Abstract
We report a case of meralgia paresthetica occurring in an amateur baseball pitcher who experienced inguinal pain and dysesthesia in the anterolateral thigh during pitching practice. The lateral femoral cutaneous nerve was pushed up by the iliac muscle to the inguinal ligament at the sharp ridge of its fascia and ensheathed in the tendinous origin of the sartorius muscle. Neurolysis of the lateral femoral cutaneous nerve and partial dissection of the inguinal ligament and sartorius muscle promptly relieved the symptoms and the patient resumed pitching 1 month later. These anatomic variations of the lateral femoral cutaneous nerve in the inguinal region might render the nerve susceptible to compression and irritation, and repetitive contraction of inguinal muscles during throwing motion might induce and exacerbate the neuropathy of the lateral femoral cutaneous nerve.
Introduction
Meralgia paresthetica (MP) is an entrapment neuropathy of the lateral femoral cutaneous nerve (LFCN) that is characterized by pain and dysesthesia in the lateral thigh. Numerous reports describe its etiology and treatment [1–15]. In some reports, the condition has occurred in relation to sports activity [7, 10, 11, 14]. We report a case of MP occurring in an amateur baseball pitcher as a result of throwing.
Case Report
A 23-year-old male, left-hand–dominant, amateur baseball pitcher experienced right inguinal pain and dysesthesia in the anterolateral thigh during pitching practice. The symptoms persisted approximately 1 year and gradually worsened 2 months before he was seen by us. At the time of examination, the patient had local tenderness just medial to the anterior superior iliac spine (ASIS), where the LFCN passes under the inguinal ligament, and Tinel’s test of the LFCN exacerbated the pain, which radiated to the anterolateral thigh. There was partial loss of sensation in the upper part of the anterolateral thigh, but no other neurologic findings. We identified no abnormal findings on plain radiographs of the pelvis and lumbar spine.
Meralgia paresthetica was suspected based on the history and clinical findings. To confirm the diagnosis, we performed a local anesthetic nerve block of the LFCN. A local anesthetic agent with corticosteroid was injected just medial to the ASIS where the local tenderness was noted. All symptoms resolved immediately after the nerve block, but the effect lasted only a few hours. Because several repeated local corticosteroid injections, oral administration of nonsteroidal antiinflammatory drugs, and various physical therapies did not produce adequate pain relief, we performed surgical exploration of the LFCN one month after the patient’s initial visit to our hospital.
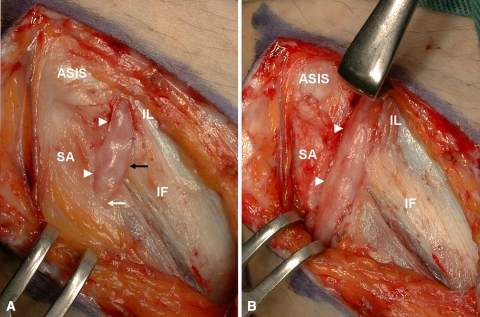
We made an S-shaped incision in the inguinal region over the point of maximal tenderness. The LFCN was pushed up and kinked by the sharp ridge on the lateral edge of the iliac fascia that resulted in a bow-string deformation of the nerve (Fig. 1A). The nerve also was ensheathed in the tendinous origin of the sartorius muscle just distal to the iliac fascia and irritated scar tissues were observed around the nerve. There were two indentations in the LFCN at the edge of the iliac fascia and the tendinous origin of the sartorius muscle, and neuroma formations (pseudoneuromas) were observed just proximal to the constriction sites. There was no constriction site proximal to the inguinal ligament. Neurolysis of the LFCN and partial excision of the sartorius fascia and inguinal ligament were performed (Fig. 1B). The symptoms resolved promptly after surgery. The patient was able to resume pitching a month later, and return to baseball game as a pitcher three months later with no recurrence of symptoms. Two years after surgery, the patient had no symptoms of MP.
Fig. 1A–B.
(A) The lateral femoral cutaneous nerve is pushed up and kinked by the sharp ridge of the iliac fascia (black arrow) and ensheathed in the tendinous origin of the sartorius muscle (white arrow). Two neuroma formations (pseudoneuromas) were observed just proximal to the constriction sites (white arrowhead). ASIS = anterior superior iliac spine; SA = sartorius muscle; IF = iliac fascia. (B) After neurolysis of the lateral femoral cutaneous nerve (LFCN) and partial dissection of the sartorius fascia and inguinal ligament, the LFCN can be seen clearly.
Discussion
Meralgia paresthetica was first described by Bernhardt [2] in 1878, and the term was adopted by Roth [13] in 1895. The term was derived from the Greek words “meros”, meaning thigh, and “algos”, meaning pain; thus, from its literal translation, the disease is characterized by pain in the thigh. Numerous clinical reviews have been published since the first reports by Bernhardt and Roth [3, 6, 8, 9, 10, 12, 15]. Various causes have been suggested, including trauma, orthopaedic procedures (such as iliac crest bone graft harvesting or pelvic osteotomy), obesity, pregnancy, and external compression from tight clothing. However, the cause of MP is considered idiopathic in most cases [1, 3, 10, 12, 14].
The LFCN is subject to compression throughout its entire course. Most commonly, the LFCN travels under the psoas major muscle and enters the thigh by crossing the groin under the inguinal ligament, after which it pierces the fascia lata and then divides into its anterior and posterior branches. Several anatomic variations of the LFCN have been described [1, 3, 5]. Ghent [5] described four anatomic variations of the LFCN that predispose to MP: Type 1, passage of the nerve through the classic split inguinal ligament; Type 2, bowstring deformation of the nerve as it crosses the iliac fascia; Type 3, passage of the nerve through the sartorius muscle; and Type 4, passage of the nerve crossing the iliac crest just behind the ASIS. In a cadaveric study of 200 specimens, de Ridder et al. [3] reported the LFCN was normal in 74% of subjects, but the remaining 26% had anatomic variations.
In our patient, the LFCN was pushed up by the sharp ridge of the iliac fascia (Ghent’s Type 2) and ensheathed in the tendinous origin of the sartorius muscle (Ghent’s Type 3). These anatomic variations of the LFCN in the inguinal region may render the nerve susceptible to compression. The findings of scar tissue around the nerve and the formation of pseudoneuromas support the possibility of repetitive compression of the LFCN.
Meralgia paresthetica has been reported as being related to sports activity [10, 11, 14]. In almost all cases, local soft tissue trauma to the upper anterolateral thigh is the main cause of MP. Kho et al. [7] reported the first three cases of MP resulting from strenuous exercise without any other possible cause such as trauma or exogenous compression. They hypothesized that the cause of MP was compression of the LFCN triggered by repetitive or continuous contraction and stretching of the iliopsoas muscle and the sartorius muscle in conjunction with anatomic abnormalities. Direct mechanical force on the nerve and secondary local ischemia to the nerve may induce neuropathy of the LFCN.
The inguinal muscles are very much involved during pitching motion. A pitcher lifts up his front foot in the windup phase and then strides toward the batter. At the time of foot landing, the front hip is deeply flexed with full weightbearing and is kept in this position up to the followthrough phase. During this time, the inguinal muscles, especially the iliac muscle, are contracting and pushing the LFCN up to the inguinal ligament. Simultaneously, the sartorius muscle is contracting and stretching, and the nerve might be irritated and constricted where it pierces the tendinous origin of the sartorius muscle. The LFCN may be repetitively strangulated and kinked at the inguinal canal every time the pitcher throws a ball.
Nonoperative treatment is generally effective for MP, and many cases resolve spontaneously with time. Williams and Trzil [15] reported a 90% resolution rate with nonoperative treatments such as nonsteroidal antiinflammatory drugs, various physical therapies, and local corticosteroid injection. We believe surgery should be considered only if nonoperative treatment does not provide adequate relief. In these patients, the possibility of anatomic variants of the LFCN should be considered. Several reports of surgical decompression suggest satisfactory results in almost all patients [4, 9, 12].
The diagnosis of MP depends on being cognizant of this entity, because the symptoms generate a low level of distress and are typically intermittent. Nevertheless, if undiagnosed, MP may lead to considerable distress and long-term disability [14]. Clinicians should consider this entity when athletes report anterolateral thigh symptoms. Atypical symptoms in the upper anterior thigh region should suggest the possibility of MP. If intractable pain persists and adversely affects performance despite nonoperative treatment, surgery should be considered to allow the patient to return to sports as soon as possible.
Acknowledgments
We thank Mitsuyoshi Uzawa, Giro Kuboi, Masafumi Saito, Hiroyuki Okada, Kouji Ugai, Kenji Oseki, Keio Ayabe, and Hideaki Imabayashi for assistance.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his institution has approved the reporting of these case reports, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Aszmann OC, Dellon ES, Dellon AL. Anatomical course of the lateral femoral cutaneous nerve and its susceptibility to compression and injury. Plast Reconstr Surg. 1997;100:600–604. [DOI] [PubMed]
- 2.Bernhardt M. Neuropathologische beobachtungen. I. Periphere Laglungen. D Arch Klin Med. 1878;22:362.
- 3.de Ridder VA, de Lange S, Popta JV. Anatomical variations of the lateral femoral cutaneous nerve and the consequences for surgery. J Orthop Trauma. 1999;13:207–211. [DOI] [PubMed]
- 4.Edelson R, Stevens P. Meralgia paresthetica in children. J Bone Joint Surg Am. 1994;76:993–999. [DOI] [PubMed]
- 5.Ghent WR. Further studies on meralgia paresthetica. Can Med Assoc J. 1961;85:871–875. [PMC free article] [PubMed]
- 6.Keegan JJ, Holyoke EA. Meralgia paresthetica: an anatomical and surgical study. J Neurosurg. 1962;19:341–345. [DOI] [PubMed]
- 7.Kho KH, Blijham PL, Zwarts MJ. Meralgia paresthetica after strenuous exercise. Muscle Nerve. 2005;31:761–763. [DOI] [PubMed]
- 8.Kitchen C, Simpson J. Meralgia paresthetica: a review of 67 patients. Acta Neurol Scand. 1972;48:547–555. [DOI] [PubMed]
- 9.Macnicol MF, Thompson WJ. Idiopathic meralgia paresthetica. Clin Orthop Relat Res. 1990;254:270–274. [PubMed]
- 10.Macrory P, Bell S. Nerve entrapment syndromes as a cause of pain in the hip, groin and buttock. Sports Med. 1999;27:261–274. [DOI] [PubMed]
- 11.McGregor J, Moncur JA. Meralgia paresthetica: a sports lesion in girl gymnasts. Br J Sports Med. 1977;11:16–19. [DOI] [PMC free article] [PubMed]
- 12.Nahabedian MY, Dellon AL. Meralgia paresthetica: etiology, diagnosis, and outcome of surgical decompression. Ann Plast Surg. 1995;35:590–594. [DOI] [PubMed]
- 13.Roth VK. Meralgia paresthetica. Meditsinskoye Obozrainie Moskova. 1895;42:678.
- 14.Ulkar B, Yildiz Y, Kunduracioglu B. Meralgia paresthetica: a long-standing performance-limiting cause of anterior thigh pain in a soccer player. Am J Sports Med. 2003;31:787–789. [DOI] [PubMed]
- 15.Williams PH, Trzil KP. Management of meralgia paresthetica. J Neurosurg. 1991;74:76–80. [DOI] [PubMed]