Abstract
We evaluated the activity of ceftobiprole against 100 community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) and 100 hospital-associated MRSA (HA-MRSA) isolates. Eight isolates were evaluated by time-kill studies for kill rate and potential for synergy with tobramycin. Ceftobiprole MIC50 and MIC90 values were 1 and 2 μg/ml, respectively, against CA-MRSA and HA-MRSA. In time-kill analysis, ceftobiprole was bactericidal at all concentrations tested.
Ceftobiprole is a new investigational broad-spectrum cephalosporin active against a wide range of gram-positive and gram-negative pathogens, including methicillin-resistant Staphylococcus aureus (MRSA) (1-3, 5, 7, 8). It accomplishes this through strong binding to and inhibition of penicillin binding protein 2A, the product of the mecA gene of MRSA (6). Two phase 3 clinical trials assessing efficacy and safety in patients with complicated skin and skin structure infections have demonstrated that ceftobiprole is not inferior to vancomycin for patients infected with gram-positive bacteria or to vancomycin plus ceftazidime for patients infected with gram-positive and gram-negative bacteria (10, 11). The objective of this investigation was to evaluate the activities of ceftobiprole, vancomycin, daptomycin, and linezolid and the potential for synergy between ceftobiprole and tobramycin against community-associated MRSA (CA-MRSA) and hospital-associated MRSA (HA-MRSA).
(A portion of this work was presented at the 47th Interscience Conference on Antimicrobial Agents and Chemotherapy, Chicago, IL, 2007 [7a].)
One hundred clinical CA-MRSA and 100 clinical HA-MRSA strains isolated from patients at the Detroit Medical Center and defined based on the Centers for Disease Control and Prevention clinical definitions were evaluated for susceptibilities. Determination of the staphylococcal cassette chromosome (SCCmec) type and identification of the genes coding for Panton-Valentine leukocidin were determined via multiplex PCR by a previously described method (9, 14). All isolates were characterized according to accessory gene regulator (agr) type by use of multiplex PCR and agr group-specific primers (12). The expression of the agr gene cluster was determined by quantifying delta-hemolysin production as previously described (13). Four of the CA-MRSA and four of the HA-MRSA strains were randomly selected for time-kill analysis.
MICs and minimum bactericidal concentrations (MBCs) of ceftobiprole (Johnson & Johnson Pharmaceutical Research & Development, Raritan, NJ), vancomycin (Sigma Chemical Company, St. Louis, MO), daptomycin (Cubist Pharmaceuticals, Lexington, MA), and linezolid (Pfizer Inc., New York, NY) were determined by broth microdilution, in duplicate, according to Clinical and Laboratory Standards Institute (CLSI) guidelines (4). Mueller-Hinton broth (Difco, Detroit, MI) supplemented with 25 mg/liter calcium and 12.5 mg/liter magnesium was used for all susceptibility testing and time-kill experiments except for those with daptomycin, where Mueller-Hinton broth was supplemented with 50 mg/liter calcium and 12.5 mg/liter magnesium. Daptomycin MIC determinations were performed in the presence of 50% human serum on 20 randomly chosen isolates. Aliquots (5 μl) from clear wells were plated onto tryptic soy agar for determination of MBCs.
Time-kill experiments were performed in triplicate using a starting inoculum of approximately 106 CFU/ml. Isolates were tested against ceftobiprole, vancomycin, linezolid, daptomycin, and daptomycin in the presence of 50% human serum at 4× the MIC. Aliquots (0.1 ml) were removed over 0 to 24 h and serially diluted in cold 0.9% sodium chloride. Additionally, all isolates were tested against ceftobiprole and tobramycin alone and in combination at 0.5× MIC and 1× MIC. Synergy was defined as a ≥2-log10-CFU/ml increase in killing at 24 h with the combination compared to what was seen for the most active single drug. Additivity was defined as a 1- to 2-log10-CFU/ml increase in killing compared to what was seen for the most active single agent. Indifference was defined as ±1-log10-CFU/ml killing or growth. Combinations resulting in ≥1-log10 growth compared to what was seen for the least active single agent were defined as antagonistic. Bacterial counts were determined using an automatic spiral plater (WASP; DW Scientific, West Yorkshire, England) and colonies were counted using the protocol colony counter (Synoptics Limited, Frederick, MD) with a lower limit of detection of 2 log10 CFU/ml. Time-kill curves were constructed by plotting the mean colony counts (log10 CFU/ml) versus time. Bactericidal activity was defined as a ≥3-log10-CFU/ml (99.9%) reduction from the starting inoculum. The time to 99.9% kill (T99.9) was determined by linear regression or visual inspection (if the R2 value was ≤0.95). Differences between CA- and HA-MRSA in susceptibility and in T99.9 values were compared by use of the Mann-Whitney U test and analysis of variance with Tukey's post hoc test. All statistical analysis was performed using SPSS statistical software (release 15.0; SPSS, Inc., Chicago, IL).
All of the CA-MRSA isolates were SCCmec type IV and 97% of the HA-MRSA isolates were SCCmec type II. The Panton-Valentine leukocidin genes were detected in 20% of HA-MRSA and 89% of CA-MRSA isolates. The HA-MRSA isolates were 74% agr group II and 41% had a dysfunctional agr locus, while the CA-MRSA isolates were 89% agr group I and all had a functional agr locus. Susceptibility results are shown in Table 1. There was no difference between CA-MRSA and HA-MRSA in susceptibility to ceftobiprole (P = 0.865). The addition of serum to daptomycin resulted either in no change or in a two- to fourfold increase in MIC.
TABLE 1.
Cumulative susceptibility results for 100 CA-MRSA and 100 HA-MRSA isolatesa
| Isolate type and drug | % of isolates susceptible at MIC of:
|
Concn (μg/ml)
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0.06 | 0.125 | 0.25 | 0.5 | 1 | 2 | 4 | MIC50 | MIC90 | MBC50 | MBC90 | MBC range | |
| CA-MRSA | ||||||||||||
| Ceftobiprole | 0 | 0 | 0 | 2 | 57 | 41 | 0 | 1 | 2 | 2 | 4 | 0.5-64 |
| Vancomycin | 0 | 0 | 1 | 12 | 79 | 8 | 0 | 1 | 1 | 1 | 2 | 0.5-2 |
| Linezolid | 0 | 0 | 0 | 0 | 5 | 79 | 16 | 2 | 4 | 8 | 32 | 2-64 |
| Daptomycin | 0 | 9 | 74 | 15 | 2 | 0 | 0 | 0.25 | 0.5 | 0.25 | 0.5 | 0.125-1 |
| Daptomycin + serum | 0 | 0 | 0 | 50 | 50 | 0 | 0 | 1 | 1 | 1 | 1 | 0.5-1 |
| HA-MRSA | ||||||||||||
| Ceftobiprole | 0 | 0 | 0 | 3 | 55 | 40 | 2 | 1 | 2 | 2 | 4 | 0.5-64 |
| Vancomycin | 1 | 0 | 0 | 7 | 58 | 34 | 0 | 1 | 2 | 1 | 2 | 0.5-8 |
| Linezolid | 0 | 0 | 1 | 3 | 6 | 70 | 20 | 2 | 4 | 16 | 64 | 1-64 |
| Daptomycin | 0 | 11 | 63 | 20 | 4 | 2 | 0 | 0.25 | 0.5 | 0.25 | 1 | 0.125-4 |
| Daptomycin + serum | 0 | 0 | 0 | 60 | 40 | 0 | 0 | 0.5 | 1 | 1 | 1 | 0.5-1 |
For daptomycin plus serum, there were 10 CA-MRSA and 10 HA-MRSA isolates.
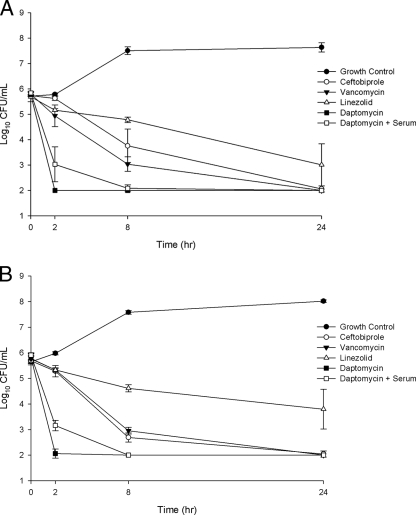
In the time-kill analysis, ceftobiprole was bactericidal and killed to detection limits (2 log10 CFU/ml) by 24 h. Kill rates (T99.9) were as follows: daptomycin (1.6 h) had a kill rate greater than that of daptomycin plus serum (2.2 h), which was greater than that of ceftobiprole (8 h), which was equal to that of vancomycin (8.6 h), which was greater than that of linezolid (did not reach 99.9% kill) (P < 0.001) against CA-MRSA; and daptomycin (1.6 h) had a kill rate greater than that of daptomycin plus serum (2.1 h), which was greater than that of vancomycin (8.6 h), which was greater than that of ceftobiprole (11.8 h), which was greater than that of linezolid (did not reach 99.9% kill) (P < 0.001) for HA-MRSA. Results are shown in Fig. 1. When ceftobiprole was combined with tobramycin, all isolates displayed indifference at 24 h. Ceftobiprole alone was bactericidal at both 1× and 0.5× the MIC. Although there was a trend toward slower killing at 0.5× MIC, there was no difference in bactericidal rates between ceftobiprole at 4× MIC, at 1× MIC (T99.9 = 8.6 h), or at 0.5× MIC (T99.9 = 14.2 h) (P = 0.172).
FIG. 1.
Time-kill curves for HA-MRSA (four isolates combined; mean ± standard deviation) (A) and CA-MRSA (four isolates combined; mean ± standard deviation) (B) versus ceftobiprole, vancomycin, linezolid, daptomycin, and daptomycin in the presence of (+) serum at 4× MIC.
Consistent with other investigations, we found ceftobiprole to be highly active against MRSA (3, 6, 7), with no differences in susceptibility seen for community or hospital origin. In time-kill analysis, ceftobiprole was persistently bactericidal to detection limits by 24 h. An interesting finding in our study was that ceftobiprole was bactericidal at 0.5× MIC. This is consistent with early results reported for the activity of ceftobiprole against S. aureus (6), which demonstrated significant killing of ceftobiprole against staphylococci at 0.5× MIC at an inoculum of ∼106 cells but no activity at an inoculum of ∼107. Other investigators have found that the combination of ceftobiprole with gentamicin showed indifference against three S. aureus isolates tested (5). However, they did find synergy with 2 of 7 coagulase-negative staphylococci and 5 of 10 enterococci.
In conclusion, we found ceftobiprole to be active against MRSA regardless of community or hospital origin. The addition of tobramycin did not enhance or diminish the bactericidal activity of ceftobiprole. Ceftobiprole was bactericidal against MRSA at all concentrations tested and represents a new alternative to vancomycin for the treatment of infections caused by MRSA.
Acknowledgments
This work was supported by Johnson & Johnson Pharmaceutical Research & Development. M.J.R. has received grant support from Johnson & Johnson Pharmaceutical Research & Development, Cubist, and Pfizer.
M.J.R. serves as a consultant and speaker for Ortho McNeil, Cubist, and Pfizer. S.N.L and C.M.C. have nothing to declare.
Footnotes
Published ahead of print on 2 June 2008.
REFERENCES
- 1.Arias, C. A., K. V. Singh, D. Panesso, and B. E. Murray. 2007. Time-kill and synergism studies of ceftobiprole against Enterococcus faecalis, including beta-lactamase-producing and vancomycin-resistant isolates. Antimicrob. Agents Chemother. 51:2043-2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bogdanovich, T., C. Clark, L. Ednie, G. Lin, K. Smith, S. Shapiro, and P. C. Appelbaum. 2006. Activities of ceftobiprole, a novel broad-spectrum cephalosporin, against Haemophilus influenzae and Moraxella catarrhalis. Antimicrob. Agents Chemother. 50:2050-2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bogdanovich, T., L. M. Ednie, S. Shapiro, and P. C. Appelbaum. 2005. Antistaphylococcal activity of ceftobiprole, a new broad-spectrum cephalosporin. Antimicrob. Agents Chemother. 49:4210-4219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clinical and Laboratory Standards Institute. 2006. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard, 7th ed. CLSI, Wayne, PA.
- 5.Deshpande, L. M., and R. N. Jones. 2003. Bactericidal activity and synergy studies of BAL9141, a novel pyrrolidinone-3-ylidenemethyl cephem, tested against streptococci, enterococci and methicillin-resistant staphylococci. Clin. Microbiol. Infect. 9:1120-1124. [DOI] [PubMed] [Google Scholar]
- 6.Hebeisen, P., I. Heinze-Krauss, P. Angehrn, P. Hohl, M. G. Page, and R. L. Then. 2001. In vitro and in vivo properties of Ro 63-9141, a novel broad-spectrum cephalosporin with activity against methicillin-resistant staphylococci. Antimicrob. Agents Chemother. 45:825-836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones, R. N., L. M. Deshpande, A. H. Mutnick, and D. J. Biedenbach. 2002. In vitro evaluation of BAL9141, a novel parenteral cephalosporin active against oxacillin-resistant staphylococci. J. Antimicrob. Chemother. 50:915-932. [DOI] [PubMed] [Google Scholar]
- 7a.Leonard, S. N., C. M. Cheng, and M. J. Rybak. 2007. In vitro activity of ceftobiprole (CEF) against clinical isolates of hospital (HA) and community-acquired (CA) methicillin-resistant Staphylococcus aureus (MRSA), abstr. E-278. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother., Chicago, IL, 17 to 20 September 2007.
- 8.Lin, G., and P. C. Appelbaum. 2008. Activity of ceftobiprole compared with those of other agents against Staphylococcus aureus strains with different resistotypes by time-kill analysis. Diagn. Microbiol. Infect. Dis. 60:233-235. [DOI] [PubMed] [Google Scholar]
- 9.Lina, G., Y. Piemont, F. Godail-Gamot, M. Bes, M. O. Peter, V. Gauduchon, F. Vandenesch, and J. Etienne. 1999. Involvement of Panton-Valentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin. Infect. Dis. 29:1128-1132. [DOI] [PubMed] [Google Scholar]
- 10.Noel, G. J., K. Bush, P. Bagchi, J. Ianus, and R. S. Strauss. 2008. A randomized, double-blind trial comparing ceftobiprole medocaril with vancomycin plus ceftazidime for the treatment of patients with complicated skin and skin-structure infections. Clin. Infect. Dis. 46:647-655. [DOI] [PubMed] [Google Scholar]
- 11.Noel, G. J., R. S. Strauss, K. Amsler, M. Heep, R. Pypstra, and J. S. Solomkin. 2008. Results of a double-blind, randomized trial of ceftobiprole treatment of complicated skin and skin structure infections caused by gram-positive bacteria. Antimicrob. Agents Chemother. 52:37-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peacock, S. J., C. E. Moore, A. Justice, M. Kantzanou, L. Story, K. Mackie, G. O'Neill, and N. P. Day. 2002. Virulent combinations of adhesin and toxin genes in natural populations of Staphylococcus aureus. Infect. Immun. 70:4987-4996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sakoulas, G., G. M. Eliopoulos, R. C. Moellering, Jr., C. Wennersten, L. Venkataraman, R. P. Novick, and H. S. Gold. 2002. Accessory gene regulator (agr) locus in geographically diverse Staphylococcus aureus isolates with reduced susceptibility to vancomycin. Antimicrob. Agents Chemother. 46:1492-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang, K., J. A. McClure, S. Elsayed, T. Louie, and J. M. Conly. 2005. Novel multiplex PCR assay for characterization and concomitant subtyping of staphylococcal cassette chromosome mec types I to V in methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 43:5026-5033. [DOI] [PMC free article] [PubMed] [Google Scholar]