Abstract
The Old World arenavirus Lassa virus (LASV) is the causative agent of severe viral hemorrhagic fever (VHF) in humans and is the most prevalent human pathogen among arenaviruses. The present study investigated the largely unknown mechanisms of cell entry of LASV, a process know to be mediated solely by the virus envelope glycoprotein (GP). To circumvent biosafety restrictions associated with the use of live LASV, we used reverse genetics to generate a recombinant variant of the prototypic arenavirus lymphocytic choriomeningitis virus (LCMV) expressing the LASV GP (rLCMV-LASVGP). The rescued rLCMV-LASVGP grew to titers comparable to that of LCMV and showed the receptor binding characteristics of LASV. We used rLCMV-LASVGP to characterize the cellular mechanisms of LASV entry in the context of a productive arenavirus infection. The kinetics of pH-dependent membrane fusion of rLCMV-LASVGP resembled those of the human-pathogenic New World arenavirus Junin virus (JUNV) and other enveloped viruses that use clathrin-mediated endocytosis for entry. However, rLCMV-LASVGP entered cells predominantly via a clathrin-, caveolin-, and dynamin-independent endocytotic pathway similar to the one recently described for LCMV. Productive infection of rLCMV-LASVGP was only mildly affected by a dominant negative mutant of Rab5 and was independent of Rab7, suggesting an unusual mechanism of delivery to endosomes. In addition, rLCMV-LASVGP infection was independent of actin but required intact microtubules. Our data indicate that LASV enters cells via a pathway distinct from the one used by human-pathogenic New World arenaviruses.
The arenaviruses Lassa virus (LASV), Junin virus (JUNV), Guanarito virus (GTOV), Machupo virus (MACV), and Sabia virus (SABV) cause severe viral hemorrhagic fevers (VHF) in humans and represent a serious public health problem (20). While most arenavirus VHF occur sporadically, the Old World arenavirus LASV is an important pathogen that infects several hundred thousand individuals yearly in areas of LASV endemicity in West Africa, resulting in high morbidity and significant mortality (31). Currently, there is no licensed LASV vaccine available and therapeutic options are restricted to supportive care and use of the antiviral ribavirin, which is only partly effective and often associated with severe side effects.
The New World arenavirus JUNV causes Argentine hemorrhagic fever, a severe illness with hemorrhagic and neurological manifestations (57), and MACV, GTOV, and SABV have emerged as causative agents of severe VHF in Bolivia, Venezuela, and Brazil, respectively (42). Apart from the severe humanitarian burden in regions of VHF endemicity, arenaviral VHF cases are regularly imported into metropolitan areas around the globe, placing local populations at risk (18, 22, 51).
Arenaviruses are enveloped viruses with a bisegmented negative-strand RNA genome. Each of the two genomic RNA segments, L (ca. 7.3 kb) and S (ca. 3.5 kb), uses an ambisense coding strategy to direct the synthesis of two polypeptides in opposite orientations, separated by a noncoding intergenic region. The L RNA encodes the viral RNA-dependent RNA polymerase (or L polymerase) and a small RING finger protein Z, which acts as a bona fide matrix protein (41). The S RNA encodes the viral glycoprotein precursor (GPC) and the nucleoprotein (NP). Arenavirus GPC is processed posttranslationally to yield the two mature virion glycoproteins GP1 and GP2. The N-terminal GP1 is located at the top of the glycoprotein (GP) spike and mediates virus interaction with host cell surface receptors (3), and the C-terminal GP2 resembles membrane-proximal fusion-active parts of other viral membrane proteins (17, 19).
A notable difference between Old World and New World arenaviruses is their use of distinct primary cellular receptors. LASV and most isolates of the prototypic Old World virus lymphocytic choriomeningitis virus (LCMV) use α-dystroglycan (α-DG), a cellular surface receptor for proteins of the extracellular matrix (7). In contrast, the human-pathogenic New World arenaviruses JUNV, MACV, GTOV, and SABV use the cellular cargo receptor transferrin receptor 1 (TfR1) (44). Upon receptor binding, arenaviruses undergo endocytosis and are delivered to acidified endosomes, where GP-mediated pH-dependent fusion between the viral and the cellular membrane occurs (4, 8). Consistent with the use of TfR1 as a primary receptor, JUNV enters cells via clathrin-mediated endocytosis (30, 46). In contrast, no particular endocytotic pathway has been associated with α-DG. Electron microscopy examination of LCMV entry demonstrated uptake of virions in noncoated vesicles (4), and we recently reported that LCMV can enter cells via an unusual endocytotic pathway that is independent of clathrin and caveolin and does not require dynamin or actin (46). Intriguingly, a recent study using retroviral pseudotypes of LASV reported a role for clathrin in LASV entry, suggesting similarities in cell entry between LASV and the pathogenic New World arenaviruses (55).
In the present study, we aimed at an in-depth investigation of the currently largely unknown mechanisms of cellular entry of LASV, a process known to be mediated solely by the virus envelope GP. To avoid possible artifacts associated with the use of LASV pseudotypes, we wanted to study cell entry of LASV in the context of a productive arenavirus infection. To circumvent biosafety restrictions associated with the use of live LASV, we used reverse genetics to generate a recombinant LCMV expressing the GP of LASV (rLCMV-LASVGP). The rescued rLCMV-LASVGP grew to titers comparable to that of LCMV and showed the receptor binding characteristics of LASV. The kinetics of pH-dependent membrane fusion of rLCMV-LASVGP resembled those of JUNV. However, productive infection of rLCMV-LASVGP involved a clathrin-, caveolin-, and dynamin-independent endocytotic pathway similar to the one we recently described for LCMV (46). Infection of rLCMV-LASVGP was only mildly affected by dominant negative (DN) Rab5 and was independent of Rab7. While actin was dispensable, infection required intact microtubules. In sum, our data indicate that LASV enters cells via an unusual endocytotic pathway distinct from those used by JUNV and other human-pathogenic New World arenaviruses.
MATERIALS AND METHODS
Proteins and antibodies.
α-DG was purified as reported previously (33). The α-DG-Fc fusion protein and its expression and purification have been described previously (26). Monoclonal antibodies (MAbs) 113 (anti-LCMVNP) and 83.6 (anti-LCMVGP) have been described previously (6, 56), as has MAb 10G4 anti-VSVNP (where VSV is vesicular stomatitis virus) (28). Mouse hyperimmune serum against New World arenaviruses was kindly provided by Christina F. Spiropoulou, Special Pathogens Branch, Centers for Disease Control and Prevention (Atlanta, GA). Rabbit polyclonal antilaminin antibody, mouse MAb to α-tubulin, and rhodamine-labeled phalloidin were purchased from Sigma (St. Louis, MO). Rabbit polyclonal antibody to caveolin-1 was obtained from Santa Cruz Biotechnology, and MAbs to clathrin heavy chain and simian virus 40 (SV40) large T antigen were purchased from BD Biosciences. Rhodamine X-conjugated and fluorescein isothiocyanate-conjugated secondary antibodies were from Jackson Immunoresearch (West Grove, PA) and horseradish peroxidase (HRP)-conjugated secondary antibodies from Pierce (Rockford, IL). 4′-6′-Diamidino-2-phenylindole (DAPI) was from Invitrogen.
Cells and viruses.
African green monkey kidney (Vero E6) cells were maintained in minimal essential medium (Gibco BRL, NY) containing 7% fetal bovine serum and supplemented with glutamine and penicillin-streptomycin. North African green monkey (Cercopithecus aethiops) kidney fibroblasts (CV1) (ATCC CCL-70), human embryonic kidney cells (HEK293T), and Syrian golden hamster kidney cells (BHK-21) were maintained in Dulbecco's modified Eagle's medium (Gibco BRL, NY) containing 10% fetal bovine serum and supplemented with nonessential amino acids, glutamine, and penicillin-streptomycin.
Seed stocks of LCMV ARM53b and clone 13 (cl-13) were prepared by growth in BHK-21 cells and titers determined as reported previously (14). The JUNV Candid 1 vaccine strain was provided by Michael Buchmeier (TSRI) and grown in Vero E6 cells, and titers were determined by plaque assay. VSV stocks were grown in Vero E6 cells and titers determined by plaque assay on Vero E6 cells. SV40 obtained from ATCC was grown in CV1 cells and the titers of virus stocks determined as described previously (39). Retroviral pseudotypes of LASV and JUNV were produced and titers determined as described earlier (47, 48).
Generation of recombinant LCMV containing the GP of LASV.
The open reading frame (ORF) of LASV GP (Josiah) was amplified from pC-LASVGP (26) with primers LFRG1 (5′-GCG AAG CTT CGT CTC TAA GGA TGG GAC AAA TAG TGA CAT TC-3′) and LFRG2 (5′-GCG TCT AGA CGT CTC TTT CTT CAT CTC TTC CAT TTC ACA GGC AC-3′), containing BsmBI restriction sites (underlined) and a HindIII and XbaI site (italics) for subcloning. After PCR amplification with Pfu Turbo polymerase (Stratagene), the resulting 1.6-kb fragment was cut with HindIII and XbaI, subcloned into pBluescript, and sequenced. The LASVGP ORF was cut with BsmBI and inserted into plasmid Pol I-MGNP/Bsm(+), where the LCMVGP ORF was replaced by a double BsmBI cloning site (43). The resulting construct, Pol I-MGNP-Bsm(+)/LASVGP, contains the complete cDNA of the antigenomic S (Sag) RNA segment of LCMV ARM53b, in which the ORF of LCMVGP was replaced by the ORF of LASVGP. The Sag sequence in this construct is flanked at its 5′ end by the promoter sequences of mouse RNA polymerase I (Pol I) and at its 3′ end by the Pol I terminator sequences. Rescue of rLCMV-LASVGP was performed as described previously (50). Briefly, BHK cells (7.5 × 105 per well) were seeded in six-well plates and cotransfected with plasmids encoding LCMVNP (pC-NP; 0.8 μg) and L polymerase (pC-Lv2; 1 μg) and either Pol I-MGNP/Bsm(+)/LASVGP or the control construct Pol I-MGNP/Bsm(+)/LCMVGP containing the GP of LCMV ARM53b (0.8 μg), together with Pol I L(+)v2 (1.4 μg), a plasmid that directs Pol I-mediated intracellular synthesis of the antigenomic L (Lag) RNA segment of LCMV ARM53b. Plasmid DNA was dissolved in 100 μl Optimem and mixed with 100 μl Optimem containing 10 μl Lipofectamine 2000 (Gibco). After 25 min of incubation, 800 μl of Optimem was added and the reaction mix was added to cells. Five hours later, the mix was removed, cells were rinsed in Optimem, and 1.5 ml/well fresh medium with 1% serum was added. Cell culture supernatants were collected after 48, 72, and 96 h. For the detection of infectious virus, serial dilutions of supernatants were added to monolayers of fresh Vero E6 cells. After infection for 1 h, cells were washed twice with medium, fresh medium was added, and cells were incubated for 36 h. Cells were fixed with 2% (wt/vol) paraformaldehyde, and immunostaining for LCMVNP was performed with MAb 113 as described previously (7). Infectious titers in culture supernatant were determined by plaque assay on Vero E6 cells. For the production of initial seed stocks, rLCMV-LASVGP from the 48-h supernatant was used to infect fresh monolayers of BHK21 cells (multiplicity of infection [MOI] of 0.1). Supernatants were harvested after 48 h and titers determined by plaque assay on Vero E6 cells. To verify the expression of LASVGP mRNA from rLCMV-LASVGP, fresh BHK21 cells were infected with rLCMV-LASVGP or LCMV ARM53b at an MOI of 0.1. After 48 h, cells were lysed in Tri reagent and total RNA was extracted. Equal amounts of RNA were subjected to reverse transcription-PCR (RT-PCR) with primers LFVGPC1 (at bp 586), 5′ TGG GGT GGG AGC TAC ATT GCT CTT 3′ (amino acid sequence WGGSYIAL); LFVGPC2 (at bp 1005), 5′ CTG AAT GCT CAT TTG TGC TTC AGC GC 3′ (amino acid sequence AEAQMSIQ); LFVGPC3 (at bp 199), 5′ GCG AGC TTC AGA CTC TGG AAC TAA AC 3′ (amino acid sequence ELQTLELN); and LFVGPC4 (at bp 978), 5′ CAA CCT TTG AAT GGC TTG GC 3′ (amino acid sequence QAIQRL).
Detection of LCMV, LASVGP2, and LCMVNP by ELISA.
For the determination of the GP/NP ratios in rLCMV-LASVGP and LCMV ARM53b, three independent preparations of viruses were analyzed for each variant studied. Viruses were isolated from cell culture supernatants by ultracentrifugation through a 20% sucrose cushion as described previously (24) and resuspended in Hanks' balanced salt solution overnight, and infectious titers were determined by plaque assay. Viruses were diluted to 106 PFU/ml in Hanks' balanced salt solution and coated in triplicate wells in 96-well EIA/RIA high-bond microtiter plates (Corning) for 2 h at 6°C, and nonspecific binding was blocked with 1% (wt/vol) bovine serum albumin (BSA)-phosphate-buffered saline (PBS). For the detection of NP, immobilized viruses were fixed with 2% (wt/vol) paraformaldehyde in PBS, washed three times in PBS, and treated with 0.1% (wt/vol) Triton X-100 for 10 min at room temperature. MAbs 83.6 (anti-LCMVGP2) and 113 (anti-LCMVNP) were applied at a 1:100 dilution for 2 h at 6°C and detected with peroxidase-conjugated anti-mouse immunoglobulin G (IgG) (1:1,000) in a color reaction using ABTS [2,2′azino-bis(3-ethylbenzthiazoline-6-sulfonic acid)] substrate. The optical density at 405 nm (OD405) was measured with an enzyme-linked immunosorbent assay (ELISA) reader. For the determination of specific binding, background binding to BSA was subtracted. GP2/NP ratios were calculated for each preparation individually: the average OD405 of the GP2 signal was divided by the average OD405 of the NP signal (n = 3) (means ± standard deviations [SD]).
Virus infection of cells.
For infection of cells with viruses, seed stocks were diluted to the indicated MOI and added to cells for 1 h at 37°C. After 1 h of incubation at the indicated temperature, the inoculum was removed, and the cells were washed twice with medium without serum and incubated for the indicated time periods at 37°C, 5% CO2. Infection was quantified by immunofluorescence (IF) detection of LCMVNP and VSVNP using MAbs 113 (anti-LCMVNP) and 10G4 (anti-VSVNP) combined with fluorescence-labeled secondary antibodies (7). Blocking of virus infection with soluble α-DG was performed as described previously (7). Ammonium chloride treatment was performed as described previously (4). Monolayers of CV1 and HEK cells were cooled on ice for 5 min and viruses added at an MOI of 3. After incubation for 2 h on ice, unbound virus was washed off and cells were quickly shifted to 37°C. After the indicated time points, 20 mM ammonium chloride was added to the medium and kept throughout the experiment. After a total of 16 h, cells were fixed and LCMVNP was detected by IF as described previously (7).
Infection assays with the wild type and DN mutants of caveolin-1, dynamin, and Eps15.
Wild-type green fluorescent protein (GFP)-tagged caveolin-1 (39) and the GFP-tagged DN caveolin-1 mutant caveolin-1Y14F (11) were provided by Jeffrey M. Bergelson (University of Pennsylvania). GFP-tagged wild-type and DN (K44E) dynamin I and dynamin II (54) were kindly provided by Sandra L. Schmid (TSRI). For analysis of the clathrin-mediated entry pathway of arenaviruses, the control Eps15DIIIΔ2 construct (2) and the DN Eps15Δ95/295 mutant construct (1) were provided by Alice Daurty-Varsat and Nathalie Sauvonnet (Institut Pasteur, Paris, France). Constructs of wild-type GFP-tagged human Rab5A and human Rab7 as well as the constitutively inactive Rab5 S34N and Rab7 T22N mutants (52, 53) were provided by Craig Roy (Yale University School of Medicine, New Haven, CT).
The impact of transgene expression on virus infection was assessed as described previously (46). Briefly, cells were transiently transfected with plasmid DNA by using either Superfect reagent (Qiagen) or the Nucleofector system (Amaxa, Gaithersburg, MD) according to the manufacturer's protocols. Transfection efficiencies with plasmids, as assessed by detection of GFP, were 40 to 60% for CV1 cells and >80% for HEK293 cells. Cells expressing GFP-tagged constructs for 16 to 24 h were infected with rLCMV-LASVGP, JUNV Candid 1, or VSV at the indicated MOI as described above and analyzed for expression of LCMVNP or JUNV antigen after 12 to 16 h, or in the case of VSV after 6 h, by IF staining (46). In three independent transfections, at least 100 cells with comparable levels of transgene expression were screened and cells positive for viral antigen scored. Fluorescent images were captured using a Zeiss Axiovert S100 microscope (Carl Zeiss Inc., Thornwood, NY) with a 20× objective and an AxioCam digital camera. Images were assembled using Adobe Photoshop.
To compare the effects of the DN mutants on infection with rLCMV-LASVGP, JUNV Candid 1, and retroviral pseudotypes of LASV and JUNV, HEK293 cells were transfected with GFP-tagged DN mutants and wild-type Eps15, dynamin II, and caveolin-1 by using nucleofection. The transfection efficiency was >90%, as assessed by detection of GFP. Twenty-four hours postnucleofection, cells were infected with rLCMV-LASVGP and JUNV at the indicated MOI or with retroviral pseudotypes of LASV and JUNV at an MOI of 1. rLCMV-LASVGP and JUNV infections were detected as described above. Pseudotype infection was assessed after 24 h by use of a SteadyGlo luciferase assay (Promega) as described previously (47, 48).
Pharmacological inhibitors.
Inhibitor drugs to study the role of the actin cytoskeleton were used at concentrations and incubation times described previously (11, 13, 40). Cytochalasin D (Sigma) was used at 25 μg/ml, latrunculin A (Calbiochem) at 1 μM, jasplakinolide (Invitrogen) at 500 nM, and nocodazole (Sigma) at 10 μM. Unless indicated otherwise, inhibitors were added at the indicated time points and were present for the duration of the experiment.
Immunoblotting and solid-phase virus-binding assay.
Standard immunoblotting involved proteins being separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis and transferred to nitrocellulose. After blocking in 5% (wt/vol) skim milk in PBS was completed, membranes were incubated with 10 μg/ml primary antibody, MAb 83.6 anti-LCMVGP2, rabbit polyclonal antibody anti-caveolin-1, and MAb anti-α-tubulin (diluted in 2% [wt/vol] skim milk-PBS) and incubated overnight at 6°C. After several washes in PBS-0.1% (wt/vol) Tween 20, secondary antibodies coupled to HRP were applied 1:5,000 in PBS-0.1% (wt/vol) Tween 20 for 1 h at room temperature. Blots were developed using Super Signal West Pico ECL substrate (Pierce).
For binding of α-DG-Fc fusion proteins to LCMV, viruses were pelleted from the supernatant by ultracentrifugation through a sucrose cushion (24). Pellets were resuspended overnight and viral titers determined by plaque assay on Vero E6 cells. Equal concentrations of virus (106 PFU/ml) were immobilized in microtiter plates and incubated with the α-DG-Fc fusion proteins. Bound α-DG-Fc was detected with HRP-conjugated anti-human IgG Fc (1:1,000) or a combination of mouse anti-human IgG Fc (1:500) and HRP-conjugated goat anti-mouse IgG (1:500). Assays were developed with ABTS substrate, and the OD405 was recorded in an ELISA reader. Background binding to BSA was subtracted.
RNA interference (RNAi).
For the depletion of clathrin heavy chain from HEK293 cells, siGENOME ON-TARGETplus SMARTpool duplex (J-004001-09) to human clathrin heavy chain and a control small interfering RNA (siRNA) pool was obtained from Dharmacon Research (Lafayette, CO). A pool of the following siRNAs was used: siRNA no. 1, 5′-GAG AAU GGC UGU ACG UAA U-3′; no. 2, 5′-UGA GAA AUG UAA UGC GAA U-3′; no. 3, 5′-GCA GAA GAA UCA ACG UUA U-3′; and no. 4, 5′-CGU AAG AAG GCU CGA GAG U-3′. For depletion of caveolin-1 from HEK293 and CV1 cells, siGENOME ON-TARGETplus SMARTpool duplex (J-003467-06) to human caveolin-1 (Dharmacon) was used, which consisted of the following siRNAs: no. 1, 5′-CUA AAC ACC UCA ACG AUG AUU-3′; no. 2, 5′-GCA AAU ACG UAG ACU CGG AUU-3′; no. 3, 5′-GCA GUU GUA CCA UGC AUU AUU-3′; and no. 4, 5′-GCA UCA ACU UGC AGA AAG AUU-3′. The siRNA no. 2, 3, and 4 targeting human caveolin-1 cDNA (GenBank accession no. NM_001753) perfectly match the corresponding sequences in the caveolin-1 cDNA of Cercopithecus aethiops (GenBank accession no. DP000029), from which CV1 cells are derived. The siRNA no. 1 contains one mismatch, U-C, between the human and Cercopithecus aethiops sequences (underlined). Depletion of clathrin heavy chain and caveolin-1 was performed as described previously (46). Briefly, cells (2 × 104 cell/well) were seeded in 96-well plates and transfected with siRNAs at concentrations of 50 nM per siRNA, corresponding to a total concentration of 200 nM (4 × 50), using Lipofectamine 2000. After 48 h, cells were lysed and depletion of clathrin heavy chain and caveolin-1 was detected by Western blot analysis, using α-tubulin for normalization. Parallel samples were infected with rLCMV-LASVGP, JUNV Candid 1, or SV40 (200 PFU/well), and virus infection was assessed by IF as described previously (46).
RESULTS
Generation and characterization of a recombinant LCMV expressing the envelope GP of LASV.
Since LASV is a biosafety level 4 (BSL4) pathogen, biosafety concerns restrict work with the live virus. To be able to study LASVGP-mediated cell entry in the context of a productive arenavirus infection outside of BSL4 facilities, we used reverse-genetics approaches (50) to generate a recombinant LCMV where LASVGP substituted for the LCMV (strain ARM53b) GP. The generation and use of rLCMV-LASVGP under BSL2 conditions were considered safe upon review by the Institutional Biosafety Committee based on the following facts. (i) The ORF of LASVGP comprises only 15% of the genetic material of LASV (5). (ii) LASV and LCMV use the same highly conserved primary receptor (7) and show very similar cellular tropisms (45, 47), strongly supporting that rLCMV-LASVGP would not exhibit significant differences in infectious potential compared to LCMV. (iii) Studies of genetic reassortants between LASV and the related nonpathogenic Mopeia virus demonstrated that virulence always correlated with the presence of the L RNA segment of LASV but not the S RNA segment that encodes the GP (29). Based on these considerations, rescue and experimentation with rLCMV-LASVGP described in this study were performed under BSL2 conditions with extra safety precautions (BSL2+).
Rescue of rLCMV-LASVGP was done using procedures similar to those published previously (50) and detailed in Materials and Methods. Briefly, cells were cotransfected with plasmids pC-L and pC-NP, together with plasmids that allowed for Pol I-mediated intracellular synthesis of the Lag and Sag RNA species (Fig. 1A). As a negative control, cells were transfected with a plasmid cocktail lacking pC-L, and as a positive control for the experimental conditions we also rescued a wild-type rLCMV (rLCMV-WT) by using in the transfection cocktail plasmid Pol I-MGNP/Bsm(+)/LCMVGP (ARM53b) instead of Pol I-MGNP/Bsm(+)/LASVGP.
FIG. 1.
Rescue of rLCMV-LASVGP. (A) Schematics of plasmids encoding antigenomic LCMV S and L RNA Pol I-MGNP-Bsm(+)/LASVGP and Pol I L(+)v2, respectively, flanked by a Pol I promoter and a Pol I terminator (Pol I ø). The ORFs for LCMVNP (NP), LASVGP, LCMV L (L), and LCMV Z (Z), as well as the intergenic region (IRG) separating the ORFs and the flanking untranslated regions (UTR) derived from LCMV, are indicated (for details, see the text). (B) Detection of LASVGP mRNA in cells infected with rLCMV-LASVGP. BHK21 cells were infected with rLCMV-LASVGP or LCMV ARM53b or were mock infected (−). As a positive control, cells were transfected with an expression plasmid for LASVGP (pC-LASVGP). After 48 h, the total RNA was extracted and equal amounts of total RNA were subjected to RT-PCR with LASVGP-specific primer sets to amplify fragments of 419 bp and 779 bp. Primers to the GAPDH (glyceraldehyde-3-phosphate dehydrogenase) housekeeping gene were used for normalization. (C) Detection of LASVGP2 and LCMVGP2 in infected cells. Vero E6 cells were infected with rLCMV-LASVGP, rLCMV-LCMVGP, or LCMV ARM53b or were mock infected (−). After 48 h, the total protein was extracted, separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis, and blotted to nitrocellulose. Blots were probed with MAb 83.6 to arenavirus GP2. Bound primary antibody was detected with HRP-conjugated secondary antibody and enhanced chemiluminescence. Note the significant shift in the apparent molecular mass of GP2 detected in cells infected with rLCMV-LASVGP. (D) Growth of rLCMV-LASVGP. Vero E6 cells were infected with rLCMV-LASVGP or wild-type LCMV ARM53b (MOI of 0.1), and virus titers in the supernatants were determined after the indicated time points. (E) Detection of GP2 and LCMVNP in rLCMV-LASVGP and LCMV ARM53b. Immobilized rLCMV-LASVGP (column 1), LCMV ARM53b (column 2), and VSV (column 3) were probed with MAb 83.6 to GP2 and MAb 113 to LCMVNP during ELISA (for details, see Materials and Methods), and GP2/NP ratios were calculated (n = 3) (means ± SD). (F) Infection of rLCMV-LASVGP is blocked by soluble α-DG. Two hundred PFU of rLCMV-LASVGP, LCMV ARM53b, and VSV was incubated with the indicated concentrations of soluble α-DG and added to monolayers of Vero E6 cells. Infection was assessed after 16 h by immunostaining for LCMVNP using MAb 113 (n = 3) (means ± SD). (G) Binding of α-DG-Fc to virus. The indicated viruses were immobilized in microtiter plates and incubated with purified α-DG-Fc, which was detected with an HRP-conjugated anti-human Fc antibody in a color reaction using ABTS substrate (n = 3) (means ± SD).
Cell culture supernatant was collected 48, 72, and 96 h after transfection and tested for the presence of infectious rLCMV by infecting fresh monolayers of Vero E6 cells and detection of LCMVNP by IF at 36 h postinfection (p.i.). Infectious virus was readily detected in the supernatants collected from cells transfected with Pol I-MGNP/Bsm(+)/LASVGP or Pol I-MGNP/Bsm(+)/LCMVGP but not from cells transfected with the control plasmid cocktail lacking pC-L.
We next conducted a series of studies to characterize and validate the use of rLCMV-LASVGP as a surrogate virus to study LASV cell entry in the context of a productive arenavirus infection. To this end, we first confirmed the production of LASVGP mRNA in cells infected with rLCMV-LASVGP. For this, we exploited the fact that the nucleotide sequence of LASVGP differs significantly from that of LCMVGP, allowing the design of LASVGP-specific primer sets for detection of LASVGP mRNA by RT-PCR. RT-PCR performed on RNA isolated from cells infected with rLCMV-LASVGP, but not from mock-infected or rLCMV-WT-infected cells, yielded bands of the expected length (Fig. 1B).
GP2 of LASV (Josiah) and GP2 of LCMV (ARM53b) differ by only one amino acid. However, LASVGP2 contains four putative N-glycosylation sites (positions 367, 375, 392, and 397), whereas LCMV contains only three (positions 373, 398, and 403) (15, 19). Since all four N-glycosylation sites of LASVGP2 are used in mammalian cells (15), we predicted a significant shift in the apparent molecular mass of LASVGP2 compared to that of LCMVGP2. To confirm this prediction and also to assess the correct N glycosylation of LASVGP2 expressed from rLCMV-LASVGP, we infected Vero E6 cells with rLCMV-LASVGP, rLCMV-WT, and parental LCMV ARM53b. At 48 h p.i., we prepared cell lysates that were analyzed by Western blotting using MAb 83.6, which recognizes a linear epitope within GP2 that is completely conserved between LASV and LCMV (56). As predicted, GP2 detected in cells infected with rLCMV-LASVGP revealed a significantly higher apparent molecular mass than GP2 of cells infected with rLCMV-WT or parental LCMV ARM53b (Fig. 1C).
Growth kinetics studies showed that rLCMV-LASVGP exhibited a mildly attenuated growth phenotype in Vero E6 cells compared to that of LCMV ARM53b (Fig. 1D). This led us to examine a possible decreased efficiency of incorporation of GP into the viral core. To this end, we quantitatively assessed the ratios of GP2 to NP in virion particles. Virus present in culture supernatants of infected cells was pelleted by ultracentrifugation through a sucrose cushion and immobilized in microtiter plates, and NP and GP2 were detected by ELISA using MAb 83.6 (anti-GP2) and MAb 113 (anti-LCMVNP) as described previously (27). Similar ratios of GP2 versus NP were obtained for rLCMV-LASVGP and LCMV ARM53b (Fig. 1E).
A marked difference between LCMV ARM53b and LASV lies in their distinct binding affinities to and levels of dependence on their primary receptor, α-DG. While LASV binds α-DG with high affinity (low nanomolar KD [equilibrium dissociation constant]), LCMV ARM53b has a ca.-100-fold-lower receptor binding affinity (7). Consistent with this, infection of cells with rLCMV-LASVGP was strongly inhibited, with low nanomolar concentrations of soluble α-DG, while only a weak reduction in LCMV ARM53b infection was observed (Fig. 1F). Likewise, the α-DG binding affinity of rLCMV-LASVGP, as assessed in a solid-phase virus-binding assay (25), was similar to that of inactivated LASV and significantly higher than that of LCMV ARM53b (Fig. 1G). Together, the data indicate that the rescued rLCMV-LASVGP is a virus of relatively high fitness that efficiently incorporates LASVGP and adopts the receptor binding characteristics of LASV. It is therefore a powerful tool to study the cellular mechanisms of LASV entry in the context of productive arenavirus infection.
rLCMV-LASVGP and JUNV exit acidic endosomes with similar kinetics.
Upon receptor binding, arenaviruses are taken up by endocytosis and delivered to acidified endosomes, where low-pH-dependent membrane fusion occurs (4, 8). To determine how fast receptor-bound rLCMV-LASVGP and JUNV traffic to endosomes and undergo membrane fusion, we determined the time required for the viruses to become resistant to the lysosomotropic agent ammonium chloride. When added to cells at a concentration of 20 mM, ammonium chloride raises the endosomal pH rapidly and blocks low-pH-dependent cellular processes without causing overall cytotoxicity (36, 37). To allow virus binding to the receptor without virus internalization, CV1 and HEK293 cells were incubated with rLCMV-LASVGP and the JUNV vaccine strain Candid 1 at 4°C for 2 h. Unbound virus was removed, and cells were quickly shifted to 37°C to allow virus internalization. After different time points, 20 mM ammonium chloride was added to cells and kept throughout the experiment. At 16 h p.i., cells were fixed and infection was assessed by IF using antibodies to LCMVNP (rLCMV-LASVGP) and a mouse hyperimmune serum to New World arenaviruses (JUNV). In both cell types, rLCMV-LASVGP and JUNV showed similar kinetics of resistance to ammonium chloride inhibition (Fig. 2).
FIG. 2.
Kinetics of endosomal trafficking and pH-dependent membrane fusion of rLCMV-LASVGP and JUNV. Monolayers of chilled CV1 and HEK293 cells were incubated with rLCMV-LASVGP and JUNV (MOI of 3) on ice for 2 h. Cells were washed and quickly shifted to 37°C. Ammonium chloride (20 mM) was added at the indicated time points and kept throughout the experiment. After a total incubation of 16 h, cells were fixed and infection was assessed by immunostaining for LCMVNP as described in the legend for Fig. 1F.
Productive infection of rLCMV-LASVGP occurs predominantly via a clathrin-, caveolin-, and dynamin-independent endocytotic pathway.
To characterize the entry pathway used by LASV, we examined the effects on rLCMV-LASVGP infection of a series of well-characterized DN mutants for cellular proteins associated with clathrin-mediated endocytosis, the caveolar/raft pathway, or both. To address the involvement of clathrin-mediated endocytosis, we used the DN mutant of the clathrin coat-associated protein Eps15, Eps15Δ95/295, which specifically interferes with clathrin-coated pit assembly without affecting clathrin-independent endocytotic pathways (2, 34). Since clathrin-mediated endocytosis depends critically on the GTPase dynamin, we also investigated the effects of the DN K44A mutants of dynamin I and dynamin II, which efficiently block both clathrin-mediated and caveolar endocytosis (12, 35, 54). To address a possible involvement of caveolae in productive infection of rLCMV-LASVGP, we used the DN caveolin-1 mutant caveolin-1Y14F, which cannot undergo phosphorylation at tyrosine Y14 and has been shown to block caveolar entry of other viruses (11).
The impact of the expression of DN mutants on virus infection was assessed as reported previously (46). Briefly, CV1 and HEK293 cells were transfected with GFP-tagged versions of the wild-type forms or the DN mutants. Twenty hours posttransfection, cells were infected with either rLCMV-LASVGP or JUNV Candid 1. At 16 h p.i., cells were fixed and analyzed by IF for viral antigen expression. Cells expressing similar levels of the GFP-tagged wild type and DN mutants were selected and those expressing viral antigens scored (46). Expression of DN Eps15, dynamin I, dynamin II, and caveolin-1 did not significantly affect infection with rLCMV-LASVGP in CV1 cells (Fig. 3A and B). While rLCMV-LASVGP infection in HEK293 cells was not affected by DN dynamin I, dynamin II, or caveolin-1, expression of DN Eps15 resulted in a small but apparently statistically significant reduction in infection. As expected, the DN mutants of dynamin I, dynamin II, and Eps15, but not caveolin-1, inhibited infection with JUNV, which uses clathrin-mediated endocytosis (30). The residual infection with JUNV of cells transfected with DN dynamin I, dynamin II, and Eps15 may occur either because of incomplete inhibition of clathrin-mediated endocytosis by the DN mutants or because a fraction of JUNV can enter cells via a different endocytotic route.
FIG. 3.
Productive infection of rLCMV-LASVGP is largely independent of clathrin, caveolin, and dynamin. (A) CV1 cells were transfected with the GFP-tagged wild type and DN mutants of Eps15, dynamin I (Dyn I), dynamin II (Dyn II), and caveolin-1 (Cav-1). Twenty hours posttransfection, cells were infected with either rLCMV-LASVGP or JUNV. After 16 h, cells were fixed and infection was assessed by IF detection of LCMVNP or JUNV antigen using a rhodamine Red X-conjugated secondary antibody (red). Cell nuclei were counterstained with DAPI. Arrows indicate individual transfected cells. Bar = 20 μm. (B) Quantification of data shown in panel A for CV1 and HEK293 cells. One hundred cells with similar levels of transgene expression, as assessed by intensity of the GFP signal, were screened, and cells positive for viral antigen were scored (n = 3) (means ± SD).
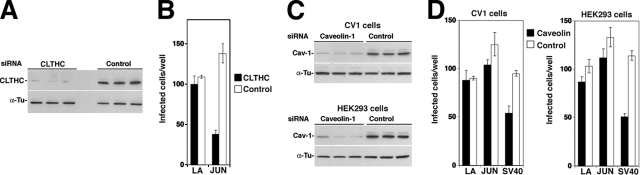
To address the role of clathrin-mediated endocytosis in rLCMV-LASVGP infection in HEK293 cells in a complementary manner, we depleted clathrin heavy chain by using RNAi. For this purpose, a pool of four siRNAs targeting the ORF of human clathrin heavy-chain polypeptide was used (for details, see Materials and Methods). Depletion of clathrin heavy-chain mRNA by specific siRNAs resulted in a >90% reduction in protein expression after 48 h, as assessed by Western blot analysis (Fig. 4A). Subsequent infection with rLCMV-LASVGP was not significantly affected, whereas infection with JUNV Candid 1 was markedly reduced (Fig. 4B). Together with the results obtained with DN Eps15, the data indicate that the main route of cellular entry of rLCMV-LASVGP is clathrin independent.
FIG. 4.
Infection with rLCMV-LASVGP is independent of clathrin and caveolin-1. (A) Depletion of clathrin heavy chain (CLTHC) by RNAi. Triplicate samples of HEK293 cells were transfected with either a pool of siRNA targeting CLTHC (50 nM per siRNA, 200 nM total concentration) or control siRNA (200 nM). After 48 h, cells were lysed and expression of CLTHC was assessed by Western blotting. For normalization, α-tubulin (α-Tu) was detected. (B) Infection with rLCMV-LASVGP does not depend on CLTHC. Cells transfected with siRNA to either CLTHC or control siRNAs (Control), as described for panel A, were infected with 200 PFU of rLCMV-LASVGP (LA) and JUNV (JUN). After 16 h, cells were fixed and infection was assessed by detection of viral antigen as described in the legend for Fig. 3. Cells positive for viral antigen were scored (n = 3) (means ± SD). (C) Depletion of caveolin-1 from CV1 and HEK293 cells by RNAi. Triplicate samples of CV1 and HEK293 cells were transfected with either a pool of siRNA targeting caveolin-1 (50 nM per siRNA, 200 nM total concentration) or control siRNA (200 nM). After 48 h, cells were lysed and caveolin-1 and α-tubulin detected by Western blotting. (D) Caveolin depletion does not affect infection with rLCMV-LASVGP. Cells subjected to RNAi, as described for panel A, were infected with 200 PFU of rLCMV-LASVGP, JUNV, or SV40. Cells were fixed after 16 h. Infection with rLCMV-LASVGP and JUNV was assessed as described for panel B. For detection of SV40 infection, cells were stained with an antibody to SV40 T antigen and a fluorescence-conjugated secondary antibody. Cells positive for viral antigen were scored (n = 3) (means ± SD).
Since the DN mutant caveolin-1Y14F perturbs some functions of caveolin-1 but not others, we also used as a complementary approach RNAi-mediated depletion of caveolin-1. Efficient depletion of caveolin-1 in CV1 and HEK293 cells by RNAi was confirmed by Western blot analysis, showing a >80% reduction in caveolin-1 protein expression 48 h after siRNA transfection (Fig. 4C). Cells depleted of caveolin-1 by RNAi showed normal susceptibility to rLCMV-LASVGP and JUNV (Fig. 4D) but reduced infection with SV40 (Fig. 4D), which enters via the caveolar/raft pathway (39, 40). The reduction of only ca. 50% in SV40 entry despite the >80% depletion of caveolin-1 is in line with a previously published report (38) and suggests that low numbers of functional caveolae are sufficient to allow SV40 to enter.
In sum, our data indicate that rLCMV-LASVGP enters cells predominantly via a clathrin-, caveolin-, and dynamin-independent pathway. These findings were in apparent contradiction to an earlier study in which expression of DN Eps15 had reduced infection of Vero E6 cells with retroviral pseudotypes bearing LASVGP (55). The reasons for this discrepancy are unclear but might be due to the use of replication-deficient retroviral pseudotypes with a reporter gene readout in the previously published report (55) versus productive arenavirus infection used in our study. We therefore directly compared the effects of DN Eps15, dynamin II, and caveolin-1 on infection with rLCMV-LASVGP and JUNV Candid 1 on the one hand and retroviral pseudotypes of LASV and JUNV on the other hand. Retroviral pseudotypes of LASV and JUNV containing a luciferase reporter gene were produced as described previously (47, 48). For our comparative study, HEK293 cells were transfected with the GFP-tagged wild type and DN mutants of Eps15, dynamin II, and caveolin-1 using nucleofection, which resulted in >90% transfection efficiency. After 24 h, cells were infected with either rLCMV-LASVGP and JUNV Candid 1 or retroviral pseudotypes of LASV and JUNV. Infection with rLCMV-LASVGP and JUNV was assessed by detection of viral antigen as described above, and pseudotype infection was quantified by luciferase assay. As shown in Fig. 5, the DN mutants affected infection with the live viruses and the pseudotypes in similar ways, excluding fundamental differences between the systems, at least in this context. The apparent differences in the role of clathrin for LASV entry between the previously published report (55) and our present study may instead be due to cell type-specific variation.
FIG. 5.
Comparison of the effects of DN mutants of Eps15, dynamin II, and caveolin-1 on infection with live arenaviruses and retroviral pseudotypes. HEK293 cells were transfected with GFP-tagged DN and wild-type Eps15, dynamin II, and caveolin-1 using nucleofection, resulting in >90% transfection efficiency, as assessed by detection of GFP. After 24 h, cells were infected with (A) rLCMV-LASVGP and JUNV Candid 1 and (B) retroviral pseudotypes of LASV (LASV-PS) and JUNV (JUNV-PS). Infection with rLCMV-LASVGP and JUNV was quantified as described in the legend for Fig. 3B. To detect infection with pseudotypes, a luciferase reporter assay was performed. Luminescence is given as increase (n-fold) over background (n = 3) (means ± SD). Note that overexpression of wild-type Eps15 consistently resulted in low infection levels compared to those of the other wild-type proteins.
rLCMV-LASVGP infection is mildly affected by DN Rab5 and independent of Rab7.
Recent studies employing cell-cell fusion assays with recombinant LASVGP (Josiah) documented a remarkably acidic fusion pH of <4.5 for LASV (23), suggesting an unusual pattern of endosomal trafficking. To gain initial information about the cellular route of endosomal delivery of LASV, we examined the roles of the small Rab GTPases Rab5 and Rab7 in productive infection with rLCMV-LASVGP. Rab5 and Rab7 are implicated in vesicular trafficking to and from early and late endosomal compartments, respectively (21, 59). Constitutively inactive (DN) mutant versions of these Rab proteins have been used to study vesicular trafficking pathways of viruses within the endosomal compartment (52, 53). CV1 and HEK293 cells were transfected with GFP-tagged constructs expressing wild-type and DN Rab5 and Rab7. Twenty-four hours later, cells were infected with rLCMV-LASVGP. As a control, we used VSV, which has a fusion pH of >6 and requires Rab5, but not Rab7, for productive infection (52). Cells were fixed after 6 h (VSV) or 16 h (rLCMV-LASVGP), and infected cells were identified by IF. The percentage of infected cells expressing a transgene was determined as described in the legend for Fig. 3. Consistent with published results (52), infection of VSV was specifically reduced in cells expressing DN Rab5 but not DN Rab7 (Fig. 6). In contrast, productive infection of rLCMV-LASVGP was only mildly reduced in cells expressing DN Rab5 and not significantly affected in cells transfected with DN Rab7 (Fig. 6).
FIG. 6.
Productive infection with rLCMV-LASVGP is only mildly perturbed by DN Rab5 and independent of Rab7. CV1 and HEK293 cells were transfected with the GFP-tagged wild type and DN Rab5 S34N and Rab7 T22N mutants. Forty hours posttransfection, cells were infected with either rLCMV-LASVGP or VSV at an MOI of 5. After 6 h for VSV and after 16 h for rLCMV-LASVGP, cells were fixed and infection was assessed by IF detection of LCMVNP or VSVNP using a rhodamine Red X-conjugated secondary antibody. Cell nuclei were counterstained with DAPI. For quantification, 100 cells with similar levels of transgene expression, as assessed by intensity of the GFP signal, were screened, and cells positive for viral antigen were scored (n = 3) (means ± SD).
Early infection with rLCMV-LASVGP is independent of actin but requires intact microtubules.
To address a possible role of the actin cytoskeleton in early steps of LASV infection, we investigated whether infection with rLCMV-LASVGP was affected in cells treated with cytochalasin D or latrunculin A, which disrupts actin fibers, as well as jasplakinolide, an actin polymer-stabilizing drug that blocks the dynamics of actin filaments. Actin dependence of infection with rLCMV-LASVGP was compared to that of infection with the LCMV isolate cl-13, whose cell entry was previously found to be actin independent (4, 46). When added to CV1 cells for 30 min, cytochalasin D, latrunculin A, and jasplakinolide induced the expected changes in the cellular actin cytoskeleton, as reported previously (46), but did not affect infection with rLCMV-LASVGP or LCMV (Fig. 7). This indicates that neither the structural integrity nor the dynamics of the actin cytoskeleton are required for productive infection of rLCMV-LASVGP.
FIG. 7.

Productive infection of rLCMV-LASVGP is independent of actin. CV1 cells were treated with 1 μM latrunculin A (Lat A), 500 nM jasplakinolide (Jas), or 25 μg/ml cytochalasin D (Cyto D) for 1 h or left untreated (Control). Cells were then infected with 200 PFU of rLCMV-LASVGP or LCMV cl-13 (LCMV), and infection was detected by immunostaining for LCMVNP (n = 3) (means ± SD).
To investigate the role of microtubules in the early steps of a productive infection with rLCMV-LASVGP and LCMV cl-13, we examined the effect of nocodazole, which causes a dramatic disruption of microtubular structures (Fig. 8A). To assess a possible role of microtubules in viral entry, nocodazole was added at different times pre- or postinfection and left throughout the experiment. Addition of nocodazole prior to or at the time of infection significantly reduced infection with rLCMV-LASVGP and LCMV, with only a mild reduction when nocodazole was added after 2 or 6 h (Fig. 8B). A more kinetic experiment with multiple time points revealed a wider time window of inhibition of rLCMV-LASVGP infection for nocodazole (Fig. 8C) than for ammonium chloride (Fig. 2). This suggests that nocodazole also affects steps in early infection that occur after pH-dependent membrane fusion in the endosome. Together, the data indicate that early infection with rLCMV-LASVGP and LCMV is independent of actin but requires intact microtubules.
FIG. 8.
Disruption of microtubules perturbs early infection of rLCMV-LASVGP and LCMV. (A) Disruption of microtubules with nocodazole. CV1 cells treated with nocodazole were immunostained with MAb anti-α-tubulin (α-Tubulin), and actin filaments were detected with phalloidin conjugated to rhodamin (Actin). Bar = 10 μM. (B) Treatment with nocodazole affects an early step of infection with rLCMV-LASVGP and LCMV. CV1 cells were either left untreated (control) or treated with nocodazole 1 h prior to infection (−1 h), at the time of infection (0 h), or at 2 h and 6 h p.i. After a total of 16 h, infection was assessed by staining for LCMVNP (n = 3) (means ± SD). (C) Kinetics of nocodazole sensitivity of rLCMV-LASVGP infection. Either CV1 cells were left untreated or nocodazole was added at the indicated time points of infection. Virus infection was assessed as described for panel B (n = 3) (means ± SD).
DISCUSSION
To circumvent biosafety restrictions associated with the use of live LASV, different pseudotype systems have been used over the years to study the mechanisms of LASVGP-mediated cell attachment and entry (25, 26, 45, 47, 55). While of great value for many applications, pseudotypes do not allow the study of LASV cell entry in the context of productive arenavirus infection. To solve this problem, we used reverse genetics to rescue a recombinant LCMV (rLCMV-LASVGP) where LASVGP substituted for LCMVGP. The rescued rLCMV-LASVGP was only slightly attenuated compared to the parental LCMV isolate and adopted the receptor binding characteristics of LASV. The efficient rescue and high fitness of rLCMV-LASVGP may be explained by the close genetic and structural relationship between the GPs of LASV Josiah and LCMV ARM53b (9, 16), with conservation of crucial molecular interaction between GP and other viral proteins required for productive infection. This is in line with previous studies of an LCMV minigenome system, where the GP of LASV efficiently substituted for LCMVGP in the generation of infectious virion-like particles (41).
Since cell entry of LASV is mediated exclusively by the viral GP, the availability of rLCMV-LASVGP allowed us for the first time to study LASV entry in the context of a productive arenavirus infection. We found that rLCMV-LASVGP penetrates the endosomal membrane rapidly with kinetics remarkably similar to those of JUNV. However, in contrast to infection with JUNV, which enters cells by clathrin-mediated endocytosis (30, 46), infection with rLCMV-LASVGP was not significantly affected by the perturbation of clathrin-mediated endocytosis upon expression of DN mutants of Eps15, dynamin I, and dynamin II or depletion of clathrin heavy chain by RNAi. Likewise, expression of a DN mutant of caveolin-1 or depletion of caveolin-1 by RNAi had no effect on rLCMV-LASVGP, also excluding a caveolar entry mechanism. Rather, our data indicate that productive infection with rLCMV-LASVGP occurs predominantly via a clathrin-, caveolin-, and dynamin-independent endocytotic pathway similar to the one we recently described for cell entry of LCMV (46).
Similarly to the situation with LCMV (4, 46), neither the structural integrity nor the dynamics of actin fibers are required for rLCMV-LASVGP infection. This rules out a mechanism of viral entry involving macropinocytosis (10) or a recently discovered clathrin- and caveolin-independent pathway involved in trafficking of glycosylphosphatidylinositol-anchored proteins (49), which critically depends on Cdc42 and actin dynamics.
The remarkably low pH optimum (<4.5) for LASVGP-mediated fusion reported recently (23) suggested an unusual pattern of endosomal trafficking. To gain first information about the intracellular route of endosomal delivery of vesicle-associated LASV, we investigated the impact of DN Rab5 S34N and Rab7 T22N mutants on rLCMV-LASVGP infection. Consistent with previous findings (52), the Rab5 S34N mutant efficiently blocked delivery of VSV to early endosomes (pH of >6.0). In contrast, infection with rLCMV-LASVGP was only mildly affected by the Rab5 S34N mutant. Expression of the Rab7 T22N mutant, which efficiently blocks late endosomal trafficking of influenza virus (52), had no significant effect on rLCMV-LASVGP infection. In contrast to influenza virus, which depends on Rab5 and Rab7 for entry and has an optimal low pH of fusion of 5.1 (52), LASV seems to be delivered to a later endosomal compartment with lower pH (<4.5) via a Rab7-independent route. Although by no means conclusive, these initial experiments suggest an unusual route of endosomal delivery for LASV.
In contrast to LASV, JUNV and other human-pathogenic arenaviruses use human TfR1 as a cellular receptor. Upon binding to transferrin, TfR1 is rapidly internalized by clathrin-mediated endocytosis and delivered to the early endosome (pH of ca. 6.0), followed by recycling to the cell membrane via recycling endosomes (32). However, the GP of JUNV requires a significantly more acidic pH (<5.5) for optimal fusion activity (58), which would require delivery of the virus to late endosomal compartments. This apparent discrepancy suggests that for productive infection, JUNV may divert TfR1 from the normal recycling pathway toward late endosomes, possibly involving a Rab7-dependent pathway. Studies to elucidate the endosomal trafficking of JUNV are under way in our laboratory.
In contrast to the role of actin, which was dispensable for infection with rLCMV-LASVGP, we have obtained initial evidence of a role for microtubules in productive infection with rLCMV-LASVGP. Disruption of microtubules markedly reduced infection when applied up to 2 h p.i. This window of time is significantly wider than the one observed for pH-dependent membrane fusion of rLCMV-LASVGP, which occurs with a half time of ca. 20 min. We conclude at this point that intact microtubules may be involved in transport processes that occur after the penetration of the ribonucleoprotein complex into the cytoplasm. However, since the ribonucleoprotein complex of rLCMV-LASVGP is derived entirely from LCMV, the data regarding LASV entry must be interpreted with caution.
In summary, using a novel approach for the study of LASV entry, we have provided the first evidence that LASV enters cells by an endocytotic pathway similar to the one used by LCMV but clearly distinct from the clathrin-dependent endocytosis of JUNV and likely the other pathogenic New World arenaviruses employing TfR1 as a receptor. The endocytotic pathway involved in cell entry of LASV may be related to cellular trafficking of its primary receptor, α-DG, a possibility that we are currently investigating.
Acknowledgments
This is publication 19399 from the Department of Immunology and Microbial Science of the Scripps Research Institute.
We thank Michael B. A. Oldstone (TSRI) and Amalio Telenti (University Hospital Center and University of Lausanne) for their generous support. We further thank Sandra L. Schmid (TSRI) for the expression plasmids for the wild type and the DN mutants of dynamin, Jeffrey M. Bergelson (University of Pennsylvania) for the expression constructs for the wild type and the DN mutants of caveolin, Alice Dautry-Varsat and Nathalie Sauvonnet (Institut Pasteur, Paris) for expression vectors for control and DN mutant Eps15, and Craig Roy (Yale University School of Medicine, New Haven, CT) for the DN and wild-type Rab5 and Rab7 constructs. Christina Spiropoulou (Centers for Disease Control and Prevention) provided inactivated LASV and the mouse serum against New Word arenaviruses. Michael J. Buchmeier (TSRI) kindly provided the JUNV Candid 1 strain used in this study. We also acknowledge Sebastien Emonet for his help with the rescue of recombinant LCMV.
This research was supported by U.S. PHS grants AI065560, AI55540, and 1U54 AI065359. Stefan Kunz was supported by a Medical Research Position award from Foundation Max Cloetta (Switzerland) and Marie Curie International Reintegration grant no. 224780 from the European Community.
Footnotes
Published ahead of print on 28 May 2008.
REFERENCES
- 1.Benmerah, A., M. Bayrou, N. Cerf-Bensussan, and A. Dautry-Varsat. 1999. Inhibition of clathrin-coated pit assembly by an Eps15 mutant. J. Cell Sci. 1121303-1311. [DOI] [PubMed] [Google Scholar]
- 2.Benmerah, A., C. Lamaze, B. Begue, S. L. Schmid, A. Dautry-Varsat, and N. Cerf-Bensussan. 1998. AP-2/Eps15 interaction is required for receptor-mediated endocytosis. J. Cell Biol. 1401055-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borrow, P., and M. B. Oldstone. 1992. Characterization of lymphocytic choriomeningitis virus-binding protein(s): a candidate cellular receptor for the virus. J. Virol. 667270-7281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borrow, P., and M. B. Oldstone. 1994. Mechanism of lymphocytic choriomeningitis virus entry into cells. Virology 1981-9. [DOI] [PubMed] [Google Scholar]
- 5.Buchmeier, M. J., J. C. de la Torre, and C. J. Peters. 2007. Arenaviridae: the viruses and their replication, p. 1791-1828. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 5th ed. Lippincott Williams & Wilkins, Philadelphia, PA.
- 6.Buchmeier, M. J., H. A. Lewicki, O. Tomori, and M. B. Oldstone. 1981. Monoclonal antibodies to lymphocytic choriomeningitis and pichinde viruses: generation, characterization, and cross-reactivity with other arenaviruses. Virology 11373-85. [DOI] [PubMed] [Google Scholar]
- 7.Cao, W., M. D. Henry, P. Borrow, H. Yamada, J. H. Elder, E. V. Ravkov, S. T. Nichol, R. W. Compans, K. P. Campbell, and M. B. Oldstone. 1998. Identification of alpha-dystroglycan as a receptor for lymphocytic choriomeningitis virus and Lassa fever virus. Science 2822079-2081. [DOI] [PubMed] [Google Scholar]
- 8.Castilla, V., S. E. Mersich, N. A. Candurra, and E. B. Damonte. 1994. The entry of Junin virus into Vero cells. Arch. Virol. 136363-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clegg, J. C. 2002. Molecular phylogeny of the arenaviruses. Curr. Top. Microbiol. Immunol. 2621-24. [DOI] [PubMed] [Google Scholar]
- 10.Conner, S. D., and S. L. Schmid. 2003. Regulated portals of entry into the cell. Nature 42237-44. [DOI] [PubMed] [Google Scholar]
- 11.Coyne, C. B., and J. M. Bergelson. 2006. Virus-induced Abl and Fyn kinase signals permit coxsackievirus entry through epithelial tight junctions. Cell 124119-131. [DOI] [PubMed] [Google Scholar]
- 12.Damke, H., T. Baba, D. E. Warnock, and S. L. Schmid. 1994. Induction of mutant dynamin specifically blocks endocytic coated vesicle formation. J. Cell Biol. 127915-934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Damm, E. M., L. Pelkmans, J. Kartenbeck, A. Mezzacasa, T. Kurzchalia, and A. Helenius. 2005. Clathrin- and caveolin-1-independent endocytosis: entry of simian virus 40 into cells devoid of caveolae. J. Cell Biol. 168477-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dutko, F. J., and M. B. Oldstone. 1983. Genomic and biological variation among commonly used lymphocytic choriomeningitis virus strains. J. Gen. Virol. 641689-1698. [DOI] [PubMed] [Google Scholar]
- 15.Eichler, R., O. Lenz, W. Garten, and T. Strecker. 2006. The role of single N-glycans in proteolytic processing and cell surface transport of the Lassa virus glycoprotein GP-C. Virol. J. 341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Emonet, S., J. J. Lemasson, J. P. Gonzalez, X. de Lamballerie, and R. N. Charrel. 2006. Phylogeny and evolution of old world arenaviruses. Virology 350251-257. [DOI] [PubMed] [Google Scholar]
- 17.Eschli, B., K. Quirin, A. Wepf, J. Weber, R. Zinkernagel, and H. Hengartner. 2006. Identification of an N-terminal trimeric coiled-coil core within arenavirus glycoprotein 2 permits assignment to class I viral fusion proteins. J. Virol. 805897-5907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Freedman, D. O., and J. Woodall. 1999. Emerging infectious diseases and risk to the traveler. Med. Clin. N. Am. 83865-883. [PubMed] [Google Scholar]
- 19.Gallaher, W. R., C. DiSimone, and M. J. Buchmeier. 2001. The viral transmembrane superfamily: possible divergence of arenavirus and filovirus glycoproteins from a common RNA virus ancestor. BMC Microbiol. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Geisbert, T. W., and P. B. Jahrling. 2004. Exotic emerging viral diseases: progress and challenges. Nat. Med. 10S110-S121. [DOI] [PubMed] [Google Scholar]
- 21.Gruenberg, J. 2001. The endocytic pathway: a mosaic of domains. Nat. Rev. Mol. Cell Biol. 2721-730. [DOI] [PubMed] [Google Scholar]
- 22.Isaacson, M. 2001. Viral hemorrhagic fever hazards for travelers in Africa. Clin. Infect. Dis. 331707-1712. [DOI] [PubMed] [Google Scholar]
- 23.Klewitz, C., H. D. Klenk, and J. ter Meulen. 2007. Amino acids from both N-terminal hydrophobic regions of the Lassa virus envelope glycoprotein GP-2 are critical for pH-dependent membrane fusion and infectivity. J. Gen. Virol. 882320-2328. [DOI] [PubMed] [Google Scholar]
- 24.Kunz, S., K. H. Edelmann, J.-C. de la Torre, R. Gorney, and M. B. A. Oldstone. 2003. Mechanisms for lymphocytic choriomeningitis virus glycoprotein cleavage, transport, and incorporation into virions. Virology 314168-178. [DOI] [PubMed] [Google Scholar]
- 25.Kunz, S., J. Rojek, M. Perez, C. Spiropoulou, and M. B. Oldstone. 2005. Characterization of the interaction of Lassa fever virus with its cellular receptor α-dystroglycan. J. Virol. 795979-5987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kunz, S., J. Rojek, C. Spiropoulou, R. Barresi, K. P. Campbell, and M. B. Oldstone. 2005. Posttranslational modification of α-dystroglycan, the cellular receptor for arenaviruses, by the glycosyltransferase LARGE is critical for virus binding. J. Virol. 7914282-14296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kunz, S., N. Sevilla, J. M. Rojek, and M. B. Oldstone. 2004. Use of alternative receptors different than alpha-dystroglycan by selected isolates of lymphocytic choriomeningitis virus. Virology 325432-445. [DOI] [PubMed] [Google Scholar]
- 28.Lefrancois, L., and D. S. Lyles. 1982. The interaction of antibody with the major surface glycoprotein of vesicular stomatitis virus. II. Monoclonal antibodies of nonneutralizing and cross-reactive epitopes of Indiana and New Jersey serotypes. Virology 121168-174. [DOI] [PubMed] [Google Scholar]
- 29.Lukashevich, I. S., J. Patterson, R. Carrion, D. Moshkoff, A. Ticer, J. Zapata, K. Brasky, R. Geiger, G. B. Hubbard, J. Bryant, and M. S. Salvato. 2005. A live attenuated vaccine for Lassa fever made by reassortment of Lassa and Mopeia viruses. J. Virol. 7913934-13942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martinez, M. G., S. M. Cordo, and N. A. Candurra. 2007. Characterization of Junin arenavirus cell entry. J. Gen. Virol. 881776-1784. [DOI] [PubMed] [Google Scholar]
- 31.McCormick, J. B., and S. P. Fisher-Hoch. 2002. Lassa fever. Curr. Top. Microbiol. Immunol. 26275-109. [DOI] [PubMed] [Google Scholar]
- 32.Mellman, I. 1996. Endocytosis and molecular sorting. Annu. Rev. Cell Dev. Biol. 12575-625. [DOI] [PubMed] [Google Scholar]
- 33.Michele, D. E., R. Barresi, M. Kanagawa, F. Saito, R. D. Cohn, J. S. Satz, J. Dollar, I. Nishino, R. I. Kelley, H. Somer, V. Straub, K. D. Mathews, S. A. Moore, and K. P. Campbell. 2002. Post-translational disruption of dystroglycan-ligand interactions in congenital muscular dystrophies. Nature 418417-422. [DOI] [PubMed] [Google Scholar]
- 34.Nichols, B. J. 2002. A distinct class of endosome mediates clathrin-independent endocytosis to the Golgi complex. Nat. Cell Biol. 4374-378. [DOI] [PubMed] [Google Scholar]
- 35.Oh, P., D. P. McIntosh, and J. E. Schnitzer. 1998. Dynamin at the neck of caveolae mediates their budding to form transport vesicles by GTP-driven fission from the plasma membrane of endothelium. J. Cell Biol. 141101-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ohkuma, S., and B. Poole. 1981. Cytoplasmic vacuolation of mouse peritoneal macrophages and the uptake into lysosomes of weakly basic substances. J. Cell Biol. 90656-664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ohkuma, S., and B. Poole. 1978. Fluorescence probe measurement of the intralysosomal pH in living cells and the perturbation of pH by various agents. Proc. Natl. Acad. Sci. USA 753327-3331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pelkmans, L., T. Burli, M. Zerial, and A. Helenius. 2004. Caveolin-stabilized membrane domains as multifunctional transport and sorting devices in endocytic membrane traffic. Cell 118767-780. [DOI] [PubMed] [Google Scholar]
- 39.Pelkmans, L., J. Kartenbeck, and A. Helenius. 2001. Caveolar endocytosis of simian virus 40 reveals a new two-step vesicular-transport pathway to the ER. Nat. Cell Biol. 3473-483. [DOI] [PubMed] [Google Scholar]
- 40.Pelkmans, L., D. Puntener, and A. Helenius. 2002. Local actin polymerization and dynamin recruitment in SV40-induced internalization of caveolae. Science 296535-539. [DOI] [PubMed] [Google Scholar]
- 41.Perez, M., R. C. Craven, and J. C. de la Torre. 2003. The small RING finger protein Z drives arenavirus budding: implications for antiviral strategies. Proc. Natl. Acad. Sci. USA 10012978-12983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peters, C. J. 2002. Human infection with arenaviruses in the Americas. Curr. Top. Microbiol. Immunol. 26265-74. [DOI] [PubMed] [Google Scholar]
- 43.Pinschewer, D. D., M. Perez, A. B. Sanchez, and J. C. de la Torre. 2003. Recombinant lymphocytic choriomeningitis virus expressing vesicular stomatitis virus glycoprotein. Proc. Natl. Acad. Sci. USA 1007895-7900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Radoshitzky, S. R., J. Abraham, C. F. Spiropoulou, J. H. Kuhn, D. Nguyen, W. Li, J. Nagel, P. J. Schmidt, J. H. Nunberg, N. C. Andrews, M. Farzan, and H. Choe. 2007. Transferrin receptor 1 is a cellular receptor for New World haemorrhagic fever arenaviruses. Nature 44692-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reignier, T., J. Oldenburg, B. Noble, E. Lamb, V. Romanowski, M. J. Buchmeier, and P. M. Cannon. 2006. Receptor use by pathogenic arenaviruses. Virology 353111-120. [DOI] [PubMed] [Google Scholar]
- 46.Rojek, J. M., M. Perez, and S. Kunz. 2008. Cellular entry of lymphocytic choriomeningitis virus. J. Virol. 821505-1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rojek, J. M., C. F. Spiropoulou, K. P. Campbell, and S. Kunz. 2007. Old World and clade C New World arenaviruses mimic the molecular mechanism of receptor recognition used by α-dystroglycan's host-derived ligands. J. Virol. 815685-5695. doi: 10.1128/JVI.02574-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rojek, J. M., C. F. Spiropoulou, and S. Kunz. 2006. Characterization of the cellular receptors for the South American hemorrhagic fever viruses Junin, Guanarito, and Machupo. Virology 349476-491. [DOI] [PubMed] [Google Scholar]
- 49.Sabharanjak, S., P. Sharma, R. G. Parton, and S. Mayor. 2002. GPI-anchored proteins are delivered to recycling endosomes via a distinct cdc42-regulated, clathrin-independent pinocytic pathway. Dev. Cell 2411-423. [DOI] [PubMed] [Google Scholar]
- 50.Sanchez, A. B., and J. C. de la Torre. 2006. Rescue of the prototypic arenavirus LCMV entirely from plasmid. Virology 350370-380. [DOI] [PubMed] [Google Scholar]
- 51.Schmitz, H., B. Kohler, T. Laue, C. Drosten, P. J. Veldkamp, S. Gunther, P. Emmerich, H. P. Geisen, K. Fleischer, M. F. Beersma, and A. Hoerauf. 2002. Monitoring of clinical and laboratory data in two cases of imported Lassa fever. Microbes Infect. 443-50. [DOI] [PubMed] [Google Scholar]
- 52.Sieczkarski, S. B., and G. R. Whittaker. 2003. Differential requirements of Rab5 and Rab7 for endocytosis of influenza and other enveloped viruses. Traffic 4333-343. [DOI] [PubMed] [Google Scholar]
- 53.Sieczkarski, S. B., and G. R. Whittaker. 2002. Influenza virus can enter and infect cells in the absence of clathrin-mediated endocytosis. J. Virol. 7610455-10464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.van der Bliek, A. M., T. E. Redelmeier, H. Damke, E. J. Tisdale, E. M. Meyerowitz, and S. L. Schmid. 1993. Mutations in human dynamin block an intermediate stage in coated vesicle formation. J. Cell Biol. 122553-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vela, E. M., L. Zhang, T. M. Colpitts, R. A. Davey, and J. F. Aronson. 2007. Arenavirus entry occurs through a cholesterol-dependent, non-caveolar, clathrin-mediated endocytic mechanism. Virology 3691-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Weber, E. L., and M. J. Buchmeier. 1988. Fine mapping of a peptide sequence containing an antigenic site conserved among arenaviruses. Virology 16430-38. [DOI] [PubMed] [Google Scholar]
- 57.Weissenbacher, M. C., R. P. Laguens, and C. E. Coto. 1987. Argentine hemorrhagic fever. Curr. Top. Microbiol. Immunol. 13479-116. [DOI] [PubMed] [Google Scholar]
- 58.York, J., and J. H. Nunberg. 2006. Role of the stable signal peptide of Junin arenavirus envelope glycoprotein in pH-dependent membrane fusion. J. Virol. 807775-7780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zerial, M., and H. McBride. 2001. Rab proteins as membrane organizers. Nat. Rev. Mol. Cell Biol. 2107-117. [DOI] [PubMed] [Google Scholar]