Abstract
Objective
To document surgical procedures performed in British Columbia between 1996 and 2001 at rural hospital sites with no resident specialist surgeons and to define the scope of practice of general practitioner (GP)–surgeons at these small-volume surgical sites.
Methods
We obtained data from published information available in the medical directories for British Columbia and from the Population Utilization Rates and Referrals For Easy Comparative Tables database (versions 6.0 and 9.0) to conduct a retrospective study of all rural BC hospitals with surgical programs that had no resident specialist surgeon and relied on GP-surgeons for emergency surgical care between 1996 and 2001. We studied surgical programs at the 12 hospitals that met inclusion criteria and interviewed the physician or nurse responsible for the program. Outcomes were measured in terms of the types and volumes of surgical procedures (elective and emergency) from 1996 to 2001, including itinerant surgery.
Results
On average, 2690 surgical procedures were performed annually at the 12 hospitals included in the study. Endoscopy, hand surgery, cesarean section, herniorrhaphy, tonsillectomy and dilation and curettage (D&C) were among the top elective and emergency procedures. For each hospital, between 8 and 26 procedures of hand surgery, cesarean section, herniorrhaphy, D&C and appendectomy were performed each year. In the 12 communities studied, 19% of all surgery was emergency and 81% elective. There was significant overlap in the types of emergency and elective procedures. GP-surgeons carried out most of the emergency procedures, which nonetheless accounted for a small portion of their surgical work.
Conclusion
GP-surgeons still perform a significant number of emergency and elective surgical procedures in rural BC hospitals. This study defines useful procedures for GP-surgeons in communities without the population base to sustain a resident specialist surgeon. This information can be used to structure training programs for GP-surgeons that will adequately meet the needs of rural communities.
Abstract
Objectif
Documenter les interventions chirurgicales pratiquées en Colombie-Britannique entre 1996 et 2001 dans des hôpitaux ruraux sans chirurgien spécialiste en résidence et définir le champ d'exercice des omnipraticiens (OP)-chirurgiens de ces établissements chirurgicaux à faible volume.
Méthodes
Nous avons extrait les données des répertoires médicaux publiés en Colombie-Britannique et de la base de données Population Utilization Rates and Referrals For Easy Comparative Tables (taux d'utilisation et références à utiliser pour établir facilement des tableaux comparatifs), versions 6.0 et 9.0, afin d'effectuer une étude rétrospective portant sur tous les hôpitaux ruraux de la C. B. dotées d'un programme chirurgical, n'ayant pas de chirurgien spécialiste en résidence et comptant sur des OP-chirurgiens pour dispenser des soins chirurgicaux d'urgence entre 1996 et 2001. Nous avons étudié les programmes chirurgicaux des 12 hôpitaux satisfaisant aux critères d'inclusion et interviewé le médecin ou l'infirmière responsable du programme. Nous avons mesuré les résultats en fonction des types et des volumes des interventions chirurgicales (électives et d'urgence) de 1996 à 2001, y compris les services de chirurgie itinérants.
Résultats
En moyenne, 2690 interventions chirurgicales ont été pratiquées par année dans les 12 hôpitaux inclus dans l'étude. L'endoscopie, la chirurgie de la main, la césarienne, l'herniorrhaphie, l'amygdalectomie et la dilatation et curetage (D et C) étaient au nombre des principales interventions électives et d'urgence. Dans chaque hôpital, on a pratiqué chaque année de 8 à 26 chirurgies de la main, césariennes, herniorrhaphies, D et C et appendicectomies. Dans les 12 communautés étudiées, 19 % des interventions chirurgicales étaient urgentes et 81 % étaient électives. Il y avait un chevauchement important au niveau des types d'interventions d'urgence et électives. Les OP-chirurgiens ont pratiqué la plupart des interventions d'urgence qui ont représenté néanmoins un faible pourcentage de leur travail en chirurgie.
Conclusion
Les OP-chirurgiens pratiquent toujours un nombre important d'interventions chirurgicales d'urgence et électives dans les hôpitaux ruraux de la C. B. Cette étude définit les interventions utiles pour les OP-chirurgiens dans les communautés dont le bassin de population est insuffisant pour faire vivre un chirurgien spécialiste en résidence. Ces renseignements pourront servir à structurer des programmes de formation d'OP-chirurgiens qui répondront adéquatement aux besoins des communautés rurales.
The delivery of surgical services at rural hospitals without resident specialist surgeons has changed greatly over the past decade. It has been influenced by technology, training programs for physicians and other health care professionals, available equipment, itinerant surgery, manpower distribution and the centralization of many elective and daycare surgical procedures. Communities that rely heavily on general practitioner (GP)–surgeons for their local care are greatly affected by these changes.1
Communities with fewer than the 15000 residents necessary to attract and maintain a specialist surgeon2,3 usually rely on GP-surgeons to deliver emergency surgical care and some degree of elective surgical care.4–8 A reliable, sustainable maternity care program depends on this continuous emergency component.9 Elective programs often evolve to meet the needs of the community. The continuation of an elective component is necessary to maintain enough surgical volume to sustain all local surgical team members. Although itinerant surgery addresses some of the barriers to access facing rural residents, it cannot be the only response to rural surgical care delivery because it lessens the volume and scope of programs for local GP-surgeons.
In general, health care policy-makers know little about what goes on at smaller community hospitals, particularly those that rely on GP-surgeons. Similarly, many other health care professionals know little about the scope of practice of GP-surgeons and the volume and variety of surgery that is performed outside of specialist-dependent centres. This is likely owing to the lack of published data describing the scope of practice at these sites and how it has changed over the past decade, as well as the volume of surgery currently performed at rural hospitals without resident specialist surgeons. Many surgical and maternity care delivery decisions continue to be made without accurate knowledge of the volumes, types of and differences between emergency and elective surgical programs or of their importance in the community.
GP-surgeons offer low-risk surgical patients local access to a broad base of low-risk surgical procedures. Our study describes the scope of practice of GP-surgeons and how it has changed from 1996 to 2001 for the 12 surgical programs in rural British Columbia that lack resident specialist surgeons. We list the most common surgical procedures at the 12 hospitals, which include 3 hospitals without itinerant surgery. We also examine case numbers per hospital per year for 5 common procedures and define a possible skill set for GP-surgeons. This information will help to guide the modelling of rural surgical care delivery and to define a possible skill set for GP-surgeons in communities unable to support a fellowship general surgeon.
Methods
Communities selected had surgical services but no resident general surgeon. After ethics approval obtained through the University of British Columbia, we retrieved data from published information available in the medical directories for British Columbia for the period 1996 to 2004. We also used the Population Utilization Rates and Referrals For Easy Comparative Tables (PURRFECT 6.0 and 9.0) database (www.hrabc.net/sites/hrdc1/files/Publications/MOHdatabasesandrptingJan2004.pdf) available from the BC Ministries of Health Planning and Health Services. Further, we used 2001 Statistics Canada Community Census data to obtain an annual summary of all procedures offered locally (separated into elective and emergency surgery) as well as some community characteristics. These data confirmed the lack of resident specialist surgeons in the chosen communities and suggested the presence and type of itinerant surgery or the absence thereof. Phone interviews with the physician or nurse most responsible for each local surgical program confirmed any unusual information obtained through the medical diiectories or PURRFECT, as well as local surgical program characteristics.
We excluded diagnostic and other surgical procedures not requiring advanced training. Operative procedures encompassing similar skill sets were grouped together. After separation into elective and emergency procedures, results were analyzed by year, community size and delivery models. Frequencies, ranges, means and averages were used to compare procedures.
Results
The 12 communities included have between 1700 and 17 000 residents and are 100 km or more from a referral centre. Most of the GP-surgeons in these communities are older and foreign-trained and have more than 5 years of experience. None of the GP-surgeons described in this study are foreign-trained specialist surgeons.
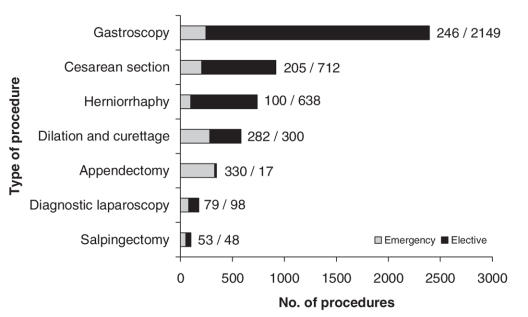
Figure 1 shows the total number of procedures per year for all 12 hospitals. The range is 2607–2768 with a mean of 2690 and a median of 2687. In both 1996–1997 and 2000–2001, there were 133 different types of procedures. Three local surgical programs closed during the study period. None were reinstated.
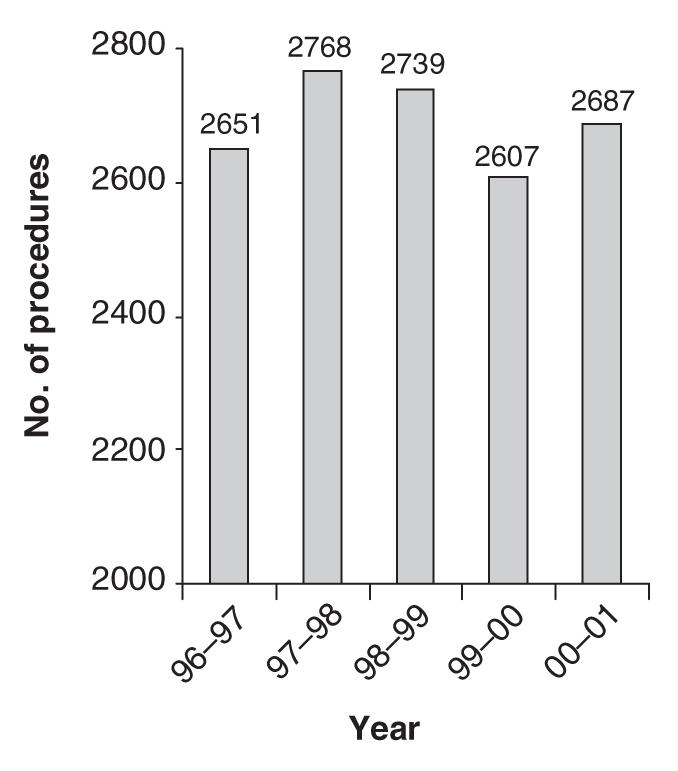
FIG. 1. Annual surgical volumes 1996–2001, all sites.
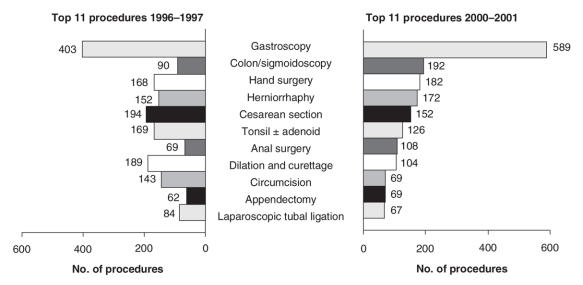
Figure 2 compares the frequency of the top 11 surgical procedures at all sites for 1996–1997 and 2000–2001. There was a significant increase in gastrocopy (46%) and also in colonoscopy or sigmoidoscopy (113%). When all these endoscopic procedures are combined, they total 493 in 1996–1997 and 781 in 2000–2001, a 58% increase. Meanwhile, other procedures decreased as follows: dilation and curettage (D&C) by 45%, cesarean section by 22% and complicated obstetric operations (not shown in Fig. 2) by 58%. Between 7 and 12 sites performed each of the top 10 surgical procedures. D&C included operative removal of placenta. Data on therapeutic abortions were not available.
FIG. 2. Top 11 procedures 1996–1997 and 2000–2001, all sites.
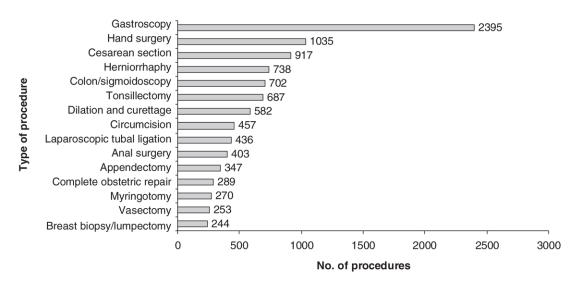
Figure 3 depicts the total number of cases for the top 15 procedures in all hospitals over all years. Gastroscopy, hand surgery (e.g., carpal tunnel release and ganglionectomy) and cesarean section are the top 3. Appendectomy and vasectomy are still present in significant numbers (347 and 253, respectively).
FIG. 3. Top 15 procedures (emergency and elective), all sites.
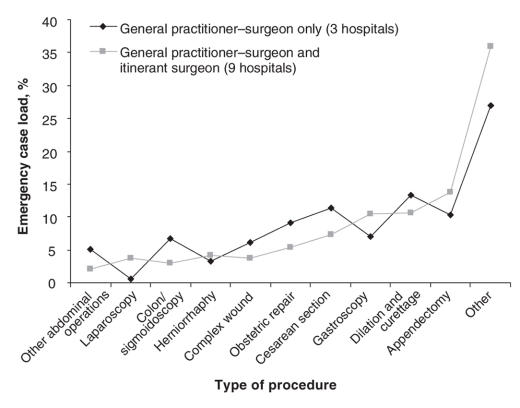
Figure 4 compares the distribution of the emergency case load for hospitals with and without itinerant surgery. Both data sets are similar, with the exception of laparoscopy.
FIG. 4. Comparison of distribution of the emergency case load with and without itinerant surgery.
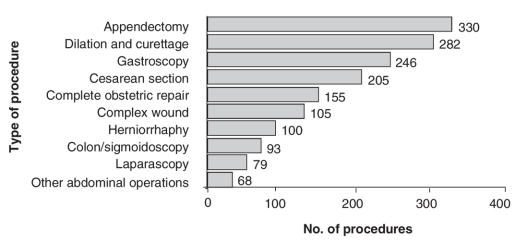
Figure 5 shows the top 10 emergency procedures for all hospitals. Appendectomy and cesarean section are among the top 5, with laparoscopy and herniorrhaphy among the top 10. Laparoscopy usually consisted of laparoscopic tubal ligations and diagnostic laparoscopy. Herniorrhaphy includes all types of hernia repair (e.g., ventral, incisional, recurrent, inguinal). Most of the emergency procedures are also common elective procedures.
FIG. 5. Top 10 emergency procedures, all sites.
Table 1 shows yearly surgical volumes per hospital for 5 procedures (hand surgeries, cesarean sections, herniorrhaphies, D&Cs and appendectomies). Most hospitals in the study performed each procedure, and where a procedure was performed, between 8 and 26 were performed annually. Cesarean section, herniorrhaphy and D&C were performed at 11 of the 12 sites.
Table 1
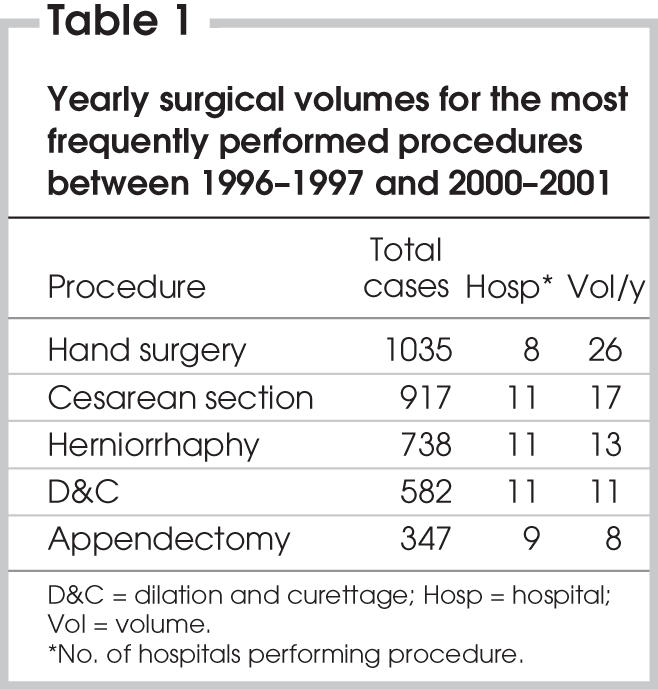
Figure 6 represents the proportion of elective and emergency procedures performed by GP-surgeons for 7 common procedures. Overall, 19% of the surgeries at the 12 sites were emergencies, compared with 81% elective surgeries. Even among the 7 procedures in Figure 6, only 25% are emergency cases. Cesarean sections represent 22% of the emergency surgeries and 78% of the elective surgeries.
FIG. 6. Elective and emergency procedures compared.
Discussion
The surgical volumes at all sites vary little over the years. Despite the loss of 3 smaller surgical programs during the course of the study, combined volumes remain over 2600 procedures per year. This is likely due to a combination of low volumes at sites that lost their surgical program and increased surgical volumes at other sites. Three local programs closed owing to the loss of either GP-surgeon or GP-anesthetist. None of these have been reinstated to date.
The top 11 procedures changed in rank but not commonality over the time period of the study (Fig. 2), with the exception of appendectomy, which ranked 10th in 2000–2001 and 14th in 1996–1997. The remarkable increase in endoscopy and decrease in D&C and other obstetrical operations reflect a shift in technology and trends in the surgical management of related illnesses.
The top 15 procedures (Fig. 3) show appendectomy, complicated obstetrical repair and vasectomy ranked 11th, 12th and 14th. Endoscopy, hand surgery, cesarean sections, herniorrhaphy, tonsillectomy and D&C are the top 7 procedures. This agrees with previously published Canadian data4 as well as with some Australian data suggesting that endoscopy, appendectomy, tubal ligation, hand surgery, herniorrhaphy, tonsillectomy and vasectomy are among the top 10 most frequent procedures.10
Figure 4 compares the distribution of emergency case loads for hospitals with and without itinerant surgery. The only significant difference occurs with laparoscopy, likely because of the cost and lack of equipment at smaller sites or the lack of laparoscopy training in foreign-trained and older GP-surgeons. This suggests that the top 10 emergency procedures in Figure 5 accurately represent the emergency procedure set offered by local programs regardless of the presence of visiting specialists. The emergency skill set overlaps almost completely with the elective skill set.
Although emergency procedures represent a small percentage of the local work, as shown in Figure 6, there are still significant numbers performed. Emergency and elective surgical programs are inextricably linked. Most would agree that it is not desirable to operate only on the sickest emergency patients. It is surgery on stable patients and procedures with collateral surgical skills that stabilize a skill set. A consistent elective surgical program alleviates some of the issues affecting staffing, community expectations, equipment, supplies and up-to-date education for all members.11
We know that a local emergency operative program also has an impact on the local maternity care program. Between 85% and 90% of women are able to deliver locally with operative backup12 (also, Dr. Stefan Grzybowski, BC Rural and Remote Health Research Network and University of British Columbia, Vancouver, BC: personal communication, 2004), whereas only 60% are able to do this in communities without a local surgical program.13
As Table 1 shows, each hospital still performs significant annual numbers of common procedures. Although many of the procedures occur at a rate of 8–13 per year, consider that, in practice, patients make on average 2–3 visits to the referral centre for investigations, follow-up examinations and surgical bookings for every referred elective procedure. Local access to surgical care helps many patients avoid multiple appointments out of town for nonoperative assessments, a factor not captured in these data.
For both elective and emergency surgery, rural patients experience many barriers to care that their urban counterparts do not face. There are many costs to consider: time lost from work, travel difficulties that worsen without local public transportation, ambulance rides, the risks and stress of travel in bad weather, accommodation and meal expenses and disruption to the family.14 These impacts are borne almost entirely by the patient and family. In addition to this, the marginalization of elderly and First Nations people and those of low socioeconomic status makes surgical care even less accessible. Existing studies already document patients' preferences for both maternity and surgical care performed by providers they know and trust; this is particularly true with maternity care.15 There are also studies suggesting that outcomes for local maternity care and local operative maternity programs are equal to or better than those in larger centres.1,13,16,17
With newly trained specialist surgeons unlikely to relocate to communities without computed tomography scan capabilities or an adequate population base,2,3 GP-surgeons could potentially continue to service these local programs with a defined skill set including cesarean section, circumcision, tonsillectomy, breast biopsies, hand surgery, vasectomy, diagnostic laparoscopy and tubal ligation, gastrointestinal endoscopy, complicated wound management (e.g., skin graft, Z-plasty), circumcision, D&C, appendectomy, herniorrhaphy and anal surgery. These agree with procedures usually performed by GP-surgeons in the rural communities of other countries.10,18 The consistency in types of procedures performed helps to define a skill set that can be useful in communities without the population base to support a resident general surgeon.
There are some outcome studies comparing GP-surgeons and general surgeons in regard to appendectomies19–21 and cesarean sections22; however, more information comparing outcomes between GP-surgeons and general surgeons is needed. The data in our study are limited in that the summaries of all surgical procedures performed locally do not differentiate between GPs and general surgeons as operators. Further study delineating itinerant specialist surgery and local GP-surgery would more accurately reflect the scope of practice and enable an outcome analysis comparing surgical procedures performed by GP-surgeons and those performed by specialist surgeons.
Conclusions
There is still a significant variety and volume of surgical procedures performed in rural BC communities with no resident specialist surgeon. The presence of a local elective surgical program is necessary in many places to allow both an emergency program and operative obstetrical program to continue. Traditionally offered by GP-surgeons, cesarean section, circumcision, tonsillectomy, breast biopsies, hand surgery, vasectomy, diagnostic laparoscopy and tubal ligation, gastrointestinal endoscopy, complicated wound management, circumcision, D&C, appendectomy, herniorrhaphy and anal surgery define a skill set that could be useful in smaller isolated communities. It is unlikely that fellowship-trained general surgeons will be interested in limiting their training to these procedures. With no nationally accredited training program for enhanced surgical skills, there are few Canadian and a dwindling pool of foreign physicians to replace GP-surgeons. Analysis of procedure outcomes and a nationally accredited training program to produce graduates to serve smaller, isolated communities is needed before the programs dwindle and disappear.
Acknowledgments
Funding was received from the Vancouver Foundation.
Contributors: Dr. Humber and Ms. Frecker both designed the study, acquired and analyzed data, wrote the article and gave final consent for its publication. Dr. Humber alone reviewed the written article.
Competing interests: None declared.
Accepted for publication Nov. 24, 2006
Correspondence to: Dr. N. Humber, Lillooet Medical Clinic, Box 850, Lillooet BC V0K 1V0; Saffron2@telus.net
References
- 1.Nesbitt TS, Connell FA, Hart LG, et al. Access to obstetric care in rural areas: effect on birth outcomes. Am J Public Health 1990;80:814-8. [DOI] [PMC free article] [PubMed]
- 2.Blair L. Are general surgeons a dying breed? CMAJ 1991;145:46-8. [PMC free article] [PubMed]
- 3.Inglis FG. Surgical care in rural Canada: training and planning for the future. CMAJ 1995;153:1453-4. [PMC free article] [PubMed]
- 4.Chiasson PM, Roy P. Role of the general practitioners in the delivery of surgical and anesthesia services in rural western Canada. CMAJ 1995;153:1447-52. [PMC free article] [PubMed]
- 5.Iglesias S, Strachan J, Ko G. Advanced skills by Canada's rural physicians. Can J Rural Med 1999;4:227-31.
- 6.Heaton P. Surgical care in small Alberta communities. Can Fam Physician 1983;29:1591-601. [PMC free article] [PubMed]
- 7.Roos N, Black C, Wade J, et al. How many general surgeons do you need in rural areas? Three approaches to physicians resource planning in southern Manitoba. CMAJ 1996;155:1395-401. [PMC free article] [PubMed]
- 8.Humber N, Frecker T. Delivery models of rural surgical services in British Columbia (1996–2005). Are GP-surgeons still part of the picture? Can J Surg 2008;51:173-8. [PMC free article] [PubMed]
- 9.Lynch N, Thommasen H, Anderson N, et al. Does having caesarean section capability make a difference to a small rural maternity service? Can Fam Physician 2005;51:1238-9. [PMC free article] [PubMed]
- 10.Dunbadin J. Procedural medicine in rural and remote NSW. The general practice workforce. Australia: New South Wales Rural Doctors; 2002.
- 11.Godwin M, Lailey J, Miller R, et al. Physician supply in rural Canada. Can Fam Physician 1996;42:1641-4. [PMC free article] [PubMed]
- 12.Kreibel SH, Pitts J. Obstetrical outcomes in rural family practice: an 8-year experience. J Fam Pract 1988;27:377-8. [PubMed]
- 13.Black DO, Fyfe I. The safety of obstetrical services in small communities in Northern Ontario. CMAJ 1984;130:571-6. [PMC free article] [PubMed]
- 14.Coopers and Lybrand Associated. The cost effectiveness of general practice [discussion document]. London: British Medical Association; 1983.
- 15.Kornelsen J, Grzybowski S. Safety and community: the maternity care needs of rural parturient women. J Obstet Gynaecol Can 2005;27:254-61. [DOI] [PubMed]
- 16.Nesbitt TS, Larson EH, Rosenblatt RA, et al. Access to maternity care in rural Washington: its effect on neonatal outcomes and resource use. Am J Public Health 1997;87:85-90. [DOI] [PMC free article] [PubMed]
- 17.Rosenblatt RA, MacFarlane A, Dawson AJ, et al. The regionalization of perinatal care in Wales and Washington State. Am J Public Health 1996;86:1011-5. [DOI] [PMC free article] [PubMed]
- 18.Iglesias S, Thompson J. Shared skill sets: a model for the training and accreditation of rural advanced skills. Can J Rural Med 1998;3:217-22.
- 19.Dhillon D, Johnston S, Makin M, et al. A statistical comparison of appendectomies done in a rural hospital by GP-surgeons vs. a regional centre by Royal College surgeons [presentation]. University of British Columbia Resident Day; Vancouver.
- 20.Caron NR, Lewis Watts DA, Webber EM. The provision of emergency surgical services in isolated communities [abstract]. Can J Surg 1998;41(Suppl):8.9492740
- 21.Iglesias S, Saunders LD, Tracy N, et al. Appendectomies in rural hospitals. Safe whether performed by specialist or GP surgeons. Can Fam Physician 2003;49:328-33. [PMC free article] [PubMed]
- 22.Deutchman M, Connor P, Gobbo R, et al. Outcomes of cesarean sections performed by family physicians and the training they received: a 15-year retrospective study. J Am Board Fam Pract 1995;8:81-90. [PubMed]