Abstract
Background
In damage-control surgery, definitive abdominal closure may not be possible for several days or weeks after laparotomy until the patient has stabilized.
Methods
We present 23 patients treated with the Canica ABRA® dynamic wound closure system that re-approximated open abdomens with silicone elastomers placed transfascially across the wound. This study aimed to assess the results of using this system and to identify risk factors for unsuccessful closure. The system maintains a medially directed force across the wound. A traditional regimen of wound dressing changes was performed.
Results
The dynamic closure system remained in place an average of 48 days and was applied an average of 18 days after the beginning of treatment for the open abdominal wound. Delayed primary fascial closure was achieved in 14 of 23 patients (61%) without further surgery. Six patients (26%) healed with ventral hernias but with a smaller abdominal defect. Two patients (9%) developed enterocutaneous fistulae through the wound that required further surgery. An overall reduction in wound area of 95% was achieved.
Conclusion
This dynamic wound closure technique permitted the delayed primary closure of open abdomens in 61% of cases when treatment was instituted an average of 18 days after initial laparotomy.
Abstract
Contexte
Au cours d'une intervention chirurgicale visant à limiter les dégâts, il arrive qu'on ne puisse pas refermer définitivement l'abdomen pendant plusieurs jours ou semaines après une laparotomie, jusqu'à ce que le patient se soit stabilisé.
Méthodes
Nous présentons le cas de 23 patients traités au moyen du système de fermeture dynamique de plaie Canica ABRAMD qui rapproche les lèvres de plaies abdominales ouvertes au moyen d'élastomères en silicone disposés perpendiculairement à la plaie. Cette étude visait à évaluer les résultats de l'utilisation du système et à déterminer les facteurs de risque d'une fermeture non réussie. Le système exerce une force perpendiculaire sur la plaie. On a appliqué un régime traditionnel de changements de pansements.
Résultats
Le système de fermeture dynamique est demeuré en place en moyenne 48 jours et a été appliqué en moyenne 18 jours après le début du traitement de la plaie abdominale ouverte. On a réussi à retarder la fermeture fasciale primaire chez 14 des 23 patients (61 %) sans autre intervention chirurgicale. Six patients (26 %) ont guéri avec une hernie ventrale mais avaient un défaut abdominal moindre. Deux patients (9 %) ont eu des fistules entérocutanées dans la plaie qui ont obligé à pratiquer une autre intervention chirurgicale. On a réussi à réduire de 95 % la superficie de la plaie.
Conclusion
Cette technique de fermeture dynamique de la plaie a permis de retarder la fermeture primaire d'abdomens ouverts dans 61 % des cas lorsqu'on a commencé le traitement en moyenne 18 jours après la laparotomie initiale.
Damage-control surgery is abbreviated surgery performed to control a patient's life-threatening illness. It minimizes the time during which the patient is exposed to coagulopathic stimuli, hypothermia and acidosis in the operating room in favour of returning the patient to the intensive care unit as expeditiously as possible for a full resuscitation. It is typically performed for treatment of trauma, abdominal sepsis and abdominal compartment syndrome. Bowel and retroperitoneal edema resulting from hypoperfusion and resuscitative efforts frequently prevent reapproximation of the abdominal fascia. The patient is returned to the operating room 24–48 hours later for definitive treatment of the injuries should he or she survive.1 Definitive abdominal closure may not be possible for several days or weeks, until the patient has stabilized.
Damage-control laparotomy has increased the number of patients surviving to require treatment for an open abdomen. Temporary abdominal wall closure can be achieved by placing an absorbable mesh or plastic visceral retainer and packing the resultant wound with gauze with or without retention sutures. The fascia then retracts laterally, and loss of abdominal domain begins. This may permanently prevent fascial closure and require treatment through a planned ventral hernia repair in which the exposed bowel, optionally covered with absorbable mesh, is allowed to develop a confluent layer of granulation tissue. After about 2 weeks, the abdomen becomes “frozen” from multiple adhesions between viscera, the remaining abdominal wall and the granulating surface. Future abdominal surgery is more complicated, with increased morbidity and mortality. The granulation tissue is later skin-grafted, and definitive repair of the resultant hernia is performed in 9–12 months, if technically feasible with techniques such as skin stretching and components of separation flaps.2–6
A ventral hernia is a suboptimal result. In the state of Washington, a study followed 10 822 patients who had surgery for incisional hernias over 13 years.7 The rates for reoccurring hernias were 12.3% at 5 years and 23.1% at 13 years. An increase in the use of mesh from 34.1% in 1987 to 65.5% in 1999 did not affect cumulative recurrence rates. Similar results are reported elsewhere.8 Patients often have permanent disabling abdominal wall defects that cause postural imbalance, gastrointestinal (GI) symptoms and loss of adequate diaphragmal support for ventilation. These defects demonstrate the importance of achieving complete fascial closure in the treatment of open abdominal wounds.
We used the ABRA® (Canica Design) abdominal wall dynamic closure system, which is designed to allow gradual reapproximation of abdominal midline muscles and fascia by using elastomers as dynamic retention sutures. Dynamic wound closure refers to placing the abdominal fascia under continuous variable medial tension that approximates the wound edges while allowing them to remain sufficiently mobile to oscillate with breathing and patient movement.
Fixation of the elastomers in self-retaining anchors away from the wound allows for traditional wound débridement and dressing regimens.
This study is an observational retrospective series of 23 patients at a single institution and follows a successful case report of this system by Urbaniak.9
The objectives of this study were to evaluate the Canica ABRA® dynamic fascial closure system and, in particular, to determine the time to fascial closure and complications such as hernia and fistula formation. We also identified risk factors for unsuccessful closures in our case series.
Methods
We present 23 patients with open abdomens that could not be primarily closed more than 7 days after the cause for primary surgical intervention had resolved. These patients were treated between September 2000 and September 2005.
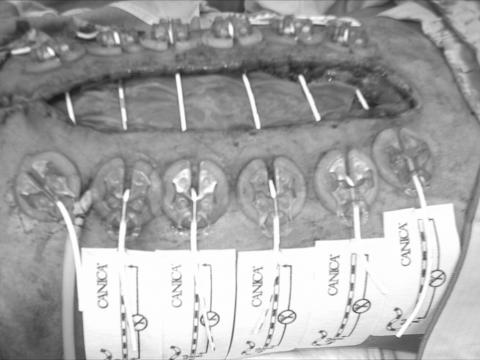
We applied the ABRA® system according to the manufacturer's instructions. An elastomer is inserted through a stab incision starting about 5 cm back from the wound edge and across the defect, preferably passing below the fascia and above a mesh or other visceral retainer. It exits an equal distance back from the wound edge on the contralateral side. These elastomers are placed about 3 cm apart along the wound length, which is as close as the padding of the button anchors will permit. Button anchors are placed, and the elastomers are connected and tensioned to about twice their tension-free length (290 g). To prevent the elastomer tearing medially through the abdominal wall, an adhesive button tail is attached to the anchor and fixed to the skin (Fig. 1).
FIG. 1. Application of the dynamic closure system through skin and subcutaneous tissue 9 days after this patient developed an open abdomen from a leaked esophagectomy with colonic interposition graft. Note the button tails hooked into the button anchors to prevent medial tearing of the elastomer.
Dressing changes are performed as per standard practices. The system is inspected daily, and elastomer tension is adjusted as needed to maintain a constant force of 290 g. In case of skin tearing or ulceration, tension is reduced and additional padding is placed under the anchor.
Primary suture closure was performed when it was possible to approximate the fascial edges (Fig. 2). Split-thickness skin grafting was employed when no further fascial approximation could be achieved by medial traction.
FIG. 2. Abdomen 37 days after the application of dynamic closure.
Patients were selected for application of this system when the consulting surgeon was of the opinion that traditional wound management approaches would not allow fascial reapproximation and that no other options existed apart from a planned ventral hernia approach. Cases were not consecutive and were chosen when a participating surgeon was consulted and when the closure equipment was available.
We measured the original length and width of the open abdomens by ruler when the system was first applied and again when the system was removed; length and width were defined as 0 if the fascia was completely reapproximated. To calculate wound area, we assumed the wound to be rectangular and multiplied the length by the width. Hernia occurrence after system removal was determined clinically. The presence of herniation and the need for a skin graft were determined by a hospital chart review conducted in November 2005. Statistics were calculated with spreadsheet functions in OpenOffice.org (Sun Microsystems). The Simplified Acute Physiology II (SAPS II) probability of dying score was calculated according to Le Gall's method.10
This study received approval from our hospital's research ethics board.
Results
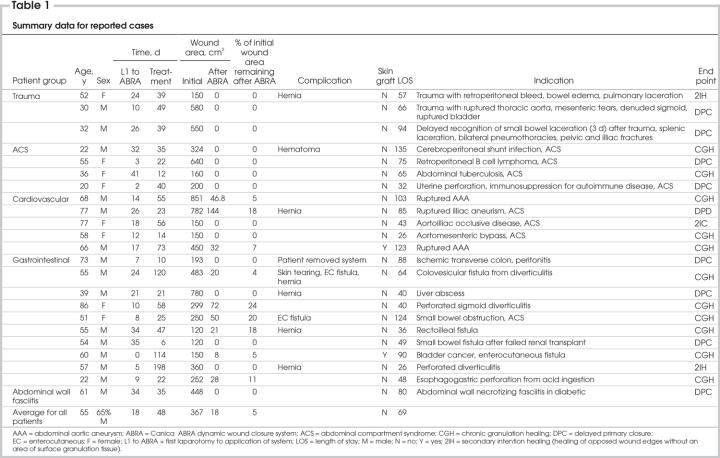
Of the 23 patients included in this study, 14 (61%) achieved delayed primary closure. The duration of system application for those achieving successful closure was 40 days on average. The time between creation of the open abdomen and application of the system was 18 days on average. Of the patients, 65% were men. In 9 cases where complete abdominal closure was not achieved, wound area decreased by an average of 87%. Not all cases of incomplete closure developed clinically apparent hernias. The rate of hernia formation was 26% (6/23), and the rate of enterocutaneous fistulization was 9% (2/23). Table 1 summarizes these cases.
Table 1
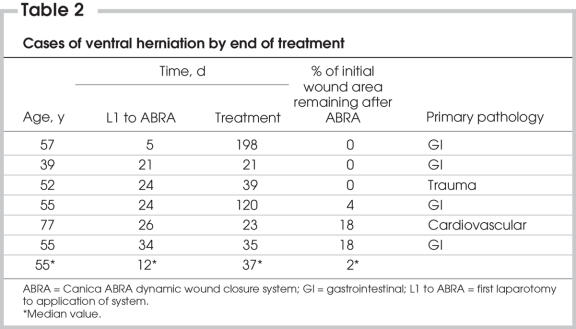
In Table 1, patients are listed according to primary pathology: trauma (n = 3), cardiovascular (n = 5), gastrointestinal (n = 10) and diagnosis of abdominal compartment syndrome (ACS; n = 4). In all trauma and ACS patients, the end point of complete closure was achieved. Of the 5 cardiovascular patients, 2 had full abdominal wall closure; of the 10 GI patients, only 4 experienced closure with this system. The age range in the cardiovascular and GI groups was higher than average (51–86 y and 58–77 y, respectively), compared with the trauma and ACS groups (32–52 y and 22–55 y, respectively). In the GI patient group, the longest treatment with dynamic closure was also experienced (120–198 d). In addition, of 6 patients with incisional hernias at the end of treatment, 4 were GI patients. (Table 2).
Table 2
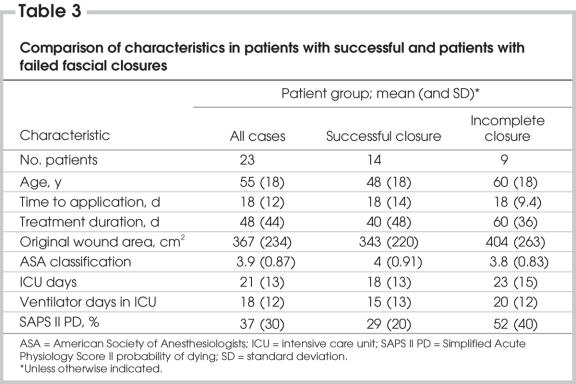
Several variables were examined to determine which patient characteristics would lead to a lower likelihood of wound closure (Table 3). Factors most strongly associated with failed closure were treatment duration, the patient's probability of dying as determined by the SAPS II and the patient's age.
Table 3
Discussion
Hernia repair after failed abdominal closure frequently requires skin grafting, can cause accidental bowel damage and can fail, leading to recurrent herniation.11
Although primary closure of the abdominal wall is not the immediate goal in damage-control laparotomy, dynamic traction allows for stretching and relaxation of the abdomen with each respiration in a physiological fashion while preventing further lateral retraction of the abdominal muscles and fascia.
Several mechanisms support the concept of dynamic closure. Direct fascial stretching and expansion works through the principles of biological and mechanical creep.12 Mechanical stress upregulates tissue growth. Breburda and colleagues13 have shown that intermittent alternating tension and pressure microstimulation of growth plate fractures in bone stimulates chondrocyte proliferation. Langevin and colleagues14 demonstrated that subjecting mouse tissue to stretching increases fibroblast cell body perimeter and cross-sectional area. Fibroblast morphology changed from dentritic to sheetlike under tissue stretching, and the changes could be diminished by subjecting the stretched cells to the antimitotics colchicine and cytochalasin D. This suggests that cell biosynthesis adapts to a proliferative phenotype as a result of stretching.14
Using complementary DNA microchip array technology, Kessler and colleagues15 showed that 60 known genes were induced in mechanically stressed fibroblasts and 64 known genes were induced in a mechanically relaxed system. They defined induction as a 3-fold or greater change above baseline and concluded that mechanically stressed fibroblasts assumed a synthetic phenotype that downregulated the production of proteases and inflammatory mediators. The expression of connective tissue growth is upregulated in cells exposed to mechanical stress.16 It is also known that fibroblasts respond differently to growth factor stimulation depending on whether they are tensioned or untensioned, with the former acquiring a proliferative or biosynthetic phenotype as opposed to a quiescent phenotype in the latter.17 Changes also occur at the endothelial level, where shear stress enhances endothelial wound closure.18 Consequently, dynamic wound closure may exert benefits through multiple mechanisms at the cellular level.
This dynamic wound closure system presents an alternative to the conventional late management of open abdomens. In this series, we report successful delayed primary closure in 61% of cases when nonconventional treatments are started an average of 18 days after creation of the open abdomen and after an average of 48 days of treatment. A similar issue was examined by Miller and colleagues,19 who suggested that vacuum-assisted fascial closure could be used to achieve closure up to 1 month after initial laparotomy. Steenvoorde20 demonstrated that use of negative pressure as a single method in the treatment of open abdomens failed because of retraction of the abdominal muscles.
The dynamic wound closure system has 2 components: silicone elastomers and silicone-padded button anchors. The elastomers are applied to penetrate all abdominal layers, or as many as possible, depending on the mobility of the wound edge. Where abundant granulation tissue overgrowth was present when the system was placed several days after initial laparotomy, safe exposure of fascial flaps on either side of the wound was hindered. In such cases, the elastomer was placed through skin and subcutaneous tissues only. Before the elastomers were placed, an absorbable mesh was placed to cover underlying bowel. Usually, a single piece of vicryl mesh was used. However, in patients with considerable widening of the abdominal defect, 2 pieces were stacked to prolong mesh integrity.
Our results were more favourable than those in a study by Howdieshell and colleagues,5 who treated 71 surviving patients with open abdomens with the tension-free insertion of a silicone sheet. Of these, 24 (34%) achieved delayed primary fascial closure during the initial admission, and 34 (66%) required visceral skin grafting and readmission for closure.
A key difference between these studies and the present case series is our extremely late initiation of treatment, when significant adhesions and fascial retraction presented a much more difficult abdomen to close.1 To our knowledge, these results are the best ever reported for the closure of open abdomens when treatment is started 2 or more weeks after the initial laparotomy.
Hernias were found in 26% of our cases, as determined by a hospital chart review. Although the true rate was possibly higher, it compares well to the alternative of a 100% hernia rate in patients treated with a “planned ventral hernia repair” approach.6,21 As a result, dynamic wound closure likely reduced the need for future reconstructive surgery and spared patients from its related morbidity. Two enterocutaneous fistulae (9%) occurred. This common complication has been reported to occur in 4%–25% of patients,19 and its incidence is considered lower with the use of absorbable mesh.1 Hence, we would recommend that a single or double layer of absorbable mesh be placed to function as a visceral retainer in patients where it may remain permanently in situ.
Advanced age, higher SAPS II probability of dying and GI disease were proportionally more common in the group with failed closure, and these factors may therefore be predictive of poor outcome. The delay between when the abdomen was considered open and the application of the closure system was not associated with successful closure in this small series. A more timely application of the system at the first laparotomy that results in the open abdomen might yield faster and higher closure rates. Arguably, there would be less scar tissue present to impede fascial reapproximation.
Survival outcomes and long-term follow-up of patients were not performed. Both of these could be assessed in future studies to elucidate whether a relation exists between fascial closure technique and survival or delayed hernia recurrence.
Conclusion
The presented data, although limited, suggest that this dynamic wound closure system shows promising results in the late management of open abdominal wounds. Of all patients treated, 61% did not need surgery for secondary fascial repair.
Future controlled studies are needed to determine the best indications for dynamic wound closure and the best timing for the application of the closure system.
Acknowledgments
Our thanks to Canica Design Inc. (Almonte, Ont., Canada) for providing the dynamic closure devices used in the initial phases of this study free of charge. (The remaining devices were purchased at market rates.)
Contributors: Drs. Reimer, Yelle, Reitsma, Doumit and Allen designed the study. Drs. Reimer, Yelle, Doumit and Allen acquired the data, which Drs. Reimer, Yelle, Reitsma and Doumit analyzed. Drs. Reimer and Reitsma wrote the article, and Drs. Reimer, Yelle, Reitsma, Doumit and Allen reviewed it. All authors gave final approval for publication.
Competing interests: Dr. Bell is an inventor of the ABRA® abdominal wall closure system and a shareholder of its manufacturer, Canica Design Inc.
Accepted for publication Oct. 3, 2007
Correspondence to: Dr. M. Reimer, the Ottawa Hospital — General Campus, Rm. K-14, 501 Smyth Rd., Ottawa ON K1H 8L6; fax 613 737-8371; mwreimer@biologicalprocedures.com
References
- 1.Scott BG, Feanny MA, Hershberg A. Early definitive closure of the open abdomen: a quiet revolution. Scand J Surg 2005;94:9-14. [DOI] [PubMed]
- 2.Rutherford EJ, Skeete DA, Brasel KJ. Management of the patient with an open abdomen: techniques in temporary and definitive closure. Curr Probl Surg 2004;41:815-76. [DOI] [PubMed]
- 3.Tremblay LN, Feliciano DV, Schmidt J, et al. Skin only or silo closure in the critically ill patient with an open abdomen. Am J Surg 2001;182:670-5. [DOI] [PubMed]
- 4.Hultman CS, Pratt B, Cairns BA, et al. Multidisciplinary approach to abdominal wall reconstruction after decompressive laparotomy for abdominal compartment syndrome. Ann Plast Surg 2005;54:269-75. [PubMed]
- 5.Howdieshell TR, Proctor CD, Sternberg E, et al. Temporary abdominal closure followed by definitive abdominal wall reconstruction of the open abdomen. Am J Surg 2004;188:301-6. [DOI] [PubMed]
- 6.Cohen M, Morales R, Fildes J, et al. Staged reconstruction after gunshot wounds to the abdomen. Plast Reconstr Surg 2001;108:83-92. [DOI] [PubMed]
- 7.Flum DR, Horvath K, Koepsell TH. Have outcomes of incisional hernia repair improved over time: a population-based analysis. Ann Surg 2003;237:129-35. [DOI] [PMC free article] [PubMed]
- 8.v'ant Riet M, Vrijland WW, Lange JF, et al. Mesh repair of incisional hernia: comparison of laparoscopic and open repair. Eur J Surg 2002;168:684-9. [DOI] [PubMed]
- 9.Urbaniak RM, Khuthaila DK, Khalil AJ, et al. Closure of massive abdominal wall defects. A case report using the abdominal reapproximation anchor (ABRA®) system. Ann Plast Surg 2006;57:573-7. [DOI] [PubMed]
- 10.Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 1993;270:2957-63. [DOI] [PubMed]
- 11.Rosen M, Brody F, Ponsky J, et al. Recurrence after laparoscopic ventral hernia repair. Surg Endosc 2003;17:123-8. [DOI] [PubMed]
- 12.Taylor RC, Reitsma BJ, Sarazin S, et al. Early results using a dynamic method for delayed primary closure of fasciotomy wounds. J Am Coll Surg 2003;197:872-8. [DOI] [PubMed]
- 13.Breburda E, Wirth T, Leiser R, et al. The influence of intermittent external dynamic pressure and tension forces on the healing of an epiphyseal fracture. Arch Orthop Trauma Surg 2001;121:443-9. [DOI] [PubMed]
- 14.Langevin HM, Bouffard NA, Badger GJ, et al. Dynamic fibroblast cytoskeletal response to subcutaneous tissue stretch ex vivo and in vivo. Am J Physiol Cell Physiol 2005;288:C747-56. [DOI] [PubMed]
- 15.Kessler D, Dethlefsen S, Haase I, et al. Fibroblasts in mechanically stressed collagen lattices assume a “synthetic” phenotype. J Biol Chem 2001;276:36575-85. [DOI] [PubMed]
- 16.Ott C, Iwanciw D, Graness A, et al. Modulation of the expression of connective tissue growth factor by alterations of the cytoskeleton. J Biol Chem 2003;278:44305-44311. [DOI] [PubMed]
- 17.Grinnell F. Fibroblast biology in three-dimensional collagen matrices. Trends Cell Biol 2003;13:264-89. [DOI] [PubMed]
- 18.Albuquerque ML, Waters CM, Savla U, et al. Shear stress enhances human endothelial cell wound closure in vitro. Am J Physiol Heart Circ Physiol 2000;279:H293-302. [DOI] [PubMed]
- 19.Miller PR, Thompson JT, Faler BJ, et al. Late fascial closure in lieu of ventral hernia: the next step in open abdomen management. J Trauma 2002;53:843-9. [DOI] [PubMed]
- 20.Steenvoorde P, Rozeboom AL, Melief P, et al. Failure of the topical negative pressure abdominal dressing system in the “fat” open abdomen: report of a case and review of the literature. Wounds 2006;18(2):44-50.
- 21.Sriussadaporn S, Rattaplee P, Bunjongsat S. Immediate closure of the open adbomen with bilateral bipedicle anterior abdominal skin flaps and subsequent retrorectus prosthetic mesh repair of the late giant ventral hernias. J Trauma 2003;54:1083-9. [DOI] [PubMed]