortality associated with co-proxamol prior to legislation, and the decline in mortality since its withdrawal. This has been associated with a sharp decline in the number of co-proxamol prescriptions [mean of six quarters pre-legislation change (July 2003 to December 2004) 300 555 prescriptions/quarter; third quarter 2006/2007 35 855 items, Figure 2]. A steady increase in the number of paracetamol and cocodamol prescriptions has occurred over the same period.
Figure 1.
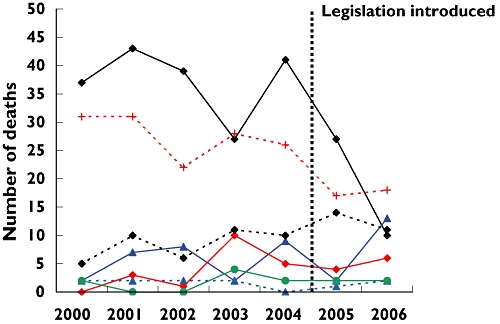
Scottish mortality figures from poisoning with commonly prescribed analgesics. Coproxamol, ( ); co-codamol, (
); co-codamol, ( ); codydramol, (
); codydramol, ( ); tramadol, (
); tramadol, ( ); dihydrocodeine, (
); dihydrocodeine, ( ); codeine, (
); codeine, ( ); paracetamol, (
); paracetamol, ( )
)
Figure 2.
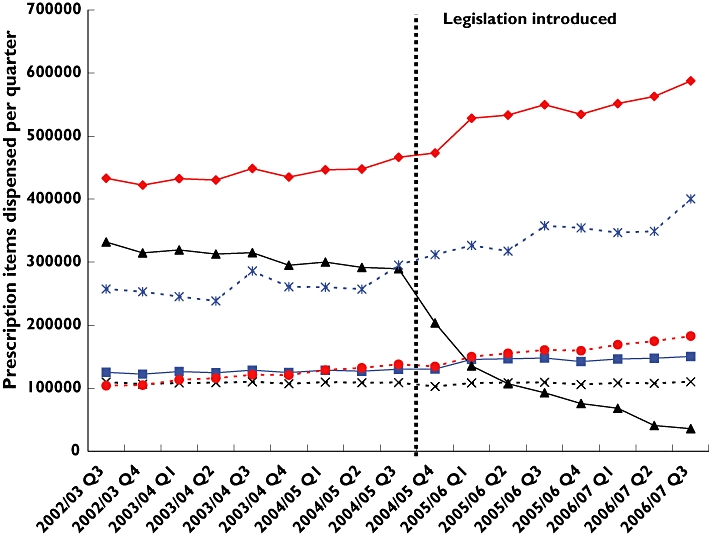
Quarterly prescription data for common analgesics in Scotland. Cocodamol, ( ); codydramol, (
); codydramol, ( ); coproxamol, (
); coproxamol, ( ); dihydrocodeine, (
); dihydrocodeine, ( ); paracetamol, (
); paracetamol, ( ); tramadol, (
); tramadol, ( )
)
Discussion
Legislation on co-proxamol availability has reduced mortality associated with co-proxamol poisoning in Scotland. This is important, as the effect of co-proxamol in overdose has contributed to influencing legislative change. Unusually, a phased withdrawal period over 2 years was undertaken to allow time for treatment adjustment, as co-proxamol was previously so widely used. While the number of co-proxamol prescriptions fell by approximately 60% within 6 months of legislation, and a downward change in mortality was observed in 2005, a significant effect on the number of co-proxamol deaths was not observed until 2006. Although immediate removal of co-proxamol would probably have been associated with a more rapid decline in mortality, it would have had significant implications for both patients and health professionals, as there were more than 1.1 million prescriptions in Scotland in 2004 alone. Nevertheless, demonstration of mortality reduction within a relatively short period, occurring in parallel to the prescription change, is an important finding and has implications for any future legislative decisions surrounding medication withdrawal.
Legislation appears to have had a marked effect in reducing out-of-hospital co-proxamol deaths, where the majority are known to occur [5]. Although a reduction was observed in the number of in-hospital deaths, the overall numbers were small. Similarly, although initial data suggest a greater reduction in male co-proxamol deaths, the numbers were small, and we would expect both male and female deaths to continue to decline following complete removal of co-proxamol. With respect to age, small numbers made statistical analysis difficult, but the number of deaths fell particularly among younger patients, who more frequently take impulsive overdoses of medication generally available in the household [7].
Deaths involving co-proxamol in a mixed overdose were excluded. While these figures may also have changed following legislation, it is often difficult to establish the precise cause of death where more than one agent is involved. Through isolating deaths involving only co-proxamol, a more focused and cogent dataset is presented.
The rapid decline in prescription items for co-proxamol has been associated with a steady rise in the number of cocodamol and paracetamol prescriptions (Figure 2). The total number of analgesic prescription items has remained relatively constant during this time [mean nine quarters pre-legislation (October 2002 to December 2004) 1 364 387 items; mean eight quarters post-legislation (January 2005 to December 2006) 1 393 478 items], suggesting that the increase in cocodamol and paracetamol prescriptions has compensated for the withdrawal of co-proxamol.
A concern following legislation was that the withdrawal of co-proxamol would lead to alternative agents being used as a means of suicide. The data shown here indicate that this is so far not the case, with mortality associated with other commonly prescribed analgesics remaining constant. Despite the steady rise in cocodamol and paracetamol prescriptions since legislation (Figure 2), there is no evidence of an increase in mortality associated with poisonings from these medications, or any other common analgesics (Figure 1). A significant fall in the total number of poisoning deaths in Scotland was observed following co-proxamol legislation. To what extent this is as a result of the reduction in co-proxamol deaths, however, is unclear, as total poisoning deaths began to fall from 2005, earlier than the full impact on co-proxamol deaths.
The data highlight the effect of legislation in reducing co-proxamol deaths in Scotland. Hawton et al. have demonstrated an annual mortality of 255 deaths associated with co-proxamol poisoning in England and Wales (1997–1999) [3]. If the epidemiology across England and Wales is similar to that in Scotland, we estimate that around 300 lives per annum in the UK will have been saved by the withdrawal of co-proxamol.
In conclusion, legislation on co-proxamol availability was implemented due to poorly established efficacy and risk of toxicity in overdose [8]. The Scottish data shown here demonstrate the significant impact this has had in reducing the number of deaths from co-proxamol poisoning, and its likely effect across the UK. Although initial data appear to refute concern regarding a compensatory rise in mortality from other analgesics, a longer period of observation is required to ensure that this remains the case. This will also allow greater appreciation of the effect on total poisoning deaths in Scotland.
Competing interests
None declared.
Acknowledgments
The authors thank Mr Iain Bishop (Principal Pharmacist, NHS National Services Scotland) and Dr D. Crookes (Lothian Health) for prescription data and helpful discussion. Graham Jackson of GRO kindly provided the mortality data.
REFERENCES
- 1.Afshari R, Good AM, Maxwell SRJ, Bateman DN. Co-proxamol overdose is associated with a 10-fold excess mortality compared with other paracetamol combination analgesics. Br J Clin Pharmacol. 2005;60:444–7. doi: 10.1111/j.1365-2125.2005.02468.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Wan PA, Zhang WY. Systematic overview of co-proxamol to assess analgesic effects of addition of dextropropoxyphene to paracetamol. BMJ. 1997;315:1565–71. doi: 10.1136/bmj.315.7122.1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawton K, Simkin S, Deeks J. Co-proxamol and suicide: a study of national mortality statistics and local non-fatal self poisonings. BMJ. 2003;326:1006–8. doi: 10.1136/bmj.326.7397.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Afshari R, Maxwell S, Dawson A, Bateman DN. ECG abnormalities in co-proxamol (paracetamol/dextropropoxyphene) poisoning. Clin Toxicol. 2005;43:255–9. [PubMed] [Google Scholar]
- 5.Whittington RM. Dextropropoxyphene deaths: a coroner's report. Hum Toxicol. 1984;3(Suppl):175S–185S. doi: 10.1177/096032718400300116. [DOI] [PubMed] [Google Scholar]
- 6.Bateman DN, Afshari R. Co-proxamol and suicide: licence needs to be changed. BMJ. 2003;327:287. doi: 10.1136/bmj.327.7409.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hawton K, Simkin S, Gunnell D, Sutton L, Bennewith O, Turnbull P, Kapur N. A multicentre study of coproxamol poisoning suicides based on coroners' records in England. Br J Clin Pharmacol. 2005;59:207–12. doi: 10.1111/j.1365-2125.2004.02252.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Medicines and Healthcare products Regulatory Agency. Coproxamol to be withdrawn from the market. Available at http://www.mhra.gov.uk/Safetyinformation/Safetywarningsalertsandrecalls/Safetywarningsandmessagesformedicines/CON1004254 (last accessed 31 January 2005.


