Abstract
OBJECTIVE—The purpose of this study was to determine whether elective use of a health plan–sponsored health club membership had an impact on health care use and costs among older adults with diabetes.
RESEARCH DESIGN AND METHODS—Administrative claims for 2,031 older adults with diabetes enrolled in a Medicare Advantage plan were obtained for this retrospective cohort study. Participants (n = 618) in the plan-sponsored health club benefit (Silver Sneakers [SS]) and control subjects (n = 1,413) matched on SS enrollment index date were enrolled in the plan for at least 1 year before the index date. Two-year health care use and costs of SS participants and control subjects were estimated in regressions adjusting for baseline differences.
RESULTS—SS participants were more likely to be male, had a lower chronic disease burden, used more preventive services, and had a lower prevalence of arthritis (P ≤ 05). SS participants had lower adjusted total health care costs than control subjects in the first year after enrollment (−$1,633 [95% CI −$2,620 to −$646], P = 0.001), and adjusted total costs in year 2 trended lower (−$1,230 [−$2,494 to $33], P = 0.06). Participants who made on average ≥2 SS visits/week in year 1 had lower total costs in year 2 ($2,141 [−$3,877 to −$405], P = 0.02) than participants who made <2 visits/week.
CONCLUSIONS—Use of a health club benefit by older adults with diabetes was associated with slower growth in total health care costs over 2 years; greater use of the benefit was actually associated with declines in total costs.
Health care costs associated with diabetes account for 32% of total Medicare spending (1). Clinical practice guidelines recommend physical activity as an important component of diabetes management (2) and for prevention of cardiovascular complications (3), but only 16% of individuals aged 65–74 years engage in at least 30 min of moderate activity ≥5 days/week (4). The benefits of physical activity for older adults include better health, improved functioning, increased quality of life, lower health care costs, and longer survival (5–8). There is growing recognition that environmental conditions and policies that promote physical activity can have an impact on modifiable behavioral risks and chronic conditions (9,10).
Health plan promotion and direct support of physical activity via sponsored exercise programs have the potential to reach many people because 61% of younger Americans had employment-based health insurance in 2004 (11) and nearly 100% of older Americans have Medicare coverage. Two previous studies of a health plan–sponsored community-based group exercise program (EnhanceFitness) for Medicare Advantage plan enrollees showed that participants in a general population (12) and in a subgroup of members with diabetes (13) who made greater use of the exercise program had lower adjusted health care costs than less active participants and control subjects. A third study examined the cost impact of a health club membership (Silver Sneakers [SS]) sponsored by the same Medicare Advantage plan with older adult members and found that SS use was associated with slower growth in total health care costs, particularly for the most active SS participants (14).
This study extends prior studies by examining whether the health care use and cost impacts of SS participation found in older adults also apply to the subset of older adults with diabetes who have the most to gain from regular physical activity. We compared dose effects of SS participation on health care use and costs, based on a dose threshold of <2 or ≥2 visits/week. This study may provide further evidence of whether health plan–sponsored health club memberships provide a return on investment for older adults with chronic conditions and the level of participation needed to reduce health care costs.
RESEARCH DESIGN AND METHODS
This study was based at Group Health Cooperative (GHC), a consumer-governed, staff model HMO with >500,000 members. We received administrative claims data for a total of 8,473 members aged ≥65 years who enrolled in the GHC Medicare Advantage plan, were continuously enrolled at GHC for at least 1 year before the date of joining the program, and participated in SS between 1 January 1998 and 30 December 2003. We age- and sex-matched up to three GHC Medicare Advantage enrollees (n = 24,331) who never used the program to serve as control subjects for each SS participant. Participants and their matched control subjects were each assigned an index date representing the month that the participant first enrolled in SS. We excluded members who had <2 years of continuous enrollment after their index date, had missing cost data in any of the 3 years, had long-term care costs at baseline, and were unmatched SS participants or control subjects, leaving 4,766 SS participants and 9,035 matched control subjects (14).
From this larger data set, only members who were on GHC's diabetes registry were included (SS participants, n = 618; control subjects, n = 1,413). Members were added to the GHC diabetes registry on the basis of one of the following criteria: 1) currently taking any diabetes medication, 2) a fasting glucose ≥126 mg/dl confirmed by a second out-of-range test within 1 year, 3) a random plasma glucose ≥200 mg/dl also confirmed by a second out-of-range test within 1 year, or 4) a hospital discharge diagnosis of diabetes at any time during GHC enrollment or two outpatient diagnoses (ICD-9) of diabetes (15).
SS Program
The SS program provided the GHC Medicare Advantage enrollees access to selected local fitness centers in an unstructured format. Participants had access to conditioning classes designed for older adults, exercise equipment, pools, saunas, and other amenities that varied across facilities. A subcontractor administered the program and interfaced with the fitness centers. The GHC Medicare Advantage enrollees learned about the SS program from targeted mailings, a member benefits Web site, or their health providers during routine preventive visits. Members who elected to participate in SS contacted their local fitness center to enroll in the program.
Data sources
Inpatient hospitalization, primary care visits, specialty care visits, and four health care costs (total, inpatient, primary care, and specialty costs) for SS participants and matched control subjects were obtained from GHC administrative data, which have been used extensively in prior research (16,17). In brief, GHC costs are derived from the Decision Support System, which integrates clinical information, units of service, and actual costs from the general ledger to identify all costs as direct patient care costs or overhead costs that are shared by more than one department (14).
Primary care costs included all direct and indirect costs associated with visits or telephone calls by primary care or preventive medicine personnel that are related to direct patient care, preventive services, or risk factor reduction counseling. Specialty care visits and costs included obstetrics and gynecology services, cardiac diagnostics, diagnostic pathology, alternative medicine, and rehabilitative services. Total health care costs included additional categories such as inpatient hospital, emergency, pharmacy, and long-term care costs.
Covariates that might influence the economic outcomes and were available in GHC administrative data were measured. These covariates included age, sex, baseline use or cost (as appropriate), a previously validated, pharmacy-based measure of chronic disease burden (RxRisk) (18,19), comorbidities derived from ICD-9-CM codes from outpatient problem lists, and a preventive services index. Members who use other preventive services (colon cancer screening, a screening mammogram, prostate cancer screening, an influenza vaccine, or a pneumococcal vaccine) may be more likely to participate in SS, so we adjusted for prior preventive service use to account for self-selection of health-oriented individuals into SS participation (13,14). Average mean attendance (visits to the health club in year 1) was calculated by adding all visits across the year and dividing by 52 weeks.
Statistical analysis
Baseline comparisons between SS participants and control groups were conducted using two-tailed t tests and χ2 tests. Ordinary least-squares (OLS) regressions were estimated to examine differences in health care use and costs between SS participants and control subjects in the first and second years after the index date while adjusting for age, sex, RxRisk, preventive services index, arthritis visits, and respective baseline use or costs. Because the results were similar to those obtained using generalized linear models with a gamma distribution and log-link function (20), we present OLS results. Previous work suggests that OLS results with large data sets (≥500 observations) will yield unbiased estimates of absolute differences in use and cost data even when assumptions about normality and homoscedasticity are not met (21).
Exploratory subgroup analyses were also performed to determine differences in total health care costs from baseline to year 2 in SS participants who attended <2 or ≥2 SS visits/week in year 1. The threshold of at least 2 visits/week was chosen because this participation rate resulted in significant reductions in total health care costs in a large sample of older adult members (14). This analysis also adjusted for differences in age, sex, RxRisk, new diagnosis of congestive heart failure or depression during year 1, and baseline total health care costs.
To improve balance of observed covariates, we used propensity score adjustments in a sensitivity analysis (22,23). We estimated a logit model to generate each patient's propensity of joining SS and entered propensity score as an additional covariate in our models. The inclusion of propensity score provided estimates similar to those in the multivariate models except that group differences in total health care costs at year 2 reached statistical significance with the propensity score model (P = 0.06 vs. P = 0.03). We therefore present results from the simpler multivariate models. Statistical tests were not adjusted for multiple comparisons because we were interested in total health care cost differences between SS participants and control subjects, and the subgroup analyses were hypothesis generating.
All cost data were adjusted to 2003 dollars. Robust SEMs that did not require the distributional assumptions to be exact were used in all regressions. All statistical procedures were performed with STATA (version 9.0; Stata, College Station, TX). Institutional review boards at GHC and the University of Washington approved the study protocol.
RESULTS
Unadjusted comparisons between SS participants and control subjects
SS participants were more likely to be male, had a slightly lower chronic disease burden, used more preventive services, had more outpatient visits for arthritis, and made more primary care and specialty care visits (all P < 0.05) than control subjects. There were no significant differences in age, level of diabetes control, or total health care costs at baseline between the two groups (Tables 1 and 2). SS participants on average made a total of 72 ± 79 and 49 ± 78 visits to SS health clubs in years 1 and 2, respectively.
Table 1.
Baseline sample characteristics
| Control subjects | SS participants | P value* | |
|---|---|---|---|
| n | 1,413 | 618 | |
| Demographics | |||
| Age (years) | 72 ± 5 | 72 ± 5 | 0.47 |
| Sex (% female) | 835 (59) | 312 (50) | <0.001 |
| Comorbidities† | |||
| RxRisk ($) | 3,498 ± 2,356 | 3,300 ± 1,990 | 0.05 |
| Arthritis | 212 (15) | 128 (21) | 0.002 |
| Coronary artery disease | 294 (21) | 140 (23) | 0.35 |
| Heart registry | 473 (33) | 230 (37) | 0.10 |
| Congestive heart failure | 134 (9) | 47 (9) | 0.17 |
| Hypertension | 503 (36) | 241 (39) | 0.14 |
| Depression | 118 (8) | 52 (8) | 0.96 |
| A1C (%)‡ | 7.48 ± 1.4 | 7.38 ± 1.28 | 0.12 |
| Serum HDL‡ | 49 ± 13 | 49 ± 13 | 0.94 |
| Total cholesterol‡ | 207 ± 46 | 202 ± 44 | 0.04 |
| Preventive services index§ | 1.4 ± 1.6 | 1.8 ± 1.7 | <0.001 |
Data are means ± SD or n (%) unless indicated otherwise. n = 2,031.
Unadjusted comparisons using t test for unequal variance (continuous variables) or χ2 test (dichotomous variables).
RxRisk is expressed as predicted 6-month costs. Higher costs represent higher comorbidity; comorbid conditions (arthritis, coronary artery disease, congestive heart failure, hypertension, diabetes, and depression) were derived from problem lists for outpatient visits.
A1C (control subjects, n = 1,325; SS participants, n = 588); serum HDL and total cholesterol (n = 907 and n = 440, respectively).
Preventive services index is the total number of preventive services that an individual used in the 2 years preceding the index date (colon cancer screening [fecal occult blood test or flexible sigmoidoscopy], a screening mammogram, prostate cancer screening, an influenza vaccine, or a pneumococcal vaccine [range 0–8]).
Table 2.
Use and costs with SS participation 1 and 2 years after index start date
| Use measures | Control subjects | SS participants | Adjusted mean difference (Δ SS participants − Δ control subjects)* | P value |
|---|---|---|---|---|
| n | 1,413 | 618 | ||
| % hospitalized | ||||
| Baseline | 174 (12.3) | 71 (11.5) | — | |
| Year 1 | 211 (14.9) | 74 (11.9) | −3.0 (−6 to 0.2) | 0.07 |
| Year 2† | 229 (16.2) | 70 (11.3) | −4.7 (−7.8 to −1.6) | 0.003 |
| Primary care visits/year | ||||
| Baseline‡ | 6.2 ± 5.2 | 6.9 ± 4.8 | — | |
| Year 1† | 6.2 ± 5.0 | 7.3 ± 5.2 | 0.77 (0.34 to 1.2) | <0.001 |
| Year 2† | 6.4 ± 5.4 | 7.0 ± 5.3 | 0.30 (−0.14 to 0.74) | 0.18 |
| Specialty care visits/year | ||||
| Baseline‡ | 3.3 ± 3.4 | 3.7 ± 3.7 | — | |
| Year 1 | 3.6 ± 3.8 | 3.8 ± 3.6 | 0.02 (−0.29 to 0.33) | 0.92 |
| Year 2† | 3.6 ± 3.7 | 4.0 ± 3.5 | 0.21 (−0.10 to 0.52) | 0.18 |
| Cost measures | ||||
| Total health care costs ($) | ||||
| Baseline | 6,280 ± 8,365 | 7,148 ± 11,854 | — | |
| Year 1† | 8,235 ± 14,752 | 6,785 ± 8,285 | −1,633 (−2,620 to −646) | 0.001 |
| Year 2 | 9,269 ± 15,683 | 8,113 ± 12,789 | −1,230 (−2,494 to 33) | 0.06 |
| Inpatient costs ($) | ||||
| Baseline | 1,305 ± 4,810 | 1,920 ± 8,536 | — | |
| Year 1† | 2,297 ± 9,613 | 1,334 ± 4,836 | −1,021 (−1,688 to −367) | 0.002 |
| Year 2 | 2,441 ± 9,395 | 1,956 ± 8,784 | −496 (−1,359 to 367) | 0.26 |
| Primary care costs ($) | ||||
| Baseline | 956 ± 993 | 1,077 ± 888 | — | |
| Year 1† | 1,022 ± 1,224 | 1,180 ± 1,062 | 129 (32 to 226) | 0.009 |
| Year 2 | 1,073 ± 1,226 | 1,157 ± 1,087 | 49 (−51 to 150) | 0.34 |
| Specialty care costs ($) | ||||
| Baseline‡ | 908 ± 1,612 | 947 ± 1,748 | — | |
| Year 1 | 1,037 ± 1,687 | 949 ± 1,171 | −97 (−212 to 18) | 0.10 |
| Year 2 | 1,133 ± 1,847 | 1,182 ± 1,636 | 51 (−96 to 199) | 0.50 |
Data are means ± SD or means (95% CI); health care costs are presented in 2003 dollars.
Adjusted mean use and costs differences for SS participants and control subjects from multivariate linear regression models using robust SEM estimates that controlled for age, sex, preventive services index, RxRisk (chronic disease score), any arthritis visits at baseline, and respective baseline use and cost measures.
Unadjusted year 1 and 2 comparisons between controls and SS participants, P < 0.05.
Baseline unadjusted comparisons between control subjects and SS participants, P < 0.05.
In year 1, SS participants had lower unadjusted total health care costs and more primary care visits than control subjects (both P < 0.05) but hospitalization rates were similar (see Table 2). In year 2, SS participants had fewer unadjusted hospitalizations (P = 0.004) and more unadjusted primary and specialty care visits (both P < 0.05) than control subjects, but unadjusted total health care costs were similar.
Adjusted comparisons between SS participants and control subjects
In year 1, SS participants had significantly lower adjusted total health care costs than control subjects (−$1,633 [95% CI −$2,620 to −$646]) (Table 2), primarily due to an adjusted lower hospitalization rate (P < 0.07) and lower adjusted inpatient costs (−$1,021 [$1,688 to −$367], P = 0.002). SS participants had a higher adjusted number of primary care visits (<0.001) and associated costs (P = 0.009) than control subjects. In year 2, SS participants had adjusted total health care costs that were similar to costs of control subjects, but these total costs trended lower (−$1,230, [−$2,494 to $33], P = 0.06). SS participants had a 29% lower adjusted hospitalization rate (P = 0.003), but adjusted inpatient costs were similar (−$496, [−$1,359 to $367], P = 0.26). There were no differences in the number or costs of primary or specialty care visits between SS participants and control subjects in year 2 (all P > 0.05).
Exploratory analysis: effects of SS visits
SS participants were dichotomized into two groups according to their average weekly attendance in year 1: fewer than two SS visits/week (n = 451) and two or more SS visits/week (n = 167). At baseline, the two groups were comparable in age, sex, and preventive services index. However, SS participants with fewer than two SS visits/week had a higher RxRisk score ($3,421 ± 2,132 vs. $2,973 ± 1,499, P = 0.004) and higher A1C levels (7.47 ± 1.3 vs. 7.1 ± 1.1, P = 0.002) compared with SS participants with two or more SS visits/week.
SS participants who made fewer than two SS visits/week had a significantly higher hospitalization rate (13.7 vs. 7.2%), more primary care visits (7.8 ± 5.5 vs. 5.8 ± 3.9), and more specialty visits (4.1 ± 3.8 vs. 3.1 ± 2.6) than SS participants who made two or more SS visits/week in year 1. Because we did not have access to specific data on whether disease burden increased in year 1, during which the exposure data of SS visits were used, we compared the proportion of outpatient visits with new diagnostic codes, e.g., arthritis, cardiovascular disease, and depression, between these two subgroups. SS participants who made fewer than two SS visits/week had slightly more outpatient visits in which arthritis (10.2 vs. 9.0%), coronary artery disease (10 vs. 8.4%), hypertension (16.9 vs. 13.8%), congestive heart failure (6.0 vs. 2.4%), and depression (4.9 vs. 1.2%) were indicated on the problem list compared with the group making two or more SS visits/week.
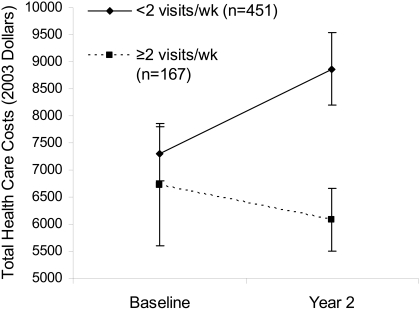
SS participants who made on average two or more SS visits/week had significantly lower adjusted total health care costs ($2,141 [95%CI −$3,877 to −$405], P = 0.02) than SS participants who made fewer than two SS visits/week (Fig. 1). SS visits per week as a continuous independent variable was included in a separate model with similar results, suggesting that higher mean visits per week over year 1 was associated with lower health care costs in year 2 (β = −542, SEM = 333 [95% CI −1,194 to 112], P = 0.10).
Figure 1.
Total health care cost difference from baseline to year 2 based on year 1 attendance (♦, fewer than two visits/week; ▪, two or more visits/week). Model adjusted for age, sex, RxRisk, new diagnosis of congestive heart failure or depression in year 1, and baseline total health care costs.
CONCLUSIONS
Older Medicare beneficiaries with diabetes who participated in an HMO-sponsored health club benefit had notable reductions in total health care costs at both 1 year (−$1,633, P < 0.001) and 2 years (−$1,230, P = 0.06) after program enrollment compared with similar enrollees who did not participate in the program. The cost savings were largely attributable to fewer hospital admissions and lower inpatient care costs with those hospitalizations. We also found that participation in the SS program of two or more visits/week on average in year 1 was associated with lower total health care costs in year 2 compared with less frequent participation. These results suggest that physical activity by older adults with diabetes has the potential to have an impact on the considerable economic burden of diabetes on the health care system and society (1,24). This is the first study to show an association between reduced health care costs and participation in a health plan–sponsored health club benefit in a cohort of older adults with diabetes over a 2-year period.
While promising, these results should be interpreted with caution. Although we were able to adjust for a number of key variables that were available from automated administrative data, we were unable to account for all possible differences in factors that could have an impact on health care use and costs. The finding that SS participants had significantly more primary care visits and a higher preventive services index compared with control subjects suggests a potential selection bias and differences in health status and health-seeking behavior between the two groups. For instance, individuals who seek out more contact with the health care system might be more motivated to comply with medical treatments, engage in more health-screening activities, increase physical activity, improve their diet, or quit smoking. These behaviors may result in lower health care costs regardless of participation in a formal exercise program. We attempted to control for both health status and health-seeking behavior by including a measure of chronic disease burden, a summary preventive services index, and an empirically derived propensity score in our regression models; however, it is possible that the observed differences are still subject to residual confounding.
We used visits to the SS program as a proxy for physical activity and did not have data on the exact dose of exercise that members engaged in at the health clubs nor were we able to characterize the density or intensity of these visits. Information on physical activity that members engaged in outside of the program was also not available. It is plausible that the cost differences associated with SS participation may have been mediated by a direct effect of regular exercise on improved cardiometabolic risk factor control (7) and fewer hospital admissions for acute hyperglycemic and cardiovascular complications. Other studies that have measured self-reported physical activity in older adults with diabetes (8) or other comorbidities (25) showed lower health care use or costs with higher levels of energy expenditure and walking duration. Di Loreto et al. (8) reported dose-response effects of increasing energy expenditure on A1C and plasma lipids. Sustained reductions in A1C were associated with lower health care costs within 1–2 years in a large cohort of adults with diabetes from this same HMO (26). A recent systematic review of diabetes disease management programs showed that in the short term, inpatient hospitalizations were reduced by a median of 18–31% in a general adult population (27). Our findings of a 20–29% difference in hospital admissions in years 1 and 2 between SS participants and control subjects compare favorably to these disease management interventions.
Experimental studies have shown that higher volumes of exercise are associated with greater reductions in A1C (7,28). Our exploratory analyses, which adjusted for potential confounding and selection bias, showed that participation in the SS program of two or more visits/week was associated with even greater cost savings. While promising, this finding should be interpreted with caution because the cost difference could primarily be due to the fact that healthier participants were able to participate more. Poor health, a greater number of comorbidities, and injuries have been associated with lower levels of physical activity in older adults (29,30)
We showed that elective participation in a health club benefit was associated with notable reductions in total health care costs over 2 years in older adults with diabetes. We also showed that greater use of such benefits resulted in even greater cost reductions in the long term; however, the dose-response results should not be interpreted as a recommendation to encourage patients with diabetes to initiate intensive physical activity. Previous studies of exercise treatment in individuals with other chronic conditions suggested that exercise itself does not place patients at increased medical risk (31), but a recent study showed higher than expected adverse events in middle- to older-aged patients with diabetes who participated in an aerobics and resistance exercise program compared with control subjects (38 vs. 14%) (28). These dose-response findings are novel, but they need to be confirmed with randomized controlled trials that address self-selection and can more closely monitor older adults with diabetes who engage in moderate or strenuous exercise. Such a study would provide more definitive evidence about the health and economic outcomes of a health plan–sponsored health club benefit for older adults with chronic conditions such as diabetes.
Our findings do suggest that the health care cost reductions associated with health club participation for older adults in general (14) also apply to older adults with diabetes. The impact on total health care costs are seen earlier and are of a threefold magnitude greater in this higher risk group. In contrast to the general older population that showed attenuated growth in total health care costs with greater participation, older adults with diabetes who made at least 2 visits/week to the SS program actually had reductions in total costs over time.
Acknowledgments
This study was funded in part by the University of Washington Health Promotion and Research Center (Centers for Disease Control and Prevention, grant U48-DP-000050) and grant 1KL2RR025015-01 to H.Q.N. from the National Center for Research Resources, a component of the National Institutes of Health.
Published ahead of print at http://care.diabetesjournals.org on 5 May 2008.
The contents of the report are solely the responsibility of the authors and do not necessarily represent the official view of the Centers for Disease Control and Prevention or the National Institutes of Health.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C Section 1734 solely to indicate this fact.
References
- 1.Hogan P, Dall T, Nikolov P: Economic costs of diabetes in the US in 2002. Diabetes Care 26:917–932, 2003 [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care 28(Suppl. 1):s4–s36, 2005 [PubMed] [Google Scholar]
- 3.Selvin E, Marinopoulos S, Berkenblit G, Rami T, Brancati FL, Powe NR, Golden SH: Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med 141:421–431, 2004 [DOI] [PubMed] [Google Scholar]
- 4. U.S. Physical Activity Statistics. Atlanta, US Department of Health and Human Services, Centers for Disease Control and Prevention. Available from http://www.cdc.gov. Accessed 14 February 2008
- 5.Martinson BC, O'Connor PJ, Pronk NP: Physical inactivity and short-term all-cause mortality in adults with chronic disease. Arch Intern Med 161:1173–1180, 2001 [DOI] [PubMed] [Google Scholar]
- 6.Pratt M, Macera C, Wang G: Higher direct medical costs associated with physical inactivity. Physician Sportsmed 28:63–70, 2000 [DOI] [PubMed] [Google Scholar]
- 7.Snowling NJ, Hopkins WG: Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Diabetes Care 29:2518–2527, 2006 [DOI] [PubMed] [Google Scholar]
- 8.Di Loreto C, Fanelli C, Lucidi P, Murdolo G, De Cicco A, Parlanti N, Ranchelli A, Fatone C, Taglioni C, Santeusanio F, De Feo P: Make your diabetic patients walk: long-term impact of different amounts of physical activity on type 2 diabetes. Diabetes Care 28:1295–302, 2005 [DOI] [PubMed] [Google Scholar]
- 9.Pratt M, Macera CA, Sallis JF, O'Donnell M, Frank LD: Economic interventions to promote physical activity: application of the SLOTH model. Am J Prev Med 27:136–145, 2004 [DOI] [PubMed] [Google Scholar]
- 10.McNeill LH, Kreuter MW, Subramanian SV: Social environment and physical activity: a review of concepts and evidence. Soc Sci Med 63:1011–1022, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Henry Kaiser Family Foundation Health Insurance Coverage in America: 2004 Data Update [article online]. Available from http://www.kff.org/uninsured/7451.cfm. Accessed 1 March 2008
- 12.Ackermann RT, Cheadle A, Sandhu N, Madsen L, Wagner EH, LoGerfo JP: Community exercise program use and changes in healthcare costs for older adults. Am J Prev Med 25:232–237, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Nguyen HQ, Ackermann RT, Berke EM, Cheadle A, Williams B, Lin E, Maciejewski ML, LoGerfo JP: Impact of a managed-medicare physical activity benefit on health care utilization and costs in older adults with diabetes. Diabetes Care 30:43–48, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Nguyen HQ, Ackermann RT, Maciejewski ML, Berke E, Patrick M, Williams B, LoGerfo JP: Managed-Medicare health club benefit and reduced health care costs among older adults. Prev Chron Dis 5:A14, 2008 [PMC free article] [PubMed] [Google Scholar]
- 15.Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P, Kinder L, Young B, Von Korff M: The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care 28:2668–2672, 2005 [DOI] [PubMed] [Google Scholar]
- 16.Wagner EH, Grothaus LC, Sandhu N, Galvin MS, McGregor M, Artz K, Coleman EA: Chronic care clinics for diabetes in primary care: a system-wide randomized trial. Diabetes Care 24:695–700, 2001 [DOI] [PubMed] [Google Scholar]
- 17.Simon GE, Katon WJ, Lin EH, Ludman E, VonKorff M, Ciechanowski P, Young BA: Diabetes complications and depression as predictors of health service costs. Gen Hosp Psychiatry 27:344–351, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Putnam KG, Buist DS, Fishman P, Andrade SE, Boles M, Chase GA, Goodman MJ, Gurwitz JH, Platt R, Raebel MA, Arnold Chan K: Chronic disease score as a predictor of hospitalization. Epidemiology 13:340–346, 2002 [DOI] [PubMed] [Google Scholar]
- 19.Fishman PA, Goodman MJ, Hornbrook MC, Meenan RT, Bachman DJ, O'Keeffe Rosetti MC: Risk adjustment using automated ambulatory pharmacy data: the RxRisk model. Med Care 41:84–99, 2003 [DOI] [PubMed] [Google Scholar]
- 20.Blough DK, Madden CW, Hornbrook MC: Modeling risk using generalized linear models. J Health Econ 18:153–171, 1999 [DOI] [PubMed] [Google Scholar]
- 21.Lumley T, Diehr P, Emerson S, Chen L: The importance of the normality assumption in large public health data sets. Annu Rev Public Health 23:151–169, 2002 [DOI] [PubMed] [Google Scholar]
- 22.D'Agostino RB Jr: Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17:2265–2281, 1998 [DOI] [PubMed] [Google Scholar]
- 23.Rosenbaum P, Rubin DB: The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55, 1983 [Google Scholar]
- 24.Garrett NA, Brasure M, Schmitz KH, Schultz MM, Huber MR: Physical inactivity: direct cost to a health plan. Am J Prev Med 27:304–309, 2004 [DOI] [PubMed] [Google Scholar]
- 25.Perkins AJ, Clark DO: Assessing the association of walking with health services use and costs among socioeconomically disadvantaged older adults. Prev Med 32:492–501, 2001 [DOI] [PubMed] [Google Scholar]
- 26.Wagner EH, Sandhu N, Newton KM, McCulloch DK, Ramsey SD, Grothaus LC: Effect of improved glycemic control on health care costs and utilization. JAMA 285:182–189, 2001 [DOI] [PubMed] [Google Scholar]
- 27.Norris SL, Nichols PJ, Caspersen CJ, Glasgow RE, Engelgau MM, Jack L, Isham G, Snyder SR, Carande-Kulis VG, Garfield S, Briss P, McCulloch D: The effectiveness of disease and case management for people with diabetes: a systematic review. Am J Prev Med 22:15–38, 2002 [DOI] [PubMed] [Google Scholar]
- 28.Sigal RJ, Kenny GP, Boulé NG, Wells GA, Prud'homme D, Fortier M, Reid RD, Tulloch H, Coyle D, Phillips P, Jennings A, Jaffey J: Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Ann Intern Med 147:357–369, 2007 [DOI] [PubMed] [Google Scholar]
- 29.Heesch KC, Brown DR, Blanton CJ: Perceived barriers to exercise and stage of exercise adoption in older women of different racial/ethnic groups. Women Health 30:61–76, 2000 [DOI] [PubMed] [Google Scholar]
- 30.Lees FD, Clark PG, Nigg CR, Newman P: Barriers to exercise behavior among older adults: a focus-group study. J Aging Phys Act 13:23–33, 2005 [DOI] [PubMed] [Google Scholar]
- 31.Brooks D, Krip B, Mangovski-Alzamora S, Goldstein RS: The effect of postrehabilitation programmes among individuals with chronic obstructive pulmonary disease. Eur Respir J 20:20–29, 2002 [DOI] [PubMed] [Google Scholar]