SYNOPSIS
The Saskatchewan Farm Injury Cohort (SFIC) is a major new Canadian study that was developed to evaluate potential causes of injury among farmers and their family members. The cohort involves 2,390 farms and 5,492 farm people being followed over a two-year period. The article describes the rationale and methodology for the baseline and longitudinal components of this study. The SFIC is one of the first studies to apply population health theory to the modeling of risks for injury in a defined Canadian population. In doing so, the relative influence of several potential causes of farm injury, including physical, socioeconomic, and cultural factors, will be estimated. Study findings will inform the content and targeting of injury prevention initiatives specific to the farm occupational environment.
Agriculture is one of the most hazardous occupations worldwide.1 In Canada between 1991 and 2000, for example, 1,256 adults and children were killed in farm-related activities and 14,980 people were hospitalized due to traumatic injury caused by the farm occupational environment.2 Losses associated with farm injury in terms of permanent disability, treatment costs, rehabilitation, and reduced potential are substantial.3 Subpopulations of people on farms who are vulnerable to injury include farm operators,2 preschool-aged children,4 adolescent and young adult workers,5 and the elderly.2
Existing etiological research in the field of injury control has been generally nontheoretical in nature, which is also characteristic of farm injury research. While various studies of risk factors for farm injury exist,6,7 few if any of these studies are based upon underlying theoretical constructs. Further, although presumed roles for the physical, social, and cultural environments in the etiology of farm injury are recognized,8 few attempts have been made to study these roles by applying theory to the development of epidemiologic models.
Population health theory,9 or the “new public health”10 that reemerged during the 1990s, provides a framework for examining structural and environmental influences on health. Proponents of this theory state that determinants of health operate at two levels: (1) ecological (contextual—e.g., physical, economic, or cultural environments) and (2) individual (e.g., personal health practices, health service use, and human biology).9 With respect to the etiology of farm injury, application of this theory suggests that contextual and individual determinants have direct and multiplicative effects that would interact to produce varying levels of risk for injury. Both levels of determinants require focused study, alone and in combination. Study of these interactions may lead to advances in the understanding of mechanisms that underlie the occurrence of injury in these settings. To our knowledge, this theoretical approach has not previously been applied to the study of farm injury.
The Saskatchewan Farm Injury Cohort (SFIC) is a major new Canadian study that provides an opportunity to test this theory. This study involves 5,492 farm people on 2,390 Saskatchewan farms over a two-year study period (2007 to 2009). This article describes the rationale and methodology for the SFIC and the characteristics of the farm operations and people who are participating. Given the importance of understanding the physical, cultural, and socioeconomic environments for injury etiology, our model and approach could be portable to the study of injury in agriculture and other contexts.
BACKGROUND OF THE SFIC
Aim, objectives, and hypothesis of the SFIC
The aim of the SFIC is to understand individual risk factors related to work (individual farm exposures) and settings (contextual or environmental exposures) associated with farm injury, with the long-term goal of informing the development of interventions directed at the prevention of injury within both farm populations and agricultural production settings. The objectives of the SFIC are twofold: (1) to examine associations between individual farm exposures and the occurrence of various types of farm injury in the province of Saskatchewan, Canada, and (2) to assess the importance of contextual factors (physical, socioeconomic, and cultural) as potential moderators of associations between individual farm exposures and the occurrence of injury. The primary study hypothesis is prevention-oriented: when contextual risks associated with physical, economic, and/or cultural settings are low, associations between individual farm exposures and farm injury will become attenuated.
Design of the SFIC
The SFIC design is a prospective cohort being conducted in two phases. The first phase, already completed, involved a baseline cross-sectional survey of residents from 2,390 Saskatchewan farm operations. The second phase defines groups of Saskatchewan farm people from the cross-sectional survey, based upon combinations of individual risk factors and contextual factors. These groups are being followed longitudinally for two years (from 2007 to 2009) to document and compare risks for farm injury.
Setting and population
The study base consists of active, operating farms in the province of Saskatchewan as of January 1, 2007. Saskatchewan is organized into 296 rural municipalities, each of which is governed by an elected council supported by local municipal staff. Collectively, the rural municipalities form a parent organization called the Saskatchewan Association of Rural Municipalities. The latter organization has supported the SFIC cohort study during its conception and development. Farms were identified from two sources: (1) lists of farms in rural municipalities that participated in the Saskatchewan Agricultural Health and Safety Network (AHSN), established in 1988 and continued in subsequent years by researchers at the University of Saskatchewan and municipal councils;11 and (2) lists of farms in non-AHSN rural municipalities. The AHSN is an agricultural health and safety extension program funded in part by local rural municipality councils on behalf of their membership. The importance of the AHSN lies in the fact that it is one of the largest and most longstanding health and safety initiatives of its kind. The AHSN has a direct mailing list of approximately 26,500 farm families representing 165 (56%) of the province's rural municipalities and, hence, farms. Prevention activities initiated by the AHSN are described elsewhere.11
For the SFIC, we planned a multistage, stratified sample of farms for study. Clusters of farms were nested within rural municipalities. Lists of AHSN and non-AHSN rural municipalities in each of the three main agricultural regions, defined by soil zone and, thus, type of agriculture,12 were identified. Fifty rural municipalities (25 each from AHSN and non-AHSN rural municipalities) were proportionally sampled. Study participation was requested formally during 50 separate meetings of the local rural municipal councils. In the case that councils refused, substitute rural municipalities were randomly selected from the same strata defined by agricultural region and AHSN participation. After receiving updated lists of farms from individual councils, all listed farms (mean per rural municipality: n=163) in the selected municipalities were contacted to participate. Farms that were inactive were excluded.
APPLICATION OF POPULATION HEALTH THEORY
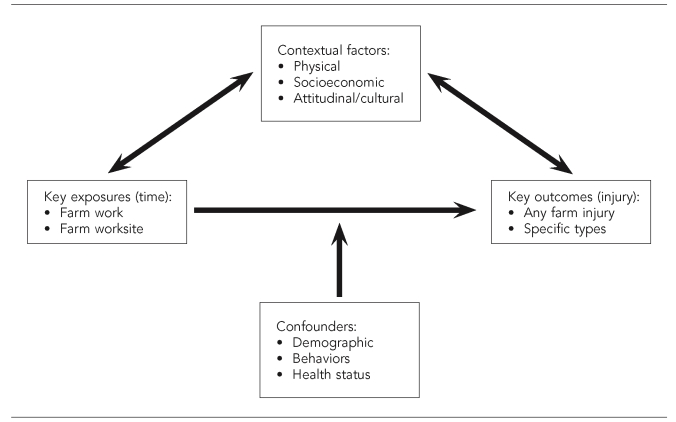
The Figure outlines the framework by which population health theory is being applied to the study of farm injuries and their etiology in the SFIC. Individual components of this framework are outlined as follows.
Figure.
Theoretical framework used to develop etiological models within the Saskatchewan Farm Injury Cohort (SFIC), adapted from population health theorya,b
aFederal, Provincial, and Territorial Advisory Committee on Population Health. Strategies for population health: investing in the health of Canadians. Ottawa (ON): Health Canada, Minister of Supply and Services Canada; 1994.
bTime that participants are exposed to farm work and farm worksites are the individual farm exposures under study. Farm injuries are the primary outcomes. Characteristics of the settings (context) in which farm people work and/or live may have a moderating influence on exposure-outcome relationships. In the SFIC, we hypothesize that when farm people are in positive contextual settings, associations between exposures and injury will be attenuated, after controlling for key confounders.
Primary outcomes
The primary outcome measures are work-related farm injuries and specific types of these injuries. Work-related farm injuries are defined as those that happen in a farm environment or during the course of farm work and that result in treatment of the injury by a doctor or nurse, or the victim missing at least four hours from work or usual activities due to the physical effects of the injury.13 A recall period of 12 months was used in the baseline survey, and four consecutive recall periods of six months will be used in the longitudinal study.
Individual farm exposures
Exposure to farm work.
Exposure to farm work was measured in terms of the duration (amount of time) that people were exposed to various types of farm work (e.g., total, mechanized, or animal-related). Measures consisted of seasonal assessments of individual items and composite scales developed from these items.
Exposure to the farm work environment.
Exposure to the work environment was measured in terms of amounts of time that people were present in the occupational farm worksite, not including the farm residence. Measures consisted of seasonal assessments of individual farm worksite exposures.
Contextual factors
Physical farm context.
Physical context was measured in terms of the number of injury-related physical hazards on the farm. A list of illustrative physical hazards was informed by the findings of the Canadian Agricultural Injury Surveillance Program2,14 and included farm descriptors such as (1) types of commodities produced, (2) area of land in production, (3) numbers of different types of animals on the farm, and (4) number and condition of various types of injury-producing machinery, including tractors, combines, and augers.
Socioeconomic farm context.
Socioeconomic context was measured using Likert-like scales that described the extent of worry on the farm attributable to cash-flow shortages and debt. These measures were developed with the input of farm operators, who recommended not asking direct questions about money, farm assets, and debt to maximize response rates.
Cultural farm context.
Cultural context was measured using individual items and scales, derived via factor analysis, that described normative farm safety practices within vulnerable populations on the farm including young children, young workers (aged 12 to 18 years), and older farm workers (older than 65 years of age). Again, items were developed based upon risk factors for injury inferred from the findings of the Canadian Agricultural Injury Surveillance Program.2,14 Examples of such practices assessed using Likert-like response options included the following:
- For young children:
- How often are young children present in the farm worksite?
- How often do young children ride in a cabbed tractor or cabbed combine with an adult operator?
- How often are young children present in the farm worksite while adults are working nearby?
- For young workers and older farm workers:
- How often do these workers operate tractors without rollover protection structures?
- How often do these workers operate farm equipment that is more than 20 years old?
- How often are these workers exposed to working at heights (e.g., climbing grain bins or large equipment)?
Confounders
Age, sex, and role on the farm.
These three demographics were included as confounders because they have been associated with injury risks and exposures to occupational situations in past analyses.13
Comorbid conditions.
Comorbid conditions were included as confounders because there is a strong correlation between health status and the ability to work, as well as between health status and the occurrence of injury, especially among older people.15,16
Health behaviors.
Health behaviors such as alcohol consumption patterns were included as confounders because these are also potential risk factors for injury in farm6 and other17 contexts.
Other items will be considered a posteriori as potential confounders if they meet contemporary criteria for confounding.18
DATA COLLECTION
Development of study instruments
Baseline questionnaire.
A panel consisting of the primary research team and active members of the farm community (three rural municipality councillors who were also farmers) developed the study questionnaire. Where possible, items that had been used in other research contexts19–21 were selected or adapted for use. All questionnaire items were submitted to pilot-testing for face validity on multiple occasions.
Testing of study materials.
Letters and questionnaires were tested via the following procedure: (1) a purposeful sample of 50 test farm people was selected for study; (2) the draft materials were administered; (3) we requested feedback on the study materials to assess question clarity, comprehension, time of completion, acceptability, and overall impressions; and (4) the study materials were refined. The 50 test farm people were not enrolled in the full cohort study.
Recruitment and baseline data collection
To maximize response, recruitment occurred using a modified version of the Dillman Total Design Method for Mail and Telephone Surveys.22 This involved a series of mail contacts with the farm, using an established recruitment approach designed to minimize nonresponse. In 2006, a formal pilot study was conducted in two rural municipalities to assess compliance with the baseline study protocol as well as projected response rates (Table 1). Baseline data collection commenced in February 2007 and ended in May 2007. Recruitment and the collection of baseline data occurred simultaneously. A knowledgeable adult from each farm was asked to provide information about the farm and its operation, a count of all people on the farm, and detailed information about each resident member of the farm family. (Data collection was not conducted for non-farm family members, as this would require collection of personal information that would be unlikely to be known or provided by the respondent.) By August 2007, the baseline data were entered, cleaned, validated, and prepared for analysis.
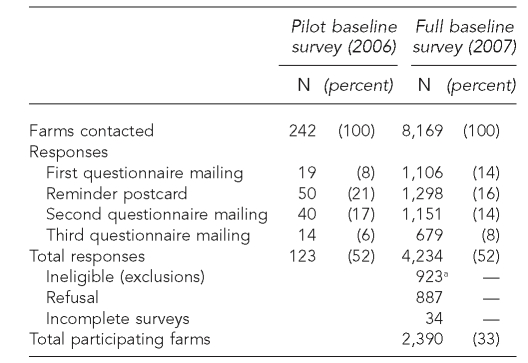
Table 1.
Response rates achieved in Saskatchewan Farm Injury Cohort in the 2006 pilot study of baseline survey methodology and the 2007 full baseline survey
aA total of 923 farms were ineligible for the following reasons: (1) the farm was no longer operating (543 farms) or no longer considered to be a farm or ranch (29 farms); (2) the farm operator was retired (172 farms); (3) the farm operator was dead (42 farms); (4) the mailing address supplied by the rural municipality was inaccurate (94 farms) or a duplicate (40 farms); or (5) the farm was ineligible for unknown reasons (three farms).
Follow-up
As part of the baseline questionnaire, a designated farm contact was identified for each participating farm. These contacts in the full SFIC have been or will be mailed a letter at six-month intervals (November 2007, April 2008, November 2008, and April 2009) to determine whether any farm injuries have occurred. If one or more injuries are reported for each follow-up period, detailed information about each injury event and the farm person involved will be collected on a study form. This follow-up protocol was informed by a randomized controlled trial that tested the relative efficacies of three different methods of maintaining contact with the farms.23 Compared with computer telephone or a choice of contact method (mail, computer telephone, or e-mail), a traditional method that relied solely on first-class mail was most efficacious. A pilot test of the mail-based follow-up method with 50 farms also resulted in high response rates (82%—41 out of 50—based upon one mailing).
STATISTICAL POWER
The primary hypothesis for the SFIC deals with associations between individual farm work and worksite exposures and the occurrence of injury. Two years of follow-up are planned for all participating farms. In planned analyses, subjects will typically be divided into groups based upon individual farm exposures assessed at baseline. Estimates of statistical power were therefore made for the highest vs. lowest exposure levels (for illustrative purposes here, based upon quartiles). Base rates of medically treated farm injury are about 5% to 10% on an annual basis.13,24 By consensus of the investigators and based upon review of existing analyses of related etiological literature, a 5% absolute shift in proportions of farm people experiencing injuries (e.g., 10% to 15% over two years) was considered an occupationally meaningful difference between highest and lowest quartiles. Statistical power will be high (.90%; α=0.05; two-tailed for all comparisons) if the full survey sample (5,492 people on 2,390 farms) is employed. Power will be reduced (1) in examination of potential effect modification (interactions) by context/setting; (2) in analyses conducted within vulnerable subgroups (some will be very limited); and (3) if substantial loss to follow-up occurs between baseline and follow-up interviews. For example, the SFIC will be 80% powered to detect only large (>20%) shifts in proportions for subgroups of 300 people (e.g., children younger than 12 years of age), and poorly powered to examine for effect modification. All calculations account for our choice to have a clustered sampling design, using inflation factors suggested by Hsieh et al.25
DATA ANALYSIS
To apply population health theory to the modeling of injury risks, we intend to use the following approach.
Descriptive
The individual farm exposures, contextual factors, confounders, and injury outcomes will be estimated for the full farm population and for population subgroups. Conventional descriptive statistics (frequencies, measures of central tendency, and variability) will be employed. Chi-square analyses, t-tests, and analysis of variance will be used for descriptive group comparisons.
Etiological
The etiological study questions lend themselves to regression analyses. The clustered nature of the data introduces a challenge for this modeling. Multilevel regression models with repeated measurements (first level), nested within individuals (second level), nested within farms (third level), and nested within rural municipalities (fourth level) will be applied to evaluate both individual-level and contextual etiological factors in regression situations.26 We will quantify the suggested effect of the individual farm exposures (fixed effects) and contextual factors (random effects) as risk factors for various types of injury. This will be done both overall, for specific injury types, and within subgroups defined by contextual features of settings. The statistical models employed (logistic, Cox proportional hazards, or Poisson regression) will depend on the type of outcome.
BASELINE RESULTS
Baseline recruitment
Of the rural municipalities selected to participate, 94%—47 out of 50—agreed to participate. The three nonparticipants were replaced by neighboring rural municipalities in the same soil zone (three out of three substitutes agreed to participate). A total of 8,169 potential farms and ranches were identified on the mailing lists of the 50 participating rural municipalities. Of these, 4,234 (52%) returned the baseline questionnaire. Of the 4,234 farms, 923 were ineligible, 887 refused participation, and 34 farms returned incomplete questionnaires, leaving 2,390 eligible and participating farms. The final response rate was 33% (2,390 out of 7,246) (Table 1).
Baseline cohort
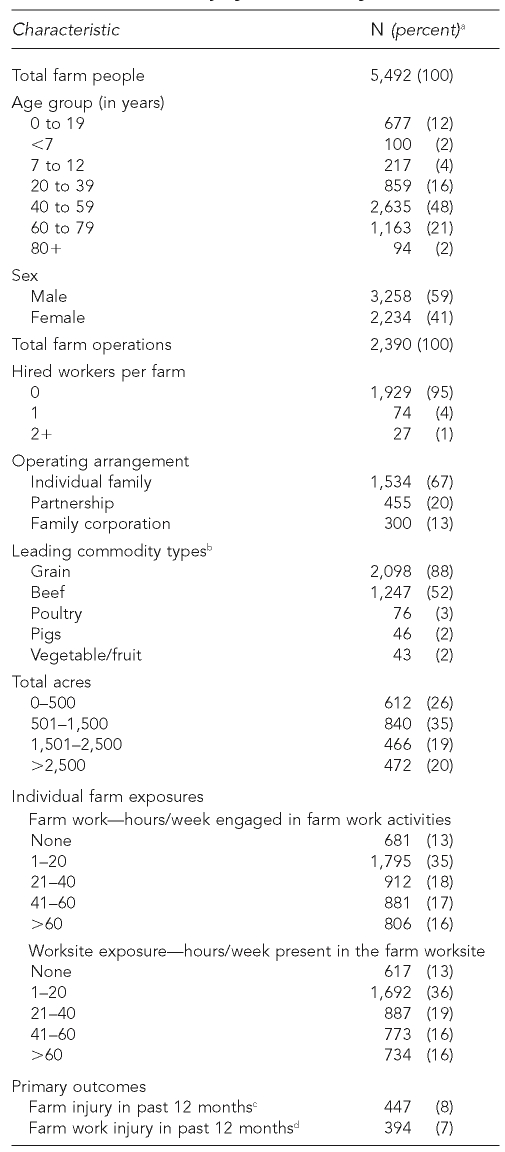
A baseline description of the 2,390 farms and 5,492 people participating in the SFIC is provided. The demographic profile of the participating farm people will permit examination of most of the vulnerable subgroups identified a priori for focused study, although the definition of young children will necessarily be expanded from younger than 7 years of age (n=100) to younger than 13 years of age (n=317) for such analyses. The sample of farms is also diverse, and there is also sufficient heterogeneity in observed individual exposures and contextual factors (Tables 2 and 3), as well as large enough numbers of reported injuries (Table 2), to undertake the proposed etiological analyses. While baseline recruitment was lower than expected, the primary aim of this study was to prospectively evaluate a number of possible determinants of farm injury in a large provincial sample, rather than to obtain estimates of farm characteristics that are representative of the province. For etiological analyses, the prospective cohort design minimized the possibility of selection bias, as participant outcomes had not occurred at the time of subject recruitment.
Table 2.
Baseline characteristics of farm people and farm operations participating in the Saskatchewan Farm Injury Cohort study
aNumbers do not always add to totals due to missing information.
bPercentages add to >100% as farms could report multiple commodities.
cInjury caused by any hazard of a farm work environment
dInjury that occurred while the victim was engaged in farm work
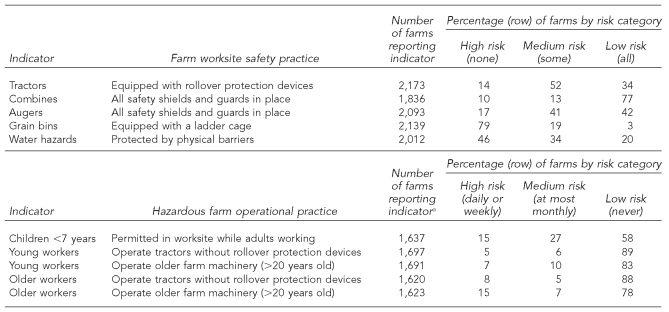
Table 3.
Percentages of farms participating in the Saskatchewan Farm Injury Cohort study reporting contextual indicators and practices (farm worksite safety practices and hazardous farm operational practices are presented as examples)
aA large number of farms that did not report resident farm children, young workers, or older workers indicated that members of these groups were sometimes present on their farms.
POPULATION HEALTH THEORY AND ETIOLOGICAL MODELING
One of the challenges of applying background theory such as the population health framework to the development of etiological models is a lack of direction about how to do this in practice. Population health theory is typically depicted in prose and/or diagrams that are useful conceptually, but not always easy to transform.9 In the SFIC, we plan to simultaneously examine individual risk factors (observations of people) and contextual factors (observations at the farm and higher levels) and how they interact to produce varying farm injury experiences. To accomplish this, we have suggested (1) the use of various multilevel models (e.g., logistic and Poisson) to simultaneously consider individual (person-level) and contextual (mainly farm-level) measures, while simultaneously accounting for the clustered nature of data collection; (2) the designation of individual farm exposures as the main effects in these models, and the contextual factors as potential effect modifiers (Figure); (3) the use of stratification or interaction terms in these models to test for effect modification; and (4) a set of a priori hypotheses surrounding findings that would be consistent with underlying theory (primary hypothesis: when contextual risks associated with physical, economic, and/or cultural settings are low, associations between individual farm exposures and farm injury will become attenuated). To our knowledge, an analogous list of practical alternatives for this type of modeling has never been published.
IMPORTANCE OF THE SFIC
While recognized as a leading public health problem in Canada and other countries,1,2 farm injury and its determinants require further etiological study. U.S. researchers have recognized the need to establish large cohort studies to further the understanding of the health of agricultural populations, particularly in the field of cancer. The best example of this is the Agricultural Health Study.27 The SFIC uses an analogous and methodologically rigorous cohort design to test the novel application of population health theory to the etiology of agricultural injury.28 The large sample size will support robust analysis and permit the examination of vulnerable subpopulations. The relatively low response rate suggests that our study group may not be fully representative of the base population. However, this is not a precondition for the successful study of relationships between risk factors and injury outcomes. Considerable heterogeneity in the risk factors under examination is required to support our hypothesis testing, and the SFIC will meet this requirement. Similarly, although a volunteer cohort could have lower rates of injury than the underlying base population, the farm injury rates reported at baseline suggest that sufficient injury events will occur. The high rates of follow-up achieved in the pilot studies suggest that our loss to follow-up, often a challenge in cohort studies, may be low.
The SFIC will contribute to further understanding the etiology of farm injury and, at the same time, make a contribution to methodological development for public health research in general. Through this research, we will simultaneously investigate the respective roles of physical, socioeconomic, and cultural contexts in the protection of farm people from operational risk factors. We expect to show that identified risk relationships will be elevated within vulnerable subpopulations. Settings that protect farm people from injury risk will be characterized, and this information will be available to provide concrete evidence in support of informed agricultural health policy and public health measures.
Acknowledgments
The authors thank Iris Rugg, Kendra Ulmer, Leanne LaBrash, Deborah Emerton, Murray Purcell, Debra Gronning, Louise Singer, and the farm families from central Saskatchewan who took the time to assist us with this research.
Footnotes
This study was supported financially, in part, by a research agreement with the Canadian Institutes of Health Research (operating grant: 200503MOP-145294-PUB-CCAA-56847) and a pilot study grant from the Canadian Centre for Health and Safety in Agriculture (also funded by the Canadian Institutes of Health Research, operating grant: CDA-66151). Lesley Day, PhD, is supported by a research fellowship (ID 236880) from the National Health and Medical Research Council of Australia.
REFERENCES
- 1.International Labour Organization. Safety and health in agriculture. Programme on Safety and Health at Work and the Environment (SafeWork) [cited 2007 Dec 7]. Available from: http://www.ilo.org/public/english/protection/safework/agriculture/index.htm.
- 2.Canadian Agricultural Injury Surveillance Program. Kingston (ON): Queen's University; 2003. Agricultural injuries in Canada for 1990–2000. [Google Scholar]
- 3.Locker AR, Dorland JL, Hartling L, Pickett W. Economic burden of agricultural machinery injuries in Ontario, 1985 to 1996. J Rural Health. 2003;19:285–91. doi: 10.1111/j.1748-0361.2003.tb00575.x. [DOI] [PubMed] [Google Scholar]
- 4.Brison RJ, Pickett W, Berg RL, Linneman J, Zentner J, Marlenga B. Fatal agricultural injuries in preschool children: risks, injury patterns and strategies for prevention. CMAJ. 2006;174:1723–6. doi: 10.1503/cmaj.050857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldcamp M, Hendricks KJ, Myers JR. Farm fatalities to youth 1995–2000: a comparison by age groups. J Safety Res. 2004;35:151–7. doi: 10.1016/j.jsr.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Simpson K, Sebastian R, Arbuckle TE, Bancej C, Pickett W. Stress on the farm and its association with injury. J Agric Saf Health. 2004;10:141–53. doi: 10.13031/2013.16471. [DOI] [PubMed] [Google Scholar]
- 7.Turner C, McClure R, Pirozzo S. Injury and risk-taking behavior—a systematic review. Accid Anal Prev. 2004;36:93–101. doi: 10.1016/s0001-4575(02)00131-8. [DOI] [PubMed] [Google Scholar]
- 8.Murphy DJ. Safety and health for production agriculture. St. Joseph (MI): American Society of Agricultural and Biological Engineers; 1992. [Google Scholar]
- 9.Federal, Provincial, and Territorial Advisory Committee on Population Health. Strategies for population health: investing in the health of Canadians. Ottawa (ON): Health Canada, Minister of Supply and Services Canada; 1994. [Google Scholar]
- 10.Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55:125–39. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- 11.Hagel LM, McDuffie HH, Dosman JA, Lupescu C, Lockinger L, Bidwell J. The agricultural health and safety network: the 10-year history of a unique extension program. J Agric Saf Health. 1999;5:227–37. [Google Scholar]
- 12.Prairie Farm Rehabilitation Administration, Agriculture and Agri-Food Canada. Land use and farming systems. In: Smith DG, Hoppe TA, editors. Prairie agricultural landscapes: a land resource review. Regina (SK): Minister of Public Works and Government Services; 2000. pp. 81–120. [Google Scholar]
- 13.Pickett W, Brison RJ, Niezgoda H, Chipman ML. Nonfatal farm injuries in Ontario: a population-based survey. Accid Anal Prev. 1995;27:425–33. doi: 10.1016/0001-4575(94)00080-6. [DOI] [PubMed] [Google Scholar]
- 14.Pickett W, Hartling L, Dimich-Ward H, Guernsey JR, Hagel L, Voaklander DC, et al. Surveillance of hospitalized farm injuries in Canada. Inj Prev. 2001;7:123–8. doi: 10.1136/ip.7.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hagel LM, Dosman JA, Rennie DC, Ingram MW, Senthilselvan A. Effect of age on hospitalized machine-related farm injuries among the Saskatchewan farm population. J Agric Saf Health. 2004;10:155–62. doi: 10.13031/2013.16472. [DOI] [PubMed] [Google Scholar]
- 16.Lord S, Sherrington C, Menz H. Falls in older people: risk factors and strategies for prevention. Cambridge (UK): Cambridge University Press; 2001. [Google Scholar]
- 17.Anderson P, Cremona A, Paton A, Turner C, Wallace P. The risk of alcohol. Addiction. 1993;88:1493–508. doi: 10.1111/j.1360-0443.1993.tb03135.x. [DOI] [PubMed] [Google Scholar]
- 18.Rothman KJ, Greenland S. Precision and validity in epidemiologic studies. In: Rothman KJ, Greenland S, editors. Modern epidemiology. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1998. pp. 123–5. [Google Scholar]
- 19.Statistics Canada. Canadian community health survey profiles. [cited 2007 Dec 3]. Available from: http://www.statcan.ca/bsolc/english/bsolc?catno=82-576-XIE.
- 20.Currie C, Samdal O, Boyce W, Smith R, editors. Research protocol for the 2001/2002 survey. Edinburgh (Scotland): University of Edinburgh Child and Adolescent Health Research Unit; 2001. Health behaviour in school-aged children: a WHO cross-national study. [Google Scholar]
- 21.Choi SW, Peek-Asa C, Sprince NL, Rautiainen RH, Flamme GA, Whitten PS, et al. Sleep quantity and quality as a predictor of injuries in a rural population. Am J Emerg Med. 2006;24:189–96. doi: 10.1016/j.ajem.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 22.Dillman DA. Mail and Internet surveys: the tailored design method. 2nd ed. New York: John Wiley and Sons, Inc.; 2000. [Google Scholar]
- 23.Day L, Dosman J, Hagel L, Dostaler S, Snodgrass P, Thiessen J, et al. Application of novel communication technologies to the study of farm families: a randomized controlled trial. Prev Med. 2008;46:364–9. doi: 10.1016/j.ypmed.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 24.Gerberich SG, Gibson RW, French LR, Lee TY, Carr WP, Kochevar L, et al. Machinery-related injuries: regional rural injury study—I (RRIS—I) Accid Anal Prev. 1998;30:793–804. [PubMed] [Google Scholar]
- 25.Hsieh FY, Lavori PW, Cohen HJ, Feussner JR. An overview of variance inflation factors for sample-size calculation. Eval Health Prof. 2003;26:239–57. doi: 10.1177/0163278703255230. [DOI] [PubMed] [Google Scholar]
- 26.Raudenbush SW, Bryk AS. Hierarchical linear models. Applications and data analysis methods. 2nd ed. Thousand Oaks (CA): Sage Publications, Inc.; 2002. [Google Scholar]
- 27.Alavanja MC, Sandler DP, McMaster SB, Zahm SH, McDonnell CJ, Lynch CF, et al. The Agricultural Health Study. Environ Health Perspect. 1996;104:362–9. doi: 10.1289/ehp.96104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rothman KJ, Greenland S. Cohort studies. In: Rothman KJ, Greenland S, editors. Modern epidemiology. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1998. pp. 79–91. [Google Scholar]