Abstract
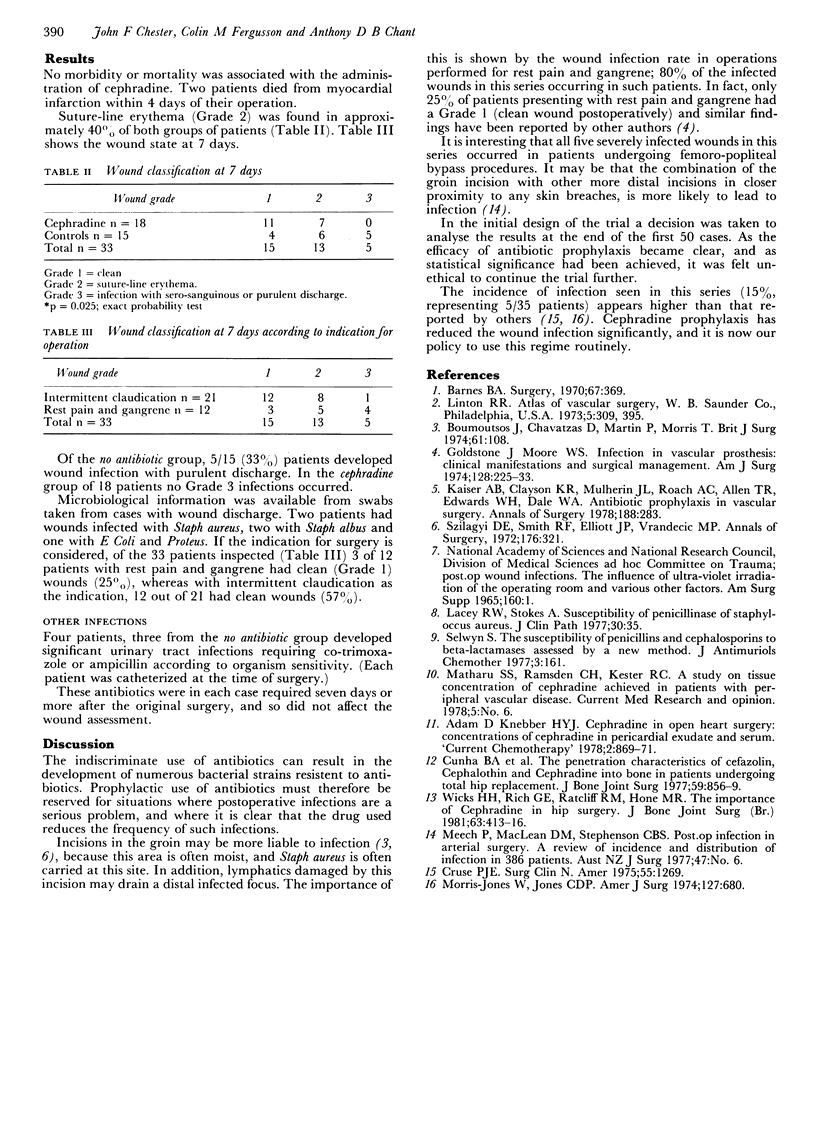
Cephradine administered prophylactically to a group of 35 patients undergoing reversed saphenous vein femoro-popliteal bypass, iliofemoral endarterectomy or profundaplasty through a groin incision, resulted in a significant reduction in the incidence of wound infection (P = 0.025; exact probability test). One gram of cephradine was given at induction of anaesthesia, followed by three postoperative doses of one gram at 6 hourly intervals. The overall wound infection rate at 7 days, as assessed by frank purulent discharge, was 15%. After cephradine prophylaxis, no infections were noted as judged on this basis, but erythema of the suture line was seen in equal numbers (40% of each group). Where the indication for operative intervention was rest pain or gangrene, the incidence of wound infection was very much increased, 80% of the infected cases being from this group.
Full text
PDF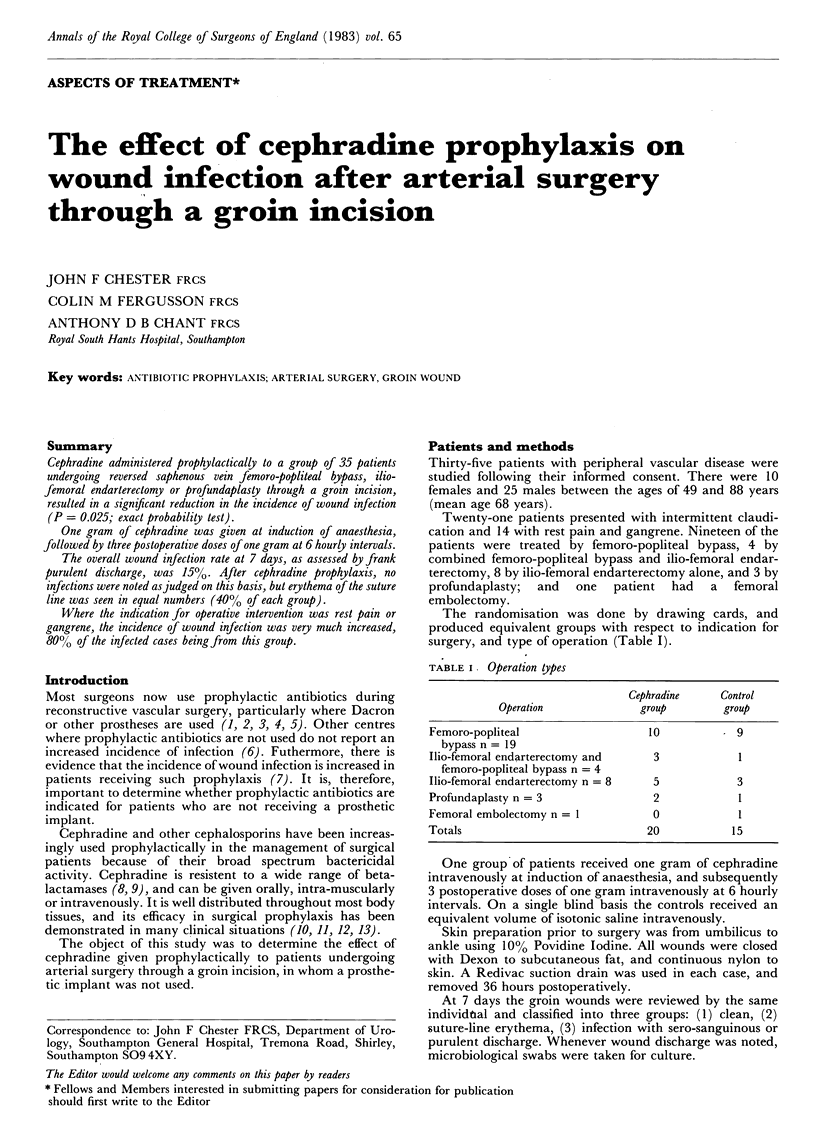
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barnes B. A. Prophylactic use of antibiotics. Surgery. 1970 Feb;67(2):369–370. [PubMed] [Google Scholar]
- Bouhoutsos J., Chavatzas D., Martin P., Morris T. Infected synthetic arterial grafts. Br J Surg. 1974 Feb;61(2):108–111. doi: 10.1002/bjs.1800610208. [DOI] [PubMed] [Google Scholar]
- Cruse P. J. Incidence of wound infection on the surgical services. Surg Clin North Am. 1975 Dec;55(6):1269–1275. doi: 10.1016/s0039-6109(16)40780-2. [DOI] [PubMed] [Google Scholar]
- Cunha B. A., Gossling H. R., Pasternak H. S., Nightingale C. H., Quintiliani R. The penetration characteristics of cefazolin, cephalothin, and cephradine into bone in patients undergoing total hip replacement. J Bone Joint Surg Am. 1977 Oct;59(7):856–859. [PubMed] [Google Scholar]
- Goldstone J., Moore W. S. Infection in vascular prostheses. Clinical manifestations and surgical management. Am J Surg. 1974 Aug;128(2):225–233. doi: 10.1016/0002-9610(74)90097-x. [DOI] [PubMed] [Google Scholar]
- Kaiser A. B., Clayson K. R., Mulherin J. L., Jr, Roach A. C., Allen T. R., Edwards W. H., Dale W. A. Antibiotic prophylaxis in vascular surgery. Ann Surg. 1978 Sep;188(3):283–289. doi: 10.1097/00000658-197809000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacey R. W., Stokes A. Susceptibility of the "penicillinase-resistant" penicillins and cephalosporins to penicillinase of Staphylococcus aureus. J Clin Pathol. 1977 Jan;30(1):35–39. doi: 10.1136/jcp.30.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris-Jones W., Jones C. D. Profundoplasty in the treatment of femoropopliteal occlusion. Am J Surg. 1974 Jun;127(6):680–686. doi: 10.1016/0002-9610(74)90346-8. [DOI] [PubMed] [Google Scholar]
- Selwyn S. Susceptibility of penicillins and cephalosporins to beta-lactamases assessed by a new test. J Antimicrob Chemother. 1977 Mar;3(2):161–168. doi: 10.1093/jac/3.2.161. [DOI] [PubMed] [Google Scholar]
- Szilagyi D. E., Smith R. F., Elliott J. P., Vrandecic M. P. Infection in arterial reconstruction with synthetic grafts. Ann Surg. 1972 Sep;176(3):321–333. doi: 10.1097/00000658-197209000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wicks M. H., Rich G. E., Ratcliff R. M., Hone M. R. The importance of cephradine in hip surgery. J Bone Joint Surg Br. 1981;63-B(3):413–416. doi: 10.1302/0301-620X.63B3.7263757. [DOI] [PubMed] [Google Scholar]


