Abstract
OBJECTIVE—Postprandial glycemic excursions may contribute to the development of diabetes-related complications. Meals of high and low glycemic index (GI) have distinct effects on postprandial glycemia (PPG). Insulin pump therapy offers the potential to tailor insulin delivery to meal composition; however, optimal bolus types for meals of different glycemic loads have not been defined. We sought to compare the impact of GI combined with varying prandial bolus types on PPG.
RESEARCH DESIGN AND METHODS—An open crossover study examining the effects of four different meal and bolus-type combinations on 3-h PPG (measured by continuous glucose-monitoring system [CGMS]) was conducted. A total of 20 young people aged 8–18 years with type 1 diabetes using insulin-pump therapy participated. Meals had equal macronutrient, energy, and fiber content and differed only in GI (low vs. high). Participants consumed meals of the same GI on consecutive days and were randomized to receive either a standard (100%) or a dual-wave (DW) (50:50% over 2 h) bolus each day. CGMS data from 10 healthy control participants established the target response to each meal.
RESULTS—A DW bolus before low-GI meals decreased PPG area under the curve (AUC) by up to 47% (P = 0.004) and lowered the risk of hypoglycemia for the same premeal glucose (P = 0.005) compared with standard bolus. High-GI meals resulted in significant upward PPG excursions with greater AUC (P = 0.45), regardless of bolus type.
CONCLUSIONS—These data support the use of a DW bolus with low GI meals to optimize PPG in patients with type 1 diabetes using insulin pump therapy.
Attention to postprandial glycemia (PPG) is emerging as a key therapeutic strategy in the prevention of adverse outcomes for patients with diabetes. Epidemiological evidence from nondiabetic adults has shown that blood glucose level 2 h after a glucose challenge is predictive of both development of cardiovascular disease and mortality (1,2). In subjects with type 2 diabetes, there is evidence that PPG is an independent risk factor for myocardial infarction (3), possibly by inducing endothelial dysfunction and oxidative stress generation. Postchallenge hyperglycemic spikes are also more strongly associated with carotid intima-media thickness than fasting plasma glucose or A1C (4). Such an association has yet to be defined for type 1 diabetes; however, because hyperglycemia can acutely alter normal homeostasis, it is reasonable to hypothesize that this effect will be accentuated in any individual with diabetes.
The Diabetes Control and Complications Trial clearly established a continuous relationship between glycemic exposure and the risk of microvascular complications (5). The investigators have, however, argued that A1C alone is insufficient to explain the onset of complications and have suggested that PPG may be implicated (6). Since PPG is a major determinant of A1C, efforts that specifically improve PPG have the ability to improve A1C (7). How best to integrate such measures into current management strategies is not well defined.
Insulin pump therapy is unique in its ability to tailor prandial insulin delivery to the composition of a meal and its anticipated glycemic effects. Current pump technology allows variation in the speed and duration of prandial insulin delivery; calculation of the premeal bolus should therefore be based both on the dose of insulin required and on bolus type. Despite access to these advanced features, there is a paucity of evidence to guide clinicians and patients in their use. Previous studies have shown reduction in late PPG with use of a dual-wave (DW) bolus for high-carbohydrate (CHO), high-fat meals (8,9) and high-fat meals alone (10). The PPG impact of altering premeal bolus type for meals of recommended nutritional composition (11) has not yet been examined.
The glycemic index (GI) ranks foods based on acute glycemic impact over a 2-h period of 50 g of available CHO of a test food compared with the reference standard glucose (12). GI is consistent between age-groups (13). The glycemic load (GL) considers both the GI and the CHO amount consumed (GL = [GI × g of CHO]/100) (14). Use of GL to predict glycemic response and insulin demand has been validated in healthy adults (15); whether it can be employed as a predictor of exogenous insulin requirements for different meals in individuals with type 1 diabetes has not previously been examined.
Our hypothesis was that consideration of the GI of a meal when determining the premeal bolus type would optimize PPG in patients with type 1 diabetes using insulin pump therapy.
RESEARCH DESIGN AND METHODS
We conducted an open crossover study examining the effects of four different meal- and bolus-type combinations on PPG in children and adolescents with type 1 diabetes using insulin pump therapy. The study received institutional ethics committee approval. Inclusion criteria were comprised of the following: age 8–18 years; type 1 diabetes duration >1 year; use of insulin pump therapy, including proficiency with use of a bolus dose calculator, for >3 months; A1C ≤ 8.5% (PDQ Primus); and reliably performing self-monitoring of blood glucose at least four times daily. Individuals with eating disorders, concomitant dietary restrictions (e.g., celiac disease or food allergy), and diabetes-related complications and those using another medication that lowers blood glucose were excluded. Data from healthy young adult control participants were used to establish the normal PPG profiles following each meal type.
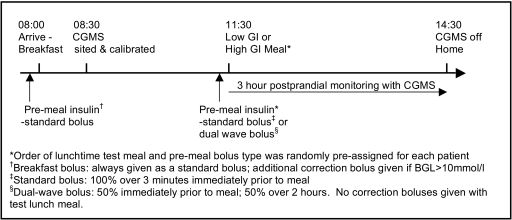
During the 2 weeks before participation, self-monitoring of blood glucose was performed eight times daily (fasting, premeals, 2 h after meals, and overnight) to allow optimization of basal rates, insulin-to-CHO ratios (ICRs), and insulin-sensitivity factors. The study was then carried out under supervision in a dedicated research unit. A schematic timeline is shown in Fig. 1. Participants arrived fasting at 8:00 a.m. and ate a standardized breakfast; this served to negate any confounding second-meal effect at the time of the subsequent test meal. The test meal was eaten at lunchtime, 3.5 h after breakfast. Nutritional composition of all study meals is outlined in Table 1. Test lunchtime meals had equivalent macronutrient (CHO, protein, and fat), fiber, and energy composition and differed only in their GI and, hence, GL.
Figure 1.
Schematic timeline of each study day.
Table 1.
Nutritional composition of meals consumed in the study
| Standardized breakfast | Low-GI test meal | High-GI test meal | |
|---|---|---|---|
| Composition | 33 g wholewheat cereal, 250 ml lowfat milk, 1 slice 9 grain toast, 5 g margarine,10 g jam, 2 halves tinned pears | 150 g boiled spaghetti, 120 g bolognaise sauce,140 g red apple, 300 ml water to drink | 280 g peeled boiled potato, 120 g bolognaise sauce, 300 g watermelon, 300 ml water to drink |
| Energy (kCal) | 412 | 429 | 430 |
| Protein (g) | 17.0 | 26.1 | 27.7 |
| Fat (g) | 8.0 | 8.3 | 8.6 |
| CHO (g) | 64.0 | 60.1 | 57.1 |
| Fibre (g) | 6.7 | 5.9 | 7.6 |
| GI | 49 | 34 | 76 |
| GL | 31 | 20.4 | 43.4 |
PPG was examined following four different meal- and bolus-type combinations. Participants consumed the same test meal type (either low or high GI) on two consecutive days, using a different premeal bolus type on each day; this process was then repeated over a further 2-day period with the other test meal type. Bolus types used were either a standard bolus delivering 100% of the dose over 3 min immediately before the meal or a DW bolus with 50% delivered over 3 min immediately before the meal and 50% delivered over the subsequent 2 h. The order of each test meal–and bolus-type combination was randomly assigned in advance for each participant. Each participant used their own ICR, as verified during the run-in period, to determine the total dose of insulin to be administered. Before breakfast, if blood glucose level was >10 mmol/l, an additional correction bolus was administered; prebreakfast insulin was given as a standard bolus over 3 min throughout the study. Correction bolus doses were not administered at the test lunchtime meal, during which total insulin dose was constant in a given individual over the study period for each meal type.
Continuous glucose-monitoring using the CGMS Gold (Medtronic MiniMed, Northridge, CA) system was used to monitor changes in PPG for 3 h after each test meal–bolus combination. A new subcutaneous sensor was inserted for each 2-day study block. Controlled conditions were employed throughout the study: insulin aspart was used by all participants, subcutaneous infusion sites were changed on the evening before each 2-day study block, catheter site (e.g., hip or stomach) remained constant in a given individual over the entire study period, and activity was limited to sedentary activities in a research unit. All meals were consumed in their entirety within 20 min; no additional food or drink was consumed in the 3-h postprandial period unless required to treat symptomatic hypoglycemia.
Statistical analysis
The primary outcome of interest was area under the curve (AUC) following each of the meal- and bolus-type combinations in participants with diabetes. AUC was defined as the sum of the absolute value of excursions from sensor value at the start of the meal and was calculated for the 3-h period following each meal and bolus combination. Data following treated hypoglycemic episodes did not form part of the analysis. To account for this, AUC was calculated using three separate methods: 1) excluding participants with treated hypoglycemic episodes, 2) extrapolating average values up to time of treatment, and 3) carrying forward the last sensor value before treatment; separate analyses were performed to ensure results were consistent. Linear regression was used to investigate the relationship between AUC and bolus type and meal GI, adjusting for sensor value at the start of the meal. Differences in PPG profiles with each of the two bolus types for each of the meals were investigated using logistic regression and the χ2 test. Analysis was performed using Stata 10 (2007; StataCorp LP, TX).
RESULTS
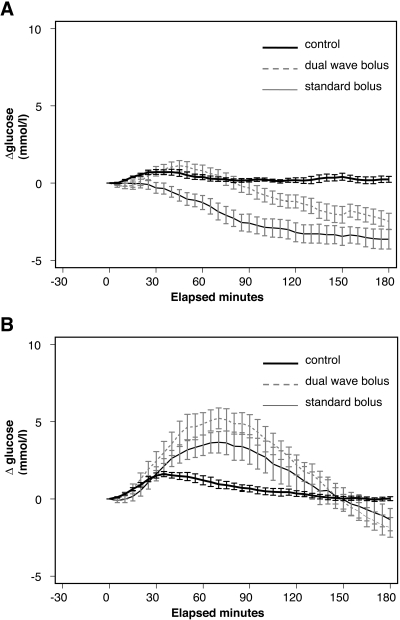
A total of 20 children and adolescents (10 male) with type 1 diabetes participated in the study. Baseline characteristics expressed as mean (range) were as follows: age 11.8 years (9.3–17.3), duration of diabetes 4.9 years (2.1–8.9), duration of insulin pump therapy 0.8 years (0.4–1.8), and A1C 7.5% (5.9–8.5). A total of 10 healthy, nondiabetic young-adult control participants (four male) also consumed the study meals on two consecutive days under comparable conditions. Profiles of mean ± SE postprandial excursion from premeal sensor glucose are shown for control participants following each meal type and for participants with diabetes following each meal type and bolus combination in Fig. 2.
Figure 2.
A: Low GI meal. B: High GI meal. PPG profiles: mean ± SE from premeal glucose.
Analysis comparing AUC of 3-h PPG following the low-GI meal showed a significant beneficial effect of use of a DW bolus. This effect of lowering AUC was significant using all methods of AUC analysis. Excluding data from those with treated postprandial hypoglycemia, use of a DW rather than a standard bolus resulted in a 47% decrease in AUC (P = 0.004) (Fig. 2A). Similarly, AUC reductions of 31% (P < 0.05) and 36% (P = 0.03) were found using methods 2 and 3 as described above, respectively. The significant differences in PPG profiles between bolus types for the low-GI meal emerged at 25 min and persisted thereafter.
In contrast, premeal bolus type had no effect on postprandial AUC following the high-GI meal (P = 0.45). As shown in Fig. 2B, substantial upward glycemic excursion was evident following this meal, regardless of bolus type; mean peak PPG excursion in participants with diabetes was 5.3 mmol/l, compared with 1.8 mmol/l in control participants. Mean time taken to reach peak glucose excursion was also significantly longer for participants with diabetes relative to control participants: 76 vs. 38 min, respectively (P < 0.01), with no difference between bolus types (P = 0.75).
Regression analysis was used to establish whether sensor glucose value immediately before the test meal had an effect on the subsequent PPG profile. No significant effect of premeal glucose on postprandial AUC was evident for either test meal type (P = 0.07 and P = 0.8 for the low-GI and high-GI meals, respectively).
In total, 13 symptomatic hypoglycemic episodes required treatment during the 3-h postprandial period. Hypoglycemia occurred in participants of all ages. Eleven episodes occurred after low-GI meals (standard bolus 7, DW bolus 4); two episodes followed the high-GI meal with standard bolus. The higher number of episodes following low-GI meals did not reach statistical significance (P = 0.07). There was, however, a significant effect of premeal glucose level for the low-GI meal–standard bolus combination, where the odds ratio of symptomatic hypoglycemia increased by 0.6 for every 1 mmol/l decrease in premeal glucose (P = 0.005).
CONCLUSIONS
This study has shown for the first time that consideration of both the GI of a meal and the type of premeal insulin bolus has important modifiable effects on PPG. With use of a DW bolus, 3-h postprandial AUC was up to 47% lower compared with a standard bolus for a low-GI meal. Mean PPG profiles obtained following a low-GI meal with a DW bolus closely mirrored physiological target profiles of control participants for the first 90 postprandial minutes. In contrast, high-GI meals were followed by significant and prolonged upward PPG excursions in participants with diabetes, irrespective of premeal bolus type.
PPG is a relatively new concept in diabetes management and many questions with regard to its assessment remain (16). In practical terms, measurement of fasting/premeal plasma glucose and A1C still dominates the assessment of glycemia. Established treatment goals of fasting/premeal normoglycemia and A1C as near to normal as possible have, however, been challenged by studies showing that even in patients achieving these goals, postprandial hyperglycemia is common (17). Thus, in light of the recent evidence linking PPG to adverse outcomes (1–4), patients with well-controlled diabetes may remain at increased risk of developing diabetes-associated complications.
Current American Diabetes Association nutrition recommendations advocate matching insulin to the CHO content of a meal (11). Traditional prandial insulin dosing, as determined by the amount of CHO in grams or weighed “exchanges,” does not account for the very different effects that different types of CHO have on PPG. Although not universally adopted in routine practice, low-GI diets have been shown in some studies to have clinically useful effects on lowering A1C in type 1 diabetes (18–20) and are acknowledged to produce modest benefits in addition to those observed when total CHO is used alone (11,21). Our center has previously reported benefits of incorporating use of the GI into routine diabetes management (18), and this continues to be recommended for our patient group.
By definition, low-GI foods result in a lower, more gradual rise in PPG; this prompted our hypothesis that a DW bolus may better suit low-GI meals. Since GI is defined relative to its PPG impact at 2 h, we chose to deliver the extended portion of the DW bolus over 2 h. In the absence of an evidence base, a 50:50 split was empirically chosen for both meals to allow for direct comparison. PPG monitoring for 3 h after the meal allowed for a lag time related to exogenous insulin delivery.
Bolus-wizard settings of all participants were verified with 8-point testing over a 2-week run-in period before this study; thereafter, ICR was consistent in a given individual throughout the study period. Despite this, meals of equivalent CHO amount (grams) resulted in markedly different PPG responses (Fig. 2). The striking difference in PPG profiles underscores the inherent difficulty with calculating meal boluses solely based on CHO quantity. Consideration of the nature of the CHO and its anticipated PPG effects (GI) can therefore help to optimize PPG and inform decisions regarding the mode of meal bolus delivery.
Symptomatic hypoglycemic episodes occurred more frequently after low-GI meals but did not reach statistical significance. Of note, however, is that those with a lower premeal glucose were significantly more likely to experience hypoglycemia using a standard bolus rather than a DW bolus for this meal type. This implies that patients attaining their target premeal glucose may gain additional benefit from reduction in PPG with use of a DW bolus for low-GI meals. Despite variable age-specific energy requirements and the consistent energy intake of the study meals, hypoglycemia occurred across all age-groups.
A finding of concern in this study was the significant upward deviation in PPG following high-GI meals in participants with diabetes, in whom the glycemic response was almost threefold greater than that of nondiabetic control participants. Thus, even with use of a rapid-acting insulin analog, participants with diabetes were unable to curtail significant hyperglycemic PPG excursions following high-GI meals with boluses initiated immediately before meals. This suggests that in order to optimize PPG, prandial insulin may need to be initiated in advance of a high-GI meal; further studies as to the timing of bolus administration with different meal types are now warranted.
This study highlights a number of important practical issues for those who care for patients with type 1 diabetes using insulin-pump therapy. The important impact of the GI of any given meal is evident in the PPG profiles following each of the two meal types. In addition, clinically significant benefits, including attainment of physiological PPG profiles for the first 90 postprandial minutes, are now apparent with use of a DW bolus for a low-GI meal. Our data reinforce the beneficial PPG impact of choosing low-GI rather than high-GI foods with relevance to commonly eaten mixed meals. Of note, the GI concept also applies to mixed meals of varying macronutrient composition (22). This should guide advice to patients regarding meal choices, informed use of insulin pump bolus technology, and the potential impact on PPG.
We acknowledge that implementation of these findings represents advanced insulin pump management, which may best be incorporated when basic insulin pumping is established. However, incorporation of GI into routine diabetes care has previously been shown to be easily adopted and accepted in pediatric patients (18). Current nutrition recommendations acknowledge that evidence from well-conducted cohort studies also supports this practice (11,21). In practical terms, nutritional advice may include basic education with regard to the GI of commonly encountered foods. When a meal contains only low-GI foods, a DW bolus should then be administered.
The long-term consequences of postprandial hyperglycemia for patients with type 1 diabetes are unclear, but given the weight of available evidence to date, it appears prudent to continue efforts to optimize advanced insulin pump techniques to achieve physiologic PPG profiles.
Acknowledgments
This study was supported by funding from the Australian Novo Nordisk Regional Diabetes Support Scheme.
Published ahead of print at http://care.diabetesjournals.org on 28 May 2008.
Clinical trial reg. no. ACTRN012605000762651.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C Section 1734 solely to indicate this fact.
References
- 1.Lowe LP, Liu K, Greenland P, Metzger BE, Dyer AR, Stamler J: Diabetes, asymptomatic hyperglycemia, and 22-year mortality in black and white men: the Chicago Heart Association Detection Project in Industry Study. Diabetes Care 20:163–169, 1997 [DOI] [PubMed] [Google Scholar]
- 2.The DECODE study group, the European Diabetes Epidemiology Group: Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria. The Lancet 354:617–621, 1999 [PubMed] [Google Scholar]
- 3.Hanefeld M, Fischer S, Julius U, Schulze J, Schwanebeck U, Schmechel H, Ziegelasch HJ, Lindner J: Risk factors for myocardial infarction and death in newly detected NIDDM: the Diabetes Intervention Study, 11-year follow-up. Diabetologia 39:1577–1583, 1996 [DOI] [PubMed] [Google Scholar]
- 4.Temelkova-Kurktschiev TS, Koehler C, Henkel E, Leonhardt W, Fuecker K, Hanefeld M: Postchallenge plasma glucose and glycemic spikes are more strongly associated with atherosclerosis than fasting glucose or HbA1c level. Diabetes Care 23:1830–1834, 2000 [DOI] [PubMed] [Google Scholar]
- 5.The Diabetes Control and Complications Trial Research Group: The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329:977–986, 1993 [DOI] [PubMed] [Google Scholar]
- 6.The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes 44:968–983, 1995 [PubMed] [Google Scholar]
- 7.Heptulla RA, Allen HF, Gross TM, Reiter EO: Continuous glucose monitoring in children with type 1 diabetes: before and after insulin pump therapy. Pediatric Diabetes 5:10–15, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Chase HP, Saib SZ, MacKenzie T, Hansen MM, Garg SK: Post-prandial glucose excursions following four methods of bolus insulin administration in subjects with Type 1 diabetes. Diabet Med 19:317–321, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Jones SM, Quarry JL, Caldwell-McMillan M, Mauger DT, Gabbay RA: Optimal insulin pump dosing and postprandial glycemia following a pizza meal using the continuous glucose monitoring system. Diabetes Technol Ther 7:233–240, 2005 [DOI] [PubMed] [Google Scholar]
- 10.Lee SW, Cao M, Sajid S, Hayes M, Choi L, Rother C, de Leon R: The dual-wave bolus feature in continuous subcutaneous insulin infusion pumps controls prolonged post-prandial hyperglycaemia better than standard bolus in Type 1 diabetes. Diabetes Nutr Metab 17:211–216, 2004 [PubMed] [Google Scholar]
- 11.American Diabetes Association: Nutrition recommendations and interventions for diabetes: A position statement of the American Diabetes Association. Diabetes Care 30:S48–S65, 2007 [DOI] [PubMed] [Google Scholar]
- 12.Jenkins DJ, Wolever TM, Taylor RH, Barker H, Fielden H, Baldwin JM, Bowling AC, Newman HC, Jenkins AL, Goff DV: Glycemic index of foods: a physiological basis for carbohydrate exchange. Am J Clin Nutr 34:362–366, 1981 [DOI] [PubMed] [Google Scholar]
- 13.Wolever TM, Jenkins DJ, Collier GR, Ehrlich RM, Josse RG, Wong GS, Lee R: The glycaemic index: effect of age in insulin dependent diabetes mellitus. Diabetes Res 7:71–74, 1988 [PubMed] [Google Scholar]
- 14.Salmeron J, Manson JE, Stampfer MJ, Colditz GA, Wing AL, Willett WC: Dietary fiber, glycemic load, and risk of non-insulin-dependent diabetes mellitus in women. Jama 277:472–477, 1997 [DOI] [PubMed] [Google Scholar]
- 15.Brand-Miller JC, Thomas M, Swan V, Ahmad ZI, Petocz P, Colagiuri S: Physiological validation of the concept of glycemic load in lean young adults. J Nutr 133:2728–2732, 2003 [DOI] [PubMed] [Google Scholar]
- 16.American Diabetes Association: Postprandial blood glucose. Diabetes Care 24:775–778, 2001 [DOI] [PubMed] [Google Scholar]
- 17.Boland E, Monsod T, Delucia M, Brandt CA, Fernando S, Tamborlane WV: Limitations of conventional methods of self-monitoring of blood glucose: lessons learned from 3 days of continuous glucose sensing in pediatric patients with type 1 diabetes. Diabetes Care 24:1858–1862, 2001 [DOI] [PubMed] [Google Scholar]
- 18.Gilbertson HR, Brand-Miller JC, Thorburn AW, Evans S, Chondros P, Werther GA: The effect of flexible low glycemic index dietary advice versus measured carbohydrate exchange diets on glycemic control in children with type 1 diabetes. Diabetes Care 24:1137–1143, 2001 [DOI] [PubMed] [Google Scholar]
- 19.Buyken AE, Toeller M, Heitkamp G, Karamanos B, Rottiers R, Muggeo M, Fuller JH: Glycemic index in the diet of European outpatients with type 1 diabetes: relations to glycated hemoglobin and serum lipids. Am J Clin Nutr 73:574–581, 2001 [DOI] [PubMed] [Google Scholar]
- 20.Brand-Miller J, Hayne S, Petocz P, Colagiuri S: Low-glycemic index diets in the management of diabetes: A meta-analysis of randomized controlled trials. Diabetes Care 26:2261–2267, 2003 [DOI] [PubMed] [Google Scholar]
- 21.Sheard NF, Clark NG, Brand-Miller JC, Franz MJ, Pi-Sunyer FX, Mayer-Davis E, Kulkarni K, Geil P: Dietary carbohydrate (amount and type) in the prevention and management of diabetes: A statement by the American Diabetes Association. Diabetes Care 27:2266–2271, 2004 [DOI] [PubMed] [Google Scholar]
- 22.Wolever TMS, Bolognesi C: Prediction of glucose and insulin responses of normal subjects after consuming mixed meals varying in energy, potein, fat, carbohydrate and glycemic index. J Nutr 126:2807–2812, 1996 [DOI] [PubMed] [Google Scholar]