Abstract
Internal fixation of a traumatic osteochondral defect presents a challenge in terms of obtaining anatomic reduction, fixation, and adequate compression for healing. Fixation with countersunk intraarticular screws, Herbert screws, bioabsorbable screws and pins, mini-cancellous screws, and glue tissue adhesive have been reported with varying results. We present an alternative fixation method used in two patients for femoral condylar defects that achieved anatomic reduction with compression via a cruciate-shaped suture bridge construct tied down over a bony bridge. This fixation method allowed early passive range of motion and permitted high-quality MRI for followup of fracture healing and articular cartilage integrity. Arthroscopic examination of one of two patients at 6 months followup showed the gross appearance of a healed, anatomically reduced fracture. With 1 year followup for one patient and 2 years for the other, the patients have resumed activity as tolerated with full, painless range of motion at the knee. Longer-term outcomes are unknown. However, the suture bridge is an alternative means of fixation with encouraging early results for treatment of traumatic osteochondral fragments in the knee.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Traumatic osteochondral fractures of the femoral condyles are uncommon injuries that pose a challenge in terms of successful reduction and maintenance of fixation. Displacement can occur in the form of translation and/or rotation in three planes (axial, sagittal, coronal), and the fragment may be severed completely from its condylar base and become entrapped elsewhere in the gutters of the joint. For a displaced fragment and subsequent loose body, many surgeons recommend operative treatment.
Much of the literature regarding traumatic osteochondral fragments involves patellar and lateral femoral condylar lesions seen after acute patellar dislocation. Historically, traumatic osteochondral fragments were excised [1, 17, 19, 25, 26, 28], although replacement and fixation of osteochondral fragments have been recommended when adequate subchondral bone remains [26].
Open, mini-open, and arthroscopically assisted fixation techniques have been described [3, 4, 7–9, 11, 12, 15–20, 25, 26, 28, 31–35]. Arthroscopically assisted procedures allow documentation of concomitant injury and direct observation of articular reduction with minimal trauma to the local soft tissues. Successful fixation with subsequent healing of lateral femoral condyle osteochondral fragments has been reported with the use of countersunk intraarticular screws [35], Herbert screws [16, 20], and bioabsorbable screws [18] and pins [3, 7]. Fixation of the rare traumatic medial femoral osteochondral lesion has been reported with mini-cancellous screws [2]. Traumatic medial lesion fixation with glue tissue adhesive was reported by Gul et al. [9], with complete healing documented at 6 months followup and a functional knee score of 90 (Knee Society Clinical Rating System).
We describe an alternative treatment, applying a new fixation technique described recently for a shear fracture of the capitellum [30], of a completely displaced traumatic osteochondral fracture of either the medial or lateral femoral condyles. A suture bridge fixation technique is used to anatomically reduce the fragment, ensure rotational stability, compress the defect into its subchondral base allowing for fragment healing, and provide secure enough fixation to allow immediate passive motion. In addition, the use of biodegradable sutures allows evaluation of the lesion with MRI after surgery and healing of the osteoarticular fragment with dissolution of the absorbable sutures. We treated two patients, one with a lateral femoral condyle injury and the other with a medial femoral condyle injury, with this technique. This is the first description of a suture bridge fixation successfully and reproducibly applied in a weightbearing joint, where osteochondral injuries are treated more commonly than other joints.
Materials and Methods
We used standard anteromedial and anterolateral arthroscopy portals. The fracture fragment was identified and inspected. We consider a fragment amenable to fixation if it has intact, undamaged, full-thickness articular cartilage attached to a small amount of nonsclerotic subchondral bone.
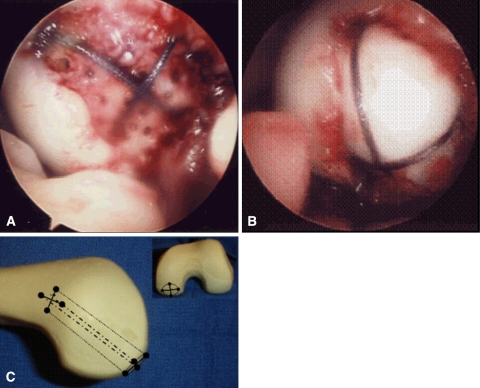
We removed fibrous tissue from the subchondral defect in the femoral condyle using a curette. Multiple perforations were made in the defect with a 1.5-mm drill bit. A 3-cm subvastus incision was made on the respective side of the defect to observe the cortical bone overlying the epicondyle. If an osteochondral fragment is too large to retrieve through the arthroscopy portal, it can be removed through this arthrotomy. Osseous tunnels were drilled with a Beath pin in a retrograde fashion beginning intraarticularly at the defect on the femoral condyle and through the anteromedial or anterolateral femoral cortices exposed through the subvastus incision. Four drill holes were made at opposing quadrants on the edge of the lesion. In this fashion, two Number 1 dyed, braided absorbable sutures (Ethicon Vicryl suture, Johnson & Johnson, Piscataway, NJ) were passed to create a cruciform configuration for subsequent fixation of the osteochondral fragment (Fig. 1A). A Hewson suture passer was used to pass the suture limbs over the bony bridge exposed through the subvastus incision.
Fig. 1A–C.
Arthroscopic images and a sawbones diagram of suture bridge fixation of a medial femoral condyle osteoarticular fracture are shown. (A) The base of the defect is drilled to stimulate progenitor cell migration. A Beath pin is used to drill four tunnels in a retrograde fashion from the opposing quadrants of the articular surface of the lesion to the medial distal femoral cortex. Braided absorbable suture is passed with a Hewson suture passer, and (B) the limbs of the sutures are tensioned around the fragment to reduce it to the condyle. After fragment stability and fluid joint motion are verified, the limbs of the suture bridge are tied down over the medial, nonarticular distal femoral cortex to secure the fragment. (C) On a sawbones model, the osteochondral fracture fragment is outlined as a circular lesion on the medial distal femur. The solid circles represent entrance and exit holes drilled with the Beath pin. One suture and its transosseous trajectory are represented by a small dashed line and the other by a larger dash. For each suture, small arrowheads represent suture knots tied down over a bony bridge.
The osteochondral fragment then was replaced in the defect under the braided absorbable sutures with proper fragment orientation (Fig. 1B). The sutures were provisionally tensioned to assess fragment conformity with the femoral articular surface and fragment stability through a full range of passive knee motion. The braided absorbable sutures were tied securely over the anterior femoral cortex (Fig. 1C) and fibrin glue was applied to the rim of the defect. The arthrotomy and subvastus incision were closed in layers and a soft dressing was applied to the knee.
Postoperatively, our two patients remained nonweightbearing for 8 weeks. Quadriceps isometric strengthening and full range of continuous passive motion were initiated immediately after surgery. Formal outpatient physical therapy was delayed until 8 weeks after surgery. Weightbearing was resumed after 8 weeks as the pain subsided and fixation and healing of the fracture were verified by plain films and MRI. On plain films we looked for restoration of the subchondral bone, absence of lucency in the cancellous bone, and absence of sclerosis of the immediate subchondral bone. We presumed resolution of bony edema on MRI indicated healing.
Case Reports
The first patient was a 19-year-old man who presented with pain, swelling, and instability after a twisting and hyperextension injury to his right knee and subsequent fall. Physical examination 10 days after the incident revealed a large effusion, motion limited from lacking 10° extension to 90° flexion, and tenderness to palpation over the lateral joint line anteriorly. Magnetic resonance images showed an osteochondral fracture of the lateral femoral condyle. At the time of surgery, the 2- × 3-cm defect was identified in the central, weightbearing portion of the lateral femoral condyle, and the loose fragment was located in the suprapatellar pouch. The fragment was prepared and fixation was performed via the described suture bridge compression technique. Postoperative management progressed as described. Radiographic images confirmed the fragment remained in its reduced position, and restoration of articular congruity was verified by followup MRI. By the third month, examination revealed full active and passive range of motion and no joint-line tenderness; at this point, the patient was allowed to progress with weightbearing. At 12 months followup, the patient maintained full, painless range of motion and had resumed full activities.
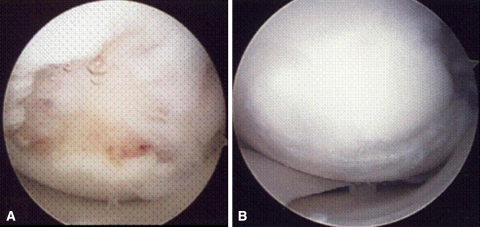
The second patient was a 25-year-old woman who presented 3 weeks after a forceful hyperextension injury to her left knee. Physical examination revealed a markedly antalgic gait, guarding, and diffuse joint-line tenderness medially and anteromedially. There was an appreciable effusion and passive range of motion lacking 30° extension to 90° flexion. Orthogonal radiographic images revealed an osteochondral defect in the medial femoral condyle. Magnetic resonance imaging and subsequent arthroscopic evaluation (Fig. 2A) showed a 2- × 2-cm defect in the central aspect of the weightbearing portion of the medial femoral condyle with a 7-mm depth into subchondral bone. The corresponding loose fragment was located in the medial gutter. Again, a suture bridge fixation was used to achieve anatomic reduction and compression of the fragment, and the described postoperative protocol was used. Six months after the index procedure, the patient reported having a mechanical click in her knee. She returned for a second-look arthroscopy, and inspection of the medial compartment revealed congruity of the distal femoral articular surface with the exception of a subtle incongruency posteriorly with surrounding fibrocartilage overgrowth (Fig. 2B). The osteochondral fragment was probed and seemingly had the gross mechanical properties of normal articular cartilage with a surrounding rim of fibrocartilage at the fracture edge. The fragment was stable circumferentially. A small amount of frayed fibrocartilaginous tissue at the posterior aspect of the lesion was smoothed down with an arthroscopic shaver, as was the posterior aspect of the healed osteochondral fragment margin where some mild incongruity was noted. There were no appreciable articular changes on the tibia. The knee was examined again through a range of motion with no more evidence of mechanical clicking. Eighteen months after the second-look arthroscopy and 24 months after the index procedure, the patient reported no pain with range of motion and participated in full activities.
Fig. 2A–B.
Photographs of Patient 2 reveal (A) an osteochondral defect in the medial femoral condyle at initial arthroscopy. Stable reduction was performed via suture bridge fixation, and (B) 6 months later, healing of the osteochondral fragment is verified during a second-look arthroscopy.
Discussion
Traumatic osteochondral fractures of the distal femoral condyle are uncommon, and medial femoral condylar involvement is rare. These injuries were likely the sequela of a shear moment generated as the knee was forced into hyperextension, and the distal femur impacted the tibial plateau. Magnetic resonance imaging is the preferred study when evaluating osteochondral injury [21, 22, 24, 27], although when adequate bone remains attached to the fragment for internal fixation, the fragment, defect, or both may be identified by plain films or computed tomography. An actual fracture should be differentiated from osteochondritis dissecans by the acuity and history of antecedent trauma; the involved tissues in an acute fracture are presumably nonpathologic and potentially more amenable to fixation.
Although historically such fragments were treated by excision [1, 17, 19, 25, 26], the traumatic nature of the injury may contribute to an environment conducive to healing when fixation is attempted acutely. Fixation of the fragment has the advantage of restoring a congruent surface with viable articular cartilage. Internal fixation requires that a sufficient amount of bone remains attached to the osteochondral fragment; without such a bony platform, the articular cartilage will not be reincorporated into the femoral condyle. Bone-to-bone healing can provide for stability of the cartilaginous island, and a fibrocartilaginous rim may effectively seal the cartilage surface [5, 6, 8, 11, 12, 28, 31–33]. Although we have not attempted fixation of nontraumatic osteochondritis dissecans lesions with this construct, we anticipate that this technique would be amenable only with a lesion with sufficient, viable, nonsclerotic subchondral bone remaining on the undersurface of the lesion.
The goals of fixation are to restore the articular surface congruity, provide compression of the fragment to allow osseous healing between the fragment and the femoral condyle, and ensure rotational stability to allow immediate range of motion. Presumably the edges of the reconstruction occur by fibrocartilage connection to adjacent normal cartilage; however, we have no good method to assess such repair. Screw or pin fixation has been described for fixation of these lesions [3, 7, 16, 18, 20, 35]. The advantage of using specially designed chondral darts or pins is that they are bioabsorbable and allow postoperative MRI without the need for implant removal. When multiple pins or chondral darts are used, rotational stability may be obtained, but compression of the lesion is compromised. The use of screws allows immediate compression and rotational stability if more than one screw is used. However, compression initially obtained by bioabsorbable screws has been observed to dissipate rapidly, within four days of placement, presumably owing to stress relaxation [10, 15]. Fragmentation of smaller osteochondral lesions is possible during screw insertion, and MRI postoperatively is marred by artifact. Finally, screw or pin fixation can lead to abrasive wear of the articulating surface and may necessitate future surgery for hardware removal [14].
In contrast, the suture bridge fixation technique we described combines the principles of lesion compression, immediate stability allowing range of motion, an absence of abrasive implants, and the ability to perform postoperative MRI. Sodl et al. described the use of this technique for an acute osteochondral shear fracture of the capitellum [30], however, this is the first report of its successful application, with reproducible results, in a lower-extremity, weightbearing joint, where osteochondral injuries are more common. Suture fixation of traumatic osteochondral patella fractures involving the articulating weightbearing surface also was described [4, 23]. In six cases described by Pritsch et al. [23], three holes were drilled in a triangular configuration and two suture limbs were passed through each hole to reduce the patella fragment with a parachute configuration.
Heavy braided absorbable suture is suitable for suture bridge fixation because it undergoes minimal absorption for the first 40 days [13], maintaining compression of the fragment for as much as 6 weeks. The suture then undergoes rapid and complete resorption by 56 to 70 days [13], in time for resumption of weightbearing, and eliminating any need for hardware removal. Nonetheless, before degradation, the sutures remain low profile enough such that the fragment is secured without blocking range of motion or causing abrasion to adjacent intraarticular structures.
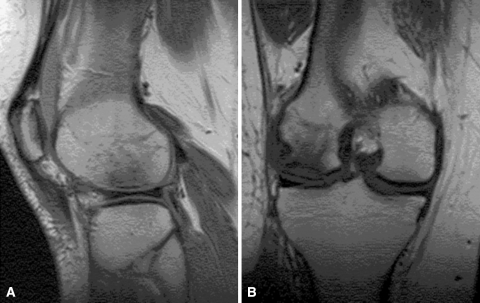
One year after his surgery, the first patient has fully recovered and followup imaging shows a healed fracture (Fig. 3). The second patient’s most recent MRI obtained at 8 months followup again showed restored articular congruity (Fig. 4). At 18 months followup, she has recovered from the second-look arthroscopy in which fragment position and healing were verified. Both patients remain weightbearing as tolerated with full, painless range of motion at the knee. Their long-term courses will be followed to monitor for posttraumatic arthritis.
Fig. 3A–B.
(A) Sagittal and (B) coronal MR images of Patient 1 at 4 months after surgery show a healed fracture with restoration of the articular surface.
Fig. 4A–B.
(A) Sagittal and (B) coronal MR images of Patient 2 at 8 months after surgery show adequate alignment of the healed fracture.
There are a few caveats to observe when performing this procedure. More patients and additional followup are needed to ultimately verify the safety or efficacy of this approach. Although neither of our patients experienced injury to the common peroneal or saphenous nerves, fragmentation of the bony bridge, or premature suture failure, these are theorized as potential complications. Should abrasion damage to the suture occur before fracture healing is complete, there is a theoretic risk of fracture displacement and consequent intraarticular damage. For this reason we recommend enforcement of strict nonweightbearing until at least 8 weeks after surgery and radiographic verification of bony healing.
We have presented a suture bridge fixation technique based on the principles of repair of traumatic osteoarticular fragments. The suture bridge fixation provides compression and rotational stability and, unlike fixation with pins or screws, obviates the risk for mechanical abrasion of articulating surfaces and the need for hardware removal. Using sutures, rather than pins or screws, allows for high-quality MRI after fixation. The suture bridge is a viable alternative to other accepted means of fixation, including screw fixation and bioabsorbable darts, for treatment of traumatic osteochondral fragments in the knee.
Acknowledgments
We thank Stephanie Robinson for clerical assistance.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Ahstrom JP Jr. Osteochondral fracture in the knee joint associated with hypermobility of the patella: report of eighteen cases. J Bone Joint Surg Am. 1965;47:1491–1502. [PubMed]
- 2.Binnet MS, Gurkan I, Karakascedil A, Yilmaz C, Erekul S, Cetin C. Histopathologic assessment of healed osteochondral fractures. Arthroscopy. 2001;17:278–285. [DOI] [PubMed]
- 3.Braune C, Rehart S, Kershbaumer F, Jager A. [Resorbable pin refixation of an osteochondral fracture of the lateral femoral condyle due to traumatic patellar dislocation: case management, follow-up and strategy in adolescents][in German]. Z Orthop Ihre Grenzgeb. 2004;142:103–108. [DOI] [PubMed]
- 4.Dhawan A, Hospodar PP. Suture fixation as a treatment for acute traumatic osteochondral lesions. Arthroscopy. 1999:15:307–311. [DOI] [PubMed]
- 5.Frisbie DD, Oxford JT, Southwood L, Trotter GW, Rodkey WG, Steadman JR, Goodnight JL, McIlwraith CW. Early events in cartilage repair after subchondral bone microfracture. Clin Orthop Relat Res. 2003;407:215–227. [DOI] [PubMed]
- 6.Frisbie DD, Trotter GW, Powers BE, Rodkey WG, Steadman JR, Howard RD, Park RD, McIlwraith CW. Arthroscopic subchondral bone plate microfracture technique augments healing of large chondral defects in the radial carpal bone and medial femoral condyle of horses. Vet Surg. 1999;28:242–255. [DOI] [PubMed]
- 7.Fuchs M, Vosshenrich R, Dumont C, Sturmer KM. [Refixation of osteochondral fragments using absorbable implants: first results of a retrospective study][in German]. Chirurg. 2003;74:554–561. [DOI] [PubMed]
- 8.Gobbi A, Nunag P, Malinowski K. Treatment of full thickness chondral lesions of the knee with microfracture in a group of athletes. Knee Surg Sports Traumatol Arthrosc. 2005;13:213–221. [DOI] [PubMed]
- 9.Gul R, Khan F, Maher Y, O’Farrell D. Osteochondral fractures in the knee treated with butyl-2-cyanoacrylate glue: a case report. Acta Orthop Belg. 2006;72:641–643. [PubMed]
- 10.Hofmann GO, Wagner FD. New implant designs for bioresorbable devices in orthopaedic surgery. Clin Mater. 1993;14:207–215. [DOI] [PubMed]
- 11.Kish G, Modis L, Hangody L. Osteochondral mosaicplasty for the treatment of focal chondral and osteochondral lesions of the knee and talus in the athlete: rationale, indications, techniques, and results. Clin Sports Med. 1999;18:45–66, vi. [DOI] [PubMed]
- 12.Knutsen G, Engebretsen L, Ludvigsen TC, Drogset JO, Grontvedt T, Solheim E, Strand T, Roberts S, Isaksen V, Johansen O. Autologous chondrocyte implantation compared with microfracture in the knee: a randomized trial. J Bone Joint Surg Am. 2004;86:455–464. [DOI] [PubMed]
- 13.Lai SY, Becker DG. Sutures and needles. E-medicine.com. Available at: http://www.emedicine.com/ent/topic38.htm. Accessed January 7, 2008.
- 14.Lange RH, Vanderby R Jr, Engber WD, Glad RW, Purnell ML. Biomechanical and histological evaluation of the Herbert screw. J Orthop Trauma. 1990;4:275–282. [DOI] [PubMed]
- 15.Larsen MW, Pietrzak WS, DeLee JC. Fixation of osteochondritis dissecans lesions using poly(l-lactic acid)/poly(glycolic acid) copolymer bioabsorbable screws. Am J Sports Med. 2005;33:68–76. [DOI] [PubMed]
- 16.Lewis PL, Foster BK. Herbert screw fixation of osteochondral fractures about the knee. Aust NZ J Surg. 1990;60:511–513. [DOI] [PubMed]
- 17.Makin M. Osteochondral fracture of the lateral femoral condyle. J Bone Joint Surg Am. 1951;33:262–264. [PubMed]
- 18.Mashoof AA, Scholl MD, Lahav A, Greis PE, Burks RT. Osteochondral injury to the mid-lateral weight-bearing portion of the lateral femoral condyle associated with patella dislocation. Arthroscopy. 2005;21:228–232. [DOI] [PubMed]
- 19.Matthewson MH, Dandy DJ. Osteochondral fractures of the lateral femoral condyle: a result of indirect violence to the knee. J Bone Joint Surg Br. 1978;60:199–202. [DOI] [PubMed]
- 20.Mbubaegbu CE, Percy AJ. Femoral osteochondral fracture: a non-contact injury in martial arts? A case report. Br J Sports Med. 1994;28:203–205. [DOI] [PMC free article] [PubMed]
- 21.Potter HG, Foo LF. Magnetic resonance imaging of articular cartilage: trauma, degeneration, and repair. Am J Sports Med. 2006;34:661–677. [DOI] [PubMed]
- 22.Potter HG, Linklater JM, Allen AA, Hannafin JA, Haas SB. Magnetic resonance imaging of articular cartilage in the knee: an evaluation with use of fast-spin-echo imaging. J Bone Joint Surg Am. 1998;80:1276–1284. [DOI] [PubMed]
- 23.Pritsch M, Velkes S, Levy O, Greental A. Suture fixation of osteochondral fractures of the patella. J Bone Joint Surg Br. 1995:77:154–155. [PubMed]
- 24.Recht M, Bobic V, Burstein D, Disler D, Gold G, Gray M, Kramer J, Lang P, McCauley T, Winalski C. Magnetic resonance imaging of articular cartilage. Clin Orthop Relat Res. 2001;391(suppl):S379–S396. [DOI] [PubMed]
- 25.Rorabeck C, Bobechko W. Acute dislocation of the patella with osteochondral fracture: a review of eighteen cases. J Bone Joint Surg Br. 1976;58:237–240. [DOI] [PubMed]
- 26.Rosenberg NJ. Osteochondral fractures of the lateral femoral condyle. J Bone Joint Surg Am. 1964;46:1013–1026. [PubMed]
- 27.Shindle MK, Foo LF, Kelly BT, Khanna AJ, Domb BG, Farber A, Wanich T, Potter HG. Magnetic resonance imaging of cartilage in the athlete: current techniques and spectrum of disease. J Bone Joint Surg Am. 2006;88(suppl 4):27–46. [DOI] [PubMed]
- 28.Sledge SL. Microfracture techniques in the treatment of osteochondral injuries. Clin Sports Med. 2001;20:365–377. [DOI] [PubMed]
- 29.Smillie IS. Osteochondritis Dissecans. Loose Bodies in Joints: Etiology, Pathology, Treatment. Baltimore, MD: The Williams and Wilkins Co; 1960.
- 30.Sodl JF, Ricchetti ET, Huffman GR. Acute osteochondral shear fracture of the capitellum in a 12-year-old patient: a case report. J Bone Joint Surg Am. 2008;90:629–633. [DOI] [PubMed]
- 31.Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG. Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy. 2003;19:477–484. [DOI] [PubMed]
- 32.Steadman JR, Miller BS, Karas SG, Schlegel TF, Briggs KK, Hawkins RJ. The microfracture technique in the treatment of full-thickness chondral lesions of the knee in National Football League players. J Knee Surg. 2003;16:83–86. [PubMed]
- 33.Steadman JR, Rodkey WG, Rodrigo JJ. Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res. 2001;391(suppl):S362–S369. [DOI] [PubMed]
- 34.Steadman JR, Rodkey WG, Singleton SB, Briggs KK. Microfracture technique for full-thickness chondral defects: technique and clinical results. Oper Tech Orthop. 1997;7:300–304. [DOI]
- 35.Taitsman LA, Frank JB, Mills WJ, Barei DP, Nork SE. Osteochondral fracture of the distal lateral femoral condyle: a report of two cases. J Orthop Trauma. 2006;20:358–362. [DOI] [PubMed]