Abstract
Objective To examine the relationship between a cumulative risk model and caregiver quality of life (QOL) in pediatric asthma and determine whether caregiver QOL is predicted by a linear or quadratic model of cumulative risk. Methods One hundred and ninety-three families of children between the ages of 5 and 12 years with mild to severe asthma completed a background questionnaire and measures of QOL, asthma severity, family burden, and family stress. A cumulative risk model based on risk factors from these measures was calculated for each caregiver. Results The cumulative risk model significantly predicted caregiver QOL as a quadratic function. Caregivers with numerous risk factors experienced a dramatic worsening of QOL. Conclusions Findings suggest that caregiver QOL is best predicted by the interaction and not the summation of these factors. Interventions focused on one area of family risk may be effective in reducing poor QOL in caregivers of children with asthma.
Keywords: asthma, caregiver, family, quality of life, risk factors
Parents of children with chronic illnesses, such as asthma, have higher rates of emotional distress than parents of well children due to the demands associated with caring for a chronically ill child, greater anxiety about their child's health, and even sleepless nights (Frankel & Wamboldt, 1998). Specifically, parents of children with chronic illnesses are at increased risk for a poorer health-related quality of life (QOL). Although there is evidence to suggest that when caregivers of adult patients report on their QOL it is related to outcomes such as disease morbidity (Markowitz, Gutterman, Sadik, & Papadopoulos, 2003), the association between parent QOL and child disease status is less clear (Price, Bratton, & Klinnert, 2002). As parents play a central role in child disease management, QOL research in pediatric asthma has begun to address such inconsistencies and focus on caregiver QOL as an important outcome in families with a child with asthma.
Previous studies have examined how factors such as negative affect, asthma severity, and family burden are each individually related to caregiver QOL (Annett, Bender, DuHamel, & Lapidus, 2003; Frankel & Wamboldt, 1998; Price et al., 2002). However, such factors rarely operate in isolation and thus many researchers have applied cumulative risk models to predict adverse outcomes (Sameroff, Seifer, Baldwin, & Baldwin, 1993; Seifer et al., 1996). These risk models are thought to more accurately reflect an individual's simultaneous exposure to more than one indicator of risk and increase predictive efficiency. Developmental psychologists have demonstrated that children's IQ and mental health problems can be reliably predicted over time by the number of risk factors children are exposed to rather than single environmental factors, such as poverty or parent mood (Evans & English, 2002; Gerard & Buehler, 2004; Sameroff et al., 1993; Seifer et al., 1996). Cumulative risk models have also been applied to the study of pediatric conditions. For instance, multiple indicators of risk accounted for greater morbidity (e.g., hospitalizations, emergency-room visits) in urban children with asthma than asthma severity or poverty alone (Koinis-Mitchell et al., 2007). Thus, considering multiple contributions to caregiver QOL may provide a more complete picture of the stressors experienced by caregivers as many of the reported contributions to caregiver QOL do not occur in isolation.
There are two ways to examine cumulative risk. Most researchers consider adverse outcomes as a result of a steady increase in risk, in that the total number of risk factors a given child or family experiences is examined for a particular outcome. This linear approach to risk analysis ignores the potential interactive nature of risk and dramatic worsening of the outcome (reflected in a quadratic trend) as a function of increasing risks. This shortcoming is present throughout much of the cumulative risk literature in child development (Dickstein et al., 1998; Evans & English, 2002; Gerard & Buehler, 2004; Seifer et al., 1996) and in fact, these studies may not have described how risks contribute to adverse outcomes as accurately as possible. An alternative to examining the linear effects of cumulative risk is to test for quadratic effects where there is a dramatic worsening of the outcome due to the interaction of risk factors. By not testing for a quadratic model and simply assuming that a linear decline in the outcome occurs, researchers may be overlooking those individuals who are likely to experience the most adverse outcomes (Jones, Forehand, Brody, & Armistead, 2002). Appleyard, Egeland, van Dulmen, and Sroufe (2005) suggest that researchers may therefore not target their interventions to those groups of individuals that would benefit the most from such an intervention. Thus, the aim of this study was to examine whether the cumulative risk associated with QOL for parents of children with asthma was linear or quadratic in nature.
We used a cumulative risk model based on the presence of six risk factors [e.g., family socioeconomic status (SES), one or two caregiver households, asthma severity, child QOL, family burden, and family stress] to predict caregiver QOL and improve upon the aforementioned shortcoming in the cumulative risk literature. Our risk factors were drawn from the research on caregiver QOL in pediatric asthma and were selected to represent different levels of the family system. Consistent with other risk research (Gerard & Buehler, 2004; Sameroff et al., 1993), SES determined by caregiver education and occupation was included in our risk model. These constructs have proven predictive of negative child outcomes, such as low levels of scholastic achievement and intelligence level (Bradley & Corwyn, 2002). Further, SES is often related to parent well-being and depression (Lorant, Deliège, Eaton, Philippot, & Ansseau, 2003). Household composition (one or two caregiver homes) was also chosen as a risk factor as the literature in developmental psychopathology has identified the absence of a father or step-father in the household as an indicator of risk (Dickstein et al., 1998; Sameroff et al., 1993; Seifer et al., 1996).
The relationship between child asthma severity and caregiver QOL is not clearly defined, perhaps because of the different methods used to measure asthma severity. Studies determining severity from a diary rating of symptoms (Annett et al., 2003) and healthcare utilization (Price et al., 2002) did not find an association between severity and caregiver QOL. However, Halterman et al. (2004) did find a relationship between asthma severity and caregiver QOL at baseline when using parent report of symptoms. Thus, we included a well-established measure of symptom expression to determine severity. Similarly, the relationship between child and caregiver QOL is not well-established. For instance, child QOL and caregiver QOL have been associated in children between the ages of 12 and 13, but not between the ages of 6 and 11 (Annett et al., 2003). One possible explanation for the lack of agreement between child and parent QOL scores in younger children is that the child QOL measure (Juniper et al., 1996a) was designed for use with children 7 years of age and older, and is not a valid measure for younger children in its present form. To address this possibility, we used a pictorial version of the measure designed by our research team.
Finally, family burden and family stress were included in our risk model. Family burden has been reported as a strong determinant of caregiver QOL in caregivers of children with mild to moderate asthma (Annett et al., 2003). Family stress was also included as families with a child with a pediatric illness experience numerous life events that deplete their resources to effectively cope with these events (Patterson & McCubbin, 1983). Thus, our choice of risk factors extended across the ecological domains thought to influence family adaptation to a chronic illness including economic conditions, disease severity, and family burden (Kazak, Rourke, & Crump, 2003).
The present study examined the relationship between a cumulative risk model and caregiver QOL in pediatric asthma. We also aimed to extend previous work on cumulative risk and adverse outcomes by assessing the predictive value of the interaction of risk, in addition to evaluating the model for traditional additive effects. Specifically, we hypothesized that cumulative risk indices would predict caregiver QOL in a nonlinear manner. Further, as the amount of risk increased, caregiver QOL would decrease.
Method
Participants
Participants included 193 children (63% boys and 37% girls) between the ages of 5 and 12 years (mean age of 7.8 years) with mild to severe asthma (22% mild, 30% mild persistent, 39% moderate persistent, and 9% severe persistent) and their primary caregivers (mean age of 35.3 years). Data were collected as part of a study assessing family routines and medication adherence among families with a child with asthma. Ninety-seven percent of families identified the primary caregiver as the child's mother, 56% of caregivers were married, and 87% had at least a high school degree or equivalent. Sixty-four percent of caregivers were Caucasian, 26% were African American, 3% were Hispanic, 2% were Native American, and 5% were of mixed race.
Families were recruited through a pediatric pulmonary clinic, a general pediatric practice clinic at a teaching hospital, and private pediatric practices in or near a midsize city in central New York State. Inclusion criteria included a primary diagnosis of asthma, child between the ages of 5 and 12 years, and the prescribed use of a daily controller medication. Exclusion criteria included the presence of other chronic health conditions that required a daily medication (e.g., diabetes), having exercise-induced asthma, being in foster care (due to informed consent restrictions), and not being able to read English. Of the 457 families identified as potential participants, 16% of families were not reachable by telephone, 22% declined to participate, 14% were ineligible, and 6% were enrolled but did not attend the lab visit. Thus, of those families that agreed to participate and were eligible (219 families), 94% of families completed the study. Although 206 families completed the study, 193 families had data available on all measures used in these analyses. The families not included in the analyses were missing data on measures collected in the home (e.g., burden, stress). Families with missing data did not differ from the retained families on any demographic variables (e.g., race, asthma severity, child age, and child gender).
Procedure
This study was approved by all relevant Institutional Review Boards. Interested families were contacted via telephone and invited to complete questionnaires and interviews about family life and asthma in a laboratory setting. At the visit, caregivers completed a background information questionnaire and measures of child asthma severity and QOL, among other measures. Children were interviewed separately and completed a measure of QOL in addition to other measures not used in these analyses. For children under 8 years of age, a picture version of the QOL scale was administered. Measures of family burden and family stress were collected at a home visit that occurred following the initial laboratory visit. Informed consent from caregivers and assent from children was obtained at the laboratory visit. All families were paid $50 for their participation.
Materials
Caregiver QOL
Caregivers completed the 13-item Pediatric Asthma Caregiver's Quality of Life Questionnaire (PACQLQ; Juniper et al., 1996b) designed to measure the impact of the child's asthma on the caregiver's daily activities (four questions), as well as the fear and worry associated with having a child with asthma (nine questions). Responses to items range from “all of the time” to “none of the time” or “very, very worried/concerned” to “not worried/concerned” on a 7-point scale. A total score is derived from the mean of all responses. Higher scores reflect a positive QOL. Cronbach's α of.93 for overall caregiver QOL was computed for this sample. This self-report measure has been validated by other health-related QOL measures, such as the Global Rating of Change Questionnaires (Juniper, Guyatt, Willan, & Griffith, 1994).
Family SES
Primary caregivers completed the Hollingshead Index of Social Status (Hollingshead, 1975) in the aforementioned background questionnaire, which includes information on the education level and occupation of each parent. Scores on the Hollingshead measure ranged from 8 to 66 (M = 38.51, SD = 16.7), suggesting that families from all socioeconomic levels were included in our sample.
Household Type
In the background questionnaire, caregivers were asked to report their marital status (e.g., single, married, separated, divorced, remarried, widowed, and cohabitating). Caregivers who were married, remarried, or cohabitating were classified as two-parent homes and those who reported being single, separated, divorced, or widowed were designated as one-parent homes.
Asthma Severity
Child asthma severity (mild, mild persistent, moderate persistent, or severe persistent) was determined from the Functional Severity of Asthma Scale, Last Year Version (Rosier et al., 1994), completed by the primary caregiver. This measure consists of a 6-item scale that assesses aspects of the child's illness, such as symptoms and night wakening, over the past year. Scores ranging from 0 to 4 were classified as mild, scores from 5 to 8 were classified as mild persistent, scores from 9 to 14 were classified as moderate persistent, and scores from 15 to 22 were classified as severe persistent. An internal consistency of.70 was reported for this sample. The FSS has been validated with school days missed, medication usage, pulmonary function, and number of medical care visits over the past year (Rosier et al., 1994).
Child QOL
Children completed the Pediatric Asthma Quality of Life Questionnaire (PAQLQ; Juniper et al., 1996a), a 23-item questionnaire that assesses the child's physical (10 questions), emotional (eight questions), and social (five questions) impairment due to asthma over the previous 7 days. Responses to items range from “all of the time” to “none of the time” or “extremely bothered” to “not at all bothered” on a 7-point scale. A total score is calculated from the mean of all responses. Higher scores represent no impairment. The PAQLQ has been validated with clinical asthma control outcomes, such as β-agonist use and morning peak flow rates (Juniper et al., 1996a). For the established version of the PAQLQ, Cronbach's α of.93 for overall QOL was reported.
Although the PAQLQ is valid for use with children as young as 7 years of age, our research team has found that children this age and younger better understand a pictorial version of the scale.1 Therefore, a pictorial version of the PAQLQ, which presents children with a line that is anchored by three thermometers that vary in the amount of “fill,” was administered to children between the ages of 5 and 7. At one extreme, the empty thermometer corresponds to “not at all” or a score of 7, at the other extreme the full thermometer corresponds to “a lot” or a score of 1, and intermediary is a half full thermometer. After the child marks along the line somewhere below the three thermometers, the mark is converted to a score between 1 and 7 depending on where the child marked his or her answer. A scoring template is used to consistently score responses that do not fall at either end of the continuum or in the middle of the scale. Children are asked to match their response to the corresponding thermometer or space in between the thermometers after they have practiced using the scale to answer questions such as, “How much do you like ice cream?” Cronbach's α of.87 for the total score was calculated for the subgroup of children <8 years of age.
Family Burden
The burden and impact of child asthma on the family was measured by the Impact on the Family Scale (IOF; Stein & Riessman, 1980), a 27-item inventory completed by the primary caregiver. The scale includes items about family finances, familial and social interactions, and personal strain and items are rated on a 4-point scale with total scores ranging from 27 to 108. Coefficient α of.95 was computed for this sample. The IOF measure has been validated with caregiver scores on the Psychiatric Symptom Index (PSI; Ilfeld, 1976) and number of hospitalizations and days of hospitalization.
Family Stress
Primary caregivers completed the 66-item Family Inventory of Life Events (FILE; Patterson & McCubbin, 1983) to assess family life stress. This measure is an inventory of life events and changes the family has experienced over the previous year, such as a child moving out of the home, retirement, or increased marital tension. Items are reported as having occurred or not and a total family score is calculated (Cronbach's α =.83). The FILE has been validated with another measure of family functioning, the Family Environment Scale (FES; Moos & Moos, 1981).
Cumulative Risk Model
In calculating cumulative risk indices, continuous risk variables (e.g., SES, asthma severity, child QOL, family burden, and family stress) were first standardized into z-scores. Before being combined as one variable, z-scores were calculated separately for child QOL scores for 5- to 7-year-olds and QOL scores for 8- to 12-year-olds. Although risk factors are traditionally dichotomized (Sameroff et al., 1993; Seifer et al., 1996), risk indices in health literature looking at issues such as high blood pressure or cardiovascular disease are often created from standardized variables (Goodman, Dolan, Morrison, & Daniels, 2005). Such a technique preserves the full range of scores in analyses and prevents the loss of important predictive information that results from dichotomizing variables (Whisman & McClelland, 2005). For our dichotomous variable, household type, families with one caregiver living in the home were placed in the risk category for this variable and assigned a score of 1. To mirror possible negative z-scores, caregivers of two-parent households were assigned a score of −1.2 As positive scores on risk factors suggest the presence of risk relative to other participants, variables in which high scores reflected less risk (e.g., child QOL and SES) were converted to negative numbers. The six risk scores were then summed to calculate the total caregiver risk score.
Statistical Analyses
All analyses were performed using SPSS version 14.0 software (Statistical Product and Service Solutions 14.0; SPSS Inc., Chicago, IL, USA). Descriptive statistics of each risk variable were generated and correlational analyses were conducted to ensure that caregiver QOL was significantly associated with all risk variables. A simple t-test and analysis of variance (ANOVA) were also used to determine possible control variables (e.g., minority status, recruitment site). Due to the low percentage of Hispanic, Native American, and mixed race families in our sample, we included caregivers in these racial categories as minority along with African-American families. For those caregivers with positive risk indices, we calculated the percentage of caregivers scoring above the mean on each risk variable to identify which risk factors were experienced most frequently within this group. Next, we determined risk variable mean scores and confidence intervals for caregivers with positive cumulative risk indices and caregivers with negative cumulative risk indices. T-test analyses were used to test for mean differences between these groups of caregivers on each risk variable. As cumulative risk scores were positively skewed, a square root transformation was used to bring cumulative risk scores to a normal distribution. Using a hierarchical multiple regression approach, control variables were entered first to control for differences in QOL based on these variables. We entered cumulative risk as a linear term in step two and as a quadratic term in step three. Finally, to test if commonly experienced risk factors were driving the overall effect, we conducted analyses removing the two most frequently occurring risk variables.
Results
Risk Measures and Cumulative Risk Indices
Table I presents descriptive information on each of the risk measures as well as total cumulative risk indices. Cumulative risk scores ranged from −7.04 to 10.69 (M = −0.34, SD = 3.63) with 42% of caregivers having a positive risk index (indicating the presence of increased risk in relation to other participants in the study). Cumulative risk indices differed by caregiver race [t (191) = 5.99, p <.01] in that caregivers of minority status had higher cumulative risk scores. Cumulative risk indices also differed by recruiting site [F (2, 190) = 41.05, p <.01], with families recruited from the general ambulatory pediatric clinic at a teaching hospital reporting higher risk indices. Therefore, caregiver race and recruitment site were controlled for in all subsequent analyses.
Table I.
Descriptive Statistics of Continuous Risk Factors and Cumulative Risk Indices
| Measure | M | SD | Range | Correlation (r) with QOL |
|---|---|---|---|---|
| Family burden (IOF) | 40.22 | 12.80 | 22–81 | −.59** |
| Family stress (FILE) | 9.87 | 6.51 | 0–39 | −.21** |
| Child QOL (PAQLQ) | .26** | |||
| Ages 5–7 | 4.64 | 1.44 | 1–7 | |
| Ages 8–12 | 5.16 | 1.15 | 2.43–7 | |
| Asthma severity (FSS) | 8.49 | 4.75 | 0–23 | −.55** |
| SES (Hollingshead) | 38.51 | 16.70 | 8–66 | .38** |
| Cumulative risk | −.34 | 3.63 | −7.04 to 10.69 | −.63** |
**p <.01.
Of those families with positive risk indices (42% of the sample), 84% were in the risk category for family burden, 80% were in the risk category for SES, 72% were in the risk category for asthma severity, 72% were in the risk category for child QOL, 65% were in the risk category for household type, and 59% were in the risk category for family stress. Further, the mean score of each risk variable significantly differed between caregivers with positive cumulative risk scores and caregivers with negative cumulative risk scores (Table II).
Table II.
Means, Standard Deviations, and Confidence Intervals for Each Risk Variable for Negative and Positive Cumulative Risk Indices
| Caregivers with negative cumulative risk indices |
Caregivers with positive cumulative risk indices |
||||||
|---|---|---|---|---|---|---|---|
| Risk variable | M | SD | 95% CI (lower limit, upper limit) | M | SD | 95% CI (lower limit, upper limit) | t |
| Family burden | 34.08 | 10.09 | 32.18–35.98 | 48.52 | 11.34 | 46.03–51.02 | −9.32** |
| Family stress | 7.95 | 5.03 | 7.00–8.89 | 12.46 | 7.36 | 10.85–14.08 | −5.07** |
| Ages 5–7 QOL | 5.25 | 1.17 | 4.93–5.57 | 3.82 | 1.37 | 3.39–4.26 | 5.48** |
| Ages 8–12 QOL | 5.67 | .91 | 5.44–5.92 | 4.44 | 1.06 | 4.11–4.78 | 6.18** |
| Asthma severity | 6.47 | 3.56 | 5.80–7.14 | 11.23 | 4.80 | 10.18–12.29 | −7.92** |
| SES | 47.25 | 13.16 | 44.78–49.73 | 26.66 | 13.40 | 23.72–29.61 | 10.66** |
**p <.01.
Caregiver QOL
The mean overall caregiver QOL score was 5.54 (SD = 1.37, range 1.2–7.0). Overall caregiver QOL differed by caregiver race [t (191) = −4.59, p <.01] and recruiting site [F (2, 190) = 16.09, p <.01], with lower QOL associated with minority status and recruitment from the general ambulatory pediatric clinic. The mean QOL score for Caucasian caregivers was 5.86 (SD = 0.12) and 4.96 for minority caregivers (SD = 0.16). For caregivers recruited from the general ambulatory pediatric clinic, the mean QOL score was 4.96 (SD = 1.45), as compared to 6.06 (SD = 1.03) for those recruited from the pediatric pulmonary clinic and 5.88 (SD = 1.24) for those recruited from private pediatric practices. All risk variables were significantly associated with caregiver QOL in the expected direction (Table I). Mean caregiver QOL differed across household type [t (191) = −4.20, p <.01], in that caregivers in two-parent households had a higher QOL. The mean QOL score for caregivers in two-parent households was 5.82 (SD = 0.12) and 4.97 (SD = 0.16) for caregivers in one-parent households.
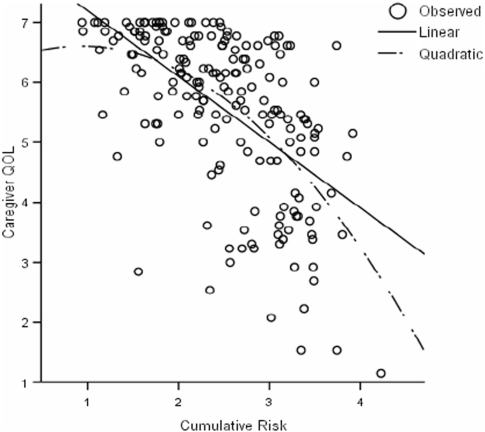
Test of Linear Versus Quadratic Trends
As presented in Table III and Fig. 1, the cumulative risk model significantly predicted overall caregiver QOL as a quadratic function [F (4, 189) = 29.32, p <.01] and was a significant improvement in fit over the linear function [ΔF (1, 189) = 7.13, p <.01]. The quadratic term accounted for additional variance in caregiver QOL beyond that accounted for by the linear term (R2 =.38, ΔR2 =.02). A comparison of effect sizes for the linear (f2 =.56) and quadratic (f2 =.62) cumulative approaches revealed a stronger relationship between caregiver QOL and the quadratic model. Caregiver QOL decreased as the presence of risk increased (Fig. 1).
Table III.
Hierarchical Multiple Regression Results for Controls, Cumulative Risk as a Linear Term, and Cumulative Risk as a Quadratic Term
| Predictor | Total R2 | ΔR2 | F | ΔF | df | B | SE |
|---|---|---|---|---|---|---|---|
| Step 1: Caregiver race and recruiting site | .12 | .12 | 13.27** | 13.27** | 2, 191 | .35 | .20 |
| −.10 | .14 | ||||||
| Step 2: Cumulative risk | .36 | .24 | 35.57** | 70.51** | 1, 190 | .41 | .55 |
| Step 3: Cumulative risk × cumulative risk | .38 | .02 | 29.32** | 7.13** | 1, 189 | −.30** | .11 |
**p <.01.
Figure 1.
Mean caregiver quality of life for each level of the cumulative risk model.
With family burden removed, the cumulative risk model significantly predicted overall caregiver QOL as a quadratic function [F (4, 189) = 21.15, p <.01] and was a significant improvement in fit over the linear function [ΔF (1, 189) = 5.39, p =.02]. Similarly, with SES removed, caregiver QOL was predicted as a quadratic function [F (4, 189) = 29.37, p <.01] and was a significant improvement in fit over the linear function [ΔF (1, 189) = 7.70, p <.01].
Discussion
The aim of this study was to determine whether the summation or interaction of risk factors is the best predictor of caregiver QOL in pediatric asthma. We have demonstrated that a dramatic worsening in caregiver QOL occurs as risk factors accumulate and interact with one another, suggesting that the relationship between risk and caregiver QOL is nonlinear. Conceptualizing risk as the interaction of risk factors and not the summation of those factors is a distinction that has not been explored in depth in the cumulative risk literature. However, findings from this study suggest that it is a distinction worth considering. If it is known that caregiver functioning dramatically worsens as more risk factors interact, we can begin to consider how best to intervene and improve the QOL of caregivers at the more extreme spectrum of risk.
In fact, had we ignored the possibility of an interactive effect and only tested our model for a linear term, a different conclusion regarding the relationship between cumulative risk and caregiver QOL would have been reached. In essence, considering only the linear function would have led us to believe that caregiver QOL steadily decreases as risks accumulate and that all caregivers experience a similar rate of decline in QOL. However, by testing for the quadratic trend, we found that this was not a true representation of how risk predicts caregiver QOL. Rather, due to the interaction of risk, a dramatic worsening in QOL occurs as risks accumulate. Caregivers with multiple risks present are, in fact, experiencing a sharper decline in QOL than the linear trend would have predicted, as depicted in Fig. 1.
This is in contrast to family life literature that suggests a pile-up of demands and stressors leads to poor outcomes for family members (Patterson, 2002). We have found that by conceptualizing the nature of risk as the interaction of risk factors and not merely the accumulation of risk factors, we are able to recognize that families with a greater number of risks are experiencing a dramatic compromise in caregiver QOL. Although this group with numerous risks represents a small percentage of families with asthma, it is an important group to identify. Consistent with public health statistics, these families are likely to demand the most resources of the health care system and to have the highest rates of health care utilization (Bernstein et al., 2003). Moreover, clinicians working long term with families might be in a unique position to recognize families that are experiencing multiple risk factors and may have a caregiver at risk for an impaired QOL.
Further, our finding suggesting the interaction of accumulated risk factors is encouraging in that families with numerous risks may benefit from any intervention attempt, no matter how narrowly focused. Even though we have found that risk factors interact with one another in predicting QOL, interventions targeting only one such area of family risk may be effective in improving caregiver QOL despite the presence of other risk factors. One strategy for intervening with families at risk for poor caregiver QOL is to use stepped care on risk indicators. Stepped care is conceptualized as focusing first on smaller, inexpensive interventions before implementing more complex and intrusive interventions (Davison, 2000). We suggest focusing stepped care on risk indicators that are most amenable to change instead of pursuing realms of family life that are less likely to change (e.g., economic factors). Specifically, researchers and clinicians should consider targeting interventions to reduce family burden or improve child QOL, as these were highly prevalent risk factors in our at-risk families. Strategies to reduce family burden might include parents and children working together to complete daily management tasks and developing plans to handle asthma-related emergencies before they arise (Fiese & Everhart, 2006).
We also found that our families with numerous risks were more likely to be of minority status, a finding that is in line with other cumulative risk research (Evans, 2004). However, it is likely that minority status may actually be a marker for other risk factors, such as economic resources, poor housing conditions, and parental education, and not necessarily a risk factor of its own accord (McLoyd, 2004). It might be that the stress related to caring for a child with asthma is exacerbated by markers of minority status (e.g., compromised resources), prompting an increase in risk accumulation and decline in caregiver QOL in these families. Single-parent caregivers also reported significantly lower QOL than caregivers who were married or cohabitating. One potential explanation is that a second adult in the home improves primary caregiver QOL by allowing caregivers to share the daily responsibilities associated with managing the child's asthma. Further, the presence of a second caregiver provides greater perceived social support for the primary caregiver, which improves caregiver functioning in families with a child with asthma (Frankel & Wamboldt, 1998).
Our findings suggest that in addition to minority status, single-parent households might also be a marker for impaired QOL. In fact, based on previous findings with the PACQLQ, the minimally important difference in QOL scores is.50, with a difference in scores of 1.0 considered of moderate importance (Juniper et al., 1994, 1996a). In comparing minority and Caucasian groups of caregivers in our sample, QOL scores differed by.90. Similarly, QOL scores between one and two-parent caregiver homes differed by.85. Thus, our findings suggest that differences in the QOL of these groups of caregivers are at the very least minimally important and close to moderately important. Clinicians and researchers should be aware of minority status and/or single-parent status as potential markers of poor caregiver QOL in pediatric asthma as such caregivers are likely experiencing a clinically significant decrease in QOL. Identifying these caregivers early on might allow clinicians and researchers to monitor caregiver functioning and suggest appropriate actions to ensure their QOL is not compromised. This might include helping the family access area support resources or strategies to reduce burden in the home.
Although minority status and single-parent household were associated with poorer caregiver QOL, we have found that a dramatic worsening of caregiver QOL is not reliant on a specific indicator of risk. For instance, when family burden and SES were removed from the cumulative risk model, our results remained unchanged. This suggests that neither factor is driving the overall effect of our model. Rather, it seems that a dramatic worsening in caregiver QOL occurs regardless of which risk factors are present in the caregiver's life. This finding underscores the importance of using stepped care approaches and suggests that such interventions will improve caregiver QOL regardless of which risk factor is initially targeted.
Limitations
One principal limitation of cumulative risk research is that such approaches treat risk factors equally, without considering the type or combination of risk factors present (Evans & English, 2002; Gerard & Buehler, 2004). Thus, it is not possible to say which risk factors or pattern of risk factors had the most detrimental impact on caregiver QOL (although we did find family burden and SES to be the most frequently occurring risk factors in our families with higher cumulative risk indices). Correlations between caregiver QOL and risk factors suggest that family burden and asthma severity may have the most impact on caregiver QOL. As all measures were completed by the same informant, however, it is difficult to ascertain the degree to which these correlations were primarily the result of method bias. Future research on caregiver QOL should attempt to reduce this issue of method bias by incorporating objective measures of constructs, such as asthma severity and observational measures of family functioning.
As our study was also correlational in nature, strong conclusions regarding causality cannot be made. Although this study conceptualized cumulative risk as predicting QOL, it is quite possible that the opposite is true and that caregiver QOL might influence certain risk factors. Such a limitation, however, highlights the continued importance of studying caregiver QOL in pediatric asthma. For instance, a caregiver with an impaired QOL may be less likely to adhere to the child's daily medication regimen, prompting an increase in child asthma symptoms. Future research should utilize longitudinal samples to determine causality between risk and QOL and consider whether reductions in risk factors, such as family stress or asthma severity, result in improvements in caregiver QOL. Moreover, longitudinal studies should be used to determine whether interventions targeting only one risk factor are effective in improving QOL in families with multiple risk factors present. In such families, risk factors are highly interconnected and thus, it is difficult to predict how effective such interventions will be from correlational findings.
It is important to note that our cumulative risk score is sample-specific and based on the mean of the sample on each risk variable. In fact, we were only able to identify families with high cumulative risk indices relative to other caregivers in our sample. It is quite possible that a family in our sample may no longer be in the risk category when compared to caregivers in other samples. Thus, it is difficult to generalize our cumulative risk findings to other samples. However, this is also a limitation that faces research dichotomizing variables based on sample-specific percentile cut-offs (Edwards, Eiden, Colder, & Leonard, 2006). Regardless, we urge other researchers to consider standardizing their continuous risk variables to prevent the loss of important predictive information when generating cumulative risk scores. We also suggest that researchers begin to move toward a more objective risk categorization in that few measures have empirically established and validated criteria for classifying an individual as above or below risk on a particular measure. This would allow researchers to move away from relying on sample-specific cut-offs to classify risk and enable risk research to generalize to other samples as well.
Further, as we required children to be prescribed a daily controller medication at study enrollment, our findings may not generalize to a sample of children with exercise-induced asthma or children who are not prescribed such a daily medication. Based on a validated measure of caregiver report of disease symptoms, children in our sample represented the full spectrum of severity for persistent asthma. However, as 22% of our sample met criteria for mild asthma based on parent report of symptoms, it may be that parents are under-reporting symptoms. Thus, future studies should utilize the new guidelines from the National Heart, Lung, and Blood Institute (NHLBI, 2007) that suggest a more precise determination of asthma severity from medication usage, lung functioning, symptoms, symptom interference with normal activities, and nighttime waking.
Finally, we recognize that our missing data were not random as missing data were most often associated with a family's failure to complete data packets at home. We suggest that although these families did not differ from our retained families on demographic variables, these families may have been experiencing more chaos in the home and were perhaps higher risk families. Our concern is that these highly stressed families may be the most difficult families to include in research studies in general. Researchers should focus on developing strategies to include and retain such families in future studies.
Conclusion
Findings from this study have important implications for cumulative risk literature and cumulative risk models in pediatric psychology, most notably that researchers should test their risk models for quadratic (or other nonlinear) effects. We found that caregiver QOL was best predicted by the interaction of risk factors, not the mere summation of such factors. Family environments in which caregivers are exposed to multiple, overlapping risk factors are more likely to have difficulty coping with their child's illness. Such families may mismanage their child's asthma, causing an exacerbation of asthma symptoms and overall decline in child health. Researchers and clinicians should utilize stepped care approaches in their interventions as targeting one area of family risk may improve caregiver QOL. The overall benefit of interventions for families may, in fact, be greater than expected because of the interactive nature of risk. Ultimately, the use of interventions, even those focused on one domain of risk, will lead to families being better able to manage their child's asthma.
Acknowledgments
Preparation of this article was supported, in part, by a grant from the National Institute of Mental Health (R01 MH51771) to B.H.F.
Conflicts of interest: None declared.
Footnotes
1Contact authors for specific details of the pictorial version of the PAQLQ.
2Coding caregivers of two-parent households as zero resulted in the same findings, as did removing household type from the cumulative risk model.
References
- Annett RD, Bender BG, DuHamel TR, Lapidus J. Factors influencing parent reports on quality of life for children with asthma. Journal of Asthma. 2003;40:577–587. doi: 10.1081/jas-120019030. [DOI] [PubMed] [Google Scholar]
- Appleyard K, Egeland B, van Dulmen MHM, Sroufe LA. When more is not better: The role of cumulative risk in child behavior outcomes. Journal of Child Psychology and Psychiatry. 2005;46:235–245. doi: 10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- Bernstein AB, Hing E, Moss AJ, Allen KF, Siller AB, Tiggle RB. Health care in America: Trends in utilization. Hyattsville, MD: National Center for Health Statistics; 2003. [Google Scholar]
- Bradley RH, Corwyn RF. Socioeconomic status and child development. Annual Review of Psychology. 2002;53:371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- Davison GC. Stepped care: Doing more with less. Journal of Consulting and Clinical Psychology. 2000;68:580–585. [PubMed] [Google Scholar]
- Dickstein S, Seifer R, Hayden LC, Schiller M, Sameroff AJ, Keitner G, et al. Levels of family assessment: II. Impact of maternal psychopathology on family functioning. Journal of Family Psychology. 1998;12:23–40. [Google Scholar]
- Edwards EP, Eiden RD, Colder C, Leonard KE. The development of aggression in 18 to 48 month old children of alcoholic parents. Journal of Abnormal Child Psychology. 2006;34:409–423. doi: 10.1007/s10802-006-9021-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW. The environment of childhood poverty. American Psychologist. 2004;59:77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- Evans GW, English K. The environment of poverty: Multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child Development. 2002;73:1238–1248. doi: 10.1111/1467-8624.00469. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Everhart RS. Medical adherence and childhood chronic illness: Family daily management skills and emotional climate as emerging contributors. Current Opinion in Pediatrics. 2006;18:551–557. doi: 10.1097/01.mop.0000245357.68207.9b. [DOI] [PubMed] [Google Scholar]
- Frankel K, Wamboldt MZ. Chronic childhood illness and maternal mental health-why should we care? Journal of Asthma. 1998;35:621–630. doi: 10.3109/02770909809048964. [DOI] [PubMed] [Google Scholar]
- Gerard JM, Buehler C. Cumulative environmental risk and youth maladjustment: The role of youth attributes. Child Development. 2004;75:1832–1849. doi: 10.1111/j.1467-8624.2004.00820.x. [DOI] [PubMed] [Google Scholar]
- Goodman E, Dolan LM, Morrison JA, Daniels SR. Factor analysis of clustered cardiovascular risks in adolescence. Circulation. 2005;111:1970–1977. doi: 10.1161/01.CIR.0000161957.34198.2B. [DOI] [PubMed] [Google Scholar]
- Halterman JS, Yoos HL, Conn KM, Callahan PM, Montes G, Neely TL, et al. The impact of childhood asthma on parental quality of life. Journal of Asthma. 2004;41:645–653. doi: 10.1081/jas-200026410. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. A four-factor classification of social status. New Haven, Unpublished manuscript. CT: Yale University; 1975. [Google Scholar]
- Ilfeld F. Further validation of a psychiatric symptom index in a normal population. Psychological Reports. 1976;39:1215–1228. [Google Scholar]
- Jones DJ, Forehand R, Brody G, Armistead L. Psychosocial adjustment of African American children in single-mother families: A test of three risk models. Journal of Marriage and Family. 2002;64:105–115. [Google Scholar]
- Juniper EF, Guyatt GH, Feeny D, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in children with asthma. Quality of Life Research. 1996a;5:35–46. doi: 10.1007/BF00435967. [DOI] [PubMed] [Google Scholar]
- Juniper EF, Guyatt GH, Feeny D, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in the parents of children with asthma. Quality of Life Research. 1996b;5:27–34. doi: 10.1007/BF00435966. [DOI] [PubMed] [Google Scholar]
- Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific quality of life questionnaire. Journal of Clinical Epidemiology. 1994;47:81–87. doi: 10.1016/0895-4356(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Rourke MT, Crump TA. Families and other systems in pediatric psychology. In: Roberts MC, editor. Handbook of pediatric psychology. New York: Guilford; 2003. pp. 159–175. [Google Scholar]
- Koinis-Mitchell D, McQuaid EL, Seifer R, Kopel SJ, Esteban C, Canino G, et al. Multiple urban and asthma-related risks and their association with asthma morbidity in children. Journal of Pediatric Psychology. 2007;32:582–595. doi: 10.1093/jpepsy/jsl050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorant V, Deliège D, Eaton W, Philippot P, Ansseau M. Socioeconomic inequalities in depression: A meta-analysis. American Journal of Epidemiology. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Markowitz JS, Gutterman EM, Sadik K, Papadopoulos G. Health-related quality of life for caregivers of patients with Alzheimer disease. Alzheimer Disease and Associated Disorders. 2003;17:209–214. doi: 10.1097/00002093-200310000-00003. [DOI] [PubMed] [Google Scholar]
- McLoyd VC. Linking race and ethnicity to culture: Steps along the road from inference to hypothesis testing. Human Development. 2004;47:185–191. [Google Scholar]
- Moos RH, Moos BS. Family environment scale manual. Palo Alto, CA: Consulting Psychologists Press, Inc; 1981. [Google Scholar]
- National Heart, Lung, and Blood Institute. Bethesda, MD: National Institutes of Health; 2007. Expert Panel Report 3: Guidelines for the diagnosis and management of asthma. [Google Scholar]
- Patterson JM. Integrating family resilience and family stress theory. Journal of Marriage and Family. 2002;64:349–360. [Google Scholar]
- Patterson JM, McCubbin HI. The impact of family life events and changes on the health of a chronically ill child. Family Relations: Journal of Applied Family & Child Studies. 1983;32:255–264. [Google Scholar]
- Price MR, Bratton DL, Klinnert MD. Caregiver negative affect is a primary determinant of caregiver report of pediatric asthma quality of life. Annals of Allergy, Asthma, & Immunology. 2002;89:572–577. doi: 10.1016/S1081-1206(10)62104-7. [DOI] [PubMed] [Google Scholar]
- Rosier MJ, Bishop J, Nolan T, Robertson CF, Carlin JB, Phelan PD. Measurement of functional severity of asthma in children. American Journal of Respiratory and Critical Care Medicine. 1994;149:1434–1441. doi: 10.1164/ajrccm.149.6.8004295. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Baldwin A, Baldwin C. Stability of intelligence from preschool to adolescence: The influence of social and family risk factors. Child Development. 1993;64:80–97. doi: 10.1111/j.1467-8624.1993.tb02896.x. [DOI] [PubMed] [Google Scholar]
- Seifer R, Sameroff AJ, Dickstein S, Keitner G, Miller I, Rasmussen S, et al. Parental psychopathology, multiple contextual risks, and one-year outcomes in children. Journal of Clinical Child Psychology. 1996;25:423–435. [Google Scholar]
- Stein RE, Riessman CK. The development of an Impact-on-Family Scale: Preliminary findings. Medical Care. 1980;18:465–472. doi: 10.1097/00005650-198004000-00010. [DOI] [PubMed] [Google Scholar]
- Whisman MA, McClelland GH. Designing, testing, and interpreting interactions and moderator effects in family research. Journal of Family Psychology. 2005;19:111–120. doi: 10.1037/0893-3200.19.1.111. [DOI] [PubMed] [Google Scholar]