Abstract
Parental monitoring has been defined as “a set of correlated parenting behaviors involving attention to and tracking of the child's whereabouts, activities, and adaptations.” This construct is of significant interest due to its relatedness to a broad range of youth risk behaviors, including risky sexual behavior, substance abuse, and poor adherence. However, to date, measures of parental monitoring are largely absent from the chronic illness literature. The present article focuses upon two key problems in the operationalization of the monitoring construct to date: (a) poor conceptual specificity in parenting constructs such as monitoring, overprotection, and over-involvement when used to date among youth with chronic conditions and (b) the confounding of existing measures of parental monitoring with items evaluating parental knowledge of youth activities, which has resulted in a lack of data regarding the mechanisms by which parents obtain their information. Recommendations for the future development of monitoring measures are discussed.
Keywords: adherence, chronic illness, parenting
During the past 20 years, research in the child development field has increasingly focused upon identifying specific aspects of parenting that are linked to problem outcomes in youth. One construct that has gained widespread attention, and has been used ubiquitously by family researchers, is parental monitoring. Parental monitoring has been defined as “a set of correlated parenting behaviors involving attention to and tracking of the child's whereabouts, activities, and adaptations” (Dishion & McMahon, 1998). Although the term “parental supervision” has frequently been used in place of “parental monitoring,” Dishion and McMahon encourage the use of the term monitoring because it encompasses a wider range of parenting behaviors than direct oversight of the child, including critical activities such as oversight through contacts with other adults who interact with the child or the child's peers. Low levels of parental monitoring have consistently predicted a variety of health risks across child developmental periods, including accidental injuries in young children (Morrongiello, Corbell, McCourt, & Johnston, 2006; Peterson & Brown, 1994) and substance abuse (Chilcoat & Anthony, 1996; Dishion & McMahon, 1998; Li, Stanton, & Feigelman, 2000), delinquency (Griffin, Botvin, Scheier, Diaz, & Miller, 2000; Pettit, Bates, Dodge, & Meece, 1999), risky sexual behavior (French & Dishion, 2003; Rose et al., 2005), and academic failure in older children and adolescents (Rodgers & Rose, 2001). Such findings have been demonstrated across samples of youth of differing ethnicity and socioeconomic status (Forehand, Miller, Dutra, & Chance, 1997). Hence, parental monitoring is of interest to pediatric psychology researchers due to its relatedness to a broad range of youth risk behaviors and due to the robust nature of the construct across different populations. In addition, in areas of particular interest to pediatric psychologists, such as regimen adherence behavior in youth with chronic conditions, numerous studies have recommended that parents maintain a high level of oversight of youth, in order to ensure optimal regimen adherence and good health outcomes (Silverstein et al., 2005). Surprisingly, in light of this, measures that assess parental monitoring are largely absent from the chronic illness literature.
The purpose of the present article is to examine the construct of parental monitoring in the chronic illness literature. We begin by reviewing the current status of monitoring measures developed for use with chronically ill youth. Next, we focus on two key problems in the operationalization of the monitoring construct to date, drawing on examples both from the general child development literature and the chronic illness literature. First, we discuss how lack of attention to parental monitoring in the chronic illness literature has led to inadequate empirical evaluation of whether parental monitoring and parental control are part of a continuum of behavior, where high parental monitoring can be equated with parental overprotection and overcontrol or whether they are discrete constructs. Second, we address the confounding of existing measures of parental monitoring in the child development literature with items evaluating parental knowledge of youth activities. This has resulted in a lack of data regarding the mechanisms by which parents obtain their information about what the youth is doing (e.g., direct supervision/presence, surveillance and information gathering, and youth disclosure). We illustrate this point with data from our own monitoring measure for parents of youth with diabetes. Finally, we conclude with recommendations for future development of monitoring measures that can be used with youth with chronic medical conditions.
Overview of Monitoring Measures Developed for Youth with Chronic Conditions
To date, a variety of measures to evaluate parental monitoring have been developed in general population samples of youth (Crouter & Head, 2002). The measurement approach has typically involved self- report on questionnaires, where the youth or parent provides information about the parent's knowledge of the youth's daily whereabouts and activities (e.g., knowledge of the youth's friends, how much time was time spent at school or in after-school activities, whether or not homework was completed, how free time is spent, etc.).
In contrast with the general child development literature, there are almost no measures of parental monitoring available for use with chronically ill youth. Items evaluating parental monitoring have frequently been embedded in other types of illness-specific measures. In the domain of parental support for the youth and parents’ support for one another, both the Diabetes Social Support Questionnaire- Family (La Greca & Bearman, 2002) and the Dads’ Active Disease Support scale (Wysocki & Gavin, 2004) include monitoring items that assess how much the parent supervised the youth's care. Monitoring items have also been included in measures of illness management. For example, the Diabetes Management Scale includes items assessing parental supervision of youth diabetes care (Frey & Denyes, 1989; Schilling, Grey, & Knafl, 2002).
Diary methods developed for assessing regimen adherence in youth with chronic conditions such as the Daily Phone Diary (Modi & Quittner, 2006) or the 24 Hour Recall Interview (Johnson, Perwien, & Silverstein, 2000) hold the potential to improve measurement of parental monitoring. However, interviewer probes must be included to prompt the respondent to report on parental direct supervision, tracking, and surveillance activities; to date, most of the diary methods developed for chronically ill youth only enquire about adult presence during youth activities (e.g., direct oversight).
Ellis et al. (2008) have developed a questionnaire measure of parental monitoring of regimen adherence for youth with diabetes—the Parent Monitoring of Diabetes Care (PMDC) scale. This measure specifically evaluates parental attempts to supervise and track their adolescent's completion of various diabetes care tasks. However, the PMDC is also limited by the lack of inclusion of items evaluating parental surveillance by means of information gathering from family members, school personnel and others who may play a role in completion of diabetes care.
In summary, measures of parental monitoring developed for general population samples have rarely been adapted and used with chronically ill youth. Furthermore, measures of parental monitoring of behaviors of interest to pediatric psychologists, such as youths’ regimen adherence, are lacking, although items measuring monitoring are often embedded in measures that assess other constructs, such as parental support. Methods such as diaries or recalls have been used in general population samples to evaluate monitoring but when used with chronic illness samples have been restricted to narrower aspects of monitoring, such as parental presence during completion of various aspects of the medical regimen. We turn now to definitional issues that are instructive to the goal of improving measurement of the monitoring construct.
Parental Monitoring and Parental Overprotection: The Devil is in the Measurement Details
One construct that may hold important conceptual similarities to parental monitoring is youth autonomy/parental overprotection. Dishion and McMahon (1998) have argued that in addition to parental supervision or surveillance, the parental monitoring construct includes any activity that facilitates parental awareness of the child's activities and communicates to the child that the parent is concerned about and aware of the child's activities. In such a definition, monitoring can also include structuring the child's environment to promote awareness of the child's activities, such as setting rules for behavior (e.g., curfews, acceptable peers, etc.). High levels of structuring or supervising the youth, however, could be intrusive or over-controlling, particularly for older adolescents. Hence, overprotection, or lack of promotion of youth autonomy, may have conceptual similarity to very high levels of parental monitoring. Demonstrating this point, at least one commonly used measure of parental overprotection developed for general population samples, the Parent Protection Scale (Thomasgard & Metz, 1999) includes items evaluating high levels of parental supervision. Wright, Mullen, West, and Wyatt (1993) developed a questionnaire measure of parental overprotection for use with children with chronic health conditions, the Vulnerable Child/Overprotecting Parent Scale (VCOP). In addition, Power, Dahlquist, Thompson, and Warren (2003) and Holmbeck et al. (2002) have used coded behavioral interaction tasks to evaluate parental overprotection in youth with juvenile rheumatoid arthritis and youth with spina bifida. Several research groups have developed questionnaire measures that assess the degree to which parents of youth with chronic conditions promote behavioral autonomy and/or independent decision making. These include the Diabetes Specific Parental Support for Adolescent's Autonomy Scale (DSPSAAS; Hanna, DiMeglio, & Fortenberry, 2005) and the Diabetes-Related Autonomy Scale (Miller & Drotar, 2003; Saletsky, 1991).
Measures to assess parental overprotection or parental granting of youth autonomy have been developed with the assumption that controlling, intrusive parenting, or overanxious parenting behaviors are detrimental to youth outcomes. For example, statements such as “perceptions of too much help will intimidate the receiver's freedom, ultimately decreasing self-esteem” (Hanna et al., 2005) and “by restricting individual freedom and ‘protecting’ the child from the consequences of his disease, parents may interfere with the development of social skills” (Power et al., 2003) are commonplace. However, closer examination of measures of parental overprotection/youth autonomy suggests that in fact these constructs have been largely operationalized as high levels of structure, helpfulness, or supervision/monitoring. For example, items on the VCOP largely assess consistency in discipline and structure (e.g., I try to reward my child immediately rather than with a promise of some later reward) rather than parental overanxiety or intrusiveness. Likewise, the DSPSAAS items evaluate supportive behaviors, including how much parents respond to youth questions about the medical regimen and show the youth how to complete adherence tasks. In their behavioral interaction task to evaluate maternal overprotection, Power et al. (2003) in fact operationalized the construct by coding for episodes of maternal helpfulness and directiveness toward the child. Given this, it is perhaps not surprising to find that none of these measures have in fact been linked to adverse general behavioral or other outcomes in youth. The broader empirical pediatric psychology literature has also found few links between overcontrol, overinvolvement, or overprotection and poor child adjustment or health outcomes to date (Berg et al., 2007; Mullins et al., 2004; Wiebe et al., 2005) and in fact overcontrol has been shown to serve as a protective factor in certain contexts (Tolou-Shams, Paikoff, McKirnan, & Holmbeck, 2007).
It appears that overprotection measures in the chronic illness literature to date have largely measured parental behavioral control—which includes parenting behaviors such as limit setting and parental monitoring—rather than parental psychological control—which includes intrusiveness and criticism/guilt induction. In the broader child development literature, it is psychological control, rather than behavioral control, that has been clearly linked to negative youth outcomes (particularly, depression and low self esteem; Barber, Stolz, & Olsen, 2005; Gray & Steinberg, 1999). From this perspective, psychological control is not part of a continuum of parenting behaviors that starts with low oversight and monitoring and ends with high levels of structuring and surveillance but is conceptually distinct. Our own data on parental monitoring among youth with diabetes also supports this distinction between behavioral control and psychological control. For example, Ellis et al. (2007) found that parental support for diabetes care and parental monitoring of youth completion of diabetes care were highly related whether ratings were obtained from parents (r =.46, p <.01) or youth (r =.62, p <.01). This suggests that competent parents engaged in both high levels of support and high levels of monitoring. In addition, there was no evidence of curvilinearity in the relationship between the PMDC measure and youth outcomes such as regimen adherence. Therefore, higher levels of parental monitoring—a form of behavioral control—did not result in poorer adherence on the part of youth as might be predicted if high levels of monitoring were equivalent to parental overprotection. However, psychological control was not directly measured in the study.
It is crucial that as pediatric psychologists develop better measures of parental monitoring, we distinguish between constructs such as monitoring, and intrusive and/or overanxious parenting. Poor operationalization of constructs affects the ability to interpret findings of studies and thus limits the development of best-practices parenting interventions for chronically ill youth and their families. For example, Anderson and Coyne's (1991) theory of “miscarried helping” proposes that due to concern for the sick youth, parents of chronically ill youth are prone to make attempts to help which fail because the help is “excessive (emphasis added), untimely or inappropriate”. Such theories are still widely referenced despite that fact that they have rarely been subjected to empirical evaluation. Better instrumentation will also allow better specificity regarding areas where high levels of monitoring could be health promoting for chronically ill youth (e.g., regimen adherence) and/or areas where it could be detrimental (e.g. depression, self-esteem). More attention to the ways that parenting is affected by child age would also inform instrument development in these areas. An example of careful measurement construction in this domain is shown by Holmbeck et al. (2002). The research group used a conceptual model that distinguished between parental overprotection, parental psychological control, and youth behavioral autonomy to develop their measure and items assessing monitoring, discipline, and related constructs (e.g., behavioral control) were not included in their overprotection measure. This is one of the few studies linking overprotection to problematic behavioral outcomes in chronic illness samples.
Confounds in Measurement: Parental Monitoring and Parental Knowledge of Youth Activities are not Equivalent
Prior to the past 5 years, measures of parental monitoring in the general child development literature almost always operationalized parental monitoring as parental knowledge; that is, parents were asked about their knowledge of youth activities, rather than about how they gathered information about their child's activities. Hence, parental knowledge of youth activities was de facto assumed to be equivalent to active attempts to supervise, keep track of and oversee the youth's activities. In 2000, Stattin and Kerr (Kerr & Stattin, 2000) called into question the validity of prior research on parental monitoring by pointing out the inherent problems with existing measures. In particular, they noted that parents could obtain knowledge of their child's activities in a variety of ways, including the possibility that the youth might disclose information about their whereabouts, behavior, and activities to the parent. If this was the case, then monitoring measures that operationalize monitoring as knowledge might in fact be evaluating something else—not parental oversight or surveillance, but in fact the youth's disclosure of information to their parent. Disclosure in turn might be influenced by factors such as parental warmth or the quality of the affective bond with the youth. In this case, parental supervision and/or active attempts to gather information about youth activities might not be the critical factor influencing youth outcomes, but rather qualities of the youth–parent affective bond. Stattin and Kerr tested their hypotheses by evaluating (a) the parent's knowledge of the youth's daily activities, (b) two methods by which the parent might obtain information about youth activities—the youth's spontaneous disclosure of information to the parent and parental solicitation of information from the youth or other people, (c) the degree of parental (behavioral) “control” or limit setting that occurred, and (d) the youth's involvement in delinquent activities. As in previous research, parental knowledge (“monitoring”) was still found to be a significant predictor of youth problem behavior. However, in multivariate analyses, the strongest predictor of what parents knew was youth disclosure rather than parental gathering of information from the youth or others. It should be noted, though, that parental presence during youth activities was not assessed and parental gathering of information from persons other than the youth was assessed with a single item.
Subsequent to the publication of these important studies, several child development researchers have attempted to improve the domain-specific measurement of parental monitoring and parental knowledge as well as to clarify whether parental knowledge of youth activities is a predictor of youth outcomes. The current consensus is that parental monitoring of adolescent behavior needs to be viewed as conceptually distinct from parental knowledge and both need to be measured (Crouter, Bumpus, Davis, & McHale, 2005; Fletcher, Steinberg, & Williams-Wheeler, 2004; Soenens, Vansteenkiste, Luyckx, & Goossens, 2006). In addition, Stattin and Kerr's (2000) work highlighted the lack of attention paid to date to constructing measures that evaluate different ways that parents gather information about their children's activities. For example, information gathering may be active (e.g., information is solicited from a neighbor) or passive (information is received from a neighbor), can be gathered from the youth or from others and can also occur through simple presence in the same context as the youth (e.g., information comes from attending sporting activities with the youth and observing his/her friendships). Since so little attention has been paid to date to measure different types of parental monitoring, recommendations that parents actively gather information about their youth's activities (The National Youth Anti-Drug Media Campaign, n.d.) may have been premature when in fact it is unclear what mechanisms of obtaining knowledge are most closely linked to positive youth outcomes. Since the chronic illness literature lags so far behind in the development of monitoring measures, almost no attention has been paid to defining and differentiating between mechanisms by which parents may gather information about and/or supervise youth activities, such as adherence behaviors, and hence even less is known about effective monitoring techniques in such families.
To illustrate that parental knowledge should be separated from parental monitoring and that exploration of monitoring processes can be of use with chronic illness samples, we reanalyzed data from an instrument development study using our PMDC monitoring measure. The measure was developed with a sample of 99 12- to 18-year-old adolescents with type 1 diabetes and their primary caregivers using cross-sectional methodology. All youth were managed by a multidisciplinary medical team and used either injected insulin or an insulin pump. Forty-seven percent were white, 36% were African-American, and the rest were of other race/ethnicity. The PMDC contains a number of items that, as is the case for most general population measures of monitoring developed to date, assess parental knowledge—in this case, of youth adherence behaviors (e.g., “When your child misses an insulin dose, how often do you know?” “When your child skips a blood glucose test, how often do you know?”). However, it also includes a number of items that do in fact assess parental monitoring. These items assess monitoring by two mechanisms: parental presence during diabetes care task completion (e.g., “How often were you present in the room when your child tested their blood glucose?” “How often were you present in the room when your child took insulin?”), and parental surveillance of diabetes care completion (e.g., “How often do you check the readings in your child's blood glucose meter?” “How often do you check your child's test strips and lancets to see if the expected number has been used?”).
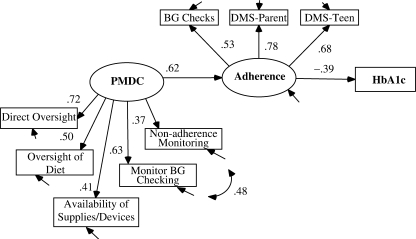
Figure 1 shows our original analysis (Ellis et al., 2008) of the concurrent validity of the PMDC. Structural equation modeling (SEM) was used to test a model where parental monitoring predicted youth adherence and, through adherence, metabolic control. Adherence was a latent construct evaluated by youth self-report, parent self-report, and objective data from blood glucose (BG) meters. In this analysis, parental monitoring was modeled as a unitary underlying construct, which was predicted by five monitoring subdomains (monitoring of the availability of medical supplies/devices, monitoring of BG testing, oversight of diet, monitoring of nonadherence, and direct oversight of diabetes care behaviors). Items evaluating parental knowledge were included in three of the five predictors. Different methods of monitoring (presence vs. surveillance) likewise were not confined to certain of the predictor scales and hence the relative importance of different monitoring approaches was not evaluated.
Figure 1.
SEM model results showing standardized path coefficients of relationship between PMDC, adherence, and metabolic control (hemoglobin A1c, HbA1c). All paths are significant, p <.05. Reprinted from Journal of Adolescent Health, 42, Ellis, D. A., Teplin, T., Podolski, C., Frey, M. A., Naar-King, S., & Moltz, K. The parental monitoring of diabetes care scale: Development reliability and validity of a scale to evaluate parental supervision of adolescent illness management, 2008, with permission from the Society for Adolescent Medicinie.
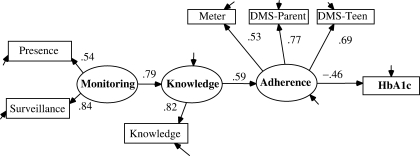
Model fit for this original conceptualization was highly acceptable (χ2 = 1.44, p =.32, comparative fit index [CFI] =.91, root mean square error of approximation [RMSEA] =.07; all paths significance at p <.05). However, an equally plausible model can be obtained by first constructing a separate parental knowledge scale using PMDC items that measure knowledge (nine items, α =.68) and then predicting parental knowledge about the youth's adherence behavior from the remaining PMDC items that actually evaluate parental monitoring. In this reanalysis, we also separated items assessing parental surveillance and parental presence into two different scales used as predictors of the latent monitoring construct (Figure 2). This model, which is more consistent with current definitions of monitoring, suggests that parental presence during completion of regimen adherence tasks and attempts by parents to track their youth's adherence behaviors may be different ways by which parents of chronically ill youth monitor adherence. SEM was used to evaluate this alternative model with AMOS 7.0 software. Parameters and standard errors were estimated using the bias corrected bootstrap method. Model fit statistics indicated a good model fit (χ2 = 1.35, p =.17, CFI =.97, RMSEA =.06] and all paths were significant (p <.01). A statistical test of the indirect effect of monitoring on adherence and hemoglobin A1c was performed using bootstrapped standard errors as recommended by Shrout and Bolger (2002). Both effects were significant (p <.01). Hence, consistent with other recent research, parental knowledge of youth adherence mediated the relationship between parental monitoring of diabetes care and youth adherence. The findings are limited by the cross-sectional nature of the study but suggest that such an alternative model of the monitoring construct is plausible.
Figure 2.
SEM model showing standardized path coefficients for relationship between parental monitoring, parental knowledge of youth's diabetes care completion, and adherence. All paths are significant, p <.01.
In summary, monitoring strategies include solicitation of information from the youth, allowing the youth to disclose information, observing and being present during youth activities, asking others about the youth's activities, and conducting other forms of tracking and surveillance. As monitoring measures for use with chronically ill youth are developed, it will be important to consider how these areas apply. For example, in the domain of regimen adherence, behavioral response products that signal whether or not a child has engaged in an activity (e.g., used medical supplies and medication usage) are relatively more available than response products that demonstrate whether or not a youth has spent time with a troubled peer, engaged in risky sex or skipped school. Hence, parents may not need to rely upon youth disclosure or solicit information from the youth to the same degree with adherence behaviors as much as when monitoring other types of behavior. Pediatric psychologists may identify mechanisms for monitoring that differ from those identified to date for general population samples of youth or may determine that certain forms of parental monitoring are differentially predictive of risk behavior in chronic illness samples. The development of appropriate psychoeducation for parents regarding how to best monitor the activities of their chronically ill child rests heavily upon our ability to evaluate the relative importance of such varied parental strategies for overseeing youth.
Recommendations for Developing Monitoring Measures in the Chronic Illness Literature
Parental monitoring has been linked to a variety of youth outcomes of particular interest to pediatric psychologists, including poor behavioral adjustment, risky sexual behavior, and inadequate regimen adherence. Measures to assess parental monitoring in samples of chronically ill youth are clearly needed given these findings. The information presented above suggests several areas for improving the development of monitoring measures as well as other related measures. First, it will be important to separate parental monitoring items from measures of disease support and illness management. The inclusion of these items decreases instrument specificity and can increase the likelihood of misinterpreting associations between variables. Second, the chronic illness literature exploring potential detrimental effects of overprotection/overinvolvement would benefit from increased measurement specificity. By disentangling parental monitoring, and other types of behavioral control, from parental psychological control, a more consistent pattern of findings of negative outcomes associated with such parenting styles may emerge. Conversely, ensuring that parental monitoring measures do not include items evaluating parental limit setting, clarity of rules, or consistency in discipline will help to determine whether this particular aspect of behavioral control is more important to youth outcomes than others.
Third, new measures must separate the processes of monitoring (surveillance, direct observation, and youth disclosure) from the outcome of monitoring (knowledge of youth activities), in order to identify those mechanisms by which parents may best monitor their child. Parents often question whether gathering information about their child's activities rather than simply accepting the information the child provides will violate the child's trust. In order to definitively answer whether “trust but verify” is the preferred strategy, a better understanding of how competent parents gather knowledge regarding their child's behavior and how these strategies are related to youth outcomes is needed. Additional research in this domain may also clarify whether better parental monitoring is dependent upon a strong youth–parent bond, as suggested by Stattin and Kerr (2000).
Due to the dearth of studies looking at parental monitoring in chronic illness samples, it is premature to conclude whether or not the processes of monitoring may differ for families with a chronically ill youth, or when illness-specific monitoring is conducted rather than monitoring of activities such as homework completion, school attendance, or association with problem peers. We noted earlier the possibility that direct supervision might be a more effective strategy when regimen adherence tasks are monitored due to the existence in many cases of medical technology that makes such supervision possible (e.g., counters on asthma medications and memory in BG meters). However, in order for such hypotheses to be evaluated, new measures capturing the various processes by which parents monitor chronically ill youth must first be developed and must include items evaluating domains such as direct supervision, surveillance of the youth through checking medical device and supply use, checking with the youth and other family members regarding adherence behavior or health status, gathering information from other adults and so on. Whether or not different types of monitoring are found to be more or less important when measures with good psychometric properties are constructed, it seems likely that the field will benefit from the development of illness-specific measures if the goal is to link parental monitoring with illness-specific health outcomes. For example, Ellis et al. (2007) showed that although a general measure of parental monitoring was highly related to a measure of illness-specific monitoring in youth with diabetes, only the illness-specific measure was related to adherence and metabolic control. Parental monitoring behaviors are also likely to vary from illness to illness when illness-specific health status is the outcome of interest; while parents of youth with asthma may need to routinely check that the child did not spend time in environments where smokers were present, such monitoring would be less important for parents of youth with other chronic conditions. The recommendation for use of illness-specific monitoring measures is consistent with prior calls for increased use of illness-specific measures (Drotar, 1997). Obtaining the perspective of multiple informants—that is, both the child and parent—will also be important, in part because social desirability biases may lead parents to overestimate their own monitoring.
A contextual view of the development of parenting behaviors that is consistent with social–ecological models of child outcomes (Bronfenbrenner, 1979; Brown, 2002; Kazak, 1992) would suggest that parenting behaviors do not emerge in a vacuum but are part of a bi-directional series of interactions between the youth and parent that develop over time and also that are influenced by cultural and community factors. For youth with externalizing behavior problems, such as problems with impulse control or disorganization, direct parental supervision and/or gathering of information from other adults (surveillance) may be the most effective way to obtain knowledge of youth activities. Conversely, youth with internalizing symptoms may respond to increases in parental warmth or general support by disclosing information about their activities so that parental surveillance is unnecessary. Youth age and maturity is clearly another area for consideration in this regard, as the eventual need for adolescents to become independent means that parents must ultimately decrease the amount of monitoring they engage in. Similarly, important interactions between family and extra-familial contexts and parental monitoring would be expected. For example, working parents have fewer opportunities to be present during youth activities and hence may be more likely to use other methods of monitoring (Waizenhofer, Buchanan, & Jackson-Newsom, 2004). Beyer, Bates, Pettit, and Dodge (2003) found that a high level of parental monitoring was most important to predicting externalizing behavior problems for youth living in disadvantaged neighborhoods, where more opportunities to engage in risky behaviors existed. As better measures are developed, consideration should be given to such important interactions between parenting behaviors and family or community-level effects as well.
Improved measures will likely depend as much on new understanding and clarity in delineating the subdomains foundational to parenting as on methodological improvements. However, pediatric psychology researchers also need to make better use of newer statistical methods that allow for better testing of latent constructs, factor structure relations, and assessment of measurement invariance across populations. In the areas of both SEM and item response theory, improved procedures for item selection, identification of item bias, and for establishing test and measurement invariance have been developed (Byrne & Stewart, 2006; Glockner-Rist & Hoijtink, 2003; Hays, Brown, Brown, Spritzer, & Crall, 2006; Teresi, 2006) and warrant increased use.
Children with chronic illnesses are a vulnerable population whose special needs have the potential to disrupt optimal parenting practices. Pediatric psychologists are in a unique position to inform the general child development literature with regard to whether a specific aspect of parenting behavior—careful monitoring of youth behavior—promotes child resiliency and positive outcomes among such at-risk youth. The development of improved measures is a much-needed step that will promote the accomplishment of this worthwhile goal.
Conflicts of interest: None declared.
References
- Anderson BJ, Coyne JC. ‘Miscarried helping’ in families of children and adolescents with chronic diseases. In: Johnson JH, Johnson SB, editors. Advances in child health psychology. Gainesville, FL: University of Florida Press; 1991. pp. 166–177. [Google Scholar]
- Barber BK, Stolz HE, Olsen JA. Parental support, psychological control, and behavioral control: Assessing relevance across time, culture, and method. Mongraphs of the Society for Research in Child Development. 2005;70:1–137. doi: 10.1111/j.1540-5834.2005.00365.x. [DOI] [PubMed] [Google Scholar]
- Berg CA, Wiebe DJ, Beveridge RM, Palmer DL, Korbel CD, Upchurch R, et al. Mother child appraised involvement in coping with diabetes stressors and emotional adjustment. Journal of Pediatric Psychology. 2007;32:995–1005. doi: 10.1093/jpepsy/jsm043. [DOI] [PubMed] [Google Scholar]
- Beyers JM, Bates JE, Pettit GS, Dodge KA. Neighborhood structure, parenting processes, and the development of youths’ externalizing behaviors: A multilevel analysis. American Journal of Community Psychology. 2003;31:35–53. doi: 10.1023/a:1023018502759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by design and nature. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Brown RT. Society of pediatric psychology presidential address: Toward a social ecology of pediatric psychology. Journal of Pediatric Psychology. 2002;27:191–201. doi: 10.1093/jpepsy/27.2.191. [DOI] [PubMed] [Google Scholar]
- Byrne BM, Stewart SM. Multigroup invariance of a second-order structure: A walk through the process. Structural Equation Modeling. 2006;13:287–321. [Google Scholar]
- Chilcoat HD, Anthony JC. Impact of parent monitoring on initiation of drug use through late childhood. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:91–100. doi: 10.1097/00004583-199601000-00017. [DOI] [PubMed] [Google Scholar]
- Crouter AC, Bumpus MF, Davis KD, McHale SM. How do parents learn about adolescents’ experiences? Implications for parental knowledge and adolescent risky behavior. Child Development. 2005;76:869–882. doi: 10.1111/j.1467-8624.2005.00883.x. [DOI] [PubMed] [Google Scholar]
- Crouter AC, Head MR. Parental monitoring and knowledge of children. In: Bornstein MH, editor. Handbook of parenting: Being and becoming a parent. 2nd. Vol. 3. Mahwah, NJ: Lawrence Erlbaum Associates; 2002. pp. 461–483. [Google Scholar]
- Dishion TJ, McMahon RJ. Parental monitoring and the prevention of child and adolescent problem behavior: A conceptual and empirical formulation. Clinical Child & Family Psychology Review. 1998;1:61–75. doi: 10.1023/a:1021800432380. [DOI] [PubMed] [Google Scholar]
- Drotar D. Relating parent and family functioning to the psychological adjustment of children with chronic health conditions: What have we learned? What do we need to know? Journal of Pediatric Psychology, 22. 1997:149–165. doi: 10.1093/jpepsy/22.2.149. [DOI] [PubMed] [Google Scholar]
- Ellis DA, Templin T, Podolski C, Frey MA, Naar-King S, Moltz K. The parental monitoring of diabetes care scale: Development, reliability and validity of a scale to evaluate parental supervision of adolescent illness management. Journal of Adolescent Health. 2008;42:146–153. doi: 10.1016/j.jadohealth.2007.08.012. [DOI] [PubMed] [Google Scholar]
- Ellis DA, Templin T, Podolski C, Frey MA, Naar-King S. The role of parental monitoring in adolescent health outcomes: Impact on regimen adherence in youth with type 1 diabetes. Journal of Pediatric Psychology. 2007;32:907–917. doi: 10.1093/jpepsy/jsm009. [DOI] [PubMed] [Google Scholar]
- Fletcher AC, Steinberg L, Williams-Wheeler M. Parental influences on adolescent problem behavior: Revisiting Sttatin and Kerr. Child Development. 2004;75:781–796. doi: 10.1111/j.1467-8624.2004.00706.x. [DOI] [PubMed] [Google Scholar]
- Forehand R, Miller KS, Dutra R, Chance MW. Role of parenting in adolescent deviant behavior: Replication across and within two ethnic groups. Journal of Consulting & Clinical Psychology. 1997;65:1036–1041. doi: 10.1037//0022-006x.65.6.1036. [DOI] [PubMed] [Google Scholar]
- French DC, Dishion T. Predictors of early initiation of sexual intercourse among high-risk adolescents. Journal of Early Adolescence. 2003;23:295–315. [Google Scholar]
- Frey MA, Denyes MJ. Health and illness self-care in adolescents with IDDM: A test of Orem's theory. Advances in Nursing Science. 1989;12:67–75. doi: 10.1097/00012272-198910000-00009. [DOI] [PubMed] [Google Scholar]
- Glockner-Rist A, Hoijtink H. The best of both worlds: Factor analysis of dichotomous data using item response theory and structural equation modeling. Structural Equation Modeling: A Multidisciplinary Journal. 2003;10:544–565. [Google Scholar]
- Gray MR, Steinberg L. Unpacking authoritative parenting: Reassessing a multidimensional construct. Journal of Marriage and Family. 1999;61:574–587. [Google Scholar]
- Griffin KW, Botvin GJ, Scheier LM, Diaz T, Miller NL. Parenting practices as predictors of substance use, delinquency, and aggression among urban minority youth: Moderating effects of family structure and gender. Psychology of Addictive Behaviors. 2000;14:174–184. doi: 10.1037//0893-164x.14.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna KM, DiMeglio LA, Fortenberry JD. Parent and adolescent versions of the diabetes-specific parental support for adolescents’ autonomy scale: Development and initial testing. Journal of Pediatric Psychology. 2005;30:257–271. doi: 10.1093/jpepsy/jsi036. [DOI] [PubMed] [Google Scholar]
- Hanna KM, Juarez B, Lenss SS, Guthrie D. Parent-adolescent communication and support for diabetes management as reported by adolescents with type 1 diabetes. Issues in Comprehensive Pediatric Nursing. 2003;26:145–158. doi: 10.1080/01460860390223871. [DOI] [PubMed] [Google Scholar]
- Hays RD, Brown J, Brown LU, Spritzer KL, Crall JJ. Classical test theory and item response theory analyses of multi-item scales assessing parents’ perceptions of their children's dental care. Medical Care. 2006;44:S60–S68. doi: 10.1097/01.mlr.0000245144.90229.d0. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN, Johnson SZ, Wills KE, McKernon W, Rose B, Erklin S, et al. Observed and perceived parental overprotection in relation to psychosocial adjustment in preadolescents with a physical disability: The mediational role of behavioral autonomy. Journal of Consulting and Clinical Psychology. 2002;70:96–110. doi: 10.1037//0022-006x.70.1.96. [DOI] [PubMed] [Google Scholar]
- Johnson SB, Perwien AR, Silverstein JH. Response to hypo- and hyperglycemia in adolescents with type I diabetes. Journal of Pediatric Psychology. 2000;25:171–178. doi: 10.1093/jpepsy/25.3.171. [DOI] [PubMed] [Google Scholar]
- Kazak AE. Family systems, social ecology, and chronic pediatric illness: Conceptual, methodological, and intervention issues. In: Akamatsu JT, Stephens MP, Hobfoll SE, Crowther JH, editors. Family health psychology. Series in applied psychology: Social issues and questions. Washington, DC: Hemisphere Publishing Corp; 1992. pp. 93–110. [Google Scholar]
- Kerr M, Stattin H. What parents know, how they know it, and several forms of adolescent adjustment: Further support for a reinterpretation of monitoring. Developmental Psychology. 2000;36:366–380. [PubMed] [Google Scholar]
- La Greca AM, Bearman KJ. The diabetes social support questionnaire-family version: Evaluating adolescents’ diabetes-specific support from family members. Journal of Pediatric Psychology. 2002;27:665–676. doi: 10.1093/jpepsy/27.8.665. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Follansbee D, Skyler JS. Developmental and behavioral aspects of diabetes management in youngsters. Children's Health Care. 1990;19:132–139. [Google Scholar]
- Li X, Stanton B, Feigelman S. Impact of perceived parental monitoring on adolescent risk behavior over 4 years. Journal of Adolescent Health. 2000;27:49–56. doi: 10.1016/s1054-139x(00)00092-6. [DOI] [PubMed] [Google Scholar]
- Miller VA, Drotar D. Discrepancies between mother and adolescent perceptions of diabetes-related decision-making autonomy and their relationship to diabetes-related conflict and adherence to treatment. Journal of Pediatric Psychology. 2003;28:265–274. doi: 10.1093/jpepsy/jsg014. [DOI] [PubMed] [Google Scholar]
- Modi AC, Quittner AL. Utilizing computerized phone diary procedures to assess health behaviors in family and social contexts. Children's Health Care. 2006;35:29–45. [Google Scholar]
- Morrongiello BA, Corbell M, McCourt M, Johnston N. Understanding unintentional injury-risk in young children I. The nature and scope of caregiver supervision of children at home. Journal of Pediatric Psychology. 2006;31:529–539. doi: 10.1093/jpepsy/jsj045. [DOI] [PubMed] [Google Scholar]
- Mullins LL, Fuemmeler BF, Hoff A, Chaney JM, Van Pelt J, Ewing C. The relationship of parental overprotection and perceived child vulnerability to depressive symptomotology in children with type 1 diabetes mellitus: The moderating influence of parenting stress. Children's Health Care. 2004;33:21–31. [Google Scholar]
- Peterson L, Brown D. Integrating child injury and abuse-neglect research: Common histories, etiologies, and solutions. Psychological Bulletin. 1994;116:292–315. doi: 10.1037/0033-2909.116.2.293. [DOI] [PubMed] [Google Scholar]
- Pettit GS, Bates JE, Dodge KA, Meece DW. The impact of after-school peer contact on early adolescent externalizing problems is moderated by parental monitoring, perceived neighborhood safety, and prior adjustment. Child Development. 1999;70:768–778. doi: 10.1111/1467-8624.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power TG, Dahlquist LM, Thompson SM, Warren R. Interactions between children with juvenile rheumatoid arthritis and their mothers. Journal of Pediatric Psychology. 2003;28:213–221. doi: 10.1093/jpepsy/jsg009. [DOI] [PubMed] [Google Scholar]
- Rodgers KB, Rose HA. Personal, family, and school factors related to adolescent academic performance: A comparison by family structure. Marriage & Family Review. 2001;33:47–61. [Google Scholar]
- Rose A, Koo HP, Bhaskar B, Anderson K, White G, Jenkins RR. The influence of primary caregivers on the sexual behavior of early adolescents. Journal of Adolescent Health. 2005;37:135–144. doi: 10.1016/j.jadohealth.2005.02.009. [DOI] [PubMed] [Google Scholar]
- Saletsky R. Autonomy and mother-child relations in a sample of adolescents with insulindependent diabetes (Doctoral dissertation, Western Reserve University, 1990) Dissertation Abstracts International. 1991;52:1081–1082. [Google Scholar]
- Schilling LS, Grey M, Knafl K. A review of measures of self-management of type 1 diabetes by youth and their parents. Diabetes Educator. 2002;28:796–808. doi: 10.1177/014572170202800520. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and non-experimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, et al. Care of children and adolescents with type 1 diabetes. Diabetes Care. 2005;28:186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- Soenens B, Vansteenkiste M, Luyckx K, Goossens L. Parenting and adoelscent problem behavior: An integrated model with adolescent self-disclosure and perceived parental knowledge as intervening variables. Developmental Psychology. 2006;42:305–318. doi: 10.1037/0012-1649.42.2.305. [DOI] [PubMed] [Google Scholar]
- Stattin H, Kerr M. Parental monitoring: A reinterpretation. Child Development. 2000;71:1072–1082. doi: 10.1111/1467-8624.00210. [DOI] [PubMed] [Google Scholar]
- Teresi JA. Overview of quantitative measurement methods: Equivalence, invariance, and differential item functioning in health applications. Medical Care. 2006;44:S39–S49. doi: 10.1097/01.mlr.0000245452.48613.45. [DOI] [PubMed] [Google Scholar]
- The National Youth Anti-Drug Media Campaign. (n.d.) Parents: The anti-drug. Retrieved June 1, 2007, from http://www.theantidrug.com/
- Thomasgard M, Metz WP. Parent-child relationship disorders: What do the Child Vulnerability Scale and the Parent Protection Scale measure? Clinical Pediatrics. 1999;38:347–356. doi: 10.1177/000992289903800605. [DOI] [PubMed] [Google Scholar]
- Tolou-Shams M, Paikoff R, McKirnan DJ, Holmbeck GN. Mental health and HIV risk among African American adolescents: The role of parenting. Social Work in Mental Health. 2007;5:27–58. [Google Scholar]
- Waizenhofer RN, Buchanan CM, Jackson-Newsom J. Mothers’ and fathers’ knowledge of adolescents’ daily activities: Its sources and its links with adolescent adjustment. Journal of Family Psychology. 2004;18:348–360. doi: 10.1037/0893-3200.18.2.348. [DOI] [PubMed] [Google Scholar]
- Wiebe DJ, Berg CA, Korbel C, Palmer DL, Beveridge RM, Upchurch R, et al. Children's appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology. 2005;30:167–178. doi: 10.1093/jpepsy/jsi004. [DOI] [PubMed] [Google Scholar]
- Wright L, Mullen T, West K, Wyatt P. The VCOP scale: A measure of overprotection in parents of physically vulnerable. Journal of Clinical Psychology. 1993;49:790–798. doi: 10.1002/1097-4679(199311)49:6<790::aid-jclp2270490606>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Gavin L. Psychometric properties of a new measure of fathers’ involvement in the management of pediatric chronic diseases. Journal of Pediatric Psychology. 2004;29:231–240. doi: 10.1093/jpepsy/jsh024. [DOI] [PubMed] [Google Scholar]