Humans evolved in the presence of numerous microbial communities that preceded the appearance of mammals on planet Earth. The role of these microbial communities in our evolution is a matter of considerable interest. Indeed, comparative studies with germfree and conventional animals have established that the intestinal microflora is essential for the development and function of the mucosal immune system during early life, a process that is now known to be important to overall immunity in adults. An absence of intestinal bacteria is associated with reductions in mucosal cell turnover, vascularity, muscle wall thickness, motility, baseline cytokine production, and digestive enzyme activity and with defective cell-mediated immunity (83). Furthermore, the intestinal microflora makes important metabolic contributions to vitamin K, folate, and short-chain fatty acids, such as butyrate, a major energy source for enterocytes, and also mediates the breakdown of dietary carcinogens (7, 50). The bacterial flora of the gastrointestinal tract varies longitudinally; the oral cavity contains about 200 different species, the stomach is almost sterile, and the bacterial content increases distally, with approximately 108 bacteria per g (dry weight) of ileal contents and up to 1012 bacteria per g (dry weight) of colonic contents (7). The conclusions of studies on the bacterial flora carried out some decades ago are still thought to be true. The large intestine contains organisms belonging to over 30 identified genera and as many as 500 separate species or phenotypes. The main types of bacteria in the colon are obligate anaerobes, and the most abundant bacteria are members of the genus Bacteroides, anaerobic gram-positive cocci, such as Peptostreptococcus sp., Eubacterium sp., Lactobacillus sp., and Clostridium sp. More recent studies of large bowel biopsies confirmed that Bacteroides was a dominant genus in the specimens examined (142).
Thus, intestinal bacteria represent a complex and incompletely understood microbiome. Since certain organisms are thought to play a role in the onset of inflammatory diseases of the bowel, whereas other organisms are considered protective, this review explores the relationship between bacteria that reside in the gastrointestinal tract and the host. There is an emphasis on bacterial interactions with epithelial cells, as well as on the role of bacteria in the development of inflammation and in defense mechanisms deployed by the host to counter such attacks. Selected homeostatic processes and mediators that may maintain the intestine in a state of “controlled inflammation” are also discussed.
ROLE OF THE COLONIZING BACTERIA IN THE GASTROINTESTINAL TRACT
The microflora of the intestinal microenvironment as a unit has important protective, metabolic, and trophic functions. Resident bacteria serve a central line of resistance to colonization by exogenous microbes and thus assist in preventing the potential invasion of the intestinal mucosa by an incoming pathogen. This protective function is known as the barrier effect or colonization resistance, and the bacteria have a number of important roles. One role is that adherent nonpathogenic bacteria can often prevent attachment and subsequent entry of suspected pathogens into epithelial cells. Another role is that commensal bacteria compete for available nutrients in ecological niches and, in doing so, maintain the collective microenvironment by administering and consuming all resources. This mutual and beneficial relationship helps dampen unwanted overproduction of nutrients, which could potentially support intrusion of microbial competitors that could have a pathogenic outcome for the host (51).
The microflora also makes an important metabolic contribution to the synthesis of certain vitamins. In fact, vitamin synthesis by the intestinal microflora has been recognized since at least 1934, when Fildes wrote, “It is not impossible that substances shown by the bacterial chemist to be necessary for the proper growth of bacteria may subsequently be found to be necessary for the growth of animals” (33). A key example of the importance of this metabolic relationship was the finding that germfree mice require supplementation with vitamin K and some B vitamins (i.e., folate, B12, and biotin) since these vitamins are microbially derived products (6, 155). Indeed, these vitamins are synthesized by several intestinal genera, including Bacteroides, Eubacterium, Propionibacterium, and Fusobacterium.
Perhaps the major metabolic function of the colonic microflora is the fermentation of nondigestible carbohydrates, which are key sources of energy in the colon. These nondigestible carbohydrates include large polysaccharides (i.e., resistant starches, pectins, and cellulose) and some oligosaccharides that escape digestion, as well as unabsorbed sugars and alcohols. The primary metabolic endpoint of this fermentation is the generation of short-chain fatty acids. A fundamental role of short-chain fatty acids in colonic physiology is their trophic effect on the intestinal epithelium. All three major short-chain fatty acids (acetate, proprionate, and butyrate) stimulate epithelial cell proliferation and differentiation in the colon in vivo, whereas butyrate inhibits cell proliferation and stimulates cell differentiation in vitro (35). Therefore, short-chain fatty acids appear to play an essential role in the control of epithelial cell proliferation and differentiation in the colon. In addition, recent studies have revealed further effects of butyrate on the intestinal barrier function (112).
Another important trophic factor is the communication network that exists between the host and the resident microflora at the mucosal interface, which channels the development of a competent immune system. There is a clear indication that microbial colonization of the gastrointestinal tract affects the composition of the gut-associated lymphoid tissue (GALT) (83). Not surprisingly, the interplay between the GALT and the microflora early in life is also crucial for the appropriate development of the complex mucosal and systemic immunoregulator circuitry.
Furthermore, the intimate relationship between the mucosal microflora residents, the intestinal epithelium, and the GALT is involved in sculpting the memory mechanisms of systemic immunity, such as oral tolerance. This was initially recognized after the discovery that the systemic response to a specific pathogen can be abrogated after ingestion of the antigen; this effect continues for several months in conventionally colonized mice, whereas in germfree mice systemic unresponsiveness persists for only a few days (100). Therefore, the innate immune system must be able to discriminate between potential pathogens and commensal bacteria. One way that this is achieved is by mammalian cell expression of Toll-like receptors (TLRs), which recognize conserved motifs on bacteria that are not present in higher eukaryotes. This innate strategy, which is discussed below, allows immediate recognition of bacteria so that the mammal can rapidly respond to a potential threat. Therefore, the unique dialogue that has developed between the bacteria in the normal flora and the epithelium with its associated GALT is critical to promoting the development as well as the homeostasis of the immune system.
EPITHELIAL CELL INTERACTIONS WITH PATHOGENS
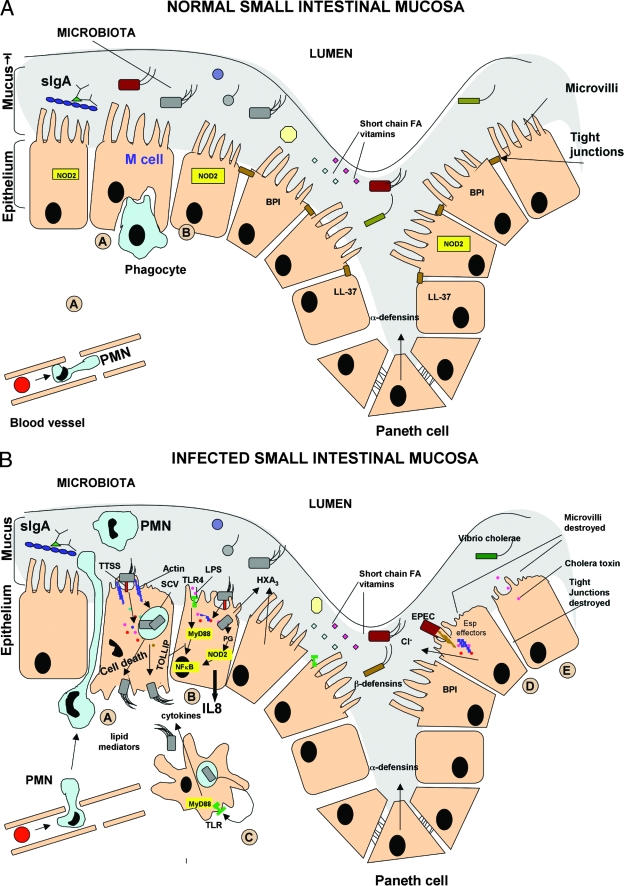
Polarized intestinal epithelial cells (IEC), as well as the resident microflora, provide a barrier that guards against microbial invasion (Fig. 1). The necessity for the epithelium to maintain an intact barrier between lumen bacteria and the lamina propria is exemplified by the consequences after the barrier function is altered. Indeed, impairment of the barrier function of the intestinal epithelium may be a predominant mechanism in the pathogenesis of inflammatory bowel disease (IBD) (23).
FIG. 1.
Schematic diagrams of small intestine mucosa in normal and infected intestines. (A) Normal intestinal mucosa, including the epithelial layer with the associated brush border, tight junctions, mucosa, and the microbiota. There are small cells at the intestinal crypts (Paneth cells) that secrete large amounts of antimicrobial peptides (defensins). A large M cell with a closely associated phagocyte is also shown. Even during the resting state some of these entrocytes express the cytoplasmic microbial pattern recognition receptors (PRR) (i.e., NOD2). (B) Infected intestinal mucosa. A typical diseased intestinal epithelium during bacterial insult is shown. On the left side (cells labeled A to C) an M cell (cell A) takes up S. enterica serovar Typhimurium after the bacterium injects its effectors through the type III secretion system (TTSS), leading to the formation of a Salmonella-containing vacuole (SCV) and eventual host cell death. Cell death liberates the bacteria, which can invade the incoming phagocytes. For a neighboring cell (cell C) the key events of the host cell response are shown, which includes LPS activation of a surface pattern recognition receptor (TLR4), leading to MyD88-dependent activation of NF-κB and basolateral release of IL-8 (CXCL8). At the same time the intracellular pattern recognition receptor, NOD2, recognizes a bacterial peptidoglycan (PG) derivative and triggers a pathway that culminates in NF-κB activation. The epithelial cells also secrete the PMN chemoattractant hepoxilin A3 (HXA3) at the apical surface, resulting in an influx of neutrophils into the mucosa and lumen from the underlying vascular bed. On the right side (cells D and E) EPEC and V. cholerae infection is shown. Cell D loosens the brush border and tight junction due to the bacterial effectors secreted by the type III secretion system. In the case of cell E the result is almost same, but the outcome is due to a toxin secreted by V. cholerae. FA, fatty acid.
Enterocytes are recognized as immunoeffector cells that have the capacity to secrete or transport cytokines, chemokines, antimicrobial peptides/proteins, mucins, immunoglobulin A (IgA), and complement components (20, 72, 107), as well as express molecules involved in antigen recognition and presentation (89). However, certain microbes have adapted to the hostile environment by targeting specific epithelial cell structures, including glycoproteins and glycolipids, which can serve as receptors for bacterial attachment (131). The strategies utilized by pathogens include directly entering epithelial cells from the apical surface, transcytosing from the apical membrane to the basolateral region, and creating direct access to basolateral domains. The latter can be achieved by direct cytotoxic injury, intracellular migration, or disruption of the epithelial cell tight junctional complex (145). It can also occur indirectly by induction of polymorphonuclear leukocyte (PMN) migration as large-scale transepithelial PMN migration results in decreased barrier function (84). Pathogens use a plethora of mechanisms to decrease the barrier function of the intestinal epithelium, and pathogen-epithelial cell interactions have been extensively reviewed (84, 145). For example, PMN migration to the epithelium can be elicited by the chemokine CXCL8, which was formerly designated interleukin-8 (IL-8) (Fig. 1). A range of pathogens upregulate the production of CXCL8 and other chemokines by IEC (26). It has been shown that enteroaggregative Escherichia coli can promote CXCL8 release from IEC via a novel flagellin (139), and this occurs by activation of TLR5 (42).
The importance of these bacterium-epithelial cell interactions is illustrated by the fact that diarrhea remains one of the leading causes of mortality in children in developing countries. Enteropathogenic E. coli (EPEC) is an important cause of severe diarrheal illness associated with high infant mortality (48). This bacterium has been shown to mediate CXCL8 release by IEC (48). In addition, infection of polarized IEC monolayers by EPEC, as well as by enterohemorragic E. coli, leads to a loss of transepithelial electrical resistance that also requires the type III secretion system. The decrease in transepithelial electrical resistance is largely due to perturbations in the apical junctional complex mediated by the EPEC and enterohemorragic E. coli type III secretion system effector protein EspF (95, 144). More recently, another EPEC effector protein, EspB, was shown to be critical for the microvillus effacing and inhibition of phagocytosis that is induced by EPEC infection (56).
All intestinal epithelial apical cell surfaces are potentially apposed to enteric microorganisms, and contact is influenced by gross anatomy (intestinal folds, crypts, and villi) and mucous layers. Some epithelial cells appear to have a specific role in sampling and processing intestinal lumen contents. These specialized epithelial M (microfold) cells, a phenotype that occurs only in the epithelium overlying organized lymphoid follicles, can deliver samples of foreign material from the lumen to organized lymphoid tissues within the mucosa of the small and large intestines (66). Many pathogens exploit mucosal lymphoid tissue to reach the mucosal barrier and to gain entry into the host. Salmonella enterica serotype Typhimurium, for example, preferentially invades M cells in murine ligated intestinal loops (60) and triggers membrane ruffling similar to that seen in cultured cells. M cells invaded by S. enterica serovar Typhimurium die, thereby facilitating dissemination of the pathogen into the tissue and systemic circulation. Members of the GTPase family, such as Rac 1, seem to regulate Salmonella invasion at the plasma membrane of cultured polarized epithelial cells (22).
EPITHELIUM-LPS INTERACTIONS: A COMPLEX SCENARIO
There are also communication networks between host cells and pathogens that seek to breach the intestinal mucosa. A variety of pathogen-associated molecular patterns (PAMPs), such as lipopolysaccharide (LPS), a glycolipid derived from the outer membrane of gram-negative bacteria, and lipoteichoic acid, derived from gram-positive bacteria, signal the immune system that “invaders” are present. Such components may also be derived from the resident microflora and thus might also be designated commensal-associated molecular patterns (15). The cellular receptors that detect the bacterial components described above in addition to flagella, bacterial DNA, and viral RNA are known as TLRs (96). TLRs are homolgous to the innate immune Toll receptors in Drosophila melanogaster, and signaling by these receptors is specific in terms of the stimulus and the type of response (69). TLR4 was the first characterized mammalian TLR and functions as the major signaling receptor for LPS in vitro and in vivo (96). The importance of the intestinal epithelium as a barrier is further underscored by the fact that the intestine is the major source of LPS, which can be found at μg/ml levels in the gut lumen (143), during sepsis, and/or after traumatic events such as surgery. Indeed, LPS is the most frequent cause of septic shock, which affects approximately 400,000 patients per year in the United States and kills more than 100,000 people per year (110).
TLRs, which are the focus of intense research, are constitutively expressed by the IEC (36), and the expression pattern is altered during IBD (16). However, there has been some controversy regarding whether enterocytes constitutively express the molecules involved in LPS signaling, and cell lines likely do not completely model the “in vivo” enterocytes (36). Activation of TLRs usually leads to sequential activation of members of the kinase family, culminating in the activation and recruitment of transcription factors such as nuclear factor κB (NF-κB), as well as the transcription of various inflammatory genes, leading to a proinflammatory cytokine cascade. NF-κB functions as a pivotal regulator of intestinal immunity (17). In addition to its immunoregulatory role, NF-κB has been demonstrated to be a regulator of apoptosis, and it is possible that pathogens use this type of cell death to their advantage (18). However, given the rapid turnover of the intestinal epithelium, it is plausible that such apoptotic mechanisms, when they occur in a controlled manner, limit infection (44) by eliminating intracellular bacteria or their components. This theory is supported somewhat by the observation that differentiated enterocytes are capable of transcytosing LPS in the basolateral-to-apical direction, an ability not shared by undifferentiated cells (4). Such mature cells sloughed off at the villus tip might clear LPS into the intestinal lumen and facilitate its removal from the body. This also correlates with the observation that enterally administered LPS does not appear in the intestinal epithelium and remains in the lumen, whereas when it is administered intravenously, it is transported to the lamina propria, largely by macrophages, and is found in enterocytes (41), where it is preferentially localized in epithelial cells at the villus tips. However, an emerging theory supports the notion that LPS recognition occurs within the enterocytes (15), where it has been shown to be bound to TLR4.
Confounding the situation further, it is still not known whether and how the body distinguishes between a pathogen and a nonpathogen. An elegant study by Rakoff-Nahoum and colleagues demonstrated that the recognition of commensal bacteria by TLRs is necessary for protection against gut injury and associated mortality (119). The very interesting series of experiments of these workers prompts the question whether it is necessary for IEC to be apposed to bacteria, if indeed IEC are the main cells involved in evoking a response. Since the protective effect was mediated by LPS alone, one wonders whether the mediator, largely viewed as proinflammatory, can mediate other, as-yet-unrecognized effects. It is not known whether this protective effect is different for bacteria termed “rough” and “smooth,” depending on the glycosylation pattern of the O antigen. Smooth strains, which are likely to be more prevalent in the intestine, are characterized by greater virulence (82). Another recent study demonstrated that in IEC, TLR4 and MyD88 expression are necessary for activation of the cyclooxygenases, such as cyclooxygenase 2, which facilitates epithelial repair in colitis (37). The interaction of LPS with enterocytes, if indeed it occurs frequently, is of significant interest but is not fully understood. The response to TLR9 agonists may differ depending on the whether signaling is activated at the apical or basolateral pole (73), underscoring the importance of epithelial cell polarity in homeostatic processes.
Recent findings indicate that certain nonpathogenic enteric bacteria initiate inflammatory signaling in the epithelium. This is thought to represent “physiologic inflammation” and with certain “control” mechanisms does not result in overt inflammation. Moreover, there are molecules that are expressed in intestinal cells, such as TOLLIP, which negatively regulate LPS/TLR4 signaling (97). Such regulatory pathways operating in IEC have been reviewed recently (45). However, the situation is complex as there are variations in LPS responsiveness between epithelial cell lines; Caco-2 cells, which express high levels of TOLLIP and low levels of TLR4, are hyporesponsive, and SW480 cells are very responsive (141). It is therefore difficult to discern which scenario best reflects the characteristics of the in vivo enterocyte. In addition, a further level of regulation in LPS-enterocyte interactions may be the phenomenon of endotoxin tolerance, whereby repeated exposure to LPS results in a lack of responsiveness (106). Indeed, it has been found that tolerance to LPS is established shortly after birth (79). Tolerance to LPS is a well-controlled active response that is orchestrated in order to prevent excessive inflammation. Homeostasis of the epithelium, therefore, likely requires a finely tuned balance between response and tolerance to bacteria within the intestinal lumen. This is influenced not only by characteristics of the epithelium and the bacterial species themselves but also by the underlying cells in the lamina propria.
MECHANISMS UTILIZED BY INTESTINAL PATHOGENS TO INITIATE AND INDUCE DISEASE
Bacterial diarrheogenic infections are characterized by disruption of the normal movement of electrolytes and water across the epithelium, which is converted from a state of net fluid absorption to a state of net fluid secretion (48, 145). Secretory diarrhea, as a result of epithelial chloride secretion, has long been considered a host defense mechanism. This conclusion is based on the notion that increased fluid and electrolyte movement into the gut lumen helps inhibit the adherence of pathogenic organisms and so “flushes” them from the body. An alternative view of pathogen-induced diarrhea is to regard it as a way to ensure transmission to new hosts. These ideas are not mutually exclusive, and secretory diarrhea may be advantageous to both the host and the pathogen. One mechanism by which Salmonella causes diarrhea was elucidated by Eckmann and colleagues. In their study it was shown that infection of cultured human IEC lines with invasive bacteria induced expression of one of the rate-limiting enzymes for prostaglandin formation, prostaglandin H synthase, an event likely to increase production of prosecretory prostaglandins (27). Verifying the physiologic importance of epithelial prostaglandin H synthase 2 expression, supernatant from bacterium-infected IEC was shown to increase chloride secretion in an in vitro model using polarized epithelial cells, and this activity was accounted for by prostaglandin E2 (27). Such reductionist models have been used extensively to elucidate the effects of bacteria, leukocytes, and drugs on barrier, transport, and immune effector properties of IEC (54).
Bacteria are not restricted to a single mechanism for host interactions that result in diarrheal disease (Fig. 1). For example, Vibrio cholerae resides in the lumen of the small intestine and produces toxins that alter ion absorption and/or secretion (1). Other bacteria, such as Shigella and enteroinvasive E. coli, invade and destroy the colonic epithelium, leading to dysentery (114). More recently, pathogenic E. coli has been shown to increase chloride ion secretion from intestinal epithelia by upregulating the expression of the receptor for the neuropeptide galanin 1 (49). Rotavirus, another important cause of diarrhea in infants, induces this condition by activating the enteric nervous system (81).
A large influx of neutrophils into the mucosa and lumen from the underlying vascular bed of the intestine is a significant feature of intestinal bacterial infections (Fig. 1). When Salmonella is added to the apical surface of T84 monolayers cocultured with PMN, transepithelial PMN migration results. CXCL8 synthesis and basolateral secretion occur and are thought to result in the recruitment of PMN through the lamina propria to the subepithelial space, but they play no role in the migration of PMN across the intestinal epithelium (91, 92). Evidence suggests that a soluble chemotactic factor, pathogen-elicited epithelial chemoattractant, is necessary for the final step of PMN transmigration into the gut lumen (94). Pathogen-elicited epithelial chemoattractant has been identified as the eicosanoid hepoxilin A3 (101). This process is quite complex, as distinct signaling pathways mediate S. enterica serovar Typhimurium invasion, induction of CXCL8 secretion, and induction of hepoxilin A3 (90). Nevertheless, the ability of Salmonella serotypes to elicit PMN transmigration in vitro correlates with their ability to cause diffuse enteritis (defined histologically as transepithelial migration of PMN), but not typhoid fever, in humans (93). In the case of S. enterica serovar Typhimurium, the effector protein SipA is necessary and sufficient to drive PMN transmigration across model intestinal epithelia (147). Since PMN can release proteases and reactive oxygen intermediates, this may result in damage to bystander cells, thus perpetuating the inflammatory process.
BACTERIA IN IBD
An increasing number of clinical and laboratory findings have provided evidence for the contribution of bacteria which reside within the intestinal lumen to the pathogenesis of IBD, and considerable data obtained with virtually all animal models have implicated bacteria in this process. The results of studies using knockout mice with disrupted genes for cytokines or cell surface structures for immunity are especially noteworthy. For example, IL-2, IL-10, or T-cell receptor knockout mice do not develop colitis when they are reared in a germfree environment (9). However, once the normal gut microflora is restored, inflammatory disease occurs. Moreover, CD4+ T cells that react with antigens of enteric bacteria produce colitis after transfer to immunodeficient hosts. This colitis resembles Crohn's disease (CD), exhibiting features such as transmural inflammation with focal ulceration (19). Among the commensal intestinal microbes colonizing both IBD patients and experimental animals, anaerobic bacteria, particularly members of the genus Bacteroides, are thought to play an important role in the development of inflammation. In a carrageenan guinea pig model of experimental colitis, germfree animals did not develop colitis until after monoassociation with Bacteroides vulgatus, and furthermore, pretreatment with the antibiotic metronidazole prevented colitis (105). The degree of cecal inflammation in HLA-B27 transgenic rats correlated with the levels of isolates of Bacteroides and increased anaerobic bacterium/aerobic bacterium and Bacteroides/aerobic bacterium ratios (121). Microorganisms other than Bacteroides have also been implicated. For example, Helicobacter muridarum has been shown to play an important role in the onset of IBD in SCID mice (58).
Data from human studies appear to corroborate the hypothesis that there is an association between the gastrointestinal flora and intestinal inflammation. Bacteria are thought to play a major role in the development of CD in particular. Indeed, mutation of a bacterial sensing gene, nucleotide oligomerization domain 2 (NOD2), accounts for a major genetic locus of CD susceptibility (53) and suppression of host protective responses (5). The sites that are typically affected by inflammation in IBD patients are the sites that bacteria colonize at a high density, such as the distal ileum and colon. Furthermore, the use of antibiotics or diversion of the fecal stream has been found to reduce inflammation in patients, thus supporting the notion that intestinal bacteria play an important role in sustaining inflammation (156). It remains unclear whether the stimulus in IBD patients is a normal response to an as-yet-unrecognized and persistent antigen or whether the inflammation represents a dysregulated response to antigens already present in the intestine secondary to a failure of normal immunoregulatory mechanisms. The hypothesis that human IBD might somehow be related to the normal bacterial flora was first proposed some years ago (138). Since then a significant amount of information has been gathered from mouse and human studies supporting the concept that a dysregulated response to the normal flora plays a critical role in the development of IBD (9). Despite these advances, interpreting the data has become somewhat confusing since what is considered “normal” or nonpathogenic flora in one rodent strain may be pathogenic in another, and similar circumstances may exist in humans. Furthermore, “normal” flora appears to be highly specific to individuals. Humans and mice are tolerant of their own autologous flora but not of heterologous flora (25); however, the underlying reasons for this are not known. Mechanisms involved in the maintenance of tolerance to commensal flora have been reviewed elsewhere (61).
Alterations in the fecal flora of IBD patients have been reported, but no consistent alterations in the balance or composition of the flora have been identified. Some studies have found greater concentrations of coliforms and aerobic bacteria in patients with severe ulcerative colitis and moderate and severe CD, whereas other studies have reported a decrease in anaerobic and Lactobacillus species in patients with active IBD (31). An investigation of the rectal mucosa-associated bacterial flora in ulcerative colitis patients showed that both the highest bacterial counts and the highest isolation frequency were observed for B. vulgatus, Bacteroides fragilis, and Bacteroides ovatus, in that order (116). Changes in colonization patterns have also been observed (134, 142), but the relative contributions of host and bacterial factors to this phenomenon remain to be elucidated. Altered host response dynamics may also account in part for the development of disease. Several studies have demonstrated that the systemic and local immune responses against gut microflora are distorted in IBD patients. The associated lesions and the immunologic changes indicate a breakdown of mechanisms that maintain oral tolerance to components of the microflora and/or foodstuffs. The findings supporting the presence of an altered immune status include an exaggerated mucosal antibody response against intestinal bacteria. For example, it has been shown that the serum antibody titer against B. fragilis was elevated in IBD patients (10), and an increased level of serum antibody to the genus Bacteroides was also demonstrated (2). B. ovatus may be a predominant commensal microbe causing a systemic IgG antibody response in IBD patients and identified a dominant bacterial antigen (126). Enzymes produced by this bacterium damage intestinal tissue (126) and may compromise the epithelial barrier. This could result in an increase in the antigen load in the submucosal compartment, culminating in an enhanced systemic IgG antibody response to the bacterium within the intestinal lumen. This is without doubt a complex process, probably involving various bacterial phenotypes.
Flagellin, a common antigen present on most motile bacteria in the intestine, was recently identified as a major antigen in CD (78). Marked reactivity of T cells to flagellin was observed, and flagellin-specific T cells induced colitis when they were adoptively transferred into immunodeficient mice. Whether such antigenic molecules consistently play a directly pathogenic role or even a potentially diagnostic role in intestinal tissue in vivo remains to be conclusively determined, but this is an exciting possibility. A systemic search for putative CD antigens is thus complicated by three issues: first, the category of microorganisms is uncertain and the microorganisms are potentially noncultivatable (123); second, resident microbes in the human ileum and colon (where CD mainly occurs) are abundant and diverse (129); and third, the disease phenotype elicited by putative microbial pathogens is very difficult to define due to host susceptibility traits (104).
SUBVERSION OF IMMUNE RESPONSES BY PATHOGENS
In the literature there are many examples of studies demonstrating that upon exposure to bacteria, eukaryotic cells activate signaling pathways that result in increased expression of several defense-related genes. However, certain pathogens, such as Yersinia enterocolitica, have developed the ability to subvert the protective host response. This microorganism has been shown to prevent the phosphorylation and subsequent degradation of the inhibitor protein IκB (132). Consequently, eukaryotic cells infected with this YopJ-expressing Yersina become impaired in NF-κB-dependent cytokine expression. Yops are believed to be the first bacterial members of a new family of ubiquitinlike proteases and act by inhibiting mitogen-activated protein kinase pathways, which in turn inhibit NF-κB activation (21). While the host substrate for this protein has not been identified, it is tempting to speculate that commensal bacteria that do not provoke a host inflammatory response may also express the Yop proteins. Indeed, microbes have developed the means to interfere with different stages of ubiquitination and related pathways in order to promote their survival and replication, and this is an area of increasing interest (125). Further, a recent study showed that S. enterica serovar Typhimurium can downmodulate CXCL8 production after invasion of IEC. The Salmonella translocated effector proteins SspH1 and SptP participate in this process (46). SspH1 is a member of the group of bacterial proteins that contain leucine-rich repeats of the LPX type that localizes to the mammalian nucleus and inhibits NF-κB-dependent gene expression. It therefore appears that downregulation of this pivotal transcripton factor is both a commensal-associated phenomenon and a pathogen-associated phenomenon.
In addition, bacteria and their products may modulate other signaling pathways, thereby influencing factors that regulate epithelial barrier function and inflammation. Hypoxia inducible factor 1 (HIF-1) is a pivotal transcription factor involved in expression of genes, including barrier protective genes, during hypoxia (39). Butyrate, which is produced by intestinal bacteria and utilized by enterocytes as an energy source, can suppress HIF activation (99). Conversely, bacteria and LPS can cause the induction of HIF-1 in human and murine epithelial cells (70). In addition, P-glycoprotein, a HIF-1-inducible protein, has been demonstrated to play a role in the inhibition of invasion of enterocytes by Listeria monocytogenes (103). Indeed, the intestine is thought to be hypoxic in the physiologic state (140), and the colonic epithelium has been shown to be severely oxygen deprived during inflammation (62). The latter study identified epithelial HIF-1 as a critical factor for barrier protection during colitis. It is therefore of great interest to determine the potential role of such cross talk between bacteria and other intestinal cell types under normal physiologic conditions, as well as under abnormal pathophysiologic conditions.
HOMEOSTASIS IN THE GUT: PATHOGENS VERSUS PROBIOTICS
The profile of the bacterial population in the intestine of an individual reflects a dynamic interaction between the many bacteria present in the lumen. Thus, there are homeostatic processes that control the inflammatory effects of certain bacteria, involving the action of nonpathogens. The normal gut flora is thought to prevent colonization by pathogens via mechanisms such as more successful competion for nutrients or for epithelial attachment sites (Fig. 1) (80). Probiotics are defined as live microbial food supplements that benefit the host by improving the intestinal microbial balance. The word “probiotic” is derived from the Greek word “biotikos,” which is literally translated as “of this life.” Probiotics have been used for many years in the animal feed industry, but they are now increasingly being made available in many forms and can be purchased over the counter as freeze-dried preparations in health food stores. Thus, possible health benefits associated with treatment using probiotic organisms are widely gaining acceptance. For example, there have been several reports of disease prevention or enhancement of immune function resulting from the administration of probiotics, such as strains of Lactobacillus, Bifidobacterium, and E. coli Nissle 1917 (EcN), in both animals and humans (38, 87). These organisms are thought to prevent the attachment of pathogens to enterocytes and invasion of these cells (80). Furthermore, probiotic bacteria have been shown to enhance the human and murine intestinal epithelial barrier function (85), thereby preventing the translocation of potentially harmful organisms.
More recent research has elucidated mechanisms by which probiotics exert beneficial effects. EcN can inhibit the growth of pathogenic organisms, probably due to the production of microcins, which are gene-encoded antimicrobial peptides secreted by Enterobacteriaceae (115), and this organism can also decrease the death of IEC induced by S. enterica serovar Dublin, a pathogenic organism (106). Furthermore, EcN induces the production of the antimicrobial peptide human β-defensin 2 (hBD-2) in IEC (149), indicating that the control of potentially harmful bacteria by probiotic strains may involve both direct and indirect mechanisms. At the intracellular level it has recently been shown that probiotic strains can inhibit NF-κB activation (113) and induce the expression of heat shock proteins (HSP) in IEC (68, 106), mechanisms likely to underlie the anti-inflammatory and cytoprotective effects of these strains. For example, the induction of HSP by bacterial products was associated with homeostatic effects and protection against colitis (119). Recently, it was also demonstrated that novel proteins isolated from Lactobacillus rhamnosus GG activate phosphoinositide-3 kinase signaling and regulate intestinal epithelial antiapoptotic and survival responses (157). Other examples of such protective phenomena include the observation that E. coli strains colonizing the gastrointestinal tract protect germfree mice against S. enterica serovar Typhimurium infection (52). It has also been reported that gram-negative enteric bacteria evoke sustained expression of HSP25 and HSP72 in the IEC of normal mice, thereby helping maintain the integrity of the intestinal barrier (67). Interestingly, it has been shown that IEC, like other immune cells, can participate in bacterial DNA recognition (59). This study demonstrated that epithelial cells recognize and respond to DNA from probiotic bacteria with attenuation of the NF-κB signaling pathway and downregulation of CXCL8 secretion in response to proinflammatory cytokines. Correlated with this observation, probiotic DNA, signaling via TLR9, can ameliorate inflammation in experimental colitis (117).
Homeostasis may even involve different strains of the same organism. An intriguing twist to the interaction of Salmonella with T84 cells is the finding that a nonpathogenic strain of Salmonella can prevent the induction of CXCL8 secretion by pathogenic Salmonella (102). Nonpathogenic Salmonella blocks IκBα degradation, which prevents subsequent nuclear translocation of the active NF-κB dimer. Although IκBα is phosphorylated, (68), its subsequent polyubiquitination is specifically inhibited, probably due to blocking of the E3-SCFβ-TrCP ubiquitination complex (68). This phenomenon has been shown to be dependent on the generation of reactive oxygen species, specifically hydrogen peroxide (71). Another mechanism of NF-κB inhibition has also been described for the abundant commensal Bacteroides thetaiotaomicron. This bacterium attenuated proinflammatory signaling by pathogenic bacteria and bacterial components, such as flagellin, and diminished inflammation and cellular infiltrate in a rat model of infection (65). The mechanism involved targeting the NF-κB subunit, RelA, and promoting its export from the nucleus in a peroxisome proliferator-activated receptor γ-dependent fashion (65). The transport of this transcriptional complex from the nucleus into the cytoplasm blocked NF-κB-activated proinflammatory genes. Moreover, peroxisome proliferator-activated receptor γ is abundantly expressed in enterocytes, possesses anti-inflammatory properties, and seems to be a potential therapeutic target (63). Thus, commensals have developed sophisticated mechanisms to regulate inflammatory pathways and protect the host from pathogens. Indeed, such findings imply that commensal bacteria are partially responsible for the unique tolerance of the gastrointestinal mucosa to the proinflammatory stimuli presented by the enormous numbers of bacteria inhabiting the gut.
ENDOGENOUS INTESTINAL ANTI-INFLAMMATORY MEDIATORS AND MECHANISMS (i) LIPOXINS
Lipoxins, which are lipid mediators that exert immunoregulatory actions on a wide range of cell types, are biosynthesized by lipoxygenases during cell-cell interactions and/or when cells are primed by cytokines (136). It has been established that lipoxins and related molecules, such as the more recently discovered resolvins, are anti-inflammatory, playing significant roles in the inhibition and resolution of inflammation (137). These lipid mediators are important in the control and resolution of low-grade inflammation throughout the body and contribute to the maintenance of immunologic homeostasis in the intestine. Indeed, it is possible that lipoxins downregulate bacterially induced inflammation in vivo, as exciting data from recent studies show that lipoxin A4 analogues attenuate the induction of a range of proinflammatory genes by IEC in response to S. enterica serovar Typhimurium infection and also reduce inflammation in colitis models (34, 43). In addition, we reported for the first time that the expression of the antibacterial endotoxin-neutralizing protein bactericidal/permeability-increasing protein (BPI) is upregulated by the stable lipoxin analogue ATLa in a range of epithelial cell lines (13). Thus, given their size (<400 Da), stability, and composition, lipoxin and resolvin analogues seem to be especially promising as future therapeutic modalities for mucosal inflammation, whereby some observed benefits may be related to the induction of epithelial BPI.
(ii) ANTIMICROBIAL PEPTIDES AND PROTEINS
Since IEC must coexist with a high density of diverse microorganisms, protection against these organisms must occur on multiple levels (Fig. 1). For example, in addition to effectors of adaptive immunity, it should be noted that there are other protective mechanisms at mucosal surfaces; one example is secretory IgA, approximately 3 g of which is secreted into the gut lumen every day. This mucosal antibody can prevent adherence to and invasion of IEC by bacteria and is a pivotal component in innate immunity (98). Mucins also comprise an important protective barrier along the gastrointestinal tract (20). Complementing these strategies, the active synthesis and secretion of small cationic antimicrobial peptides (defensins) by the epithelium and immune cells have more recently been recognized as a key mechanism for host defense. In humans, over a dozen of these antimicrobial peptides have been identified to date, and they include several salivary histadins, lactoferrin, α-defensins, β-defensins, and an 18-kDa human cationic antimicrobial protein, hCAP18 (cathelicidin LL-37).
Antimicrobial peptides and proteins are considered major effectors of innate immunity, regulating bacterial density in the intestine, and their gastrointestinal expression is evolutionarily conserved (8). Most antimicrobial peptides and proteins expressed by mammalian epithelial cells are members of peptide families that mediate nonoxidative microbial cell killing by phagocytes (8). Paneth cells are a major source of α-defensins and are located at the base of the crypts of Lieberkuehn in the small intestine of many mammalian species (108). Paneth cells are recognized by the unusually large apical secretary granules that they release into the crypt. These cells play a crucial role in innate immunity and, in particular, are a source of several antimicrobial enzymes, such as lysozyme, Reg3γ, and group IIA phospholipase A2, as well as α-defensins, which are stored in secretory granules (154). In common with other cationic antimicrobial peptides, defensins are thought to kill target microbes by disrupting their membrane integrity.
Preserving stem cell viability is vital to maintaining epithelial monolayer integrity, and thus, the proximity of Paneth cells with their armament of antimicrobial agents appears to provide an effective mechanism for protection against potential pathogenic insult. The antimicrobial activity of α-defensins likely targets both the resident microflora and pathogenic microorganisms. It has been proposed that by shaping the composition of the endogenous flora, Paneth cell α-defensins may also indirectly contribute to host defense since the resident flora competes for nutrients with incoming pathogenic microbes. The resident flora can also secrete antimicrobial substances (i.e., bacteriocins) (109). Therefore, the release of Paneth cell α-defensins into the crypt lumen is presumed to protect the mitotically active crypt cells, stem cells, and the host from ingested pathogens as a way of limiting the number microbes that colonize the crypt and the lumen and to help stabilize the composition of the endogenous flora (109). Under optimal pH and ionic conditions, mouse Paneth cell α-defensins have microbial activity against E. coli, Staphylococcus aureus, and S. enterica serovar Typhimurium. Likewise, human α-defensins are active against several bacterial species, including L. monocytogenes, E. coli, and S. enterica serovar Typhimurium (128, 150).
β-Defensins are expressed in several organs, such as skeletal muscle, airways, the esophagus, the tongue, the skin, and the intestine (111). To date six hBDs (hBD-1 to hBD-6) have been identified, and of these six, hBD-2 is perhaps the most relevant β-defensin in the gastrointestinal tract, where it is expressed only when there is infection or inflammation (32). Regulation of hBD-2 in the intestinal epithelium is not fully understood, although there is evidence that its induction is mediated by proinflammatory cytokines, such as IL-1, mostly through NF-κB- and AP-1-dependent pathways (149). Interestingly, there is also recent evidence which suggests that hBD-2 expression is regulated by TLR signaling in IEC (146). Intriguingly, this observation is consistent with previous reports which showed that IEC are poorly responsive to gram-positive and gram-negative pathogen PAMPs, since under normal baseline conditions IEC express low levels of TLR2, TLR6, and TLR4 (and the accessory molecule MD-2) (97). However, in response to cytokine stimulation, expression of TLR4 and MD-2 can be markedly increased, suggesting that TLR expression is induced during infections and inflammation (141). Thus, it appears that TLRs are required for PAMP-mediated expression of β-defensin 2 in IEC and that this mechanism may protect the intestinal epithelium from pathogen invasion, as well as from potential invaders among the commensal intestinal flora.
Several β-defensins have activity against certain bacteria. Compared with other hBDs, hBD-1 showed weaker antibacterial activity. hBD-2, however, is microbicidal against Pseudomonas aeruginosa, E. coli, and Candida albicans (a yeast) and is also bacteriostatic with S. aureus. hBD-3 has activity against S. aureus and is less sensitive to the ion composition of the medium, whereas hBD-4 is bactericidal against staphylococci, P. aeruginosa, and some yeasts (111).
Evidence of a critical role for cathelicidin LL-37 in antimicrobial defense at the gastrointestinal mucosa comes from both clinical observations and experimental models. Central to the demonstration that cathelicidin expression is relevant to gastrointestinal mucosal defense were experiments that showed that mice lacking cathelicidins were more susceptible to bacterial attachment to the intestinal wall (55). Moreover, macrophages isolated from cathelicidin-deficient animals were significantly less able to fight intracellular Salmonella bacteria (124).
Cathelicidin LL-37 is expressed within the epithelial cells located at the surface and upper crypts of a normal human colon (47). However, little or no expression was seen within the deeper colon crypts or within epithelial cells of the small intestine (47). The expression of this peptide was not upregulated in response to tumor necrosis factor alpha, IL-1α, gamma interferon, LPS, or IL-6, nor did the expression patterns and levels of LL-37 in the epithelia of normal and inflamed colons differ (150). Microbial products in general do not activate epithelial cathelicidin expression in vitro, with the exception of short-chain fatty acids, especially butyrate (130). Butyrate is a by-product of bacterial fiber fermentation that is produced by the endogenous intestinal flora, and it is a major trophic factor for colonocytes. A recent compelling study showed that oral butyrate treatment of Shigella-infected dysenteric rabbits led to improvement of clinical symptoms, decreased blood in the stool, and a reduction in the bacterial load in the stool (120). Furthermore, examination of the rectal tissue of butyrate-treated rabbits demonstrated that there was upregulation of LL-37 expression. By contrast, untreated rabbits showed strong cathelicidin suppression after infection (120). These data not only support the notion that cathelicidin is an essential effector molecule but also suggest that certain intestinal infections may be treatable through stimulation of epithelium-derived antibiotics.
BPI is a highly cationic protein with a molecular mass of approximately 55 kDa. It was first found to be present in the azurophilic granules of neutrophils by Weiss and colleagues, and it is thought to be the most potent component in nonoxidative killing mediated by these cells (152). More recently, BPI has also been shown to be expressed on the surface of neutrophils (148), on the surface of monocytes (24), in the granules of eosinophils (11), and in fibroblasts (122). Functional BPI is expressed in IEC and in the epithelium at other mucosal sites (13). By employing a BPI-neutralizing antiserum, it was revealed that surface BPI blocks endotoxin-mediated signaling in epithelia and kills S. enterica serovar Typhimurium. These studies identified epithelium-associated BPI as a potentially important “molecular shield” for protection of mucosal surfaces against gram-negative bacteria and their endotoxins (12, 13). BPI is a member of a protein family that includes other lipid- and LPS-binding proteins and is most closely related (approximately 45% sequence homology) to another LPS-binding protein, an acute-phase secretory product of hepatocytes (135). BPI mediates its antibacterial and LPS neutralizing effect by binding to the lipid A portion of LPS with a high-affinity attraction (40). The N-terminal half of the molecule is important for the antibacterial and endotoxin neutralization functions, and the motif necessary for bacterial opsonization is located in the C terminus (3).
Once BPI has bound LPS, hydrophobic interactions between the protein and the acyl chains of both LPS and phospholipids are also thought to contribute to the perturbations in the outer membrane of the bacterium. The accompanying alterations correlate with the bacteriostatic effects of BPI (86). The second effect in BPI-mediated bacterial killing is thought to be time-dependent further penetration of BPI into the envelope, allowing the molecule to extend the damage to the bacterial inner membrane, which results in disruption of critical biochemical machinery and bacterial killing. Whereas the early effects of BPI on the gram-negative bacterial wall are enhanced by defensin and cathelicidin peptides (77), late effects are thought to be accelerated by complement and by bacterial phospholipid hydrolysis (86). The implications of such cooperative activity among antimicrobial peptides and proteins in vivo are largely unexplored. Thus, binding of BPI to live bacteria results in (i) a discrete increase in the permeability of the outer membrane, (ii) hydrolysis by bacterial phospholipase and some host phospholipases of bacterial phospholipids (151), and (iii) interruption of cell division.
The bactericidal activity of BPI varies depending on the structure of the LPS; smooth strains of bacteria, possessing longer O-linked side chains, show greater resistance to BPI (14), and as previously mentioned, such strains exhibit greater virulence in vivo (82). In contrast, the antiendotoxic activities of BPI against the LPS isolated from a broad range of gram-negative bacteria are very similar regardless of the LPS structure. In general, the cytotoxic activity of BPI is limited to a wide range of gram-negative bacterial species, including encapsulated, serum-resistant E. coli K1-R, Salmonella species, and Shigella species. BPI exhibits less activity against Klebsiella pneumoniae (153) and little in vitro activity against Serratia marcescens and Burkholderia cepacia (28). Furthermore and importantly, BPI is not toxic to the eukaryotic cells that have been tested (28) and has been safe and efficacious in the human trials carried out thus far (76). Therefore, antimicrobial peptides and proteins represent a future therapeutic modality in the treatment of intestinal inflammatory disorders.
AUTOPHAGY
Autophagy is a lysosomal degradation pathway that is essential for cell survival, differentiation, development, and homeostasis. In the case of pathogenic insult, the autophagic machinery is a clever defense system against intracellular pathogens that targets the selective delivery of microorganisms to degradative lysomsomes (a process termed xenophagy) and the delivery of microbial nucleic acids and antigens to endosomal/lysosomal compartments for actvation of innate and adaptive immunity (74, 75, 133). Examples of bacteria that are degraded in vitro by xenophagy include S. enterica serovar Typhimurium, Shigella flexneri, L. monocytogenes, Mycobacterium tuberculosis, group A Streptococcus, and Francisella tularensis. Although it is envisaged that xenophagy occurs in vivo, the current data supporting this hypothesis are limited to certain viral diseases, such as the diseases caused by tobacco mosaic virus in plants and herpes simplex virus type 1 and Sindbis virus in mice (74, 75). However, given the significance of autophagy in host defense against intracellular pathogens, microbial virulence (sculpted by a coevolutionary process) may be partially determined by the ability of such pathogens to prosper and successfully antagonize host autophagy. For example, successful intracellular microbes may antagonize the signaling pathways that antagonize autophagy, as well as membrane trafficking events that are required for lysosomal delivery and degradation (74, 75). Interestingly, autophagy genes have recently been linked with the development of CD (88).
PATHOGENIC DEFENSES
To counter the effectiveness of antimicrobial peptides, many bacterial pathogens have developed defensive strategies for survival. Thus, resistance to antimicrobial peptides is considered a strong virulence determinant, and many of the defensive strategies appear to be species specific. Some general mechanisms include bacterial downregulation of antimicrobial peptide expression by host cells and the expression of factors that prevent the effectiveness of antimicrobial peptides and proteins. There are two striking examples for intestinal pathogens. For effective pathogenesis Salmonella needs to survive in the small intestine lumen. Interestingly, it has been documented that S. enterica serovar Typhimurium can downregulate both message and stored protein levels of several Paneth cell antimicrobials in mice, including defensins and lysozyme (127). Such regulation of Paneth cell antimicrobial peptide and protein expression appears to be linked to successful invasion via the Salmonella pathogenicity island 1 type III secretion system. This finding raises the possibility that specific interactions between the bacterium and the mucosa, and perhaps Salmonella pathogenicity island 1-secreted effectors, are required for induction of the alteration in antimicrobial peptide expression. Thus, this example illustrates that Salmonella may gain a specific survival advantage in the intestinal lumen by decreasing the expression of antimicrobial peptides and proteins.
Likewise, S. flexneri infection was found to decrease the expression of α-defensin 1 and LL-37 in colonic epithelial cell lines, as well as in human colonic biopsy specimens. Such regulation requires only the Shigella virulence plasmid DNA (even in the absence of live bacteria) (57). The fact that S. enterica serovar Typhi and L. monocytogenes do not modulate Paneth cell antimicrobial expression indicates that such effects are species specific. These observations further suggest that distinct antimicrobial effector molecules of the intestinal mucosa are capable of responding differently, depending on the bacterial stimulus.
Enteric pathogens can also change their structural components to evade immune recognition and susceptibility to antimicrobial peptides. A key pathway for the induction of inflammation in response to gram-negative bacteria is the activation of TLR4 signaling by LPS. The immunity-activating moiety of LPS is lipid A, a diglucoasamine unit with covalently attached acyl chains that interacts with the host LPS receptor complex consisting of TLR4 and its coreceptor MD-2 to induce cellular responses. While the lipid A structure is conserved among gram-negative bacteria, it is not invariant. Consequently, the number, location, and composition of the acyl chains vary among species and are profoundly influenced by the environment. For instance, in response to environmental conditions, S. enterica covalently modifies its lipid A through a variety of processes, including, palmitoylation, deacylation, hydroxylation, and the addition of 4-amino-4-deoxy-l-arabinose (aminoarabinose) or phosphoethanolamine (29, 118). Similar modifications occur in other gram-negative bacteria, including E. coli (158), Yersinia pestis (64), and P. aeruginosa (30). Thus, changes in the acylation pattern of LPS and other LPS modifications are important bacterial adaptation responses, making the invading bacteria “Trojan horses” since they are less likely to be recognized by TLR4.
CONCLUSION
The first recorded citation in the Oxford English Dictionary of the term inflammation dates from the mid-1500s, and this word means the action of “setting on fire.” Indeed, an expression for the condition that we recognize today as inflammation can be found in the earliest Egyptian medical papyri (ca. 2500 BC). However, inflammation, its onset, and the agents that limit it remain incompletely understood. In this context there is still confusion regarding the exact role of bacteria in the intestine. While bacteria are essential for immune development in this organ, it is clear that these organisms can cause inflammation. It is increasingly recognized that communication between bacteria and mucosal epithelial cells is a bidirectional process, with bacteria being able to both diminish and augment inflammatory pathways. The development of tolerance or unresponsiveness to the indigenous microflora and protective immune responses to enteropathogens remains an intruiging paradox, and the cellular context of a protective or detrimental response remains to be fully clarified. With an understanding of how such homeostatic processes function to maintain the host in a state of health, it can perhaps be divined how these mechanisms malfunction in disease.
Acknowledgments
We thank C. V. Srikanth for his critical reading of the manuscript and for his valued assistance with composing the figure.
This study was supported by National Institutes of Health grants DK56754 and DK33506 to B.A.M.
Editor: J. B. Kaper
Footnotes
Published ahead of print on 12 May 2008.
REFERENCES
- 1.Asakura, H., and M. Yoshioka. 1994. Cholera toxin and diarrhoea. J. Gastroenterol. Hepatol. 9186-193. [DOI] [PubMed] [Google Scholar]
- 2.Bamba, T., H. Matsuda, M. Endo, and Y. Fujiyama. 1995. The pathogenic role of Bacteroides vulgatus in patients with ulcerative colitis. J. Gastroenterol. 30(Suppl. 8)45-47. [PubMed] [Google Scholar]
- 3.Beamer, L. J., S. F. Carroll, and D. Eisenberg. 1997. Crystal structure of human BPI and two bound phospholipids at 2.4 angstrom resolution. Science 2761861-1864. [DOI] [PubMed] [Google Scholar]
- 4.Beatty, W. L., and P. J. Sansonetti. 1997. Role of lipopolysaccharide in signaling to subepithelial polymorphonuclear leukocytes. Infect. Immun. 654395-4404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Begue, B., C. Dumant, J. C. Bambou, J. F. Beaulieu, M. Chamaillard, J. P. Hugot, O. Goulet, J. Schmitz, D. J. Philpott, N. Cerf-Bensussan, and F. M. Ruemmele. 2006. Microbial induction of CARD15 expression in intestinal epithelial cells via Toll-like receptor 5 triggers an antibacterial response loop. J. Cell Physiol. 209241-252. [DOI] [PubMed] [Google Scholar]
- 6.Bentley, R., and R. Meganathan. 1982. Biosynthesis of vitamin K (menaquinone) in bacteria. Microbiol. Rev. 46241-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berg, R. D. 1996. The indigenous gastrointestinal microflora. Trends Microbiol. 4430-435. [DOI] [PubMed] [Google Scholar]
- 8.Bevins, C. L., E. Martin-Porter, and T. Ganz. 1999. Defensins and innate host defence of the gastrointestinal tract. Gut 45911-915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blumberg, R. S., L. J. Saubermann, and W. Strober. 1999. Animal models of mucosal inflammation and their relation to human inflammatory bowel disease. Curr. Opin. Immunol. 11648-656. [DOI] [PubMed] [Google Scholar]
- 10.Brown, W. R., and E. Lee. 1974. Radioimmunological measurements of bacterial antibodies. II. Human serum antibodies reactive with Bacteroides fragilis and Enterococcus in gastrointestinal and immunological disorders. Gastroenterology 661145-1153. [PubMed] [Google Scholar]
- 11.Calafat, J., H. Janssen, A. Tool, M. A. Dentener, E. F. Knol, H. F. Rosenberg, and A. Egesten. 1998. The bactericidal/permeability-increasing protein (BPI) is present in specific granules of human eosinophils. Blood 914770-4775. [PubMed] [Google Scholar]
- 12.Canny, G., E. Cario, A. Lennartsson, U. Gullberg, C. Brennan, O. Levy, and S. P. Colgan. 2006. Functional and biochemical characterization of epithelial bactericidal/permeability-increasing protein. Am. J. Physiol. Gastrointest. Liver Physiol. 290G557-G567. [DOI] [PubMed] [Google Scholar]
- 13.Canny, G., O. Levy, G. T. Furuta, S. Narravula-Alipati, R. B. Sisson, C. N. Serhan, and S. P. Colgan. 2002. Lipid mediator-induced expression of bactericidal/permeability-increasing protein (BPI) in human mucosal epithelia. Proc. Natl. Acad. Sci. USA 993902-3907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Capodici, C., S. Chen, Z. Sidorczyk, P. Elsbach, and J. Weiss. 1994. Effect of lipopolysaccharide (LPS) chain length on interactions of bactericidal/permeability-increasing protein and its bioactive 23-kilodalton NH2-terminal fragment with isolated LPS and intact Proteus mirabilis and Escherichia coli. Infect. Immun. 62259-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cario, E., D. Brown, M. McKee, K. Lynch-Devaney, G. Gerken, and D. K. Podolsky. 2002. Commensal-associated molecular patterns induce selective Toll-like receptor-trafficking from apical membrane to cytoplasmic compartments in polarized intestinal epithelium. Am. J. Pathol. 160165-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cario, E., and D. K. Podolsky. 2000. Differential alteration in intestinal epithelial cell expression of Toll-like receptor 3 (TLR3) and TLR4 in inflammatory bowel disease. Infect. Immun. 687010-7017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen, L. W., L. Egan, Z. W. Li, F. R. Greten, M. F. Kagnoff, and M. Karin. 2003. The two faces of IKK and NF-κB inhibition: prevention of systemic inflammation but increased local injury following intestinal ischemia-reperfusion. Nat. Med. 9575-581. [DOI] [PubMed] [Google Scholar]
- 18.Collier-Hyams, L. S., H. Zeng, J. Sun, A. D. Tomlinson, Z. Q. Bao, H. Chen, J. L. Madara, K. Orth, and A. S. Neish. 2002. Cutting edge: Salmonella AvrA effector inhibits the key proinflammatory, anti-apoptotic NF-κB pathway. J. Immunol. 1692846-2850. [DOI] [PubMed] [Google Scholar]
- 19.Cong, Y., S. L. Brandwein, R. P. McCabe, A. Lazenby, E. H. Birkenmeier, J. P. Sundberg, and C. O. Elson. 1998. CD4+ T cells reactive to enteric bacterial antigens in spontaneously colitic C3H/HeJBir mice: increased T helper cell type 1 response and ability to transfer disease. J. Exp. Med. 187855-864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corfield, A. P., D. Carroll, N. Myerscough, and C. S. Probert. 2001. Mucins in the gastrointestinal tract in health and disease. Front. Biosci. 6D1321-1357. [DOI] [PubMed] [Google Scholar]
- 21.Cornelis, G. R., and G. Denecker. 2001. Yersinia lead SUMO attack. Nat. Med. 721-23. [DOI] [PubMed] [Google Scholar]
- 22.Criss, A. K., D. M. Ahlgren, T. S. Jou, B. A. McCormick, and J. E. Casanova. 2001. The GTPase Rac1 selectively regulates Salmonella invasion at the apical plasma membrane of polarized epithelial cells. J. Cell Sci. 1141331-1341. [DOI] [PubMed] [Google Scholar]
- 23.DeMeo, M. T., E. A. Mutlu, A. Keshavarzian, and M. C. Tobin. 2002. Intestinal permeation and gastrointestinal disease. J. Clin. Gastroenterol. 34385-396. [DOI] [PubMed] [Google Scholar]
- 24.Dentener, M. A., G. J. Francot, and W. A. Buurman. 1996. Bactericidal/permeability-increasing protein, a lipopolysaccharide-specific protein on the surface of human peripheral blood monocytes. J. Infect. Dis. 173252-255. [DOI] [PubMed] [Google Scholar]
- 25.Duchmann, R., H. Lochs, and W. Kruis. 1999. Crohn disease, ulcerative colitis. When bacteria attack the intestinal wall. MMW Fortschr. Med. 14148-51. [PubMed] [Google Scholar]
- 26.Eckmann, L., and M. F. Kagnoff. 2001. Cytokines in host defense against Salmonella. Microbes Infect. 31191-1200. [DOI] [PubMed] [Google Scholar]
- 27.Eckmann, L., W. F. Stenson, T. C. Savidge, D. C. Lowe, K. E. Barrett, J. Fierer, J. R. Smith, and M. F. Kagnoff. 1997. Role of intestinal epithelial cells in the host secretory response to infection by invasive bacteria. Bacterial entry induces epithelial prostaglandin h synthase-2 expression and prostaglandin E2 and F2α production. J. Clin. Investig. 100296-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elsbach, P. 1994. Bactericidal permeability-increasing protein in host defence against gram-negative bacteria and endotoxin. Ciba Found. Symp. 186176-187. (Discussion, 186:187-189.) [DOI] [PubMed] [Google Scholar]
- 29.Ernst, R. K., T. Guina, and S. I. Miller. 2001. Salmonella typhimurium outer membrane remodeling: role in resistance to host innate immunity. Microbes Infect. 31327-1334. [DOI] [PubMed] [Google Scholar]
- 30.Ernst, R. K., E. C. Yi, L. Guo, K. B. Lim, J. L. Burns, M. Hackett, and S. I. Miller. 1999. Specific lipopolysaccharide found in cystic fibrosis airway Pseudomonas aeruginosa. Science 2861561-1565. [DOI] [PubMed] [Google Scholar]
- 31.Fabia, R., A. Ar'Rajab, M. L. Johansson, R. Andersson, R. Willen, B. Jeppsson, G. Molin, and S. Bengmark. 1993. Impairment of bacterial flora in human ulcerative colitis and experimental colitis in the rat. Digestion 54248-255. [DOI] [PubMed] [Google Scholar]
- 32.Fahlgren, A., S. Hammarstrom, A. Danielsson, and M. L. Hammarstrom. 2003. Increased expression of antimicrobial peptides and lysozyme in colonic epithelial cells of patients with ulcerative colitis. Clin. Exp. Immunol. 13190-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fildes, P. 1934. Some medical and other aspects bacterial chemistry. Proc. R. Soc. Med. 2879-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fiorucci, S., J. L. Wallace, A. Mencarelli, E. Distrutti, G. Rizzo, S. Farneti, A. Morelli, J. L. Tseng, B. Suramanyam, W. J. Guilford, and J. F. Parkinson. 2004. A beta-oxidation-resistant lipoxin A4 analog treats hapten-induced colitis by attenuating inflammation and immune dysfunction. Proc. Natl. Acad. Sci. USA 10115736-15741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Frankel, W. L., W. Zhang, A. Singh, D. M. Klurfeld, S. Don, T. Sakata, I. Modlin, and J. L. Rombeau. 1994. Mediation of the trophic effects of short-chain fatty acids on the rat jejunum and colon. Gastroenterology 106375-380. [DOI] [PubMed] [Google Scholar]
- 36.Fukata, M., and M. T. Abreu. 2008. Role of Toll-like receptors in gastrointestinal malignancies. Oncogene 27234-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fukata, M., A. Chen, A. Klepper, S. Krishnareddy, A. S. Vamadevan, L. S. Thomas, R. Xu, H. Inoue, M. Arditi, A. J. Dannenberg, and M. T. Abreu. 2006. Cox-2 is regulated by Toll-like receptor-4 (TLR4) signaling: role in proliferation and apoptosis in the intestine. Gastroenterology 131862-877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Furrie, E., S. Macfarlane, A. Kennedy, J. H. Cummings, S. V. Walsh, D. A. O'Neil, and G. T. Macfarlane. 2005. Synbiotic therapy (Bifidobacterium longum/Synergy 1) initiates resolution of inflammation in patients with active ulcerative colitis: a randomised controlled pilot trial. Gut 54242-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Furuta, G. T., J. R. Turner, C. T. Taylor, R. M. Hershberg, K. Comerford, S. Narravula, D. K. Podolsky, and S. P. Colgan. 2001. Hypoxia-inducible factor 1-dependent induction of intestinal trefoil factor protects barrier function during hypoxia. J. Exp. Med. 1931027-1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gazzano-Santoro, H., J. B. Parent, L. Grinna, A. Horwitz, T. Parsons, G. Theofan, P. Elsbach, J. Weiss, and P. J. Conlon. 1992. High-affinity binding of the bactericidal/permeability-increasing protein and a recombinant amino-terminal fragment to the lipid A region of lipopolysaccharide. Infect. Immun. 604754-4761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ge, Y., R. M. Ezzell, and H. S. Warren. 2000. Localization of endotoxin in the rat intestinal epithelium. J. Infect. Dis. 182873-881. [DOI] [PubMed] [Google Scholar]
- 42.Gewirtz, A. T., T. A. Navas, S. Lyons, P. J. Godowski, and J. L. Madara. 2001. Cutting edge: bacterial flagellin activates basolaterally expressed TLR5 to induce epithelial proinflammatory gene expression. J. Immunol. 1671882-1885. [DOI] [PubMed] [Google Scholar]
- 43.Gewirtz, A. T., A. S. Neish, and J. L. Madara. 2002. Mechanisms of active intestinal inflammation and potential down-regulation via lipoxins. Adv. Exp. Med. Biol. 507229-236. [DOI] [PubMed] [Google Scholar]
- 44.Grassme, H., S. Kirschnek, J. Riethmueller, A. Riehle, G. von Kurthy, F. Lang, M. Weller, and E. Gulbins. 2000. CD95/CD95 ligand interactions on epithelial cells in host defense to Pseudomonas aeruginosa. Science 290527-530. [DOI] [PubMed] [Google Scholar]
- 45.Haller, D., and C. Jobin. 2004. Interaction between resident luminal bacteria and the host: can a healthy relationship turn sour? J. Pediatr. Gastroenterol. Nutr. 38123-136. [DOI] [PubMed] [Google Scholar]
- 46.Haraga, A., and S. I. Miller. 2006. A Salmonella type III secretion effector interacts with the mammalian serine/threonine protein kinase PKN1. Cell. Microbiol. 8837-846. [DOI] [PubMed] [Google Scholar]
- 47.Hase, K., L. Eckmann, J. D. Leopard, N. Varki, and M. F. Kagnoff. 2002. Cell differentiation is a key determinant of cathelicidin LL-37/human cationic antimicrobial protein 18 expression by human colon epithelium. Infect. Immun. 70953-963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hecht, G. 2001. Microbes and microbial toxins: paradigms for microbial-mucosal interactions. VII. Enteropathogenic Escherichia coli: physiological alterations from an extracellular position. Am. J. Physiol. Gastrointest. Liver Physiol. 281G1-G7. [DOI] [PubMed] [Google Scholar]
- 49.Hecht, G., J. A. Marrero, A. Danilkovich, K. A. Matkowskyj, S. D. Savkovic, A. Koutsouris, and R. V. Benya. 1999. Pathogenic Escherichia coli increase Cl− secretion from intestinal epithelia by upregulating galanin-1 receptor expression. J. Clin. Investig. 104253-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hooper, L. V., T. Midtvedt, and J. I. Gordon. 2002. How host-microbial interactions shape the nutrient environment of the mammalian intestine. Annu. Rev. Nutr. 22283-307. [DOI] [PubMed] [Google Scholar]
- 51.Hooper, L. V., J. Xu, P. G. Falk, T. Midtvedt, and J. I. Gordon. 1999. A molecular sensor that allows a gut commensal to control its nutrient foundation in a competitive ecosystem. Proc. Natl. Acad. Sci. USA 969833-9838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hudault, S., J. Guignot, and A. L. Servin. 2001. Escherichia coli strains colonising the gastrointestinal tract protect germfree mice against Salmonella typhimurium infection. Gut 4947-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hugot, J. P. 2006. CARD15/NOD2 mutations in Crohn's disease. Ann. N. Y. Acad. Sci. 10729-18. [DOI] [PubMed] [Google Scholar]
- 54.Hurley, B. P., and B. A. McCormick. 2003. Translating tissue culture results into animal models: the case of Salmonella typhimurium. Trends Microbiol. 11562-569. [DOI] [PubMed] [Google Scholar]
- 55.Iimura, M., R. L. Gallo, K. Hase, Y. Miyamoto, L. Eckmann, and M. F. Kagnoff. 2005. Cathelicidin mediates innate intestinal defense against colonization with epithelial adherent bacterial pathogens. J. Immunol. 1744901-4907. [DOI] [PubMed] [Google Scholar]
- 56.Iizumi, Y., H. Sagara, Y. Kabe, M. Azuma, K. Kume, M. Ogawa, T. Nagai, P. G. Gillespie, C. Sasakawa, and H. Handa. 2007. The enteropathogenic E. coli effector EspB facilitates microvillus effacing and antiphagocytosis by inhibiting myosin function. Cell Host Microbe 2383-392. [DOI] [PubMed] [Google Scholar]
- 57.Islam, D., L. Bandholtz, J. Nilsson, H. Wigzell, B. Christensson, B. Agerberth, and G. Gudmundsson. 2001. Downregulation of bactericidal peptides in enteric infections: a novel immune escape mechanism with bacterial DNA as a potential regulator. Nat. Med. 7180-185. [DOI] [PubMed] [Google Scholar]
- 58.Jiang, H. Q., N. Kushnir, M. C. Thurnheer, N. A. Bos, and J. J. Cebra. 2002. Monoassociation of SCID mice with Helicobacter muridarum, but not four other enterics, provokes IBD upon receipt of T cells. Gastroenterology 1221346-1354. [DOI] [PubMed] [Google Scholar]
- 59.Jijon, H., J. Backer, H. Diaz, H. Yeung, D. Thiel, C. McKaigney, C. De Simone, and K. Madsen. 2004. DNA from probiotic bacteria modulates murine and human epithelial and immune function. Gastroenterology 1261358-1373. [DOI] [PubMed] [Google Scholar]
- 60.Jones, B. D., N. Ghori, and S. Falkow. 1994. Salmonella typhimurium initiates murine infection by penetrating and destroying the specialized epithelial M cells of the Peyer's patches. J. Exp. Med. 18015-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jump, R. L., and A. D. Levine. 2004. Mechanisms of natural tolerance in the intestine: implications for inflammatory bowel disease. Inflamm. Bowel Dis. 10462-478. [DOI] [PubMed] [Google Scholar]
- 62.Karhausen, J., G. T. Furuta, J. E. Tomaszewski, R. S. Johnson, S. P. Colgan, and V. H. Haase. 2004. Epithelial hypoxia-inducible factor-1 is protective in murine experimental colitis. J. Clin. Investig. 1141098-1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Katayama, K., K. Wada, A. Nakajima, H. Mizuguchi, T. Hayakawa, S. Nakagawa, T. Kadowaki, R. Nagai, Y. Kamisaki, R. S. Blumberg, and T. Mayumi. 2003. A novel PPAR gamma gene therapy to control inflammation associated with inflammatory bowel disease in a murine model. Gastroenterology 1241315-1324. [DOI] [PubMed] [Google Scholar]
- 64.Kawahara, K., H. Tsukano, H. Watanabe, B. Lindner, and M. Matsuura. 2002. Modification of the structure and activity of lipid A in Yersinia pestis lipopolysaccharide by growth temperature. Infect. Immun. 704092-4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kelly, D., J. I. Campbell, T. P. King, G. Grant, E. A. Jansson, A. G. Coutts, S. Pettersson, and S. Conway. 2004. Commensal anaerobic gut bacteria attenuate inflammation by regulating nuclear-cytoplasmic shuttling of PPAR-gamma and RelA. Nat. Immunol. 5104-112. [DOI] [PubMed] [Google Scholar]
- 66.Kerneis, S., and E. Pringault. 1999. Plasticity of the gastrointestinal epithelium: the M cell paradigm and opportunism of pathogenic microorganisms. Semin. Immunol. 11205-215. [DOI] [PubMed] [Google Scholar]
- 67.Kojima, K., M. W. Musch, H. Ren, D. L. Boone, B. A. Hendrickson, A. Ma, and E. B. Chang. 2003. Enteric flora and lymphocyte-derived cytokines determine expression of heat shock proteins in mouse colonic epithelial cells. Gastroenterology 1241395-1407. [DOI] [PubMed] [Google Scholar]
- 68.Kojima, K., M. W. Musch, M. J. Ropeleski, D. L. Boone, A. Ma, and E. B. Chang. 2004. Escherichia coli LPS induces heat shock protein 25 in intestinal epithelial cells through MAP kinase activation. Am. J. Physiol. Gastrointest. Liver Physiol. 286G645-G652. [DOI] [PubMed] [Google Scholar]
- 69.Kopp, E., and R. Medzhitov. 2003. Recognition of microbial infection by Toll-like receptors. Curr. Opin. Immunol. 15396-401. [DOI] [PubMed] [Google Scholar]
- 70.Koury, J., E. A. Deitch, H. Homma, B. Abungu, P. Gangurde, M. R. Condon, Q. Lu, D. Z. Xu, and R. Feinman. 2004. Persistent HIF-1α activation in gut ischemia/reperfusion injury: potential role of bacteria and lipopolysaccharide. Shock 22270-277. [DOI] [PubMed] [Google Scholar]
- 71.Kumar, A., H. Wu, L. S. Collier-Hyams, J. M. Hansen, T. Li, K. Yamoah, Z. Q. Pan, D. P. Jones, and A. S. Neish. 2007. Commensal bacteria modulate cullin-dependent signaling via generation of reactive oxygen species. EMBO J. 264457-4466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lamm, M. E. 1998. Current concepts in mucosal immunity. IV. How epithelial transport of IgA antibodies relates to host defense. Am. J. Physiol. 274G614-G617. [DOI] [PubMed] [Google Scholar]
- 73.Lee, J., J. H. Mo, K. Katakura, I. Alkalay, A. N. Rucker, Y. T. Liu, H. K. Lee, C. Shen, G. Cojocaru, S. Shenouda, M. Kagnoff, L. Eckmann, Y. Ben-Neriah, and E. Raz. 2006. Maintenance of colonic homeostasis by distinctive apical TLR9 signalling in intestinal epithelial cells. Nat. Cell Biol. 81327-1336. [DOI] [PubMed] [Google Scholar]
- 74.Levine, B., and V. Deretic. 2007. Unveiling the roles of autophagy in innate and adaptive immunity. Nat. Rev. Immunol. 7767-777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Levine, B., and G. Kroemer. 2008. Autophagy in the pathogenesis of disease. Cell 13227-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Levy, O. 2002. Therapeutic potential of the bactericidal/permeability-increasing protein. Expert Opin. Investig. Drugs 11159-167. [DOI] [PubMed] [Google Scholar]
- 77.Levy, O., C. E. Ooi, J. Weiss, R. I. Lehrer, and P. Elsbach. 1994. Individual and synergistic effects of rabbit granulocyte proteins on Escherichia coli. J. Clin. Investig. 94672-682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lodes, M. J., Y. Cong, C. O. Elson, R. Mohamath, C. J. Landers, S. R. Targan, M. Fort, and R. M. Hershberg. 2004. Bacterial flagellin is a dominant antigen in Crohn disease. J. Clin. Investig. 1131296-1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lotz, M., D. Gutle, S. Walther, S. Menard, C. Bogdan, and M. W. Hornef. 2006. Postnatal acquisition of endotoxin tolerance in intestinal epithelial cells. J. Exp. Med. 203973-984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lu, L., and W. A. Walker. 2001. Pathologic and physiologic interactions of bacteria with the gastrointestinal epithelium. Am. J. Clin. Nutr. 731124S-1130S. [DOI] [PubMed] [Google Scholar]
- 81.Lundgren, O., A. T. Peregrin, K. Persson, S. Kordasti, I. Uhnoo, and L. Svensson. 2000. Role of the enteric nervous system in the fluid and electrolyte secretion of rotavirus diarrhea. Science 287491-495. [DOI] [PubMed] [Google Scholar]
- 82.Lyman, M. B., J. P. Steward, and R. J. Roantree. 1976. Characterization of the virulence and antigenic structure of Salmonella typhimurium strains with lipopolysaccharide core defects. Infect. Immun. 131539-1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Macdonald, T. T., and G. Monteleone. 2005. Immunity, inflammation, and allergy in the gut. Science 3071920-1925. [DOI] [PubMed] [Google Scholar]
- 84.Madara, J. L. 2000. Modulation of tight junctional permeability. Adv. Drug Deliv. Rev. 41251-253. [DOI] [PubMed] [Google Scholar]
- 85.Madsen, K., A. Cornish, P. Soper, C. McKaigney, H. Jijon, C. Yachimec, J. Doyle, L. Jewell, and C. De Simone. 2001. Probiotic bacteria enhance murine and human intestinal epithelial barrier function. Gastroenterology 121580-591. [DOI] [PubMed] [Google Scholar]
- 86.Mannion, B. A., J. Weiss, and P. Elsbach. 1990. Separation of sublethal and lethal effects of polymorphonuclear leukocytes on Escherichia coli. J. Clin. Investig. 86631-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Marteau, P., P. Seksik, P. Lepage, and J. Dore. 2004. Cellular and physiological effects of probiotics and prebiotics. Mini Rev. Med. Chem. 4889-896. [DOI] [PubMed] [Google Scholar]
- 88.Massey, D. C., and M. Parkes. 2007. Genome-wide association scanning highlights two autophagy genes, ATG16L1 and IRGM, as being significantly associated with Crohn's disease. Autophagy 3649-651. [DOI] [PubMed] [Google Scholar]
- 89.Mayer, L. 2000. Epithelial cell antigen presentation. Curr. Opin. Gastroenterol. 16531-535. [DOI] [PubMed] [Google Scholar]
- 90.McCormick, B. A. 2007. Bacterial-induced hepoxilin A3 secretion as a pro-inflammatory mediator. FEBS J. 2743513-3518. [DOI] [PubMed] [Google Scholar]
- 91.McCormick, B. A., S. P. Colgan, C. Delp-Archer, S. I. Miller, and J. L. Madara. 1993. Salmonella typhimurium attachment to human intestinal epithelial monolayers: transcellular signalling to subepithelial neutrophils. J. Cell Biol. 123895-907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.McCormick, B. A., P. M. Hofman, J. Kim, D. K. Carnes, S. I. Miller, and J. L. Madara. 1995. Surface attachment of Salmonella typhimurium to intestinal epithelia imprints the subepithelial matrix with gradients chemotactic for neutrophils. J. Cell Biol. 1311599-1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.McCormick, B. A., S. I. Miller, D. Carnes, and J. L. Madara. 1995. Transepithelial signaling to neutrophils by salmonellae: a novel virulence mechanism for gastroenteritis. Infect. Immun. 632302-2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.McCormick, B. A., C. A. Parkos, S. P. Colgan, D. K. Carnes, and J. L. Madara. 1998. Apical secretion of a pathogen-elicited epithelial chemoattractant activity in response to surface colonization of intestinal epithelia by Salmonella typhimurium. J. Immunol. 160455-466. [PubMed] [Google Scholar]
- 95.McNamara, B. P., A. Koutsouris, C. B. O'Connell, J. P. Nougayrede, M. S. Donnenberg, and G. Hecht. 2001. Translocated EspF protein from enteropathogenic Escherichia coli disrupts host intestinal barrier function. J. Clin. Investig. 107621-629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Medzhitov, R. 2001. Toll-like receptors and innate immunity. Nat. Rev. Immunol. 1135-145. [DOI] [PubMed] [Google Scholar]
- 97.Melmed, G., L. S. Thomas, N. Lee, S. Y. Tesfay, K. Lukasek, K. S. Michelsen, Y. Zhou, B. Hu, M. Arditi, and M. T. Abreu. 2003. Human intestinal epithelial cells are broadly unresponsive to Toll-like receptor 2-dependent bacterial ligands: implications for host-microbial interactions in the gut. J. Immunol. 1701406-1415. [DOI] [PubMed] [Google Scholar]
- 98.Mestecky, J., M. W. Russell, and C. O. Elson. 1999. Intestinal IgA: novel views on its function in the defence of the largest mucosal surface. Gut 442-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Miki, K., N. Unno, T. Nagata, M. Uchijima, H. Konno, Y. Koide, and S. Nakamura. 2004. Butyrate suppresses hypoxia-inducible factor-1 activity in intestinal epithelial cells under hypoxic conditions. Shock 22446-452. [DOI] [PubMed] [Google Scholar]
- 100.Moreau, M. C., and V. Gaboriau-Routhiau. 1996. The absence of gut flora, the doses of antigen ingested and aging affect the long-term peripheral tolerance induced by ovalbumin feeding in mice. Res. Immunol. 14749-59. [DOI] [PubMed] [Google Scholar]
- 101.Mrsny, R. J., A. T. Gewirtz, D. Siccardi, T. Savidge, B. P. Hurley, J. L. Madara, and B. A. McCormick. 2004. Identification of hepoxilin A3 in inflammatory events: a required role in neutrophil migration across intestinal epithelia. Proc. Natl. Acad. Sci. USA 1017421-7426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Neish, A. S., A. T. Gewirtz, H. Zeng, A. N. Young, M. E. Hobert, V. Karmali, A. S. Rao, and J. L. Madara. 2000. Prokaryotic regulation of epithelial responses by inhibition of IκB-alpha ubiquitination. Science 2891560-1563. [DOI] [PubMed] [Google Scholar]
- 103.Neudeck, B. L., J. M. Loeb, N. G. Faith, and C. J. Czuprynski. 2004. Intestinal P glycoprotein acts as a natural defense mechanism against Listeria monocytogenes. Infect. Immun. 723849-3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ogura, Y., D. K. Bonen, N. Inohara, D. L. Nicolae, F. F. Chen, R. Ramos, H. Britton, T. Moran, R. Karaliuskas, R. H. Duerr, J. P. Achkar, S. R. Brant, T. M. Bayless, B. S. Kirschner, S. B. Hanauer, G. Nunez, and J. H. Cho. 2001. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature 411603-606. [DOI] [PubMed] [Google Scholar]
- 105.Onderdonk, A. B. 1985. The carrageenan model for experimental ulcerative colitis. Prog. Clin. Biol. Res. 186237-245. [PubMed] [Google Scholar]
- 106.Otte, J. M., and D. K. Podolsky. 2004. Functional modulation of enterocytes by gram-positive and gram-negative microorganisms. Am. J. Physiol. Gastrointest. Liver Physiol. 286G613-G626. [DOI] [PubMed] [Google Scholar]
- 107.Ouellette, A. J. 2004. Defensin-mediated innate immunity in the small intestine. Best Pract. Res. Clin. Gastroenterol. 18405-419. [DOI] [PubMed] [Google Scholar]
- 108.Ouellette, A. J. 1999. IV. Paneth cell antimicrobial peptides and the biology of the mucosal barrier. Am. J. Physiol. 277G257-G261. [DOI] [PubMed] [Google Scholar]
- 109.Ouellette, A. J. 2006. Paneth cell alpha-defensin synthesis and function. Curr. Top. Microbiol. Immunol. 3061-25. [DOI] [PubMed] [Google Scholar]
- 110.Parrillo, J. E. 1993. Pathogenetic mechanisms of septic shock. N. Engl. J. Med. 3281471-1477. [DOI] [PubMed] [Google Scholar]
- 111.Pazgier, M., D. M. Hoover, D. Yang, W. Lu, and J. Lubkowski. 2006. Human beta-defensins. Cell. Mol. Life Sci. 631294-1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Peng, L., Z. He, W. Chen, I. R. Holzman, and J. Lin. 2007. Effects of butyrate on intestinal barrier function in a Caco-2 cell monolayer model of intestinal barrier. Pediatr. Res. 6137-41. [DOI] [PubMed] [Google Scholar]
- 113.Petrof, E. O., K. Kojima, M. J. Ropeleski, M. W. Musch, Y. Tao, C. De Simone, and E. B. Chang. 2004. Probiotics inhibit nuclear factor-κB and induce heat shock proteins in colonic epithelial cells through proteasome inhibition. Gastroenterology 1271474-1487. [DOI] [PubMed] [Google Scholar]
- 114.Phalipon, A., and P. J. Sansonetti. 2007. Shigella's ways of manipulating the host intestinal innate and adaptive immune system: a tool box for survival? Immunol. Cell Biol. 85119-129. [DOI] [PubMed] [Google Scholar]
- 115.Pons, A. M., I. Lanneluc, G. Cottenceau, and S. Sable. 2002. New developments in non-post translationally modified microcins. Biochimie 84531-537. [DOI] [PubMed] [Google Scholar]
- 116.Poxton, I. R., R. Brown, A. Sawyerr, and A. Ferguson. 1997. Mucosa-associated bacterial flora of the human colon. J. Med. Microbiol. 46 85-91. [DOI] [PubMed] [Google Scholar]
- 117.Rachmilewitz, D., K. Katakura, F. Karmeli, T. Hayashi, C. Reinus, B. Rudensky, S. Akira, K. Takeda, J. Lee, K. Takabayashi, and E. Raz. 2004. Toll-like receptor 9 signaling mediates the anti-inflammatory effects of probiotics in murine experimental colitis. Gastroenterology 126520-528. [DOI] [PubMed] [Google Scholar]
- 118.Raetz, C. R., and C. Whitfield. 2002. Lipopolysaccharide endotoxins. Annu. Rev. Biochem. 71635-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Rakoff-Nahoum, S., J. Paglino, F. Eslami-Varzaneh, S. Edberg, and R. Medzhitov. 2004. Recognition of commensal microflora by Toll-like receptors is required for intestinal homeostasis. Cell 118229-241. [DOI] [PubMed] [Google Scholar]
- 120.Raqib, R., P. Sarker, P. Bergman, G. Ara, M. Lindh, D. A. Sack, K. M. Nasirul Islam, G. H. Gudmundsson, J. Andersson, and B. Agerberth. 2006. Improved outcome in shigellosis associated with butyrate induction of an endogenous peptide antibiotic. Proc. Natl. Acad. Sci. USA 1039178-9183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Rath, H. C., J. S. Ikeda, H. J. Linde, J. Scholmerich, K. H. Wilson, and R. B. Sartor. 1999. Varying cecal bacterial loads influences colitis and gastritis in HLA-B27 transgenic rats. Gastroenterology 116310-319. [DOI] [PubMed] [Google Scholar]
- 122.Reichel, P. H., C. Seemann, E. Csernok, J. M. Schroder, A. Muller, W. L. Gross, and H. Schultz. 2003. Bactericidal/permeability-increasing protein is expressed by human dermal fibroblasts and upregulated by interleukin 4. Clin. Diagn. Lab Immunol. 10473-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Relman, D. A. 1999. The search for unrecognized pathogens. Science 2841308-1310. [DOI] [PubMed] [Google Scholar]
- 124.Rosenberger, C. M., R. L. Gallo, and B. B. Finlay. 2004. Interplay between antibacterial effectors: a macrophage antimicrobial peptide impairs intracellular Salmonella replication. Proc. Natl. Acad. Sci. USA 1012422-2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Rytkonen, A., and D. W. Holden. 2007. Bacterial interference of ubiquitination and deubiquitination. Cell Host Microbe 113-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Saitoh, S., S. Noda, Y. Aiba, A. Takagi, M. Sakamoto, Y. Benno, and Y. Koga. 2002. Bacteroides ovatus as the predominant commensal intestinal microbe causing a systemic antibody response in inflammatory bowel disease. Clin. Diagn. Lab Immunol. 954-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Salzman, N. H., M. M. Chou, H. de Jong, L. Liu, E. M. Porter, and Y. Paterson. 2003. Enteric salmonella infection inhibits Paneth cell antimicrobial peptide expression. Infect. Immun. 711109-1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Salzman, N. H., M. A. Underwood, and C. L. Bevins. 2007. Paneth cells, defensins, and the commensal microbiota: a hypothesis on intimate interplay at the intestinal mucosa. Semin. Immunol. 1970-83. [DOI] [PubMed] [Google Scholar]
- 129.Sartor, R. B. 1997. Review article: role of the enteric microflora in the pathogenesis of intestinal inflammation and arthritis. Aliment. Pharmacol. Ther. 11(Suppl. 3)89-96. [Discussion, 11(Suppl. 3)96-97.] [DOI] [PubMed] [Google Scholar]
- 130.Schauber, J., C. Svanholm, S. Termen, K. Iffland, T. Menzel, W. Scheppach, R. Melcher, B. Agerberth, H. Luhrs, and G. H. Gudmundsson. 2003. Expression of the cathelicidin LL-37 is modulated by short chain fatty acids in colonocytes: relevance of signalling pathways. Gut 52735-741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Schauer, D. B. 1997. Paving the way for pathogens? Curr. Biol. 7R75-R77. [DOI] [PubMed] [Google Scholar]
- 132.Schesser, K., A. K. Spiik, J. M. Dukuzumuremyi, M. F. Neurath, S. Pettersson, and H. Wolf-Watz. 1998. The yopJ locus is required for Yersinia-mediated inhibition of NF-κB activation and cytokine expression: YopJ contains a eukaryotic SH2-like domain that is essential for its repressive activity. Mol. Microbiol. 281067-1079. [DOI] [PubMed] [Google Scholar]
- 133.Schmid, D., and C. Munz. 2007. Innate and adaptive immunity through autophagy. Immunity 2711-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Schultsz, C., F. M. Van Den Berg, F. W. Ten Kate, G. N. Tytgat, and J. Dankert. 1999. The intestinal mucus layer from patients with inflammatory bowel disease harbors high numbers of bacteria compared with controls. Gastroenterology 1171089-1097. [DOI] [PubMed] [Google Scholar]
- 135.Schumann, R. R., S. R. Leong, G. W. Flaggs, P. W. Gray, S. D. Wright, J. C. Mathison, P. S. Tobias, and R. J. Ulevitch. 1990. Structure and function of lipopolysaccharide binding protein. Science 2491429-1431. [DOI] [PubMed] [Google Scholar]
- 136.Serhan, C. N. 1997. Lipoxins and novel aspirin-triggered 15-epi-lipoxins (ATL): a jungle of cell-cell interactions or a therapeutic opportunity? Prostaglandins 53107-137. [DOI] [PubMed] [Google Scholar]
- 137.Serhan, C. N. 2005. Novel eicosanoid and docosanoid mediators: resolvins, docosatrienes, and neuroprotectins. Curr. Opin. Clin. Nutr. Metab. Care 8115-121. [DOI] [PubMed] [Google Scholar]
- 138.Shorter, R. G., K. A. Huizenga, and R. J. Spencer. 1972. A working hypothesis for the etiology and pathogenesis of nonspecific inflammatory bowel disease. Am. J. Dig. Dis. 171024-1032. [DOI] [PubMed] [Google Scholar]
- 139.Steiner, T. S., J. P. Nataro, C. E. Poteet-Smith, J. A. Smith, and R. L. Guerrant. 2000. Enteroaggregative Escherichia coli expresses a novel flagellin that causes IL-8 release from intestinal epithelial cells. J. Clin. Investig. 1051769-1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Suski, M. D., D. Zabel, V. Levin, H. Scheuenstuhl, and T. K. Hunt. 1997. Effect of hypoxic hypoxia on transmural gut and subcutaneous tissue oxygen tension. Adv. Exp. Med. Biol. 411319-322. [DOI] [PubMed] [Google Scholar]
- 141.Suzuki, M., T. Hisamatsu, and D. K. Podolsky. 2003. Gamma interferon augments the intracellular pathway for lipopolysaccharide (LPS) recognition in human intestinal epithelial cells through coordinated up-regulation of LPS uptake and expression of the intracellular Toll-like receptor 4-MD-2 complex. Infect. Immun. 713503-3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Swidsinski, A., A. Ladhoff, A. Pernthaler, S. Swidsinski, V. Loening-Baucke, M. Ortner, J. Weber, U. Hoffmann, S. Schreiber, M. Dietel, and H. Lochs. 2002. Mucosal flora in inflammatory bowel disease. Gastroenterology 12244-54. [DOI] [PubMed] [Google Scholar]
- 143.van Deventer, S. J., J. W. ten Cate, and G. N. Tytgat. 1988. Intestinal endotoxemia. Clinical significance. Gastroenterology 94825-831. [DOI] [PubMed] [Google Scholar]
- 144.Viswanathan, V. K., A. Koutsouris, S. Lukic, M. Pilkinton, I. Simonovic, M. Simonovic, and G. Hecht. 2004. Comparative analysis of EspF from enteropathogenic and enterohemorrhagic Escherichia coli in alteration of epithelial barrier function. Infect. Immun. 723218-3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Viswanathan, V. K., R. Sharma, and G. Hecht. 2004. Microbes and their products—physiological effects upon mammalian mucosa. Adv. Drug Deliv. Rev. 56727-762. [DOI] [PubMed] [Google Scholar]
- 146.Vora, P., A. Youdim, L. S. Thomas, M. Fukata, S. Y. Tesfay, K. Lukasek, K. S. Michelsen, A. Wada, T. Hirayama, M. Arditi, and M. T. Abreu. 2004. Beta-defensin-2 expression is regulated by TLR signaling in intestinal epithelial cells. J. Immunol. 1735398-5405. [DOI] [PubMed] [Google Scholar]
- 147.Wall, D. M., W. J. Nadeau, M. A. Pazos, H. N. Shi, E. E. Galyov, and B. A. McCormick. 2007. Identification of the Salmonella enterica serotype Typhimurium SipA domain responsible for inducing neutrophil recruitment across the intestinal epithelium. Cell. Microbiol. 92299-2313. [DOI] [PubMed] [Google Scholar]
- 148.Weersink, A. J., K. P. van Kessel, M. E. van den Tol, J. A. van Strijp, R. Torensma, J. Verhoef, P. Elsbach, and J. Weiss. 1993. Human granulocytes express a 55-kDa lipopolysaccharide-binding protein on the cell surface that is identical to the bactericidal/permeability-increasing protein. J. Immunol. 150253-263. [PubMed] [Google Scholar]
- 149.Wehkamp, J., J. Harder, K. Wehkamp, B. Wehkamp-von Meissner, M. Schlee, C. Enders, U. Sonnenborn, S. Nuding, S. Bengmark, K. Fellermann, J. M. Schroder, and E. F. Stange. 2004. NF-κB- and AP-1-mediated induction of human beta defensin-2 in intestinal epithelial cells by Escherichia coli Nissle 1917: a novel effect of a probiotic bacterium. Infect. Immun. 725750-5758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wehkamp, J., J. Schauber, and E. F. Stange. 2007. Defensins and cathelicidins in gastrointestinal infections. Curr. Opin. Gastroenterol. 23 32-38. [DOI] [PubMed] [Google Scholar]
- 151.Weiss, J. 1994. Purification and assay of bactericidal/permeability-increasing protein. Methods Enzymol. 236173-196. [DOI] [PubMed] [Google Scholar]
- 152.Weiss, J., P. Elsbach, I. Olsson, and H. Odeberg. 1978. Purification and characterization of a potent bactericidal and membrane active protein from the granules of human polymorphonuclear leukocytes. J. Biol. Chem. 2532664-2672. [PubMed] [Google Scholar]
- 153.Weiss, J., P. Elsbach, C. Shu, J. Castillo, L. Grinna, A. Horwitz, and G. Theofan. 1992. Human bactericidal/permeability-increasing protein and a recombinant NH2-terminal fragment cause killing of serum-resistant gram-negative bacteria in whole blood and inhibit tumor necrosis factor release induced by the bacteria. J. Clin. Investig. 901122-1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.White, S. H., W. C. Wimley, and M. E. Selsted. 1995. Structure, function, and membrane integration of defensins. Curr. Opin. Struct. Biol. 5521-527. [DOI] [PubMed] [Google Scholar]
- 155.Wostmann, B. S. 1981. The germfree animal in nutritional studies. Annu. Rev. Nutr. 1257-279. [DOI] [PubMed] [Google Scholar]
- 156.Xavier, R. J., and D. K. Podolsky. 2007. Unravelling the pathogenesis of inflammatory bowel disease. Nature 448427-434. [DOI] [PubMed] [Google Scholar]
- 157.Yan, F., H. Cao, T. L. Cover, R. Whitehead, M. K. Washington, and D. B. Polk. 2007. Soluble proteins produced by probiotic bacteria regulate intestinal epithelial cell survival and growth. Gastroenterology 132562-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Zhou, Z., S. Lin, R. J. Cotter, and C. R. Raetz. 1999. Lipid A modifications characteristic of Salmonella typhimurium are induced by NH4VO3 in Escherichia coli K12. Detection of 4-amino-4-deoxy-l-arabinose, phosphoethanolamine and palmitate. J. Biol. Chem. 27418503-18514. [DOI] [PubMed] [Google Scholar]