SYNOPSIS
Objective.
We reported on the distribution of very preterm (VPT) birth rates by race across metropolitan statistical areas (MSAs).
Methods.
Rates of singleton VPT birth for non-Hispanic white, non-Hispanic black, and Hispanic women were calculated with National Center for Health Statistics 2002–2004 natality files for infants in 168 MSAs. Subanalysis included stratification by parity, age, smoking, maternal education, metropolitan size, region, proportion of MSA that was black, proportion of black population living below the poverty line, and indices of residential segregation.
Results.
The mean metropolitan-level VPT birth rate was 12.3, 34.8, and 15.7 per 1,000 live births for white, black, and Hispanic women, respectively. There was virtually no overlap in the white and black distributions. The variation in mean risk across cities was three times greater for black women compared with white women. The threefold disparity in mean rate, and two- to threefold increased variation as indicated by standard deviation, was maintained in all subanalyses.
Conclusion.
Compared with white women, black women have three times the mean VPT birth risk, as well as three times the variance in city-level rates. The racial disparity in VPT birth rates was composed of characteristics that were constant across MSAs, as well as factors that varied by MSA. The increased sensitivity to place for black women was unexplained by measured maternal and metropolitan factors. Understanding determinants of differences in both the mean risk and the variation of risk among black and white women may contribute to reducing the disparity in risk between races.
Birth prior to 32 weeks gestation, called very preterm (VPT) birth, occurs in 2% of all pregnancies ending in live birth.1 One-third of all infant deaths are attributable to complications of prematurity, and 95% of those are from the small population of sub-32-week births.2 In addition to increased mortality, VPT birth results in increased morbidity, such as respiratory disease, developmental delays, and cerebral palsy.3–5 Variation in risk for VPT birth by maternal race is well described, although the sources of this disparity remain unresolved. African American women experience VPT birth at 2.5 times the rate of non-Hispanic white women,1 and this disparity attenuates little with statistical control for education, income, medical comorbidities, or behaviors associated with risk.6,7 The persistence of this disparity in the face of control for (measured) confounders has led some to suggest the difference is largely genetic,8 yet nativity studies comparing the experience of immigrant women of African ancestry to U.S.-born African American women suggest the toxic exposure may be more environmental than ancestral.9,10
Interest in the role of maternal residential environment—variably conceptualized from the local census tract up to the national level—has increased in recent years.11 Place-based exposures that have been associated with pregnancy outcomes include neighborhood crime,12 access to retail food outlets,13 city-level segregation,14 city-level air pollution,15 state-level income inequality,16 and national politics and welfare state status.17 Most studies of social or environmental determinants of racial disparities compare mean risk among racial groups, providing interracial contrasts. Less is known about the role, if any, of intraracial variation in understanding determinants of VPT birth disparities.
This article describes the distribution of metropolitan-level rates of VPT birth by race and ethnicity to characterize the inter- and intraracial variation across cities.
METHODS
Data
Birth files from the National Center for Health Statistics (NCHS) for 2002–2004 were combined. These files include an observation for every birth in the U.S. during the given time period. Births were restricted to singletons born to mothers who self-report race and ethnicity as non-Hispanic white, non-Hispanic black, or Hispanic. A further restriction was to mothers residing in one of the 311 metropolitan statistical areas (MSAs) with populations of 100,000 or more in the 2000 census. An MSA is a geographical unit defined by the U.S. Office of Management and Budget as a county or group of counties around a core city that are socially and economically integrated.18 New England City and Town Area Divisions (NECTAs) are parallel units used in New England, and for this analysis were analyzed as MSAs.
Gestational age was calculated from maternally reported last menstrual period (LMP) for the vast majority of births. In 2002 2003, 4.6% of births used clinical estimates of gestational age because of missing LMP or birth weight incompatible with LMP.19,20 In 2004, 5.9% of births used clinical estimates of gestational age.21
There were 11.8 million singleton live births from 2002 to 2004, with 56.2% born to non-Hispanic white mothers, 14.1% to non-Hispanic black mothers, and 22.7% to Hispanic mothers. Because VPT birth is a rare event, to insure stability of rates we restricted analyses to MSAs with at least 1,000 live births in 2002–2004 for each racial group. Exclusion of MSAs with fewer than 1,000 race-specific births resulted in 301, 168, and 169 MSAs for white, black, and Hispanic mothers, respectively. The vast majority of all births in the U.S. (76% of all white, 84% of black, and 87% of Hispanic births) occurred in these eligible MSAs. Rates of VPT birth were calculated separately for each racial/ethnic group within each MSA.
Analysis
The unit of analysis was the MSA. Rates were first described graphically with race-stratified histograms of all eligible MSAs. Subsequent analyses were limited to the 168 MSAs with adequate numbers of both white and black births. Of these MSAs, 115 also had adequate numbers of Hispanic births. It is plausible that national distribution of births by race (there were 4.2 million births to white women in the 168 MSAs, but only 1.5 million births to black women) could result in differing observed variances that reflect sample size rather than true variation. Because we were interested in both the mean rate in each MSA and the variance in rates across MSAs, we assessed the effect of sample size on variance by taking a random sample of all white births in the 168 MSAs with sufficient black births, so as to simulate exactly equal numbers of black and white births. Because sample size did affect variance to a small degree, all stratified analyses were conducted on the equalized sample.
Descriptive statistics for each racial/ethnic group include the mean and standard deviation (SD) of the empiric distribution of city-level rates. Variances of black and Hispanic distributions were compared with the white distribution with F-statistics, with the respective number of MSAs as the numerator and denominator degrees of freedom.
Different distributions of women in cities by proportion native-born, and by maternal age, education, marital status, smoking status, or parity, could drive an observed difference among cities. To assess these possibilities, the analysis was repeated after further restriction to U.S.-born women, to primiparous women, and to nonsmokers. Additionally, we reported on distributions adjusted for age and stratified on maternal education and marital status.
Because broad-ranging regional variation and population composition of metropolitan areas could influence distributions of rates, analyses were repeated within each of four Census regions, and for three different sizes of MSAs. All MSAs with sufficient number of black births were categorized according to quintiles of the proportion of total MSA population that was black, as well as quintiles of the black population living below the poverty line, as reported in the 2000 U.S. Census. The MSA distribution within racial/ethnic groups was reported for the MSAs in the first and fifth quintile of each spectrum. Regional variation in other pregnancy outcomes has been partially explained by racial segregation22 and income inequality.23 Multiple dimensions of segregation have been described, including evenness/unevenness (the degree to which a minority group is evenly distributed across sub-areas of the MSA) and exposure/isolation (the probability that a randomly drawn minority member shares a neighborhood with someone in his/her own group [isolation] or in a different group [exposure]).24
For this analysis, we used two indices calculated by the Census Bureau, each assessing black-white segregation. Theil's Entropy Index (sometimes termed H) is a measure of unevenness, and xPx measures isolation. Each ranges from 0 to 1, with 0 being complete integration, and 1 being complete segregation. Income inequality was measured by the Census Bureau with the Gini coefficient, which ranges from 0 (where income is equally distributed across the population) to 1 (where all income is held by one person).
True length of gestation was likely causally associated with infant mortality and morbidity. However, measurement error in common proxies for true gestational length can influence rate estimates. For investigators interested in racial disparities, this may be more concerning, as there is evidence that the measurement error is differential with respect to race or ethnicity.25–27 Birth weight, on the other hand, is much more reliably measured, although perhaps less causally plausible.28 Controversy exists about the causal association of low birth weight (<2,500 grams) to infant mortality and morbidity, but the more extreme very low birth weight (VLBW) (<1,500 grams) infants overlap significantly with VPT infants (83% of singleton VLBW infants in this dataset were also VPT). Because quality of gestational age reporting might vary regionally, the analysis was repeated using birth weight <1,500 grams as the outcome.
To explore metropolitan-level sources of variation for black women, multivariate linear regression models were fit, with the rate of VPT birth per 1,000 births as the outcome. Variables initially considered for the model were region, MSA size (in three categories), proportion of MSA population that was black, proportion of black population below poverty line, median household income (both overall and for black households), proportion of black adults >25 years of age with a college degree, and proportion without a high school degree, both segregation indices, and the Gini coefficient. Backward stepwise regression proceeded, and subsequent analysis for colinearity was conducted.
For every analysis, the calculation of whether an MSA-race-stratification group had at least 1,000 total births was repeated, thus insuring stable rates in each subanalysis. However, this did result in varying numbers of MSAs being eligible for each analysis.
All data analysis was conducted using SAS 9.2.29
RESULTS
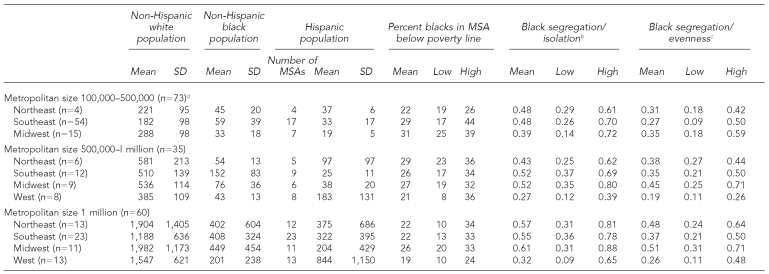
The population distribution of 168 MSAs with sufficient numbers of black and white births is detailed by race, region, and metropolitan size in Table 1. The Southeast region had the largest number of MSAs, with the remainder roughly evenly divided among the other three regions. Segregation by either index tended to be lower in the West, as did black poverty rates. Smaller MSAs also had slightly lower levels of segregation, while the largest MSAs had lower black poverty rates.
Table 1.
Population distribution by metropolitan characteristicsa
aAll population estimates are derived from U.S. Census 2000 data and reported in thousands.
bIsolation segregation (xPx) is interpreted as the probability of two randomly chosen people from a given area (e.g., Census tract) being from the same group. It ranges from 0 (full integration) to 1 (complete segregation).
cEvenness segregation (Theil's H index) is interpreted as the degree to which a minority group is evenly distributed across sub-areas (e.g., Census tracts) in a metropolitan area. It ranges from 0 (full integration) to 1 (complete segregation).
dWest was n=0, so it is not included.
MSA = metropolitan statistical area
SD = standard deviation
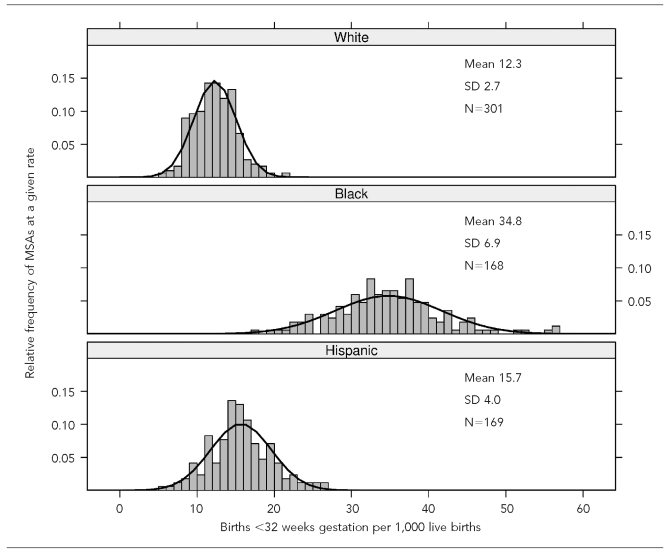
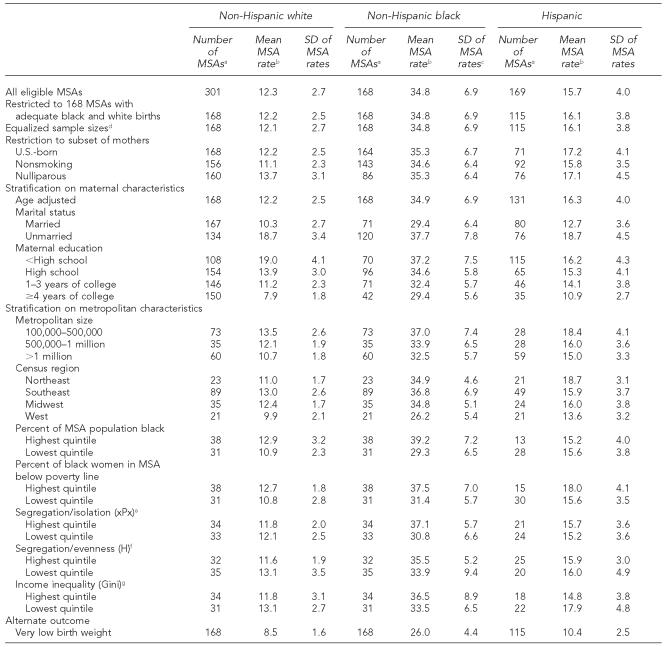
The Figure displays the distribution of VPT birth rates by race across all eligible MSAs for each racial/ethnic group. The x-axis is the rate of VPT birth per 1,000 live births, and the y-axis is the relative frequency of MSAs; in other words, it is the proportion of all MSAs at a given rate. For white women, the mean MSA rate of VPT birth was 12.3/1,000 (SD=2.7); for black women, the mean rate was 34.8/1,000 (SD=6.9); and for Hispanic women, the mean MSA rate was 15.7/1,000 (SD=4.0). Restricting the analysis to the 168 MSAs, which had sufficient white and black births, changed these estimates very little, as seen in Table 2. F-tests comparing the variance in white and black distributions of MSA rates were statistically significant (p<0.0001) for every stratum investigated. Similarly, the random selection of white births to equalize sample sizes only reduced the white SD by 7%, from 2.7 to 2.5, leaving the ratio of the variance in the black distribution to the white distribution relatively unchanged.
Figure.
Rates of very preterm birth in U.S. metropolitan statistical areas (MSAs) by race, 2002–2004
SOURCE: National Center for Health Statistics Natality Files, 2002–2004; Singleton live births.
SD = standard deviation
Table 2.
Distribution of rates of very preterm births aggregated at the MSA level by race, 2002–2004
SOURCE: National Center for Health Statistics Natality File, 2002–2004
aOnly MSAs having at least 1,000 live births in 2002–2004 within a given racial/ethnic group and within given strata were included for analysis.
bSingleton births <32 weeks gestation per 1,000 live births
cFor every analysis in this table, F-tests comparing the variance in the non-Hispanic black distribution with the variance in the non-Hispanic white distribution were statistically significant at p<0.0001.
dA simple random sample of all white births in the 168 MSAs with sufficient black births was drawn to simulate the effect of an equalized sample size of white and black births. The full number of black and Hispanic births was used.
eEvenness segregation (Theil's H index) is interpreted as the degree to which a minority group is evenly distributed across sub-areas (e.g., Census tracts) in a metropolitan area. It ranges from 0 (full integration) to 1 (complete segregation).
fIsolation segregation (xPx) is interpreted as the probability of two randomly chosen people from a given area (e.g., Census tract) being from the same group. It ranges from 0 (full integration) to 1 (complete segregation).
gThe Gini Index is a measure of distribution of income across a population. It ranges from 0 (each person has an equal share income) to 1 (all income is received by one person, while others receive none).
MSA = metropolitan statistical area
SD = standard deviation
Within each racial group, the lowest mean rate was in Western cities (9.9, 26.2, and 13.6 per 1,000 live births for white, black, and Hispanic women, respectively), among married mothers (10.3, 29.4, and 12.7), and college-graduated mothers (7.9, 29.4, and 10.9). The respective high rates for each group varied, with white mothers seeing the highest mean rate among unmarried women (18.7) and women without a high school degree (19.0). Black women also had a high risk of VPT birth among unmarried mothers (37.7), as well as mothers residing in cities with the highest quintile of proportion black (39.2) and highest quintile of black women below the poverty line (37.5). For Hispanic women, high rates occurred among unmarried women (18.7), cities in the Northeast region (18.7), for nulliparous women (17.1) and women residing in cities with the highest quintile black population below poverty line (18.0). Cities with the highest unevenness segregation had lower VPT birth rates for white women (11.6 vs. 13.1 in the lowest quintile), while the opposite was true for black women (first quintile = 33.9, fifth quintile = 35.5). The effect of higher isolation segregation in black women was even stronger, with a range of 30.8 to 37.1 from the first to fifth quintiles.
Given equalization of the sample size, the SD of the distribution of city rates in each stratum could be a rough indicator of the similarity or variation among cities. For all three groups, the greatest city-to-city variation was seen when restricting to unmarried mothers (SD=3.4, 7.8, and 4.5 for white, black, and Hispanic women, respectively). Black women also had greater city-to-city variation in the group of cities with the lowest unevenness segregation (SD=9.4) and the highest income inequality (SD=8.9), while for white women, high variation was seen when restricting to mothers without a high school diploma (SD=4.1). For all three groups, city-to-city variation was lowest when restricting to mothers with a college education, and in the cities with the largest populations.
In addition to describing the within-race patterns of VPT birth rates, the means and SDs suggest varying interracial patterns. Black women consistently had two to three times the city-to-city variation for any given analysis as compared with white and Hispanic women. Although increasing education and marital status were protective for all groups, the magnitude of protection varied so that the black-white rate ratio among college-graduated mothers was 3.7 as compared with a ratio of 1.9 among women without a high school degree. The mean rate for U.S.-born Hispanic mothers was greater than the overall rate, suggesting increased risk with subsequent generations (mean of 15.7 overall, 17.2 for U.S.-born mothers). Hispanic women without a high school degree had lower rates than similarly schooled white or black women (16.2 vs. 19.0), although this advantage waned with increasing education.
The overall pattern of a threefold black-white racial disparity in mean rates, as well as a threefold increased variance, persisted with the use of VLBW as an alternate outcome. There was moderate correlation within cities of white and black VPT birth rates (r2 = 0.21, p<0.01) and of white and Hispanic rates (r2 = 0.20, p<0.01). Related is the observation that MSA-specific black/white rate ratios varied across MSAs with a median ratio of 2.8, and a range from 1.5 to 5.8.
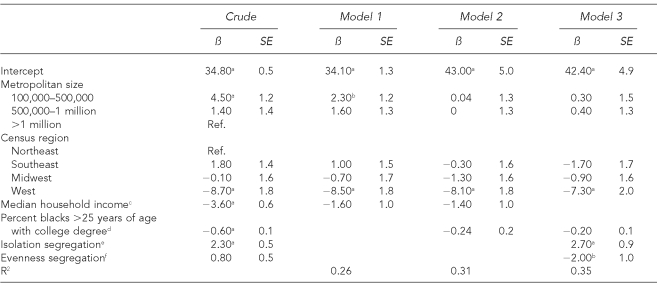
Metropolitan area size and region of the country explained 26% of the black inter-city variance in VPT birth rates (Table 3). The black poverty rate and black median household income did not provide any better model fit than overall median household income alone, and so were dropped. The Gini coefficient was not significant in base models including region and metropolitan size, although both segregation indices were independently predictive in all models tested. A one SD increase in isolation segregation was associated with an increase in the black VPT birth rate of 2.7/1,000, while a one SD increase in unevenness reduced VPT rates to 2/1,000.
Table 3.
Linear regression of metropolitan characteristics and black very preterm birth rates per 1,000 live births
ap<0.01
bp<0.05
cThe median household income was scaled so that the beta is the change in very preterm birth rate for a $10,000 change in median household income.
dThe proportion of black women with a college degree was centered around its mean (13.6%) and scaled to integers. The beta was interpreted as a change in very preterm birth rate for a 1% change from mean black college percent.
eThe isolation index (xPx) was standardized so that the beta could be interpreted as the change in the very preterm birth rate for one standard deviation change in isolation.
fThe evenness index (Theil's H) was standardized so that the beta could be interpreted as the change in the very preterm birth rate for one standard deviation change in isolation.
SE = standard error
Ref. = reference group
DISCUSSION
Three observations are apparent from the Figure. First, the mean MSA rate for black women is nearly three times that of white women. This is the ecologic corollary of the individual racial disparity in VPT birth. Nonetheless, it is quite striking, particularly in light of the second observation, which is that there is almost no overlap in the white and black distribution. The rate of VPT birth in the very best city for black women was virtually identical to the rate in the very worst city for white women. The final observation is that the variation or spread of the empiric distribution of rates among MSAs was significantly greater for black women than for white women, with the SD for black women approximately 2.5 times greater than for white women (p<0.0001). This increased spread remains after accounting for sample sizes, differences in distribution of key predictors of VPT birth, and measurement error of the outcome.
The first two observations suggest that regardless of where black women live, they experience excess risk of VPT birth, implying an exposure that is ubiquitous or constant across space. The third observation suggests that in addition to this excess risk experienced in all cities, there is increased sensitivity to city of residence for black women as compared with white women. While regional differences in mean risk for various pregnancy outcomes have been reported,30–32 to our knowledge no study to date has described the extent of regional variation in VPT birth, nor reported racial differences in both means and variance.
Explanations for the persistent excess rates of poor pregnancy outcomes among black women have been stubbornly hard to find. The increasing magnitude of the racial disparity among seemingly lower-risk, college-graduated, married black and white women has been previously reported7,33 and suggests either residual confounding by socioeconomic status or a negative exposure that counterbalances the protective effects of increasing socioeconomic status among black women. Candidate exposures for persistent elevated risk despite statistical control for (measured) socioeconomic status include exposure to interpersonal racism,34,35 “weathering” of biologic systems as a result of lifelong exposure to stress,36 or genetic predisposition to preterm birth.37 Any of these factors, or an epigenetic combination of them,38 could potentially represent the ubiquitous exposure accounting for elevated VPT birth rates for black women across cities.
The increased city-to-city variance for black women as compared with either white or Hispanic women suggests metropolitan-level exposures that are uniquely relevant for black women. While differences in population composition could still explain some of this variation, the persistent pattern after stratifying on the strongest risk factors for VPT birth, including marital status, maternal education, parity, and age, suggest that structural or contextual factors rather than purely compositional factors are the source of observed variance. State-level income inequality has been found to associate with infant mortality—an outcome strongly correlated with VPT birth—in several recent studies.23,39 Increasing income inequality could associate with infant mortality through poverty concentration, lower social capital, and level of investment in social and welfare systems. We found increased VPT birth rates for black women in cities with the highest compared with the lowest inequality, but the reverse was true for white and Hispanic women, although the remaining inter-city variance in all cases was larger than the change in the mean. Income inequality was not independently predictive in multivariate models. It is not clear whether income inequality at the state level has the same meaning as inequality at the MSA level.
Residential segregation has also been associated with increased black but not white infant mortality and VPT birth.40,41 Segregation is a process of sorting individuals into residential environments on the basis of race or income, and has been termed a fundamental cause of racial health disparities.42,43 These neighborhoods influence school quality, educational attainment, economic opportunity, and exposure to crime, high crowding, and quality of housing.42 The evenness dimension of segregation (measured here with Theil's H index) describes how evenly a minority group is distributed across sub-areas of a city. The exposure (or isolation) dimension describes the potential for interaction between individuals of the same or different groups. Although evenness is frequently used in research (the dissimilarity index is another measure of the same dimension), it may be less theoretically compelling for health outcomes than the exposure dimension.44 We found that cities with higher isolation had higher black VPT birth rates, but cities with higher unevenness had lower black and white VPT birth rates. For both white and black people, there was less city-to-city variation in rates among MSAs with highest segregation in either evenness or isolation.
Findings of paradoxically low rates of pregnancy outcomes among Hispanic women have been consistently noted.45,46 We found that U.S.-born Hispanic mothers had higher rates of VPT birth than immigrant Hispanic women, although Hispanic people overall have an inter-city distribution that is closer to white women than black women. If immigrants are more likely to be without a high school degree, this healthy immigrant effect may explain the Hispanic advantage over white women without a high school degree. However, as seen with black women, the protective effect of education is weaker for Hispanic women than it is for white women.
Neither the persistence of disparity in mean risk nor the heterogeneity of variation after the adjustments reported in this article should be seen as immutable. Rather, they are as yet unexplained clues that open opportunities for improved understanding of and intervention on excess VPT birth. Notably, this analysis suggests an interaction between race and factors associated with MSAs. The moderate amount of correlation of MSA rates among races suggests that what is a “bad” city for one group is not necessarily bad for all, and some factor or group of factors cause great variation in risk for black women while having almost no effect (in the aggregate at least) on white women.
Limitations
The cross-sectional use of vital statistics data to understand the social or environmental experience of mothers is limited in many regards. Residence is recorded only for the point at time of delivery, but does not necessarily represent the residential environment either preconceptionally or perinatally. Additionally, place of residence is only reported by NCHS when the place has a population in excess of 100,000, thus limiting inference regarding smaller metropolitan, micropolitan, or rural areas. However our requirement that there be at least 1,000 births to a given group in an area would likely have excluded all such smaller areas had they been available. Vital statistics data are also limited by measurement error not only of gestational age, but also of maternal residence and maternal characteristics.
CONCLUSIONS
This analysis demonstrates that rates of VPT birth vary not only among races, but also by city of residence for black women as compared with white women. Explanations for racial disparities in VPT birth may include determinants that are ubiquitous across cities and that vary by city. The apparent enhanced sensitivity to location of maternal residence among black women suggests a possible interaction between race and characteristics of MSAs, such as degree of segregation.
This observation raises opportunities and challenges for further research focused on understanding and eventually eliminating racial disparities in preterm birth. One implication is that future analyses comparing rates across MSAs must be wary of statistical assumptions in their model for homogeneity of variance. Identification of factors that explain the wide variation in black MSA rates could illuminate determinants for excess VPT birth, as well as opportunities for intervention. Disparities should not be conceived of as simply a shift in the mean of a distribution, but possibly also involving interaction with environmental characteristics, resulting in a change in variation around the mean.
Acknowledgments
Michael Kramer acknowledges financial support from a Health Resource and Service Adminstration Maternal and Child Health training grant (T03MC07651).
REFERENCES
- 1.Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2006. Natl Vital Stat Rep. 2007 Dec 5;56:1–18. [PubMed] [Google Scholar]
- 2.Callaghan WM, MacDorman MF, Rasmussen SA, Qin C, Lackritz EM. The contribution of preterm birth to infant mortality rates in the United States. Pediatrics. 2006;118:1566–73. doi: 10.1542/peds.2006-0860. [DOI] [PubMed] [Google Scholar]
- 3.Keogh JM, Badawi N. The origins of cerebral palsy. Curr Opin Neurol. 2006;19:129–34. doi: 10.1097/01.wco.0000218227.35560.0d. [DOI] [PubMed] [Google Scholar]
- 4.Thorngren-Jerneck K, Herbst A. Perinatal factors associated with cerebral palsy in children born in Sweden. Obstet Gynecol. 2006;108:1499–505. doi: 10.1097/01.AOG.0000247174.27979.6b. [DOI] [PubMed] [Google Scholar]
- 5.Marret S, Ancel PY, Marpeau L, Marchand L, Pierrat V, Larroque B, et al. Neonatal and 5-year outcomes after birth at 30–34 weeks of gestation. Obstet Gynecol. 2007;110:72–80. doi: 10.1097/01.AOG.0000267498.95402.bd. [DOI] [PubMed] [Google Scholar]
- 6.Goldenberg RL, Cliver SP, Mulvihill FX, Hickey CA, Hoffman HJ, Klerman LV, et al. Medical, psychosocial, and behavioral risk factors do not explain the increased risk for low birth weight among black women. Am J Obstet Gynecol. 1996;175:1317–24. doi: 10.1016/s0002-9378(96)70048-0. [DOI] [PubMed] [Google Scholar]
- 7.McGrady GA, Sung JF, Rowley DL, Hogue CJ. Preterm delivery and low birth weight among first-born infants of black and white college graduates. Am J Epidemiol. 1992;136:266–76. doi: 10.1093/oxfordjournals.aje.a116492. [DOI] [PubMed] [Google Scholar]
- 8.Kistka ZA, Palomar L, Lee KA, Boslaugh SE, Wangler MF, Cole FS, et al. Racial disparity in the frequency of recurrence of preterm birth. Am J Obstet Gynecol. 2007;196:131. doi: 10.1016/j.ajog.2006.06.093. [DOI] [PubMed] [Google Scholar]
- 9.Howard DL, Marshall SS, Kaufman JS, Savitz DA. Variations in low birth weight and preterm delivery among blacks in relation to ancestry and nativity: New York City, 1998–2002. Pediatrics. 2006;118:e1399–405. doi: 10.1542/peds.2006-0665. [DOI] [PubMed] [Google Scholar]
- 10.David RJ, Collins JW., Jr. Differing birth weight among infants of U.S.-born blacks, African-born blacks, and U.S.-born whites. N Engl J Med. 1997;337:1209–14. doi: 10.1056/NEJM199710233371706. [DOI] [PubMed] [Google Scholar]
- 11.Culhane JF, Elo IT. Neighborhood context and reproductive health. Am J Obstet Gynecol. 2005;192(Suppl 5):S22–9. doi: 10.1016/j.ajog.2005.01.071. [DOI] [PubMed] [Google Scholar]
- 12.Messer LC, Kaufman JS, Dole N, Savitz DA, Laraia BA. Neighborhood crime, deprivation, and preterm birth. Ann Epidemiol. 2006;16:455–62. doi: 10.1016/j.annepidem.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Lane SD, Keefe RH, Rubinstein R, Levandowski BA, Webster N, Cibula DA, et al. Structural violence, urban retail food markets, and low birth weight. Health Place. 2008;14:415–23. doi: 10.1016/j.healthplace.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Grady SC. Racial disparities in low birthweight and the contribution of residential segregation: a multilevel analysis. Soc Sci Med. 2006;63:3013–29. doi: 10.1016/j.socscimed.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 15.Ritz B, Wilhelm M, Hoggatt KJ, Ghosh JK. Ambient air pollution and preterm birth in the environment and pregnancy outcomes study at the University of California, Los Angeles. Am J Epidemiol. 2007;166:1045–52. doi: 10.1093/aje/kwm181. [DOI] [PubMed] [Google Scholar]
- 16.Reagan PB, Salsberry PJ. Race and ethnic differences in determinants of preterm birth in the USA: broadening the social context. Soc Sci Med. 2005;60:2217–28. doi: 10.1016/j.socscimed.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 17.Chung H, Muntaner C. Political and welfare state determinants of infant and child health indicators: an analysis of wealthy countries. Soc Sci Med. 2006;63:829–42. doi: 10.1016/j.socscimed.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 18.Office of Management and Budget (US) Final report and recommendations from the metropolitan area standards review committee to the Office of Management and Budget concerning changes to the standards for defining metropolitan areas. Washington: OMB (US); 2000. [Google Scholar]
- 19.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2003. Natl Vital Stat Rep. 2005 Sep 8;54:1–116. [PubMed] [Google Scholar]
- 20.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2002. Natl Vital Stat Rep. 2003 Dec 17;52:1–113. [PubMed] [Google Scholar]
- 21.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S. Births: final data for 2004. Natl Vital Stat Rep. 2006 Sep 29;55:1–101. [PubMed] [Google Scholar]
- 22.Polednak AP. Trends in US urban black infant mortality, by degree of residential segregation. Am J Public Health. 1996;86:723–6. doi: 10.2105/ajph.86.5.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mayer SE, Sarin A. Some mechanisms linking economic inequality and infant mortality. Soc Sci Med. 2005;60:439–55. doi: 10.1016/j.socscimed.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 24.Massey DS, Denton NA. The dimensions of residential segregation. Social Forces. 1988;67:281–315. [Google Scholar]
- 25.Reichman NE, Schwartz-Soicher O. Accuracy of birth certificate data by risk factors and outcomes: analysis of data from New Jersey. Am J Obstet Gynecol. 2007;197:32. doi: 10.1016/j.ajog.2007.02.026. [DOI] [PubMed] [Google Scholar]
- 26.Qin C, Dietz PM, England LJ, Martin JA, Callaghan WM. Effects of different data-editing methods on trends in race-specific preterm delivery rates, United States, 1990–2002. Paediatr Perinat Epidemiol. 2007;21(Suppl 2):41–9. doi: 10.1111/j.1365-3016.2007.00860.x. [DOI] [PubMed] [Google Scholar]
- 27.Parker JD, Schoendorf KC. Implications of cleaning gestational age data. Paediatr Perinat Epidemiol. 2002;16:181–7. doi: 10.1046/j.1365-3016.2002.00407.x. [DOI] [PubMed] [Google Scholar]
- 28.Wilcox AJ. On the importance—and the unimportance—of birthweight. Int J Epidemiol. 2001;30:1233–41. doi: 10.1093/ije/30.6.1233. [DOI] [PubMed] [Google Scholar]
- 29.SAS Institute Inc. SAS: Version 9.1 for Windows. Cary (NC): SAS Institute, Inc.; 2002–2003. [Google Scholar]
- 30.Allen DM, Buehler JW, Hogue CJ, Strauss LT, Smith JC. Regional differences in birth weight-specific infant mortality, United States, 1980. Public Health Rep. 1987;102:138–45. [PMC free article] [PubMed] [Google Scholar]
- 31.Racial and ethnic disparities in infant mortality rates—60 largest U.S. cities, 1995–1998. MMWR Morb Mortal Wkly Rep. 2002;51(15):329-32–343. [PubMed] [Google Scholar]
- 32.Polednak AP, King G. Birth weight of US biracial (black-white) infants: regional differences. Ethn Dis. 1998;8:340–9. [PubMed] [Google Scholar]
- 33.Schoendorf KC, Hogue CJ, Kleinman JC, Rowley D. Mortality among infants of black as compared with white college-educated parents. N Engl J Med. 1992;326:1522–6. doi: 10.1056/NEJM199206043262303. [DOI] [PubMed] [Google Scholar]
- 34.Jackson FM, Phillips MT, Hogue CJ, Curry-Owens TY. Examining the burdens of gendered racism: implications for pregnancy outcomes among college-educated African American women. Matern Child Health J. 2001;5:95–107. doi: 10.1023/a:1011349115711. [DOI] [PubMed] [Google Scholar]
- 35.Collins JW, Jr., David RJ, Handler A, Wall S, Andes S. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am J Public Health. 2004;94:2132–8. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med. 1996;42:589–97. doi: 10.1016/0277-9536(95)00159-x. [DOI] [PubMed] [Google Scholar]
- 37.Esplin MS. Preterm birth: a review of genetic factors and future directions for genetic study. Obstet Gynecol Surv. 2006;61:800–6. doi: 10.1097/01.ogx.0000248747.52343.5f. [DOI] [PubMed] [Google Scholar]
- 38.Hogue CJ, Bremner JD. Stress model for research into preterm delivery among black women. Am J Obstet Gynecol. 2005;192(5) Suppl:S47–55. doi: 10.1016/j.ajog.2005.01.073. [DOI] [PubMed] [Google Scholar]
- 39.Kennedy BP, Kawachi I, Prothrow-Stith D. Income distribution and mortality: cross sectional ecological study of the Robin Hood index in the United States. BMJ. 1996;312:1004–7. doi: 10.1136/bmj.312.7037.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bird ST. Separate black and white infant mortality models: differences in the importance of structural variables. Soc Sci Med. 1995;41:1507–12. doi: 10.1016/0277-9536(95)00029-7. [DOI] [PubMed] [Google Scholar]
- 41.Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, Huebner CE. Birth outcomes among urban African-American women: a multilevel analysis of the role of racial residential segregation. Soc Sci Med. 2006;63:3030–45. doi: 10.1016/j.socscimed.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 42.Acevedo-Garcia D, Osypuk TL, McArdle N, Williams DR. Toward a policy-relevant analysis of geographic and racial/ethnic disparities in child health. Health Aff (Millwood) 2008;27:321–33. doi: 10.1377/hlthaff.27.2.321. [DOI] [PubMed] [Google Scholar]
- 43.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93:215–21. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hummer RA, Powers DA, Pullum SG, Gossman GL, Frisbie WP. Paradox found (again): infant mortality among the Mexican-origin population in the United States. Demography. 2007;44:441–57. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Scribner RA. Infant mortality among Hispanics: the epidemiological paradox. JAMA. 1991;265:2065–6. [PubMed] [Google Scholar]