Abstract
Objective
To define the models of surgical service delivery in rural communities that rely solely on general practitioner (GP)–surgeons for emergency care, to examine how they have changed over the past decade and to identify some effects on communities that have lost their local surgical program.
Methods
We undertook a retrospective study using the Population Utilization Rates and Referrals For Easy Comparative Tables database (versions 6.0 and 9.0) and telephone interviews to hospitals that we identified. We included all hospitals in rural British Columbia with surgical programs that had no resident specialist surgeon and that relied on general practitioner–surgeons (GP-surgeons) for emergency surgical care. We examined surgical program characteristics, community size, distance from referral centre, role of itinerant surgery, where GPs were trained, their age and years of experience and referral rates for appendectomies and obstetrics.
Results
Changes over the past decade include a decrease in the total number of GP-surgeons operating in these communities, more itinerant surgery and the loss of 3 of 12 programs. GP-surgeons are older, are usually foreign-trained and have more than 5 years of experience. Communities with no local program or that rely on solo practitioners refer more emergencies out of the community and do less maternity care than those with more than a single GP-surgeon.
Conclusion
GP-surgeons still play an integral role in the provision of emergency and elective surgical services in rural communities without the population base to sustain resident specialist surgeons. As GP-surgeons retire and surgical programs close, there is no accredited training program to replace them. More outcome comparisons between procedures performed by GP-surgeons and general surgeons are needed, as is the creation of a nationally accredited training program to replace these practitioners as they retire.
Abstract
Objectif
Définir les modèles de prestation des services chirurgicaux dans les communautés rurales qui comptent uniquement sur les omnipraticiens (OP)-chirurgiens pour les soins d'urgence, déterminer comment ils ont évolué au cours de la dernière décennie et cerner les effets sur les communautés qui ont perdu leur programme chirurgical local.
Méthodes
Nous avons entrepris une étude rétrospective fondée sur la base de données Population Utilization Rates and Referrals For Easy Comparative Tables (taux d'utilisation et références à utiliser pour établir facilement des tableaux comparatifs), versions 6.0 et 9.0, et sur des entrevues téléphoniques menées auprès des hôpitaux sélectionnés. Nous avons inclus tous les hôpitaux ruraux de la Colombie-Britannique qui avaient un programme chirurgical mais n'avaient pas de chirurgien spécialisé en résidence et qui comptaient sur des OP-chirurgiens pour dispenser les soins chirurgicaux d'urgence. Nous avons étudié les caractéristiques des programmes chirurgicaux, la taille de la communauté, l'éloignement du centre de référence, le rôle des services de chirurgie itinérants, l'endroit où les OP ont reçu leur formation, leur âge et leur expérience, ainsi que les taux de référence pour les appendicectomies et les soins obstétriques.
Résultats
Les changements survenus au cours de la dernière décennie comprennent une diminution du nombre total d'OP-chirurgiens dans ces communautés, une augmentation des services de chirurgie itinérants et la disparition de 3 des 12 programmes. Les OP-chirurgiens sont plus âgés, ont habituellement reçu leur formation à l'étranger et comptent plus de 5 ans d'expérience. Les communautés qui n'ont pas de programme local ou qui comptent sur un seul praticien réfèrent davantage de cas d'urgence à l'extérieur et dispensent moins de soins en maternité que celles qui comptent sur plus qu'un seul OP-chirurgien.
Conclusion
Les OP-chirurgiens jouent toujours un rôle essentiel dans la prestation de services chirurgicaux d'urgence et électifs dans les communautés rurales qui n'ont pas la population nécessaire pour faire vivre des chirurgiens spécialistes en résidence. À mesure que les OP-chirurgiens prennent leur retraite et que les programmes de chirurgie ferment leurs portes, il n'existe pas de programme de formation agréé pour les remplacer. D'autres comparaisons des résultats entre les interventions pratiquées par les OP-chirurgiens et les chirurgiens généraux s'imposent et il faut aussi créer un programme de formation agréé à l'échelle nationale pour remplacer ces praticiens à mesure qu'ils prennent leur retraite.
General practitioner–surgeons (GP-surgeons) provide important services to small rural Canadian communities, particularly in British Columbia, Northern Ontario and Alberta.1–5 With the centralization of health care delivery, the specialization of medical professionals and the lack of replacement rural surgical care providers, the sustainability of smaller rural surgical programs is threatened. Although the rural population growth rate is less than that in urban areas, it is still increasing. In 1991, 33% of Canadians lived in rural areas, with 22% living in communities of fewer than 10 000 people.6 In other words, 9 million Canadians were living in rural areas. Like the rest of Canada, British Columbia has and likely always will have a significant rural population.
As both general surgeons and GP-surgeons age and retire, there are few new graduates to replace them as rural surgical care providers.7,8 Those who remain are older, usually have a narrower scope of practice and focus primarily on cesarean sections.9,10 If elective surgical procedures continue to be centralized, the delivery of emergency surgery, including obstetric care and cesarean sections, becomes tenuous. With the growing trend toward centralization and the dwindling number of rural surgical care providers, there is a real threat that the current models of rural surgical delivery will slowly erode into a system that is unsustainable.
There are few published data describing British Columbia's current and past models of surgical service delivery, especially in communities that have no resident specialist surgeons.1,11,12 There are also few published data linking different models with their impact on local surgical service delivery. Communities with fewer than 15 000 residents cannot attract and maintain specialist surgeons and tend to rely heavily on GP-surgeons for both elective and emergency surgical procedures.7
This study documents previous and current models of rural surgical service delivery in communities that rely solely on GP-surgeons for the delivery of emergency surgical care. We clearly define the current models in these communities, including the training and age of GP-surgeons and some characteristics of the local surgical programs. We also illustrate the impact that different models of service delivery have on maternity and emergency care. This information will provide a more complete picture of rural surgical service delivery models and their impact on their communities and will allow both training institutions and health care policy-makers to make more informed decisions regarding rural surgical service delivery.
Methods
Communities selected had surgical services but no resident general surgeon. After ethics approval obtained through the University of British Columbia, we retrieved data from already published information available in the medical directories for British Columbia for the period 1996 to 2004. We also used the Population Utilization Rates and Referrals For Easy Comparative Tables (PURRFECT 6.0 and 9.0) database (www.hrabc.net/sites/hrdcl/files/Publications/MOHdatabasesandrptingJan2004.pdf) available from the BC Ministries of Health Planning and Health Services. Further, we used 2001 Statistics Canada Community Census Profiles to obtain an annual summary of all procedures provided locally. These procedures were separated into elective and emergency surgery, confirming the lack of resident specialist surgeons in the chosen communities and suggesting the presence and type of itinerant surgery or the absence thereof.
Phone interviews with the physician or nurse most responsible for each local surgical program confirmed information obtained through the medical directories and PURRFECT. As well, we determined the current state of each surgical service from the interviews, including the number of resident physicians performing surgical procedures and their age, experience, level of training and country of training.
Results
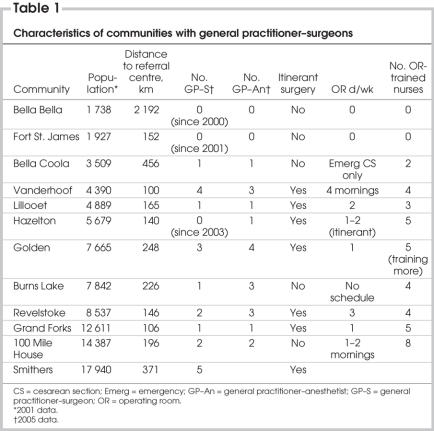
We identified 12 communities that had no resident general surgeon yet had offered local surgical procedures at some point since 1996. All communities are 100 km or more from referral centres with specialist surgeons. Table 1 defines their characteristics. Local surgical programs serve catchment areas with populations of 1738 to 17940, with a mean of 7593 and a median of 6672. Of the 12 communities, 9 had regular itinerant surgical services during our study period. General surgery, ear/nose/throat, orthopedic surgery, urology and obstetrics/gynecology were various types of itinerant surgery found. One of the communities had a resident orthopedic surgeon. Communities had a range of 1 to 5 GP-surgeons, with 2 or more casual nurses trained in operating room procedures; the GP-surgeons operated 1–4 days per week.
Table 1
Figure 1 allows the reader to visualize the proximity and size of the communities in relation to the referral centres as well as changes in delivery models since 1996. Models of delivery are divided into solo GP-surgeon, GP-surgeons (more than 1), GP-surgeon with itinerant specialist surgeon, and no local surgical program. Past models (1996, left of vertical line) and present models (2005, right of vertical line) are illustrated. Three of the 5 communities operating with a solo GP-surgeon in 1996 lost their surgical program. At the time of our study, 4 of the remaining programs operated with a solo GP-surgeon.
FIG. 1. Rural surgical services in British Columbia without resident specialist surgeons. Past models (1996, left of vertical line) and models at the time of study (2005, right of vertical line) are illustrated. GP = general practitioner.
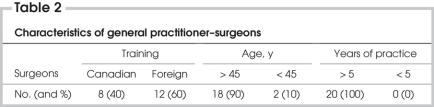
The 20 GP-surgeons working in these 12 communities at the time of our study are described in Table 2. Of these, 60% were foreign-trained and 40% Canadian-trained. Graduates trained in Canada and providers with less experience tended to focus more on cesarean sections and to offer a narrower scope of practice.13 All GP-surgeons had been practising for more than 5 years, and 90% were over the age of 45 years.
Table 2
Figure 2 illustrates referral patterns for appendectomies, linked to the number of GP-surgeons in the communities. In communities with more than 2 resident GP-surgeons, 30% of appendectomies were referred out, whereas 62% were referred out in communities with 1–2 resident GP-surgeons and 100% in communities that lost their resident GP-surgeon. A total of 347 appendectomies were performed at 9 of the 12 hospitals, an average of 8 per year per hospital.
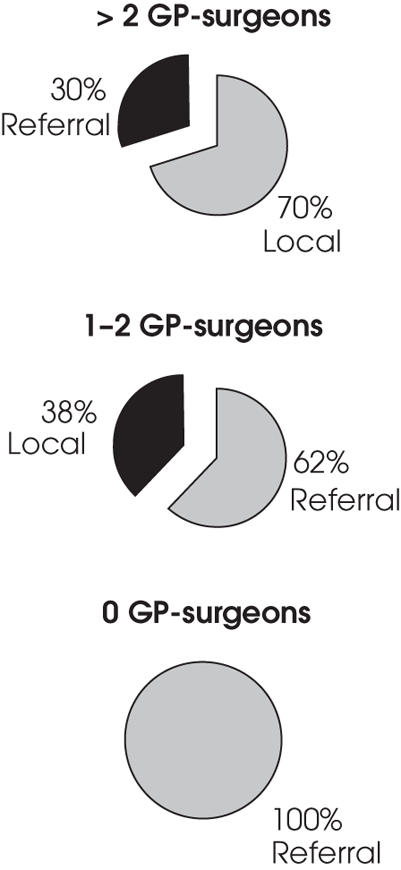
FIG. 2. Referral patterns for appendectomies, linked to the number of GP-surgeons in the communities. The dramatic effect of attrition and loss of surgical programs is evident. GP = general practitioner.
Figure 3 compares local obstetrical referral patterns according to different models of delivery. In a representative community with a single GP-surgeon, 47% of women were able to deliver locally, compared with 15% able to delivery locally in the 3 years after the program closed. The number able to deliver locally decreased until, at the time of our study, all cases were referred out. Although operative backup was available from 1996 to 2000, there were no cesarean sections performed. This compares to a local delivery rate of 78% (range 74%–83%) in a representative community with more than a single GP-surgeon and a continuous local surgical program. A total of 917 cesarean sections were performed at 11 of the 12 hospitals, an average of 17 per year per hospital.
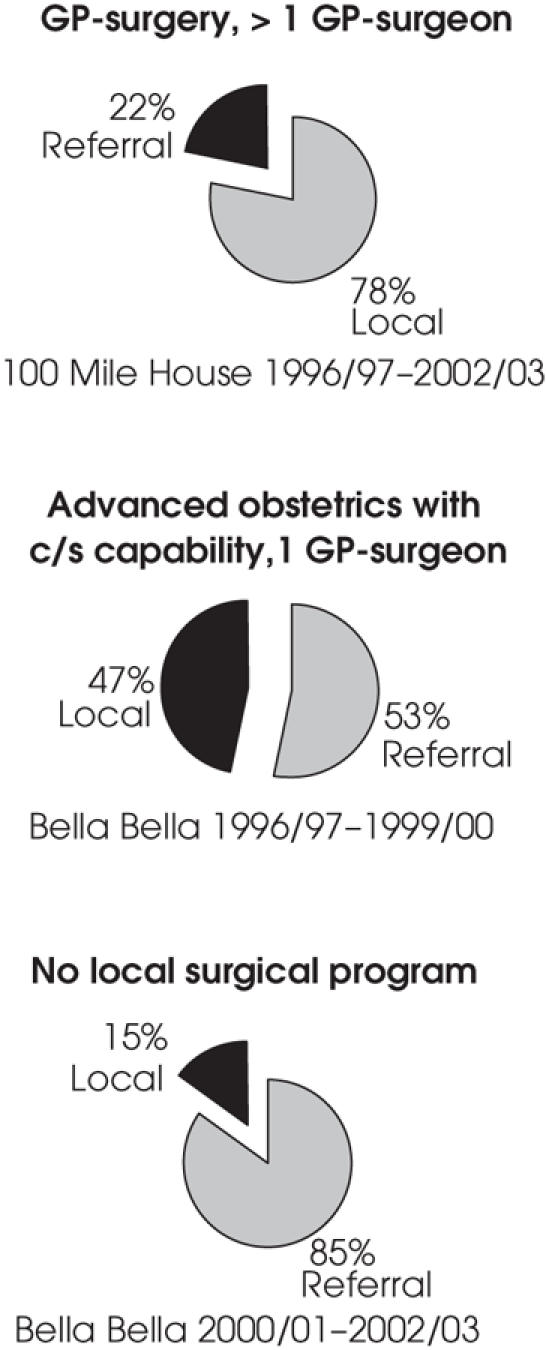
FIG. 3. Comparison of local obstetric referral patterns in representative communities, according to different models of delivery. c/s = cesarean section; GP = general practitioner.
Discussion
Despite surgical program closures and a decrease in the total number of rural GP-surgeons, the models of rural surgical service delivery have changed little since 1996. As in Table 1, surgical programs in communities with fewer than 15 000 residents still rely heavily on GP-surgeons. Itinerant surgery is still common; it includes general surgery, ear/nose/ throat surgery, orthopedic surgery, urology and obstetrics/gynecology. None of these communities have the population base to support a specialist general surgeon, and all are 100 km or more from a referral centre with specialist surgeons.
Communities that wish to consistently provide full-service maternity care to 85%–90% of women but are more than 100 km from a referral centre need to maintain a local surgical program.14,15 The local surgical program in these hospitals tends to function as a stabilizing factor on delivery of local acute care and maternity care.16,17 Offering services for day care and inpatient surgical patients allows local health care providers to obtain more experience in caring for other acutely ill patients. This comfort level also transfers to the emergency department, where stabilization of life-threatening illness, procedural sedation, cardioversion and more complex procedures use collateral surgical skills. Overall, the local presence of a surgical program stabilizes the delivery of emergency medicine, maternity care and acute care, along with the recruitment and retention of health care staff.18
The role of itinerant surgery is also important. The strong presence of this in many communities is likely a result of the increased specialization of surgical skills and equipment, with fewer older and foreign-trained GP-surgeons having been trained in laparoscopy, arthroscopy, endoscopy and cystoscopy. Many itinerant surgeons also bring equipment with them from the referral centres. The relationship between small communities and itinerant specialists from referral centres is different in every community. Some programs receive continuing education and training from itinerant surgeons. Others are based purely on unique community demands or reductions in specialist-surgeon operating room time at referral centres. Some itinerant programs survive because of the willingness of a surgeon to visit and operate in a smaller community regardless of personal financial impact. Others continue because of prior relationships formed between local physicians and visiting specialists.
Figure 1, which compares 1996 and 2005 delivery models, demonstrates that all the communities that lost their local surgical program had a solo GP-surgeon and fewer than 4000 residents. It is interesting that, of the 12 original communities, 7 either lost their program completely or operated with a solo GP-surgeon. Three programs closed owing to loss of either the GP-surgeon or the GP-anesthetist. At the time of our study, no communities that lost their surgical program later reinstated it. Once programs are closed, they are difficult to reinstate due to changes in local referral patterns, loss of confidence among community residents, loss of associated surgical staff and the difficulties of reversing the cascade effect on local health care. Because rural surgical services are more costly to health regions, there has been little administrative and financial support to sustain these models.
As Table 2 suggests, many GP-surgeons are foreign-trained, have more than 5 years of experience and are over 45 years of age. This fits with other data that emphasize the loss of Canadian-trained rural generalists and the lack of new replacements.1,2 The statistics also agree with Australian GP-surgeon data depicting the slow attrition of GP-surgeons in New South Wales.19 Notably, in the Australian study, 87% of GP-surgeons stated that they decided to continue practising in their communities because they had the opportunity to pursue their surgical skills and that, without this, they would relocate to communities where their skills could be used.19 With no formalized training program in Canada, there is little hope that new Canadian graduates will replace GP-surgeons as they retire.20,21 The strong South African recruitment pool has been less successful in recent years, and many question the ethics of recruiting so strongly from other countries.22 Canadian programs are still unstructured and focus mostly on advanced obstetrical skills with an operative component. As noted, local surgical programs help stabilize local maternity programs; however, in many communities a local maternity program does not generate enough surgical volume to make a local surgical program sustainable.
Figure 2 shows the dramatic effect that attrition and loss of surgical programs has on local community referral patterns. Likely, for every appendectomy patient, there are 3 or 4 more that were sent for assessment to a referral centre, observed and later discharged. When one considers the cost borne to the patient regarding time lost from work, time lost from work of accompanying family or friends, transportation costs, the stressors of being cared for at a larger centre without health care professionals that the patient knows or trusts, the lack of culturally sensitive care at larger centres, the disruption to family life and the costs associated with accommodation and meals away from home, the impact is more significant. The impact on maternity services has been alluded to before and behaves in a similar fashion, as shown in Figure 3. The loss of an operative program, especially in communities that have depended on these models of care, is significant.3,23–26 All the above-mentioned stressors are even more apparent because the mother is usually the cohesive factor in the home.
Although our study only focused on communities with no resident general surgeon, there are a few communities where GP-surgeons and general surgeons coexist. In these communities, the GP-surgeons tend to perform only complicated obstetrical procedures and cesarean sections, whereas general surgeons perform all the general surgical procedures, with or without cesarean sections. This model has the potential to stabilize communities with fewer than 3 general surgeons who wish to share or opt out of obstetrical call.27
Conclusions
Despite over a decade of concerns regarding the delivery of rural surgical services, since 1996 there has been a 25% reduction in the number of programs focused on GP-surgeons. Although they are aging and have less Canadian training and a narrower scope of practice, GP-surgeons still play a role at these sites. There is a negative impact on both maternity and acute surgical services in communities with a single local GP-surgeon or less. There needs to be better outcome analysis comparing general surgeons and GP-surgeons, as well as a nationally accredited training program to replace GP-surgeons who service these communities before the delivery of rural surgical services is irreversibly eroded.
Acknowledgments
Grant funding generously provided by the Vancouver Foundation.
Contributors: Dr. Humber and Ms. Frecker both designed the study, acquired and analyzed data, wrote the article and gave final consent for its publication. Dr. Humber alone reviewed the written article.
Competing interests: None declared.
Accepted for publication Nov. 24, 2006
Correspondence to: Dr. N. Humber, Lillooet Medical Clinic, Box 850, Lillooet BC V0K 1V0; Saffron2@telus.net
References
- 1.Chiasson PM, Roy P. Role of the general practitioners in the delivery of surgical and anesthesia services in rural western Canada. CMAJ 1995;153:1447-52. [PMC free article] [PubMed]
- 2.Iglesias S. Advanced skills by Canada's rural physicians. Can J Rural Med 1999;4:227-31.
- 3.Heaton P. Surgical care in small Alberta communities. Can Fam Physician 1983;29:1591-601. [PMC free article] [PubMed]
- 4.Roos N, Black C, Wade J, et al. How many general surgeons do you need in rural areas? Three approaches to physician's resource planning in southern Manitoba. CMAJ 1996;155:395-401. [PMC free article] [PubMed]
- 5.Roos LL Jr. Supply, workload and utilization: a population-based analysis of surgery in rural Manitoba. Am J Public Health 1983;73:414-21. [DOI] [PMC free article] [PubMed]
- 6.Statistics Canada. Population and dwelling counts for urban areas. Ottawa: Statistics Canada; 1992.
- 7.Blair L. Are general surgeons a dying breed? CMAJ 1991;145:46-8. [PMC free article] [PubMed]
- 8.Inglis FG. Surgical care in rural Canada: training and planning for the future. CMAJ 1995;153:1453-4. [PMC free article] [PubMed]
- 9.Rourke JT. Trends in small hospital obstetric services in Ontario. Can Fam Physician 1998;44:2117-24. [PMC free article] [PubMed]
- 10.Henderson N, Grzybowski S, Thommasen C, et al. Procedural skills practised by British Columbia family physicians. Can J Rural Med 2001;6:179-85.
- 11.Iglesias S. Rural surgical programs in Western Canada. Can J Rural Med 2002;7:103-7.
- 12.Brown JS, Smith R, Cantor J, et al. General practitioners as providers of minor surgery — A success story? Br J Gen Pract 1997;47:205-10. [PMC free article] [PubMed]
- 13.Humber N. Rural surgery in British Columbia: Is there anybody out there? Can J Surg 2008;51:179-84. [PMC free article] [PubMed]
- 14.Kreibel SH, Pitts J. Obstetrical outcomes in rural family practice: an 8-year experience. J Fam Pract 1988;27:377-8. [PubMed]
- 15.Lynch N, Thommasen H, Anderson N, et al. Does caesarean section capability make a difference to a small rural maternity service? Can Fam Physician 2005;51:1238-9. [PMC free article] [PubMed]
- 16.Guard MC. Management of obstetric complication s at small rural hospitals [letter]. CMAJ 1979;120:919. [PMC free article] [PubMed]
- 17.Walker DE. The obstetrical crisis facing Ontario hospitals. CMAJ 1993;149:1541-5. [PMC free article] [PubMed]
- 18.Klein MC, Christilaw J, Johnston S. Loss of maternity care: the cascade of unforeseen dangers. Can J Rural Med 2002;7:120-1.
- 19.Dunbadin J. Procedural medicine in rural and remote NSW [discussion paper]. Newcastle (Australia): NSW Rural Doctors Network; 2002. Available: www.nswrdn.com.au/site/content.cfm?document_id=411605¤t_page_category_code=92&did=50442345&dmodule=DIGITALASSETS (accessed 2008 Apr 21).
- 20.Gutkin C, Rainsberry P. Innovative new program: enhanced skills for family practice. Can J Rural Med 2002;7:77-8.
- 21.Chang J. Third year family medicine programs. Can Fam Physician 2001;47:1438-40.
- 22.Barer ML, Stoddart GL. Improving access to needed medical services in rural and remote Canadian communities: recruitment and retention revisited [discussion paper]. Vancouver: Centre for Health Services and Policy Research; 1999. Available: www.chspr.ubc.ca/files/publications/1999/hhru99-05.pdf (accessed 2008 Apr 21).
- 23.Black DP, Fyfe I. The safety to obstetric services in small communities in Northern Ontario. CMAJ 1984;130:571-6. [PMC free article] [PubMed]
- 24.Nesbitt TS, Connell FA, Hart LG, et al. Access to obstetric care in rural areas: effect on birth outcomes. Am J Public Health 1990;80:814-8. [DOI] [PMC free article] [PubMed]
- 25.Nesbitt TS, Larson EH, Rosenblatt RA, et al. Access to maternity care in rural Washington: its effect on neonatal outcomes and resource use. Am J Public Health 1997;87:85-90. [DOI] [PMC free article] [PubMed]
- 26.Rosenblatt RA, MacFarlane A, Dawson AJ, et al. The regionalization of perinatal care in Wales and Washington State. Am J Public Health 1996;86:1011-5. [DOI] [PMC free article] [PubMed]
- 27.Coopers and Lybrand Associated. The cost effectiveness of general practice. A General Medical Services Committee [discussion document]. London: British Medical Association; 1983.