Abstract
Angiopoietins were thought to be endothelial cell-specific via the tie2 receptor. We showed that angiopoietin-1 (ang1) also interacts with integrins on cardiac myocytes (CMs) to increase survival. Because ang1 monomers bind and activate integrins (not tie2), we determined their function in vivo. We examined monomer and multimer expressions during physiological and pathological cardiac remodeling and overexpressed ang1 monomers in phenylephrine-induced cardiac hypertrophy. Cardiac ang1 levels (mRNA, protein) increased during postnatal development and decreased with phenylephrine-induced cardiac hypertrophy, whereas tie2 phosphorylations were unchanged. We found that most or all of the changes during cardiac remodeling were in monomers, offering an explanation for unchanged tie2 activity. Heart tissue contains abundant ang1 monomers and few multimers (Western blotting). We generated plasmids that produce ang1 monomers (ang1–256), injected them into mice, and confirmed cardiac expression (immunohistochemistry, RT-PCR). Ang1 monomers localize to CMs, smooth muscle cells, and endothelial cells. In phenylephrine-induced cardiac hypertrophy, ang1–256 reduced left ventricle (LV)/tibia ratios, fetal gene expressions (atrial and brain natriuretic peptides, skeletal actin, β-myosin heavy chain), and fibrosis (collagen III), and increased LV prosurvival signaling (akt, MAPKp42/44), and AMPKT172. However, tie2 phosphorylations were unchanged. Ang1–256 increased integrin-linked kinase, a key regulator of integrin signaling and cardiac health. Collectively, these results suggest a role for ang1 monomers in cardiac remodeling.—Dallabrida, S. M., Ismail, N. S., Pravda, E. A., Parodi, E. M., Dickie, R., Durand, E. M., Lai, J., Cassiola, F., Rogers, R. A., Rupnick, M. A. Integrin binding angiopoietin-1 monomers reduce cardiac hypertrophy.
Keywords: cardiac myocytes, endothelial cells, integrin-linked kinase, AMP-activated protein kinase, Tie2
Aging societies, increasingly prevalent risk factors such as obesity and diabetes, and improved survival from acute coronary syndromes have produced a growing population with reduced cardiac function. Compromised cardiac function triggers a process of cardiac remodeling whereby progressive changes in heart composition and structure occur to counterbalance stress and salvage function. Although initially stabilizing, the changes cannot offset the impairment. The evolving cardiac phenotype becomes maladaptive and decompensates, manifesting as heart failure. Once cardiac reserve is exhausted, mortality rates exceed 50%. With heart failure the fastest growing form of cardiovascular disease in developed countries, the need for new advances is pressing. As a final common pathway, cardiac remodeling has emerged as a primary therapeutic target for heart failure of all causes.
Ang1 is vital to cardiovascular development, with a burgeoning role in heart disease. It is widely reported as an endothelial cell (EC) -specific regulator of vessel maturation because its receptor, tie2, is almost exclusive to EC (1, 2). However, our studies (3) and others (4) are revising this view. We showed that ang1 acts on cardiac and skeletal myocytes as a potent survival factor via select integrins, resulting in enhanced adhesion and activation of prosurvival signaling. Thus, ang1 is well-positioned at the vessel/tissue interface to mediate cardiac remodeling and preserve function.
Establishing that ang1/cardiac myocyte (CM) interactions promote myocyte survival invites reinterpretation of in vivo studies showing that ang1 is cardioprotective to include broader mechanisms of action. Ang1 knockout mice have embryonic lethal cardiac defects (impaired endocardial development, trabeculae formation, vessel maturation) (5). In myocardial infarction (MI) models, ang1 overexpression reduced infarct zones and preserved ejection fractions (6). These benefits were attributed solely to the role of ang1 in angiogenesis, causing increased capillary density (6,7,8). However, our data suggest that direct actions of ang1 on CMs and smooth muscle cells (SMCs) contribute to the protective effects.
Ang1 protein structure is complex, with quaternary multimeric forms unique among growth factors. From amino to carboxyl terminus, the domains are superclustering (9), coiled-coil (oligomerization) (10), linker (binds ang1 to matrix) (11), and fibrinogen-like (binds tie2) (9, 12, 13). Coiled-coil domains join monomers into disulfide-linked ang1 homo-oligomers that multimerize about the superclustering domains (9, 10).
Ang1’s quaternary protein structure is a determinant of its receptor targeting. Ang1 tetramers and pentamers bind and activate tie2 (9). Ang1 trimers bind soluble tie2-Fc without phosphorylating tie2 (10, 12). Ang1 dimers weakly bind soluble tie2-Fc (63-fold<tetramer) (9) and do not phosphorylate EC tie2 (12). Ang1 monomers show little (290-fold<tetramer) (9) to no (12) binding to soluble tie2-Fc and do not activate EC tie2 but bind integrin α5β1 (13).
The findings that ang1 monomers bind integrins (13), whereas tie2 activation requires at least tetramers (9, 12), suggested to us that ang1 forms may be differentially regulated in vivo during remodeling and among organs. Here, we show that ang1 monomers are in adult tissues, shift during cardiac remodeling, and localize to CMs, SMCs, and ECs in vivo. Recombinant ang1 monomers reduced murine cardiac hypertrophy, activated prosurvival signaling and AMPKT172 (master regulator of cardiac energetics and metabolism), and integrin-linked kinase (ILK) (central mediator of CM contractility and cell survival) (14). Thus, we propose that differential expression of ang1 quaternary forms is a unique regulatory mechanism for directing receptor/cell interactions in vivo and that ang1 monomer/integrin interactions have a cardioprotective role in remodeling.
MATERIALS AND METHODS
Animals
The investigation conforms with the U.S. National Institutes of Health Guide for the Care and Use of Laboratory Animals. C57BL/6J (C57) mice (Jackson Laboratory, Bar Harbor, ME, USA) were given free access to water and standard chow. Where indicated, 7-wk-old male mice received phenylephrine hydrochloride (PE) (Sigma, St. Louis, MO, USA) in saline (75 mg/kg/day) or saline (control) via subcutaneous miniosmotic pumps (Alzet, Cupertino, CA, USA). CMs were isolated from Sprague-Dawley rats (Charles River Laboratory, Wilmington, MA, USA).
Recombinant Ang1 constructs
Ang1 was cloned from C57 mouse heart as we described (15). Using pcDNA3.1/V5-His TOPO/TA (Invitrogen, Carlsbad, CA, USA) vector, we cloned in N-terminal hemagluttinin secretion signal (MKTIIALSYIFCLVFA) and FLAG tag (DYKDDDDK) fused to mouse ang1 from amino acids 256–498 (ang1–256/pcDNA). The vector contains C-terminal V5 and 6X polyhistidine tags. Plasmids were double-purified with Endotoxin-free plasmid DNA purification kits (Qiagen, Valencia, CA, USA) and sequenced. Mice were retroorbitally injected with ang1–256/pcDNA or pcDNA (40 μg) using InVivo Jet-polyethylenimine (PEI) transfection agent plus glucose (ISC Bioexpress, Kaysvilla, UT, USA).
Cell culture and isolations
C2C12 myoblast cell lines were maintained as we described (3). Myoblasts were differentiated into myocytes by confluency or by 3% horse serum in Dulbecco modified Eagle medium (DMEM) (16). Rat neonatal CMs (RNCMs) and rat neonatal cardiac fibroblasts (RNCFs) were isolated from ventricles of 2-day-old pups. RNCMs were cultured as described (3) except for preplatings (2×, 1 h), cytosine-β-D-arabinofuranoside (cβDa) (10 μg/ml) added to media, and 1% gelatin coating on plates. RNCFs were isolated using published methods (17). Media was changed to low-glucose (LG) -DMEM with 10% fetal bovine serum (FBS) and 1% penicillin–streptomycin–glutamine (PSG). Cells were grown to confluency and passaged to eliminate residual nonfibroblasts. Rat adult cardiac myocytes (RACMs) were isolated from 8-wk-old rat ventricles using published procedures (18). Hearts were sterilely removed, hung by the aorta (23-gauge blunt needle), and secured (4.0-gauge suture). Hearts were retrograde perfused with Ca2+-free Krebs-Henseleit buffer (KHB), 11 mM glucose, and 25 mM NaHCO3 at pH 7.4 until clear and perfusion digested (20 min, 37°C) with Enzyme I solution [0.33 mg/ml type II collagenase (Worthington, Lakewood, NJ, USA), 0.3 mg/ml type II hyaluronidase, Ca2+-free KHB, 11 mM glucose, and 25 mM NaHCO3]. Ventricles were minced and further digested with Enzyme I, 0.02 mg/ml trypsin type IX, and 0.02 mg/ml DNase (Worthington) (20 min, 37°C with shaking). Tissues were filtered (80-μm nylon mesh) into 1:1 Ca2+-free KHB/LG-DMEM and centrifuged, supernatant was removed, and the cell pellet was resuspended in 1:1 Ca2+-free KHB/LG-DMEM. Cells were placed in Ca2+-free KHB with 6.5% bovine serum albumin (BSA) (Fisher Scientific, Morris Plains, NJ, USA) until myocytes settled. Supernatant was removed and myocytes were plated on 10 μg/ml laminin-coated plates in Medium199 with 5 mM creatine, 2 mM carnitine, 5 mM taurine, 10 μM cβDa, 4% FBS, and 1% PSG (37°C, 5% CO2, 1 day).
Polymerase chain reaction (PCR)
Real-time primers for mouse [ang1, ang2, tie1, tie2, atrial natriuretic peptide (ANP), brain natriuretic peptide (BNP), β-myosin heavy chain (βMHC), skeletal actin, smooth muscle actin (SMA), collagen III, and GAPDH] (19) and reverse-transcription PCR (RT-PCR) mouse [ang1, ang2, tie2, platelet/endothelial cell adhesion molecule (PECAM), vascular endothelial growth factor (VEGF) (20), and VEGF receptors 1 and 2 (VEGFR1, VEGFR2)] and rat [ang1 (forward mouse ang1, ref. 15; reverse 5′, ref. 21)] and GAPDH (Integrated DNA Technology, Coralville, IA, USA) were used for PCR as described (15). Ang1–256 mRNA was amplified with forward 5′-TACAAAGACGATGACGACAAGGACACA-3′ and reverse 5′-AGGGTTAGGGATAGGCTTACCTTCGAA-3′ primers. GAPDH mRNA levels were stable among groups and used for normalization.
Western blotting and cell signaling
Protein lysates were made as we described (3), except 50 mM NaF was added. Some lysates were PNGaseF-treated (Sigma) following manufacturer’s instructions to assess for N-linked glycosylation. SDS-PAGE analyses were conducted under nonreduced and reduced conditions. Tissue (100 μg) and recombinant human ang1 (rhAng1) lysates (R&D Systems, Minneapolis, MN, USA) received sample loading buffer (Bio-Rad, Hercules, CA, USA). Some lysates received reducing agent (Bio-Rad reducing agent or 0.435 M βMe) and were heated (5 min, 95°C). Samples were loaded on 3–8% Tris-acetate criterion gels (Bio-Rad), separated by SDS-PAGE, and transferred to nitrocellulose (Perkin Elmer, Boston, MA, USA). Membranes were probed for ang1 with the following antibodies: 100–401-403 (Rockland, Gilbertsville, PA, USA), MAB050 or AF923 (R&D Systems), A0604 (Sigma), sc6319 (Santa Cruz, Santa Cruz, CA, USA), ab8451 (Abcam, Cambridge, MA, USA), and AB3120 (Chemicon/Millipore, Temecula, CA, USA). Blots were blocked (30 min), incubated in primary antibody in block (1 h), rinsed 3× in 10 mM Tris-base with 150 mM NaCl and 0.1% Tween20 (TBST), incubated in appropriate horseradish peroxidase (HRP) -conjugated secondary antibody [anti-mouse, anti-rabbit immunoglobulin G (IgG); 1:1500] in block (1 h), rinsed (3×, TBST), and exposed to chemiluminescence using ECL kits (Amersham, Piscataway, NJ, USA, or Perkin Elmer). Blots were reprobed for GAPDH (Santa Cruz) as we described (3). Blots were probed for phosphorylation of aktS473, MAPKp42(T202)/44(T204), AMP-activated protein kinase (AMPK)T172, AMPKS485/S491, ILK (Cell Signaling, Danvers, MA, USA), and FAKT397 (BD Pharmingen, Billerica, MA, USA); stripped with Restore Stripping Buffer (Pierce Biotechnology, Rockford, IL, USA); and reprobed for total akt, AMPK α1/α2 (Cell Signaling), MAPKp42/44 (Chemicon/Millipore), FAK (BD Pharmingen), or GAPDH (Santa Cruz) as we described (3).
Tie2 immunoprecipitation
Protein lysates (1000 μg) from mouse left ventricle (LV) were incubated (overnight, 4°C) with 7 μg mouse anti-tie2 monoclonal clone AB33 (Upstate, Waltham, MA, USA), protein G PLUS agarose beads (Santa Cruz) were added (4 h, 4°C), pellets were rinsed (modified RIPA buffer, 3×), and sample loading buffer with Bio-Rad reducing agent was added. Membranes were probed with mouse anti-phosphotyrosine monoclonal recombinant 4G10 (1:200; Upstate) and HRP-linked anti-mouse IgG (1:2000). Blots were stripped with Restore Stripping Buffer (45 min), rinsed in PBS with 0.05% Tween20, and reprobed with rabbit anti-tie2 polyclonal sc324 (1:400; Santa Cruz) and HRP-linked anti-rabbit IgG (1:1500).
Ang1 immunoprecipitation
C2C12 myocytes, RNCMs, and RNCFs were cultured in antibiotic-free media (3 days). Media (90 ml) was collected and centrifuged, and protease and phosphatase inhibitors were added as we described (3). Media was precleared with agarose beads, and anti-ang1 antibody (2 μg; R&D monoclonal) was added (2 h, 4°C) followed by protein A/G PLUS agarose beads (overnight, 4°C). Beads were centrifuged and washed in modified RIPA buffer (3 min, 3×), and sample loading buffer was added. Samples were divided in half, prepared as nonreduced and reduced (0.435 M βMe), and analyzed by SDS-PAGE. Membranes were probed with anti-ang1 antibody. Negative controls included substituting mouse IgG for primary antibody. When these control samples were probed with ang1 antibodies on a Western blot, there were no bands (unpublished observations).
Hanging heart perfusions
Mice were given intraperitoneal injections of heparin (4 U/g) with 2.5% avertin. For some studies, anesthetized mice were retroorbitally injected (30-gauge needle) with 10% fluorescein isothiocyanate (FITC) -tomato lectin (Vector, Burlingame, CA, USA) in PBS and given 5 min to allow the lectin to circulate. Hearts were removed, dipped in KHB with 25 mM NaHCO3 and 1.4 mM CaCl2, and hung by the aorta (23-gauge blunt needle). Aortas were tied (4.0-gauge suture), retrograde perfused (KHB, 25 mM NaHCO3, 1.4 mM CaCl2, 40 mM KCl, and 4 mM sodium nitroprusside dihydrate) until exiting perfusates were cleared, and perfusion fixed (2% formaldehyde in PBS, 10 min). Where indicated, hearts were then perfused with tissue-marking dye (Triangle Biomedical, Durham, NC, USA). Hearts were trimmed to the ventricles. The left and right ventricles (LVs and RVs) were filled with and then immersed into warmed (37°C) TissueTek optimal cutting temperature (OCT) compound (Fisher Scientific), and frozen (–80°C).
Immunohistochemistry
Endogenous LV Ang1
Ventricles embedded in OCT compound were cryosectioned (5 μm, −20°C) and mounted on Superfrost Plus slides. Sections were air-dried (warming plate), postfixed (ice-cold acetone, 2 min), washed in TBS, and blocked in appropriate normal serum buffer. Tissues were incubated (overnight, 4°C) in primary antibodies ang1 (Rockland and Santa Cruz) or goat polyclonal troponin I (Santa Cruz) (1:100) in antibody diluent (Dako, Carpinteria, CA, USA). Negative controls incubated in the appropriate IgG or serum (Vector) showed no signal (unpublished observations). Slides were washed in TBS, blocked (serum buffer), and incubated (2 h) in rabbit anti-goat Texas Red (Jackson Immunoresearch, West Grove, PA, USA), rabbit anti-goat Alexa Fluor 647 (Invitrogen), or goat anti-rabbit Alexa Fluor 568-conjugated secondary antibodies (Invitrogen) (1:200, serum block buffer). Slides were washed (TBS) and coverslips were placed (Fluoromount G antifade mounting media; Southern Biotech, Birmingham, AL, USA).
Alternatively, 100-μm-thick sections were cut using an oscillating tissue slicer, washed (buffer with 0.1% Triton X-100) and incubated in secondary antibody (4 h). Slides were scanned in fluorescence mode with a Leica PL APO ×40 NA 1.25 oil-immersion objective lens using a Leica TCS-NT laser scanning confocal microscope (Leica Microsystems, Wetzlar, Germany) fitted with argon and krypton lasers at room temperature. Serial optical sections of ventricle were recorded beginning at the ventricular apex, using confocal microscopy with a photomultiplier tube detector and Leica confocal software to capture images digitally. Where indicated, the resultant stacks were rendered in three dimensions using VoxelView 2.5.1 software (Vital Images, Minnetonka, MN, USA).
Recombinant Ang1–256
Mouse heart tissues were fixed in 4% paraformaldehyde and PBS, dehydrated through a graded ethanol series, embedded in paraffin, and cut into 8-μm sections. Sections were rehydrated, and epitopes were retrieved with 10 mM sodium citrate buffer and 0.05% Tween-20 (pH 6.0) (20 min, 95°C), rinsed in PBS, and blocked with normal goat serum in PBS (0.5 h); then primary antibody or relevant control (IgG or normal serum) was added in block. FLAG rabbit polyclonal antibody (Sigma) was added (1:50; overnight, 4°C). SMA mouse monoclonal antibody (Sigma; 1:100, 45 min), von Willebrand factor (vWF) rabbit polyclonal antibody (Dako; 1:150, 1 h), or phalloidin-conjugated to Alexa Fluor 488 (Invitrogen; 1:100, 0.5 h) was added. Slides were rinsed (PBS), and the appropriate secondary antibodies were added: for FLAG, goat anti-rabbit Alexa Fluor 647 (1:200, 1 h); for SMA, goat anti-mouse Alexa Fluor 568 (1:200, 45 min); for VWF, biotinylated anti-rabbit IgG (Vector; 1:100, 1 h) and strepavidin-conjugated Alexa Fluor 568 (1:200, 1 h). Slides were rinsed and Vectashield Mounting Medium with DAPI was added (Vector). Optical sections were taken with a Leica TCS SP2-AOBS attached to a DMIRE-2 inverted microscope with an ×63 objective (Leica Microsystems).
Statistical analysis
Results are reported as mean ± sd; 2-tailed Student’s t tests with 2-sample equal variance and P ≤ 0.05 were considered significant.
RESULTS
Ang1 mRNA levels shift during cardiac remodeling
We examined angiopoietin ligands and receptors in different-aged C57 mouse hearts during physiological remodeling (RT-PCR analysis using GAPDH as control and PECAM as EC marker). Ang1 mRNA levels increased with age in the LV, RV, and atria (AT), whereas ang2, tie2, and PECAM levels were stable (Fig. 1A). Western blotting showed parallel increases in ang1 LV protein levels (Fig. 1B) with stable tie2 protein levels (unpublished observations). Rat neonatal CMs had trace ang1 mRNA, whereas adult CMs expressed ang1 strongly (Fig. 1C).
Figure 1.
Ang1 mRNA levels change during cardiac remodeling. A) RT-PCR analysis of mRNA transcripts in mouse LV, RV, and AT. From neonate to adult, ang1 and VEGF188 mRNA expressions increase, whereas VEGF120 mRNA decreases. B) Western blotting shows corresponding increases in ang1 protein levels in mouse LV with age. *P ≤ 0.05 vs. 2 days. C) Blots show ang1 mRNA levels in rat CMs: trace levels in neonatal rats; abundant in adults. Studies done in duplicate; n = 4/group (A–C). D–F) Real-time PCR analysis of ang1 mRNA in mice: levels in LV (D), RV (E), and AT (F) increase with age. Insets (dashed boxes) magnify days –1 to 21. Studies done in triplicate; n = 5/group. G, H) Analysis of mice treated with PE or saline (control): PE increases LV/tibia ratios (G); real-time PCR shows LV ang1 mRNA levels decrease with PE-induced hypertrophy.
To quantify ang1 mRNA increases, we conducted real-time PCR with LV, RV, and AT from different-aged mice [(–1 day=embryonic day 20), 1, 2, 4, 7, 14, 21, 56, 133, and 238 days]. Relative fold increases in ang1 were graphed alongside increasing chamber weights. Ang1 mRNA levels increased over 1000-fold in LV (Fig. 1D) and RV (Fig. 1E), with smaller atrial increases (Fig. 1F). A small spike in LV and RV ang1 occurred between days 1 and 4, which returned to near baseline, then climbed. During the fetal to adult transition, similar ang1 increases (LV, RV, AT) were found in female and male mice with stable ang2 and tie2 mRNA levels (unpublished observations).
To assess ang1 in pathological cardiac remodeling, mice were given PE to induce hypertrophy, or saline as control. PE increased LV/tibia ratios (Fig. 1G) and LV mRNA levels of ANP, BNP, βMHC, collagen III, skeletal actin, and SMA (Supplemental Fig. 1A–F), and decreased ang1 mRNA levels in LV (Fig. 1H) and RV, whereas ang2 and tie2 were stable (real-time PCR) (unpublished observations).
Integrin-binding ang1 monomers are abundant in heart tissue
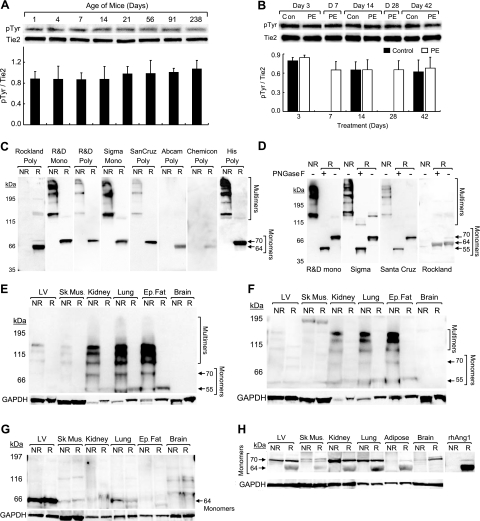
Using immunoprecipitation and Western blotting, we found that tie2 phosphorylation was stable in different-aged (Fig. 2A) and PE-treated (Fig. 2B) mice, despite substantial shifts in ang1 (Fig. 1). Thus, we proposed that integrins are the target for ang1 shifts.
Figure 2.
Tie2 activation is stable during cardiac remodeling and heart has abundant ang1 monomers compared to other tissues. A, B) Tie2 phosphorylation [immunoprecipitation and Western blotting for phosphotyrosine (pTyr) and tie2] shows no change during physiological (A) and pathological (PE-induced) (B) LV remodeling, remaining stable in neonatal through adult (A) and control vs. hypertrophic LVs (B). Studies done in triplicate; n = 3/group. C, D) Results of Western blotting conducted with rhAng1 (0.09 μg) in nonreduced (NR) and reduced (R) (βMe) conditions. Blots were probed with anti-ang1 monoclonal (mono) or polyclonal (poly) antibodies in duplicate studies. The ang1 monomers and multimers detected vary (C). PNGase-F treatment of rhAng1 reveals that some ang1 forms were glycosylated (D). E–H) Western blot analysis of protein lysates from mouse (E–G) and human (H) LV, skeletal muscle (sk. mus), kidney, lung, epididymal fat (ep. fat), and brain tissue, evaluated in nonreduced and reduced (βMe) conditions. Blots were probed with anti-ang1 [monoclonal: R&D (E) and Sigma (F); polyclonal: Rockland (G, H)] and anti-GAPDH antibodies in duplicate studies. Ang1 monomers and multimers are seen in mouse (E–G) and human (H) adult tissues. Heart and skeletal muscle show low multimer levels (E, F) and high monomer levels (G) vs. other tissues.
We first established whether integrin-binding ang1 monomers and various multimers are present in heart tissue. We defined the ang1 forms recognized by available ang1 antibodies (monoclonal: R&D Systems and Sigma; polyclonal: Abcam, Chemicon/Millipore, R&D Systems, Rockland, and Santa Cruz) using rhAng1 (R&D Systems). Using Western blotting under nonreducing conditions, monoclonal (R&D and Sigma) and polyclonal (R&D and Santa Cruz) ang1 antibodies detected several multimers (Fig. 2C). Using a 6× polyhistidine antibody to the polyhistidine tag on rhAng1, we detected a similar pattern of multimers as observed with ang1 antibodies (Fig. 2C). In reduced conditions, rhAng1 monomer was found at 64 kDa (Rockland, Abcam, and Chemicon polyclonals) and 70 kDa (R&D and Sigma monoclonals; Santa Cruz, R&D, and Rockland polyclonals), similar to a prior report (12).
Ang1 has potential glycosylation sites. We treated rhAng1 with PNGase-F and conducted Western blotting with ang1 antibodies. In reduced conditions, PNGase-F-treated rhAng1 monomer shifted from 70 to 55 kDa (R&D and Sigma monoclonal; Santa Cruz polyclonal; Fig. 2D) as was previously shown (22). However, the Rockland anti-ang1 antibody detects ang1 monomer at 64 kDa. PNGase-F treatment did not alter the mobility of the 64 kDa monomer, indicating that this form is not glycosylated (Fig. 2D).
To establish whether ang1 monomers and multimers exist in vivo, we conducted Western blotting with ang1 and GAPDH (control) antibodies on adult mouse (Fig. 2E–G) and human tissues (Fig. 2H; USBiological, Swampscott, MA, USA, and Imgenex, San Diego, CA, USA; unpublished observations). Also, rhAng1 (nonreduced and reduced) was run on these blots to confirm the location of ang1 bands (Fig. 2H). In nonreduced conditions, mouse tissues probed with R&D (Fig. 2E) and Sigma (Fig. 2F) monoclonal antibodies revealed ang1 monomers (70 and 55 kDa), dimmers, and trimers, but few larger forms. Human tissues had only trace ang1 multimers (R&D and Sigma monoclonals, unpublished observations), perhaps due to degradation or instability of higher complexes (9, 12, 13) or poor epitope recognition.
With βMe, all ang1 forms reduced to 55 kDa with R&D (Fig. 2E) and Sigma (Fig. 2F) monoclonal anti-ang1, and PNGase-F treatment shifted all ang1 forms to 55 kDa (Supplemental Fig. 2A, B), similarly to rhAng1. Mouse LV and skeletal muscle had trace ang1 multimers (Fig. 2E, F). Multimers were abundant in kidney, lung, and adipose tissue, but without appreciable expression in brain.
Using Rockland anti-ang1, mouse LV highly expressed 64 kDa monomer vs. other tissues (Fig. 2G), and ang1 monomers were in all human tissues tested (Fig. 2H). PNGase-F did not alter mobility of the 64 kDa form in tissue or with rhAng1 (Supplemental Fig. 2C). Thus, integrin-binding ang1 monomers are broadly produced in vivo with tissue-specific differential expressions of ang1 forms.
Nonendothelial cells produce ang1, so we assessed whether CMs, cardiac fibroblasts, and skeletal myocytes produce ang1 monomers and multimers. We collected rat neonatal CM, cardiac fibroblast, and differentiated C2C12 skeletal myocyte media and immunoprecipitated ang1. In nonreduced conditions, Western blotting showed that neonatal CMs, cardiac fibroblasts, and C2C12 myocytes produced ang1 monomer (70 kDa), dimer, trimer, tetramer, and trace larger forms as were seen with rhAng1 (Sigma anti-ang1, Supplemental Fig. 2D; R&D anti-ang1, unpublished observations). In reduced conditions, different ang1 forms converted to 55 kDa monomer.
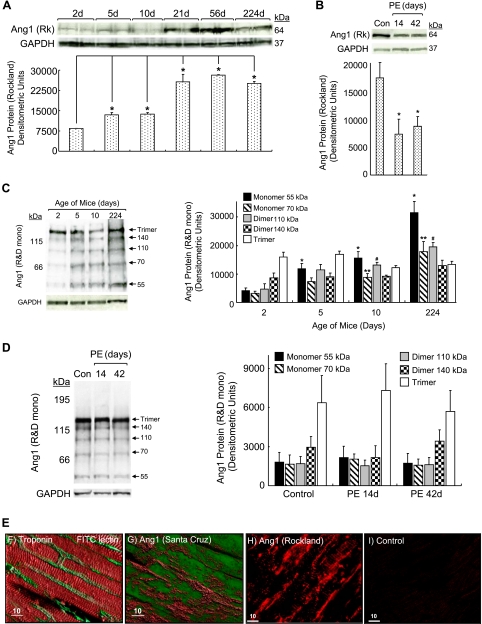
Ang1 monomers shift during cardiac remodeling and interact with CMs and ECs in vivo
We conducted Western blotting with LV protein lysates from different-aged mice or mice treated with PE or saline (control). Under nonreduced conditions, 64 kDa (Rockland polyclonal, Fig. 3A), 55 kDa, and 70 kDa (R&D monoclonal, Fig. 3C) ang1 monomers increased during the neonatal to adult transition. At 10 days, 110 kDa ang1 dimers increased, but ang1 dimers (140 kDa) and trimers were stable (Fig. 3C). With hypertrophy, in nonreduced conditions (Fig. 3B), 64 kDa (Rockland anti-ang1) monomer declined, but 55 and 70 kDa monomer, dimer, and trimer (R&D monoclonal anti-ang1) levels were stable (Fig. 3D). Reduced conditions converted various ang1 forms to monomers (unpublished observations). Thus, shifts in ang1 during physiological and pathological cardiac remodeling are primarily in integrin-binding monomers.
Figure 3.
Ang1 monomers shift during cardiac remodeling. Western blotting was conducted under nonreduced conditions with LVs from neonate to adult mice (A, C) or mice with PE-induced hypertrophy vs. saline-treated controls (con) (B, D). Blots were probed with anti-ang1 Rockland (Rk) polyclonal (A, B) or R&D monoclonal antibodies (C, D). Studies done in duplicate; n = 3/group. A) Ang1 monomers increase with age. *Left to right: P = 0.015, 0.036, 0.013, 0.00002, 0.0007. B) Ang1 monomers decline during PE-induced remodeling. *P ≤ 0.03. C) Western blotting with anti-ang1 (R&D monoclonal) shows that 55 kDa monomers (*left to right: P=0.023, 0.017, 0.011), 70 kDa monomers (**left to right: P=0.038, 0.029), and 110 kDa dimers (#left to right: P=0.029, 0.014) increase with age, whereas other dimmers and trimers are stable (arrows indicate ang1 forms). D) In PE-induced remodeling, blots probed with anti-ang1 (R & D monoclonal) show no change in monomer (55 and 70 kDa), dimer, and trimer levels. E) Fluorescent immunohistochemistry and confocal imaging of ang1 forms in perfusion-fixed mouse LV; studies done in triplicate. F) CMs are labeled with troponin-I linked to Texas Red (red) and ECs are tagged with FITC-lectin (green). G) LV labeled with anti-ang1 (Santa Cruz) conjugated to Alexa Fluor 647 (red), and CMs autofluoresce (green). Labeling of CMs and ECs indicates that ang1 multimers interact with both cell types. H) Anti-ang1 (Rockland) conjugated to Alexa Fluor 568 (red), which recognizes only monomers, immunostains CMs and ECs in vivo. I) Rabbit sera (negative control) were substituted for anti-ang1 (Rockland). Scale bars = 10 μm.
To identify in vivo interactions of ang1 forms with cardiac cells, we conducted fluorescent immunohistochemistry on perfusion-fixed mouse LV (Fig. 3E). Confocal images of CMs labeled with troponin I conjugated to Alexa Fluor 647 (red) show a typical ladder pattern (Fig. 3E, F). ECs perfusion stained with FITC-conjugated ulex lectin (green) border CMs (Fig. 3E, F). Anti-ang1 (Santa Cruz; detects multimers and monomers; 70 and 55 kDa) conjugated to Alexa Fluor 647 (red) appeared to label CMs (autofluorescent green) and the vasculature (Fig. 3E, G). Anti-ang1 (Rockland; detects monomers; 70 and 64 kDa) conjugated to Alexa Fluor 568 (red) also appeared to label CMs (ladder and punctuate pattern) and ECs (Fig. 3E, H). Rabbit IgG substituted for primary antibody was used as negative control (Fig. 3E, I). We propose that ang1 monomers interact with adult CMc and cardiac ECs in vivo, likely via integrins.
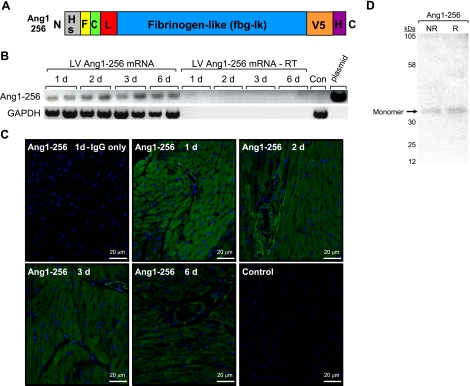
Ang1–256 monomer expression in heart tissue
To determine the function of integrin-binding ang1 monomers in cardiac remodeling, we generated a truncated recombinant ang1 form (ang1–256) known to generate only monomers (12). Ang1–256 consists of ang1’s amino acids 256–498, N-terminal hemagluttinin secretion signal and FLAG tag, and C-terminal V5 and polyhistidine tags (Fig. 4A). Using pcDNA plasmid-based expression, we transfected human embryonic kidney (HEK) 293 cells with ang1–256/pcDNA and purified ang1–256 protein. Western blotting with an anti-V5 antibody showed a single ang1 monomer band (34 kDa) under nonreduced and reduced conditions (Fig. 4D), verifying that ang1–256/pcDNA generates only ang1 monomers. We retroorbitally injected ang1–256/pcDNA or pcDNA vector alone using In Vivo-Jet-PEI into C57 mice and examined the expression of ang1–256 mRNA (RT-PCR) and protein (fluorescent immunohistochemistry and confocal imaging). This method of delivering plasmids to heart tissue is very effective, reliable, efficient, and nontoxic, and is used in clinical trials to deliver cancer gene therapy (ISC Bioexpress) (23,24,25). Ang1–256 mRNA was detected in mouse LV at all time points tested (Fig. 4B). Control mice injected with pcDNA alone were negative for ang1–256 mRNA, as were LVs from mice injected with ang1–256 where cDNA synthesis reactions were conducted without reverse transcriptase (Fig. 4B). Ang1–256 plasmid was used as a positive control. Ang1–256 protein expression was detected using FLAG antibody linked to Alexa Fluor 647 (green), and nuclei were stained with DAPI (blue). Ang1–256 protein was observed at all time points, with the highest expression on day 1 (Fig. 4C). Ang1–256 appeared to be present in CMs and cardiac ECs. Negative controls included pcDNA alone-injected mice (control) and rabbit IgG substituted for primary antibody in LV sections from ang1–256-injected mice.
Figure 4.
Ang1–256 monomers are expressed in heart tissue. A) Recombinant truncated ang1–256 has a modified influenza hemagluttinin secretion signal (HS) and FLAG (F) tag fused to ang1 at amino acid 256. Ang1–256 has 6 amino acids of the coiled coil domain (C) and the linker (L) and fibrinogen-like domains of ang1 followed by C-terminal V5 and 6× polyhistidine (H) tags. B, C) Ang1–256/pcDNA (ang1–256) or pcDNA control (con) were retroorbitally injected into C57 mice in triplicate studies. cDNA synthesis reactions conducted ±RT with ang1–256/pcDNA plasmid (positive control) show LV ang1–256 mRNA at all time points (B). Fluorescent immunohistochemistry and confocal imaging of mouse heart tissue shows ang1–256 protein at all time points (C). Ang1–256 was labeled using FLAG antibody linked to Alexa Fluor 647, and nuclei were labeled using DAPI. Negative controls included substituting rabbit IgG for primary antibody and injecting mice with pcDNA vector (control) (1 day). Scale bars = 20 μm. D) Western blot analysis of HEK293 cells transfected with ang1–256/pcDNA. Ang1–256 proteins were purified by anti-FLAG M1 affinity column chromatography (Sigma), dialyzed, and concentrated. Western blots probed with V5 antibody show ang1–256 monomer protein at the predicted molecular mass (34 kDa) in nonreduced (NR) and reduced (R) conditions.
Ang1–256 protein localizes to CMs, SMCs, and ECs
We conducted fluorescent immunohistochemistry and confocal imaging to discern the location of ang1–256 on day 1 in mouse hearts. Phalloidin-linked Alexa Fluor 488 (red) -stained F-actin, vWF antibody linked to biotinylated anti-rabbit IgG and strepavidin-linked Alexa Fluor 488-labeled ECs, αSMA antibody linked to anti-mouse Alexa Fluor 568-labeled SMCs, FLAG antibody linked to anti-rabbit Alexa Fluor 647-tagged ang1–256, and nuclei were labeled with DAPI. Negative controls included LV ang1–256 (day 1) where the appropriate sera or IgGs were substituted for primary antibodies. These sections had no appreciable signal (unpublished observations). In merged images, we found that ang1–256 localizes with phalloidin on CMs, vWF on ECs, and SMA on SMCs, appearing yellow in each case (Fig. 5).
Figure 5.
Ang1–256 protein in heart tissue localizes to CMs, SMCs, and ECs. Ang1–256/pcDNA (ang1–256) was retroorbitally injected into C57 mice (1 day), and fluorescent immunohistochemistry with confocal imaging was conducted on heart tissue in triplicate studies. CMs are labeled with Alexa Fluor 488-linked phalloidin (red), ECs are tagged with vWF antibody and biotinylated anti-rabbit IgG linked to strepavidin-linked Alexa Fluor 568 (red), SMCs are tagged with α-SMA antibody linked to Alexa Fluor 568 (red), ang1–256 is immunostained with FLAG antibody conjugated to Alexa Fluor 647 (green), and nuclei are stained with DAPI (blue). Merged images show that ang1–256 localizes to CMs, ECs, and SMCs. Scale bars = 50 μm.
Ang1–256 reduces PE-induced cardiac hypertrophy
Ang1 monomer levels decrease in PE-induced cardiac hypertrophy (Fig. 3B), so we determined whether replacement of ang1 monomer attenuates cardiac hypertrophy. We retroorbitally injected C57 mice with ang1–256/pcDNA or pcDNA alone, and the next day implanted osmotic pumps containing PE or saline. Mice in control and PE groups received pcDNA. Mice in control and ang1–256 groups received saline-filled pumps. On day 6, we found that PE increased LV/tibia ratios, whereas mice given PE + ang1–256 had significantly lower LV/tibia ratios (Fig. 6A). We examined mRNA levels (real-time PCR) of fetal genes that increase during cardiac hypertrophy. PE increased mRNA levels of ANP (Fig. 6B), BNP (Fig. 6C), collagen III (Fig. 6D), skeletal actin (Fig. 6E), and βMHC (Fig. 6F). In contrast, ang1–256 decreased mRNA levels for each of those fetal genes (Fig. 6B–F) as well as for SMA (Fig. 6G) mRNA levels ± PE treatment. Ang1–256 protein completely blocked the PE-induced increases in collagen III, skeletal actin, and βMHC, maintaining normal transcript levels.
Figure 6.
Ang1–256 monomer reduces cardiac hypertrophy in vivo. Ang1–256/pcDNA (ang1–256) or pcDNA (control) was retroorbitally injected into C57 mice. On day 2, mice were given PE or saline via pumps (n=4/group; studies done in duplicate). A) At day 6, PE increased LV/tibia ratios, and ang1–256 monomer blunted PE-induced increases in LV/tibia ratios. *P = 0.009; **P=0.02. B–G) RT-PCR analysis shows PE up-regulated mRNA levels of ANP (B), BNP (C), collagen III (D), skeletal actin (E), and (F) βMHC, but not SMA (G). Ang1–256 monomer reduced ANP, BNP, collagen III, skeletal actin, βMHC, and SMA mRNA levels in the absence or presence of PE. *P ≤ 0.03; **P ≤ 0.02; ***P = 0.006.
Ang1–256 does not change tie2 phosphorylation, but up-regulates ILK
Ang1 monomers do not bind or activate tie2. However, Ang1 binding to EC α5β1 integrin in vitro induces complexation and activation of tie2 (26). Thus, we determined whether ang1–256 plasmid-based expression in heart tissue changes tie2 phosphorylation by conducting tie2 immunoprecipitation and Western blotting on hearts from C57 mice injected with ang1–256/pcDNA or pcDNA (control). At 1 and 2 days after plasmid injection, levels of tie2 phosphorylation were similar in hearts from control and ang1–256/pcDNA-injected mice (Fig. 7A). We also measured tie2 phosphorylation in hearts of mice with PE-induced cardiac hypertrophy. On day 6, levels of tie2 phosphorylation were similar among the groups (Fig. 7B). We examined (Western blotting) the effect of ang1–256 on mouse LV ILK protein levels. Ang1–256 ± PE increased ILK (Fig. 7C), a major regulator of integrin subunit β1- and β3-based signaling, survival, and CM contractility (14), which suggests that ang1–256 actions are integrin mediated.
Figure 7.
Ang1–256 monomer does not change LV tie2 phosphorylation, but increases ILK. A–C) Ang1–256/pcDNA (ang1–256) or pcDNA (control) was retroorbitally injected into C57 mice. A, B) Results of tie2 immunoprecipitation and Western blotting for pTyr and tie2 (studies done in duplicate) show that tie2 phosphorylations were unchanged in adult heart tissue on days 1 and 2 after plasmid injection (A) and on day 6 in PE-induced cardiac hypertrophy (B). C) Six days after plasmid injection, Western blotting of mouse LV shows that ILK protein levels were increased by ang1–256, either alone or with PE-induced cardiac hypertrophy. Studies done in duplicate; n = 4/group. *P = 0.01; **P = 0.03. ILK was normalized to GAPDH.
Ang1–256 monomer activates Akt, MAPKp42/44, and AMPK
To assess the effect of ang1–256 monomer on cardiac function, we examined major cardioprotective regulators of survival and energetics (akt, MAPKp42/44, AMPK, and FAK). We tracked LV levels of phosphorylated vs. total receptor over time (day 1–6) (Fig. 8A, C, E) and ±PE-induced cardiac hypertrophy (Fig. 8B, D, F). Ang1–256 monomer phosphorylated aktS473 and AMPKT172 with the largest increases on day 1, and lesser increases on days 2–6 (Fig. 8A, C) and ±PE treatment (Fig. 8B, D). PE-induced decreased AMPKT172 phosphorylation (Fig. 8D) is consistent with increased protein synthesis during pathological cardiac hypertrophy and reduces cardiac energetics. Ang1–256-mediated increases in AMPKT172 phosphorylation suggest reduced protein synthesis. Ang1–256 monomer increased phosphorylation of MAPKp42(T202)/44(T204) on day 1 only (Fig. 8E–F). Ang1–256 monomer did not alter FAKY397 or AMPKS485/S491 phosphorylation on days 1–6 or ±PE-induced cardiac hypertrophy (unpublished observations).
Figure 8.
Ang1–256 monomer activates Akt, AMPK, and MAPKp42/44. Ang1–256/pcDNA (ang1–256) or pcDNA (control) was retroorbitally injected into C57 mice. On day 2 (B, D, F), mice were given PE or saline (control) via pumps. Western blotting on mouse hearts measured phosphorylated vs. total protein (n=4/group; studies done in duplicate). Ang1–256 activated aktS473 (A) and AMPKT172 (C) at 1 (*P≤0.01), 2 (**P≤0.03), 3 (#P≤0.05), and 6 (##P≤0.04) days, and MAPKp42(T202)/44(T204) (E) on day 1 (*P=0.05) only. On day 6 (B, D, F), ang1–256 monomers phosphorylated LV akt S473 (B) and AMPKT172 (D) without (*P≤ 0.02) or with PE treatment (**P≤0.01), but did not alter MAPKp42/44 phosphorylation (F).
DISCUSSION
Ang1 mRNA/protein (Fig. 1) levels shift during physiological and pathological cardiac remodeling without changes in tie2 phosphorylation (Figs. 2and 7). This disparity was also seen in an MI model (27). These findings support a novel mechanism of action for ang1 in heart tissue, which our prior work suggested is integrin-mediated (3). Herein we show it is associated with changes in ILK, a molecule central to integrin-based signaling.
We show that integrin-binding ang1 monomers are abundant in mouse and human heart tissue (Fig. 2) and that they shift during cardiac remodeling (Fig. 3) and bind CMs and ECs (Fig. 3). These findings suggest a major role for ang1 monomer/integrin interactions in cardiac health and disease. Ang1–256 increased ILK in mouse LV (Fig. 7C). ILK binds the cytoplasmic tail of β1and β3 integrins, and we identified CM β1 and β3 subunits as those that interact with ang1 (3). ILK is abundant in human and mouse heart tissue and regulates physiological cardiac hypertrophy (28). ILK ablation in murine heart tissue causes cardiomyopathy and heart failure (28). In humans, loss of ILK causes a dilated cardiomyopathy. ILK promotes cell survival via aktS473. We showed that full-length ang1 (3) and ang1–256 monomers phosphorylate aktS473 (Fig. 8A, B) in mouse heart tissue and isolated CMs. ILK is important to CMs, which rely on ILK- and integrin-based interactions to support the force of contraction. Increased ILK blocks cardiac fibrosis, and we show that ang1–256 blocked PE-induced increases in collagen III (Fig. 6D).
Here, we introduce a new regulatory mechanism for ang1 receptor targeting that is based on changes in different ang1 quaternary forms. EC tie2 activation requires ang1 tetramers or larger (9, 29). Cartilage oligomeric matrix protein fused to ang1 linker/fibrinogen-like domains (COMP-ang1) forms mainly tetramers and pentamers and increases EC tie2 phosphorylation more than native ang1 (29, 30). COMP-ang1, but not native ang1, tracks with tie2 in adult heart and other tissues. Our data may explain this finding, in that we show native ang1 in mouse and human heart and other tissues is predominately composed of monomers, dimers, and trimers (Fig. 2), and these forms may act chiefly via integrins.
Ang1 monomer and multimer expressions were tissue specific. Multimers were abundant in adipose tissue, lung, and kidney (Fig. 2E, F). Monomers were prevalent in heart tissue (Fig. 2G, H). In support of this finding, COMP-ang1 weakly stains heart tissue but prominently labels lung tissue (30). Further, brain tissue has little tie2 (31), and we did not detect ang1 multimers in brain tissue, only monomers (Fig. 2). Ang1 has an antipermeability effect in brain tissue, and integrin-binding recombinant ang1 monomers blocked trans-EC permeability (13). Thus, our data suggest a new role for ang1 monomer/integrin interactions in brain tissue.
We found ang1 monomers and dimers in all tissues tested (Fig. 2), however, other studies using soluble tie2-Fc identified ang1 trimers, tetramers, and pentamers (10, 12). Because monomers and dimers show weak or no tie2 binding, they may not be detected with tie2-Fc. Use of soluble tie2-Fc to block the actions of ang1 may not disrupt monomer and dimer functions and may prevent ang1 from binding integrins and tie1. Also, our studies demonstrated the importance of ang1 antibody selection, as antibodies differ in the ang1 forms they detect (Fig. 2).
Akt and MAPKp42/44 (32) activities are decreased in failing human hearts (33). Akt phosphorylation prevents CM apoptosis and positively affects CM inotropism (34). Our studies show that integrin-binding ang1–256 monomer retains at least some of the functions of full-length ang1 (3), including akt and MAPKp42/44 activation (Fig. 8A, B, E, F). Another recombinant truncated ang1 that produces monomers and dimers and binds integrins, but does not phosphorylate tie2, also has some capacities of full-length ang1 (promotes EC adhesion, activates MAPKp42/44, and reduces EC permeability) (13). Besides CMs, ang1–256 localized to cardiac ECs and SMCs, indicating that these monomers act on vasculature, likely via integrins. Ang1 binds human umbilical vein endothelial cell (HUVEC) integrins (4), and ang1-driven angiogenesis in chorioallantoic membrane assays was inhibited completely by anti-α5β1 and partly by anti-αvβ3 function-blocking antibodies (26). Thus, ang1 monomer/integrin interactions may mediate some EC functions in vivo.
Here, we introduced new functions for ang1–256 monomers, including AMPK phosphorylation and decreased cardiac hypertrophy and fetal gene expressions. These new cardioprotective actions have several implications, all of which are consistent with improved cardiac function and energetics in injured myocardium.
AMPK phosphorylation is largely determined by α subunit phosphorylation at threonine 172 (35) and increases energy production and inhibits apoptosis, protecting the heart during stress (36). AMPK is a key regulator of energetics and is known as the “guardian of energy status” (37) in heart tissue. AMPK responds to stress by activating ATP-generating pathways (glycolysis, glucose uptake, fatty acid oxidation, and glycogenolysis) and down-regulating ATP-consuming pathways (protein synthesis and hypertrophy).
MI, hypertension, cardiac hypertrophy, and heart failure are associated with increases in collagen III. Increased collagen III causes fibrosis and myocardial stiffening (38). Ang1–256 monomers blunt PE-induced increase in collagen III, which may decrease pathological cardiac remodeling, preserving LV function.
In summary, we show that integrin-binding ang1 monomers have a regulatory role in cardiac remodeling. Ang1–256 monomers localize to CMs, ECs, and SMCs and block PE-induced cardiac hypertrophy, activating cardioprotective signaling pathways. These data introduce a novel mechanism of ang1 regulation, whereby quaternary forms are differentially expressed in vivo as a function of tissue type and remodeling state to direct receptor/cell type interactions. Such a mechanism may serve to coordinate ang1’s actions as a CM survival factor and vascular regulator during cardiac remodeling to preserve function and impede the development of heart failure.
Supplementary Material
Acknowledgments
This work was supported by U.S. National Institutes of Health (NIH) grant K02-HL071840-01, American Heart Association grant-in-aid 0455824T, grant R21-CA107976-01, and a Thomas Smith award to M.A.R.; grant K01-DK063970-01 and a David M. Bray Scholars in Medicine award to S.M.D; and NIH grant P01-CA45548 and philanthropic funds provided to Dr. Judah Folkman (Children’s Hospital, Boston, MA, USA).
References
- Dumont D J, Yamaguchi T P, Conlon R A, Rossant J, Breitman M L. tek, a novel tyrosine kinase gene located on mouse chromosome 4, is expressed in endothelial cells and their presumptive precursors. Oncogene. 1992;7:1471–1480. [PubMed] [Google Scholar]
- Korhonen J, Partanen J, Armstrong E, Vaahtokari A, Elenius K, Jalkanen M, Alitalo K. Enhanced expression of the tie receptor tyrosine kinase in endothelial cells during neovascularization. Blood. 1992;80:2548–2555. [PubMed] [Google Scholar]
- Dallabrida S M, Ismail N, Oberle J R, Himes B E, Rupnick M A. Angiopoietin-1 promotes cardiac and skeletal myocyte survival through integrins. Circ Res. 2005;96:e8–e24. doi: 10.1161/01.RES.0000158285.57191.60. [DOI] [PubMed] [Google Scholar]
- Carlson T R, Feng Y, Maisonpierre P C, Mrksich M, Morla A O. Direct cell adhesion to the angiopoietins mediated by integrins. J Biol Chem. 2001;276:26516–26525. doi: 10.1074/jbc.M100282200. [DOI] [PubMed] [Google Scholar]
- Suri C, Jones P F, Patan S, Bartunkova S, Maisonpierre P C, Davis S, Sato T N, Yancopoulos G D. Requisite role of angiopoietin-1, a ligand for the TIE2 receptor, during embryonic angiogenesis. Cell. 1996;87:1171–1180. doi: 10.1016/s0092-8674(00)81813-9. [DOI] [PubMed] [Google Scholar]
- Takahashi K, Ito Y, Morikawa M, Kobune M, Huang J, Tsukamoto M, Sasaki K, Nakamura K, Dehari H, Ikeda K, Uchida H, Hirai S, Abe T, Hamada H. Adenoviral-delivered angiopoietin-1 reduces the infarction and attenuates the progression of cardiac dysfunction in the rat model of acute myocardial infarction. Mol Ther. 2003;8:584–592. doi: 10.1016/s1525-0016(03)00230-2. [DOI] [PubMed] [Google Scholar]
- Siddiqui A J, Blomberg P, Wardell E, Hellgren I, Eskandarpour M, Islam K B, Sylven C. Combination of angiopoietin-1 and vascular endothelial growth factor gene therapy enhances arteriogenesis in the ischemic myocardium. Biochem Biophys Res Commun. 2003;310:1002–1009. doi: 10.1016/j.bbrc.2003.09.111. [DOI] [PubMed] [Google Scholar]
- Chen S L, Zhang B R, Mei J, Xu Z Y, Zhu J L, Cai K H, Huang S D, Liu Y L. Induction of angiogenesis in ischemic myocardium by adenovirus mediated angiopoietin-1 gene transfer, an experimental study. Zhonghua Yi Xue Za Zhi. 2003;83:637–640. [PubMed] [Google Scholar]
- Davis S, Papadopoulos N, Aldrich T H, Maisonpierre P C, Huang T, Kovac L, Xu A, Leidich R, Radziejewska E, Rafique A, Goldberg J, Jain V, Bailey K, Karow M, Fandl J, Samuelsson S J, Ioffe E, Rudge J S, Daly T J, Radziejewski C, Yancopoulos G D. Angiopoietins have distinct modular domains essential for receptor binding, dimerization and superclustering. Nat Struct Biol. 2003;10:38–44. doi: 10.1038/nsb880. [DOI] [PubMed] [Google Scholar]
- Procopio W N, Pelavin P I, Lee W M, Yeilding N M. Angiopoietin-1 and -2 coiled coil domains mediate distinct homo-oligomerization patterns, but fibrinogen-like domains mediate ligand activity. J Biol Chem. 1999;274:30196–30201. doi: 10.1074/jbc.274.42.30196. [DOI] [PubMed] [Google Scholar]
- Xu Y, Yu Q. Angiopoietin-1, unlike angiopoietin-2, is incorporated into the extracellular matrix via its linker peptide region. J Biol Chem. 2001;276:34990–34998. doi: 10.1074/jbc.M103661200. [DOI] [PubMed] [Google Scholar]
- Kim K-T, Choi H-H, Steinmetz M O, Maco B, Kammerer R A, Ahn S Y, Kim H-Z, Lee G M, Koh G Y. Oligomerization and multimerization are critical for angiopoietin-1 to bind and phosphorylate tie2. J Biol Chem. 2005;280:20126–20131. doi: 10.1074/jbc.M500292200. [DOI] [PubMed] [Google Scholar]
- Weber C C, Cai H, Ehrbar M, Kubota H, Martiny-Baron G, Weber W, Djonov V, Weber E, Mallik A S, Fussenegger M, Frei K, Hubbell J A, Zisch A H. Effects of protein and gene transfer of the angiopoietin-1 fibrinogen-like receptor-binding domain on endothelial and vessel organization. J Biol Chem. 2005;280:22445–22453. doi: 10.1074/jbc.M410367200. [DOI] [PubMed] [Google Scholar]
- Hannigan G E, Coles J G, Dedhar S. Integrin-linked kinase at the heart of cardiac contractility, repair, and disease. Circ Res. 2007;100:1408–1414. doi: 10.1161/01.RES.0000265233.40455.62. [DOI] [PubMed] [Google Scholar]
- Dallabrida S M, Zurakowski D, Shih S C, Smith L E, Folkman J, Moulton K S, Rupnick M A. Adipose tissue growth and regression are regulated by angiopoietin-1. Biochem Biophys Res Commun. 2003;311:563–571. doi: 10.1016/j.bbrc.2003.10.007. [DOI] [PubMed] [Google Scholar]
- McMahon D K, Anderson P A, Nassar R, Bunting J B, Saba Z, Oakeley A E, Malouf N N. C2C12 cells: biophysical, biochemical, and immunocytochemical properties. Am J Physiol. 1994;266:C1795–C1802. doi: 10.1152/ajpcell.1994.266.6.C1795. [DOI] [PubMed] [Google Scholar]
- Kim N N, Villarreal F J, Printz M P, Lee A A, Dillmann W H. Trophic effects of angiotensin II on neonatal rat cardiac myocytes are mediated by cardiac fibroblasts. Am J Physiol Endocrinol Metab. 1995;269:E426–E437. doi: 10.1152/ajpendo.1995.269.3.E426. [DOI] [PubMed] [Google Scholar]
- Mitcheson J S, Hancox J C, Levi A J. Cultured adult cardiac myocytes: future applications, culture methods, morphological and electrophysiological properties. Cardiovasc Res. 1998;39:280–300. doi: 10.1016/s0008-6363(98)00128-x. [DOI] [PubMed] [Google Scholar]
- Schoenfeld J R, Vasser M, Jhurani P, Ng P, Hunter J J, Ross J, Jr, Chien K R, Lowe D G. Distinct molecular phenotypes in murine cardiac muscle development, growth, and hypertrophy. J Mol Cell Cardiol. 1998;30:2269–2280. doi: 10.1006/jmcc.1998.0787. [DOI] [PubMed] [Google Scholar]
- Kim I, Ryan A M, Rohan R, Amano S, Agular S, Miller J W, Adamis A P. Constitutive expression of VEGF, VEGFR-1, and VEGFR-2 in normal eyes. Invest Ophthalmol Vis Sci. 1999;40:2115–2121. [PubMed] [Google Scholar]
- Goede V, Schmidt T, Kimmina S, Kozian D, Augustin H G. Analysis of blood vessel maturation processes during cyclic ovarian angiogenesis. Lab Invest. 1998;78:1385–1394. [PubMed] [Google Scholar]
- Davis S, Aldrich T H, Jones P F, Acheson A, Compton D L, Jain V, Ryan T E, Bruno J, Radziejewski C, Maisonpierre P C, Yancopoulos G D. Isolation of angiopoietin-1, a ligand for the TIE2 receptor, by secretion-trap expression cloning. Cell. 1996;87:1161–1169. doi: 10.1016/s0092-8674(00)81812-7. [DOI] [PubMed] [Google Scholar]
- Bragonzi A, Boletta A, Biffi A, Muggia A, Sersale G, Cheng S H, Bordignon C, Assael B M, Conese M. Comparison between cationic polymers and lipids in mediating systemic gene delivery to the lungs. Gene Ther. 1999;6:1995–2004. doi: 10.1038/sj.gt.3301039. [DOI] [PubMed] [Google Scholar]
- Chemin I, Moradpour D, Wieland S, Offensperger W B, Walter E, Behr J P, Blum H E. Liver-directed gene transfer: a linear polyethlenimine derivative mediates highly efficient DNA delivery to primary hepatocytes in vitro and in vivo. J Viral Hepat. 1998;5:369–375. doi: 10.1046/j.1365-2893.1998.00126.x. [DOI] [PubMed] [Google Scholar]
- Ferrari S, Pettenazzo A, Garbati N, Zacchello F, Behr J P, Scarpa M. Polyethylenimine shows properties of interest for cystic fibrosis gene therapy. Biochim Biophys Acta. 1999;1447:219–225. doi: 10.1016/s0167-4781(99)00153-0. [DOI] [PubMed] [Google Scholar]
- Cascone I, Napione L, Maniero F, Serini G, Bussolino F. Stable interaction between alpha5beta1 integrin and Tie2 tyrosine kinase receptor regulates endothelial cell response to Ang-1. J Cell Biol. 2005;170:993–1004. doi: 10.1083/jcb.200507082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandhu R, Teichert-Kuliszewska K, Nag S, Proteau G, Robb M J, Campbell A I, Kuliszewski M A, Kutryk M J, Stewart D J. Reciprocal regulation of angiopoietin-1 and angiopoietin-2 following myocardial infarction in the rat. Cardiovasc Res. 2004;64:115–124. doi: 10.1016/j.cardiores.2004.05.013. [DOI] [PubMed] [Google Scholar]
- White D E, Coutu P, Shi Y F, Tardif J C, Nattel S, St. Arnaud R, Dedhar S, Muller W J. Targeted ablation of ILK from the murine heart results in dilated cardiomyopathy and spontaneous heart failure. Genes Dev. 2006;20:2355–2360. doi: 10.1101/gad.1458906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho C H, Kammerer R A, Lee H J, Steinmetz M O, Ryu Y S, Lee S H, Yasunaga K, Kim K T, Kim I, Choi H H, Kim W, Kim S H, Park S K, Lee G M, Koh G Y. COMP-Ang1: a designed angiopoietin-1 variant with nonleaky angiogenic activity. Proc Natl Acad Sci U S A. 2004;101:5547–5552. doi: 10.1073/pnas.0307574101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho C H, Kammerer R A, Lee H J, Yasunaga K, Kim K T, Choi H H, Kim W, Kim S H, Park S K, Lee G M, Koh G Y. Designed angiopoietin-1 variant, COMP-Ang1, protects against radiation-induced endothelial cell apoptosis. Proc Natl Acad Sci U S A. 2004;101:5553–5558. doi: 10.1073/pnas.0307575101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong A L, Haroon Z A, Werner S, Dewhirst M W, Greenberg C S, Peters K G. Tie2 expression and phosphorylation in angiogenic and quiescent adult tissues. Circ Res. 1997;81:567–574. doi: 10.1161/01.res.81.4.567. [DOI] [PubMed] [Google Scholar]
- Ravingerova T, Barancik M, Strniskova M. Mitogen-activated protein kinases: a new therapeutic target in cardiac pathology. Mol Cell Biochem. 2003;247:127–138. doi: 10.1023/a:1024119224033. [DOI] [PubMed] [Google Scholar]
- Baba H A, Stypmann J, Grabellus F, Kirchhof P, Sokoll A, Schafers M, Takeda A, Wilhelm M J, Scheld H H, Takeda N, Breithardt G, Levkau B. Dynamic regulation of MEK/Erks and Akt/GSK-3beta in human end-stage heart failure after left ventricular mechanical support: myocardial mechanotransduction-sensitivity as a possible molecular mechanism. Cardiovasc Res. 2003;59:390–399. doi: 10.1016/s0008-6363(03)00393-6. [DOI] [PubMed] [Google Scholar]
- Latronico M V G, Costinean S, Lavitrano M L, Peschle C, Condorelli G. Regulation of cell size and contractile function by AKT in cardiomyocytes. Ann N Y Acad Sci. 2004;1015:250–260. doi: 10.1196/annals.1302.021. [DOI] [PubMed] [Google Scholar]
- Kemp B E, Mitchelhill K I, Stapleton D, Michell B J, Chen Z P, Witters L A. Dealing with energy demand: the AMP-activated protein kinase. Trends Biochem Sci. 1999;24:22–25. doi: 10.1016/s0968-0004(98)01340-1. [DOI] [PubMed] [Google Scholar]
- Russell R R, 3rd, Li J, Coven D L, Pypaert M, Zechner C, Palmeri M, Giordano F J, Mu J, Birnbaum M J, Young L H. AMP-activated protein kinase mediates ischemic glucose uptake and prevents postischemic cardiac dysfunction, apoptosis, and injury. J Clin Invest. 2004;114:495–503. doi: 10.1172/JCI19297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardie D G. AMP-activated protein kinase: the guardian of cardiac energy status. J Clin Invest. 2004;114:465–468. doi: 10.1172/JCI22683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedak P W, Verma S, Weisel R D, Li R K. Cardiac remodeling and failure From molecules to man (Part II) Cardiovasc Pathol. 2005;14:49–60. doi: 10.1016/j.carpath.2005.01.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.