Abstract
OBJECTIVES— To assess the association between impaired chronotropic response (CR) and adverse events among patients with diabetes referred for exercise treadmill testing (ETT).
RESEARCH DESIGN AND METHODS— Impaired CR was defined as achievement of <80% of a patient's heart rate reserve. We used multivariable Cox proportional hazards regression to assess the independent association between impaired CR and adverse outcomes adjusting for demographics, comorbidities, and treadmill variables including the Duke Treadmill score.
RESULTS— Of 1,341 patients with diabetes, 35.7% (n = 479) demonstrated impaired CR during ETT. Patients with impaired CR were at increased risk of all-cause mortality, myocardial infarction, or coronary revascularization procedures. In multivariable analyses, impaired CR remained significantly associated with adverse outcomes (hazard ratio 1.53 [95% CI 1.10–2.14]).
CONCLUSIONS— Among patients with diabetes, impaired CR is common during ETT and is associated with adverse outcomes. Impaired CR can be used as another noninvasive tool to risk-stratify patients with diabetes following ETT.
Impaired chronotropic response (CR) is defined as inability of the heart rate to increase normally with exercise and may be related to alterations in sympathetic and parasympathetic tone, as well as autonomic dysfunction (1). Impaired CR during exercise treadmill testing (ETT) is associated with increased risk of cardiac events and all-cause mortality (2–4). Patients with diabetes have a higher incidence of autonomic dysfunction, and therefore impaired CR during ETT may identify patients with diabetes at risk for adverse outcomes (1). However, prior studies assessing the prognostic import of impaired CR have not specifically focused on this subgroup or have only included small numbers of patients with diabetes or the association between impaired CR and adverse outcomes has been inconclusive among patients with diabetes (1,3,5). Therefore, the objective of this study was to assess the association between impaired CR and adverse events, including all-cause mortality, myocardial infarction, and coronary revascularization procedures among patients with diabetes referred for ETT in routine clinical practice.
RESEARCH DESIGN AND METHODS
We examined a consecutive, prospective cohort of patients (n = 9,569) referred for ETT between July 2001 and June 2004. Details of this cohort have been previously described (6). All patients were enrolled in Kaiser Permanente of Colorado (KPCO), an integrated, nonprofit managed care organization that provides medical services to over 475,000 members in the Denver, Colorado, metropolitan area. Of these patients, 1,341 (14.0%) had diabetes and comprise the analytical cohort.
Before ETT, a structured history and medical record review were performed. Symptom-limited ETT was conducted according to standardized protocols, with the Bruce protocol used in 85% of tests. During each exercise and recovery stage, symptoms, blood pressure, heart rate, cardiac rhythm, and metabolic equivalents were recorded. The Duke Treadmill Score (DTS) was calculated using the total exercise time or energy expenditure, maximal ST-segment depression, and angina severity score (7). Only 35 patients had high-risk DTS (score < −10) and were excluded given the low likelihood that their clinical management would change by additional ETT information. For patients undergoing multiple treadmill tests during this period, only the first test was considered in the analyses.
Predictor variable
Impaired CR was defined as achievement of <80% of a patient's heart rate reserve, calculated as (220 − age) − resting heart rate, at peak exercise or <62% for patients taking β-blockers within 72-h of ETT (2).
Outcome variables
The primary outcome of interest was the combined end point of all-cause mortality, hospitalization for acute myocardial infarction (MI), or receipt of coronary revascularization procedure (coronary artery bypass graft surgery or percutaneous intervention). All-cause mortality was determined from KPCO databases and validated by comparison with State of Colorado death certificates. Data on acute MI hospitalizations and coronary revascularization procedures within and outside of the KPCO system were identified from KPCO databases. Follow-up and vital status information was available after the exercise test on 99% of patients through 31 October 2005.
Statistical analysis
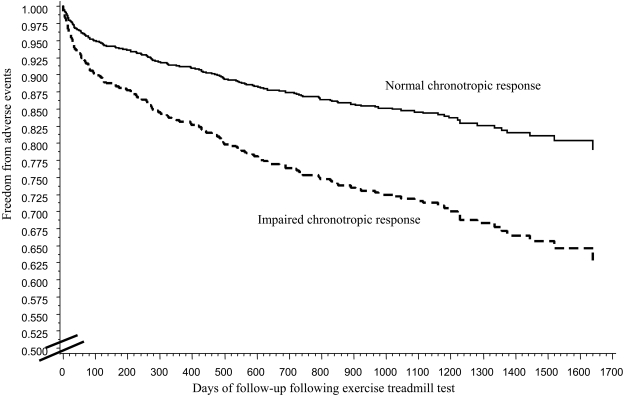
Baseline characteristics were compared between diabetic patients with or without impaired CR. Freedom from events by CR category was graphically represented by Kaplan-Meier curves and compared with the log-rank test.
Multivariable Cox proportional hazards models assessed the independent association between impaired CR and outcomes. Variables entered into the multivariable models included demographic factors (age and sex), clinical factors (smoking status, history of coronary artery disease, cerebral vascular disease, peripheral vascular disease, cancer, chronic obstructive pulmonary disease, obstructive sleep apnea, diabetes, hypertension, lipid disorders, depression, and congestive heart failure), and treadmill variables (DTS, abnormal heart rate recovery, and ventricular ectopy in recovery). We also stratified our cohort into low- or intermediate-risk DTS and repeated the analyses assessing the association between impaired CR and adverse outcomes. The Cox proportional hazards assumption was verified for all models by calculating and graphing Schoenfeld residuals by survival time. The study was approved by the Kaiser Permanente Colorado Institutional Review Board.
RESULTS
Over one-third of patients with diabetes (35.7%, n = 479) demonstrated impaired CR during ETT. Patients with impaired CR were more likely to have comorbid conditions (e.g., hypertension, coronary artery disease, peripheral vascular disease, and congestive heart failure) and abnormal heart rate recovery during ETT. In addition, patients with impaired CR, compared with patients with normal CR, were at increased risk of adverse outcomes including all-cause mortality (4.2 vs. 1.9%, P = 0.02), myocardial infarction (3.3 vs. 1.7%, P = 0.06), and revascularization procedures (23.8 vs. 11.7%, P < 0.01) (Fig. 1).
Figure 1.
Kaplan-Meier curve for freedom from adverse events (all-cause mortality, MI, or revascularization procedures) between patients with and without impaired CR during ETT.
In multivariable analyses, impaired CR remained significantly associated with increased risk of adverse outcomes, including all-cause mortality, MI, or revascularization procedures (hazard ratio 1.53 [1.10–2.14]). In stratified analyses, the association between impaired CR and adverse outcomes demonstrated a similar trend for patients with low- (1.36 [0.85–2.20]) or intermediate- (1.95 [1.15–3.31]) risk DTS.
CONCLUSIONS
In a community-based cohort of patients with diabetes referred for ETT, impaired CR was common and associated with adverse outcomes even after adjusting for DTS. These findings add to the literature by demonstrating the prognostic utility of impaired CR during ETT among patients with diabetes and complement the prior work on impaired CR and outcomes in the general population of patients referred for ETT. Together, these studies support the use of impaired CR as another noninvasive tool to risk stratify patients following ETT beyond the routine parameters of ST-segment change, presence of angina, and treadmill exercise time. Additional studies are needed to determine whether the presence of impaired CR during ETT among patients with diabetes should lead to more aggressive medical therapy, additional noninvasive testing with imaging, or invasive evaluation.
Acknowledgments
This study was funded in part by CV Therapeutics, Inc. The sponsors were not directly involved in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation of the manuscript. P.M.H. is supported by a VA Research & Development Career Development Award.
Published ahead of print at http://care.diabetesjournals.org on 13 May 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C Section 1734 solely to indicate this fact.
References
- 1.Albers AR, Krichavsky MZ, Balady GJ: Stress testing in patients with diabetes mellitus: diagnostic and prognostic value. Circulation 113:583–592, 2006 [DOI] [PubMed] [Google Scholar]
- 2.Kligfield P, Lauer MS: Exercise electrocardiogram testing: beyond the ST segment. Circulation 114:2070–2082, 2006 [DOI] [PubMed] [Google Scholar]
- 3.Lauer MS, Francis GS, Okin PM, Pashkow FJ, Snader CE, Marwick TH: Impaired chronotropic response to exercise stress testing as a predictor of mortality. JAMA 281:524–529, 1999 [DOI] [PubMed] [Google Scholar]
- 4.Lauer MS, Okin PM, Larson MG, Evans JC, Levy D: Impaired heart rate response to graded exercise: prognostic implications of chronotropic incompetence in the Framingham Heart Study. Circulation 93:1520–1526, 1996 [DOI] [PubMed] [Google Scholar]
- 5.Chacko KM, Bauer TA, Dale RA, Dixon JA, Schrier RW, Estacio RO: Heart rate recovery predicts mortality and cardiovascular events in patients with type 2 diabetes. Med Sci Sports Exerc 40:288–295, 2008 [DOI] [PubMed] [Google Scholar]
- 6.Peterson PN, Magid DJ, Ross C, Ho PM, Rumsfeld JS, Lauer MS, Lyons EE, Smith SS, Masoudi FA: Association of exercise capacity on treadmill with future cardiac events in patients referred for exercise testing. Arch Intern Med 168:174–179, 2008 [DOI] [PubMed] [Google Scholar]
- 7.Mark DB, Shaw L, Harrell FE, Jr. et al. Prognostic value of a treadmill exercise score in outpatients with suspected coronary artery disease. N Engl J Med 325:849–853, 1991 [DOI] [PubMed] [Google Scholar]