Bone wax is widely used in various surgical specialties to control bleeding from bone surfaces. Surgeons should be aware of possible related complications. We report a case in which foreign-body reaction to bone wax applied over femoral neck osteoplasty required reoperation.
Case report
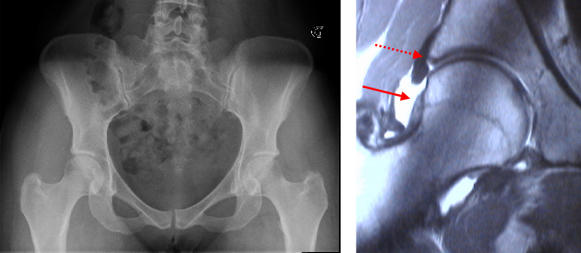
A 37-year-old woman presented with sharp pain in the right hip that had been present for 3 years; the pain was localized to the groin. She also had episodes of “catching” in the hip joint. Conservative treatment had been tried but without success. On examination, there was an antalgic limp, a positive impingement sign and a reduction in internal rotation. Radiographs did not show any hip joint disease, but magnetic resonance imaging demonstrated a torn anterior labrum with an abnormal osseous bump at the junction of the femoral head and neck, confirming the diagnosis of femoroacetabular impingement (Fig. 1).
FIG. 1. Anteroposterior pelvic radiograph (left) with right hip joint showing no apparent abnormalities. Preoperative gadolinium-enhanced MRI of the right hip (right) showing contrast material at the base of the labrum, suggesting a labral tear (dotted red arrow), and an abnormal osseous bump at the femoral head and neck junction (plain red arrow) responsible for the repetitive abutment of the femoral neck on the anterior acetabular labrum during hip motion.
The hip joint was explored surgically through a digastric trochanteric flip approach. The lesion of the anterior labrum was confirmed, and contact between the anterolateral femoral neck and the labrum was observed on motion. The labrum was stable, but a partial horizontal detachment of the labrum at its junction with the anterior acetabular cartilage was debrided because refixation was not possible, and an anterior femoral neck osteoplasty was performed with an osteotome to give a normal neck contour. Cancellous bleeding from the anterior femoral neck was controlled by applying bone wax (Ethicon, Johnson and Johnson, Somerville, NJ). The bleeding area from cancellous bone of the anterior femoral neck measured about 3.5 cm2. One gram of bone wax was firmly pressed onto this area until bleeding stopped, and the excess (about 0.5 g) was removed.
Six weeks after surgery, the patient had a pain-free hip with improved internal rotation. She returned to work 3 months postoperatively. Six months postoperatively, she presented because of the reappearance of pain and stiffness of the hip joint. The hip was irritable with minimal motion. Infection was ruled out: there was negative growth from culture of a hip joint aspirate, C-reactive protein level was 5.4 (normal, < 8) mg/L and erythrocyte sedimentation rate was 7 (normal < 20) mm/h. A new magnetic resonance image showed an abnormal signal in the anterior labrum, suggesting a new or persistent tear (Fig. 2). Hip injection with local anesthetic and steroid relieved the pain, but only for 4 weeks. The hip joint was reexplored and dislocated with open surgery through a digastric trochanteric flip approach instead of hip arthroscopy because labrum fixation was planned; however, the labrum was found to be healed to the acetabular bony rim and stable. A thin layer of tissue was found on the anterior femoral neck where the bone wax had been applied during the previous surgery. Neovascularization with multiple small vessels was observed within this tissue. All this tissue was removed by curettage and sent for histologic examination. No bone wax was applied, and no other treatment was used apart from bone-wax removal. No progression of joint disease could be identified, and intraoperative motion of the hip joint confirmed the absence of persisting impingement. No evidence of new bone formation was identified on imaging studies and intraoperatively.

FIG. 2. Postoperative arthro-magnetic resonance image showing possible persistent labral tear (dotted red arrow), without evidence of granulomatous tissue on the remodelled femoral neck after the osteoplasty (plain red arrow).
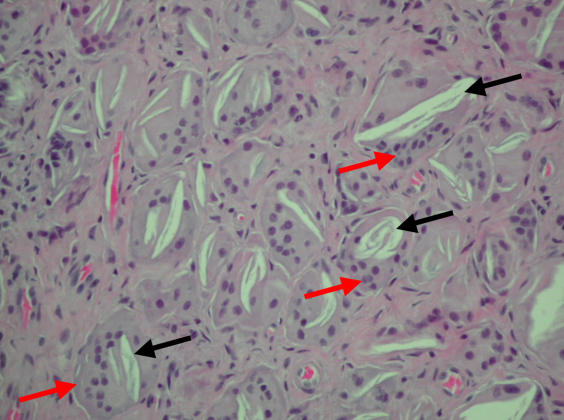
Histologic examination showed foreign-body granulomatous reaction consisting of multinucleated giant cells surrounding wax particles interspersed with abundant mononuclear cells (Fig. 3). After this operation, the patient returned to her previous activity without symptoms, thus supporting bone-wax granuloma as the cause of her second admission.
FIG. 3. Photomicrograph of tissue removed from the femoral neck osteoplasty site. Foreign-body granulomatous reaction consisting of multinucleated giant cells (red arrows) engulfing wax particles (black arrows) can be seen with surrounding mononuclear cells (hematoxylin–eosin stain; original magnification ×200).
Discussion
Since their development in 1886 by Horsley,1 bone-wax formulations have not changed much. Bone wax contains beeswax softened with isopropyl palmitate or paraffin. Bone wax controls bone bleeding mechanically by occluding the bleeding channels and tamponading the spaces in bone. It has no biochemical action and is nonabsorbable. Several adverse effects have been reported with bone wax.2 It is known to interfere with bone healing and osteogenesis. It has been shown to reduce bacterial clearance in cancellous bone and to increase the risk of infection. Bone wax applied on a sternotomy may even embolize to lungs, with clinical consequences.
Foreign-body granulomatous reaction due to bone wax has been reported in various surgical sites with different clinical implications, requiring surgical exploration in some cases.2 Bone-wax granulomas have been reported at sternotomy sites (with one case leading to saphenous vein thrombosis), in orbits, in cranial defects, after tibial tubercle elevation surgery, after foot surgery, in mastoid (with one case resulting in sigmoid sinus thrombosis), at the cerebellopontine angle and in the subarachnoid space near the medulla oblongata. In one instance, in which bone wax had been used to stop bleeding from the iliac crest after the harvesting of autogenous graft, the patient presented 19 years later with a large, symptomatic, retroperitoneal tumour associated with a foreign-body reaction, which had to be removed operatively.3
Other hemostatic agents such as gelatine foam (Gelfoam; Pharmacia & Upjohn, Kalamazoo, Mich.), oxidized cellulose (Surgicel; Ethicon) and microfibrillar collagen (Avitene; C.R. Bard, Murray Hill, NJ) are absorbable, less prone to tissue reaction, do not interfere with bone healing and have platelet-stimulating effects.2 Unlike bone wax, however, because of their physical properties, they are not ideal to seal the bleeding cancellous surfaces. A composite of polyethylene glycol and microfibrillar collagen has shown promising results.4 Recently, a powder form of gelatine (Surgifoam; Ethicon) has been introduced; it forms a paste that can be spread to conform to bone surfaces better than bone wax.5 An alkylene oxide copolymer (Ostene; Ceremed, Los Angeles, Calif.) has been introduced that has physical properties similar to those of bone wax.6 This material is water-soluble, dissolves in 48 hours, elicits minimal tissue response and acts by mechanical effect alone. We have no experience with these alternatives.
Such materials may be tissue-friendly alternatives to traditional bone wax. Nevertheless, when necessary, bone wax should be used just for the time needed to achieve hemostasis. If it is left in place, meticulous removal of excess is strongly recommended. We have stopped using this material after femoral neck osteoplasty because bleeding is minimal and capsular adhesion can now be avoided with more aggressive postoperative rehabilitation. When significant bleeding from a bone surface occurs, we use bone wax temporarily during the procedure, remove it before closure and leave a suction drain in place to avoid hematoma formation. Awareness of potential complications is essential if a surgeon is to deal with them successfully.
Competing interests: None declared.
Accepted for publication July 10, 2007
Correspondence to: Dr. M. Lavigne, Maisonneuve-Rosemont Hospital, 5345, boul de l'Assomption, Ste. 55, Montréal QC H1T 4B3; fax 514 254-1596; lavigma2@hotmail.com
References
- 1.Tan TC, Black PM. Sir Victor Horsley (1857–1916): pioneer of neurological surgery. Neurosurgery 2002;50:607-11; discussion 611-2. [DOI] [PubMed]
- 2.Schonauer C, Tessitore E, Barbagallo G, et al. The use of local agents: bone wax, gelatin, collagen, oxidized cellulose. Eur Spine J 2004;13(Suppl 1):S89-96. [DOI] [PMC free article] [PubMed]
- 3.Verborgt O, Verellen K, Van Thielen F, et al. A retroperitoneal tumor as a late complication of the use of bone wax. Acta Orthop Belg 2000;66:389-91. [PubMed]
- 4.Orgill DP, Ehret FW, Regan JF, et al. Polyethylene glycol/microfibrillar collagen composite as a new resorbable hemostatic bone wax. J Biomed Mater Res 1998;39: 358-63. [DOI] [PubMed]
- 5.Sabel M, Stummer W. The use of local agents: Surgicel and Surgifoam. Eur Spine J 2004;13(Suppl 1):S97-101. [DOI] [PMC free article] [PubMed]
- 6.Wellisz T, Armstrong JK, Cambridge J, et al. Ostene, a new water-soluble bone hemostasis agent. J Craniofac Surg 2006; 17:420-5. [DOI] [PubMed]