Appendicitis occurs most commonly in the second and third decades of life. Obstruction of the appendiceal lumen appears to be one of the most common physiologic mechanisms for the development of acute appendicitis. Once obstructed, the dilatation of the lumen causes ischemia and necrosis of the wall.
The most common organisms involved in gangrenous and perforated appendicitis are Escherichia coli, Peptostreptococcus, Bacillus fragilis and Pseudomonas sp. Rarely, Actinomyces sp. is involved in this process.
Actinomyces causes a nonspecific inflammatory response composed of neutrophils, foamy histiocytes, lymphocytes and plasma cells. Less frequently, it may induce a granulomatous inflammation, as seen in the case we report here.
Case report
A 45-year-old woman presented with a 10-day history of progressively worsening abdominal pain in the right lower quadrant. Her medical history included tonsillectomy during childhood. Clinically, she was apyrexial, and her vitals signs were normal. Examination of her abdomen revealed rebound tenderness over the right lower quadrant. Rectal examination was painful with referred pain to the right lower quadrant.
Initial blood counts and results of blood chemistry tests were entirely normal except for an elevated leukocyte count at 14.3 g/L and C-reactive protein at 109 mg/L. Abdominal computed tomography (CT) with intravenous contrast medium enhancement demonstrated an inflammatory mass in the ileocecal zone, with localized signs of perforation; the appendix was not visible (Fig. 1). A laparoscopic appendectomy was performed.
FIG. 1. On CT, an inflammatory mass was visualized in the ileocecal area, with localized signs of perforation (arrow). The appendix cannot be seen.
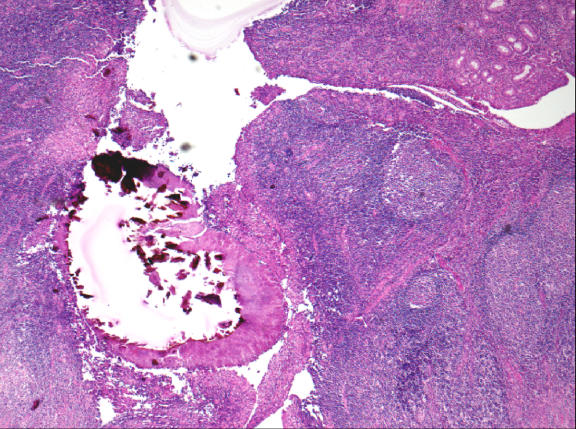
A microscopic examination revealed chronic follicular transmural inflammation throughout the appendiceal wall, associated with nonnecrotic granulomas consisting of epithelioid and giant cells. There were no signs of acute inflammation. In the appendiceal lumen, colonies of actinomycotic organisms exhibiting club-shaped filaments arranged in a radiating rosette pattern were found (Fig. 2).
FIG. 2. Colonies of actinomycotic organisms in the appendiceal lumen exhibiting club-shaped filaments arranged in a radiating rosette pattern (hematoxylin–eosin stain, original magnification ×50).
The patient's postoperative course was uncomplicated. On day 2, she returned home with a normal level of C-reactive protein and a normal leukocyte count. After definitive diagnosis, the patient was readmitted to the hospital for a 2-week course of intravenous penicillin G therapy. This was followed by 6-month amoxicillin oral therapy. Control abdominal CT performed 2 weeks postoperatively did not show other lesions suspicious for actinomycosis in the abdominal cavity, and a colonoscopy performed 2 months postoperatively showed normal colonic mucosa of the cecum.
Discussion
Actinomycosis is a well-recognized disease entity in the kidney and gallbladder and has been reported in the ovaries, fallopian tubes, lymph nodes, bones, lungs, soft tissue, appendix, epididymis and adrenal glands.
Actinomycosis is a rare infectious disease caused in almost all cases by the filamentous anerobic gram-positive bacterium Actinomyces israelii. This microorganism is not very virulent and is usually found in the human oropharynx. Actinomycosis occurs worldwide, predominating in areas with poor standards of dental care.1 When it is pathogenic, it causes a characteristic reaction of xanthogranulomatous inflammation. Actinomycosis infection has been categorized into 4 main clinical manifestations including the cervicofacial, abdominopelvic, thoracic and central nervous system. The most frequent location is cervicofacial (30%), followed by abdominopelvic (20%), thoracic (15%) and central nervous system (3%).2–4 The involvement of the gynecologic tract has been reported recently in relation to the use of an intrauterine device.3,4 Anorectal and hepatobiliary primary actinomycosis have been described.5 The involvement of multiple organs is rare but has been reported.2,3 In the case of abdomino-pelvic actinomycosis, the rate of appendiceal localization is about 65%. The symptoms are unspecific and mimic a typical appendicitis. The predisposing factors include previous abdominal surgery, foreign bodies, appendicitis, bowel perforation, neoplasm and idiopathic bowel inflammatory diseases (Crohn's disease). Preoperative diagnosis is rare and is made in fewer than 10% of cases. Once the diagnosis is made, intense, prolonged medical treatment with systemic antibiotics should be initiated to eradicate the disease. Surgery is used only as a therapeutic adjunct to remove necrotic tissue or persistent sinuses.
In our case, no predisposing factors could be identified, and primary actinomycosis of the appendix seems to be the sole etiology. Clinically, actinomycosis mimics appendicitis. A prolonged course of antibiotics is of paramount importance to decrease the risk of recurrence. To rule out any symptomatic and local complications, CT and colonoscopy should be performed
Competing interests: None declared.
Accepted for publication Nov. 20, 2007
Correspondence to: Dr. M. Maternini, Department of Surgery, Riviera Hospital, Av. Belmont 25, 1820 Montreux, Switzerland; fax 41 21 966 66 20; Matteo.Maternini@fhv.ch
References
- 1.Tedder M, Wolfe WG. Actinomycosis and nocardial infections. Chest Surg Clin N Am 1993;3:653-70.
- 2.Yeguez JF, Martinez SA, Sands LR, et al. Pelvic actinomycosis presenting as malignant large bowel obstruction: a case report and a review of the literature. Am Surg 2000;66:85-90. [PubMed]
- 3.Cintron JR, Del Pino A, Duarte B et al. Abdominal actinomycosis. Dis Colon Rectum 1996;39:105-8. [DOI] [PubMed]
- 4.O'Connor KF, Bagg MN, Croley MR. Pelvic actimomycosis associated with intrauterine devices. Radiology 1989;170:559-60. [DOI] [PubMed]
- 5.Alvarado-Cerna R, Bracho-Riquelme R. Perianal actinomycosis — a complication of a fistula-in-ano. Report of a case. Dis Colon Rectum 1994;37:378-80. [DOI] [PubMed]