SYNOPSIS
Objective.
We determined the association of demographic, psychosocial, and contextual factors with condom use among a large community sample of at-risk adolescents recruited from four locations in the U.S.
Methods.
We enrolled 1,410 adolescents/young adults between the ages of 15 and 21 with a history of unprotected sex in the past 90 days at four study sites. Subjects completed an audio-assisted, computerized assessment that gathered information about sexual behavior and its contexts, substance use, and relevant risk and protective attitudes.
Results.
Nearly two-thirds of adolescents did not use condoms at the time of last intercourse and adolescents reported a mean of 15.5 (median = 5) unprotected intercourse occasions in the past 90 days. Controlling for relevant demographic variables, not using condoms was associated with the perception that condoms reduce sexual pleasure, the perception that partners will not approve of condom use, and less discussion with partners about condoms.
Conclusions.
Even across racial/ethnic groups, gender, and geographic locations, several important correlates of adolescents' sexual risk reduction were identified. Many adolescents may feel that condoms reduce their sexual pleasure and fear partner reactions if they initiate condom use. These attitudes may be malleable through clinical and community-based interventions.
The prevention of sexually transmitted diseases (STDs) among adolescents is a national priority.1–5 To monitor prevention needs, the Centers for Disease Control and Prevention has conducted behavioral surveillance of adolescents' self-reported sexual risk behaviors.3 One common indicator of risk in these studies is adolescents' failure to use condoms. Trend studies from this surveillance system suggest that males are more likely than females to report recent condom use and that African American adolescents are more likely than their white or Hispanic counterparts to use condoms.6 Unfortunately, while informative, the surveillance system is limited with respect to the number of potential factors assessed that may be associated with not using condoms. Further, this system uses a school-based sampling methodology. Thus, the findings are limited to adolescents attending school.
Emerging evidence strongly suggests that condom use by adolescents is influenced by socioecological factors rather than simply cognitive factors.7 Socioecological factors include constructs related to adolescents' relational behaviors. In essence, these factors can be considered as contextual influence on sexual risk behavior. Thus, in addition to traditional demographic and psychosocial measures, relational measures such as the presence of a main partner can be very useful in attempts to understand why some adolescents do not use condoms.8,9
Several review articles have summarized empirical findings relevant to the correlates of adolescents' condom use.2,7,10,11 However, much of the evidence contained in these reviews is not based on community-recruited samples of adolescents and lacks a relational perspective. Further, many studies have recruited adolescents from within a single geographic area, or have recruited a specific gender or racial/ethnic group, potentially limiting the generalizability of the findings for the design of human immunodeficiency virus (HIV)/STD behavior change interventions. Accordingly, the purpose of this study was to determine the association of demographic, attitudinal, and contextual factors with condom use among a large community sample of at-risk sexually active adolescents recruited from several areas of the U.S.
METHODS
Study sample
A variety of recruitment strategies was employed both across and within the four adolescent sites as part of a larger study, Project SHIELD, which was designed to test the efficacy of a brief (four-hour) group HIV prevention skills-based intervention. This article focuses on the baseline assessment of behaviors and attitudes. Two sites, Emory University in Atlanta, Georgia, and Rhode Island Hospital in Providence, Rhode Island, recruited people in medical facilities including primary care clinics and STD clinics with limited community recruitment activities. In contrast, Miriam Hospital in Providence and the University of Miami in Miami, Florida, employed street outreach in which staff made initial contact with high-risk adolescents in public housing projects, parks, schools, detoxification facilities, and homeless shelters. All sites also employed passive recruitment via Project SHIELD posters and flyers. Adolescents were approached individually. The study was briefly described and potential participants were offered an opportunity to answer screening questions, privately, to determine whether or not they qualified for study participation. Adolescents who verbally consented to screening were administered a 23-item questionnaire focusing on study inclusion and exclusion criteria. In addition, the recruiter was asked to evaluate the individuals' capacity to understand English and to give informed consent.
Eligible participants had to be between the ages of 15 and 21. The primary inclusion criterion for this study was sexual activity (vaginal or anal) within the past 90 days during which a condom was not used on at least one occasion. Adolescents were excluded if they were currently pregnant or had delivered a baby within the past 90 days; actively trying to get pregnant; HIV-positive by self-report; or currently participating in another HIV prevention study.
Procedures
All procedures were approved by each site's Institutional Review Board and the coordinating center's Institutional Review Board. Adolescents younger than 18 years of age gave assent and their parents gave informed consent. Those aged 18 and older gave informed consent. Adolescents completed a 30-minute baseline, audio computer-assisted structured interview (A-CASI) and were compensated $50 for their time and effort. Assessments were conducted on an individual basis or administered in a group format (with monitors ensuring privacy). Prior to starting the interview, adolescents were shown a 90-day calendar to help them recall significant events during the period and accurately remember sexual risk behaviors. Research staff remained in the testing room to answer any questions.
Measures
The interview questions were largely derived from measures used in Project LIGHT, a National Institute of Mental Health/National Institutes of Health-funded multisite trial of HIV prevention for high-risk young adults.12 The primary sexual risk measures were (1) number of sex acts when a condom was not used in the past 90 days and (2) condom use at last intercourse. Condom use was assessed for each reported partner within the past 90 days, and the instances of unprotected sex were summed for all partners.
The interview also included questions regarding attitudes and perceptions about condom use, which were used to create a set of four scales that were hypothesized to be associated with sexual risk behavior.2,12 In subsequent analyses, these attitude scales were related to a range of adolescent risk behaviors.13,14 Response alternatives for these scales ranged from 1 (strongly disagree) to 5 (strongly agree) and higher scores on scales reflected unfavorable attitudes toward condom use. The Condom Pleasure Scale (α=0.85, range 4–20) reflected pleasurable and unpleasurable expectations regarding condom use (e.g., “Sex with condoms doesn't feel natural”). The Main Partner Condom Expectancy Scale (α=0.65, range 8–40) and the Casual Partner Condom Expectancy Scale (α=0.68, range 8–40) included questions regarding perceptions of partners' reactions to discussions of condom use as well as the actual use of condoms (e.g., “Msy main partner would get mad if I said we had to use a condom”; “A casual partner would prefer that we use condoms during sex”). The Peer Norms Scale (α=0.71, range 8–40) included questions regarding perceptions of peer values about abstinence, sexual activity, and condom use (e.g., “How many of your friends think that it's fine to have vaginal or anal sex without a condom?”).
In addition, adolescents completed the Condom Communication and Negotiation Checklist. This measure contained questions regarding communication about condoms and negotiation of condom use in the past 90 days. Yes/no responses were provided (e.g., “In the past 90 days, did you have vaginal or anal sex without a condom because a partner refused to use one?”). A higher score indicated greater communication with partners (range 0–6).
Data analyses
Due to a skewed distribution, the variable representing the number of unprotected sex acts (median = 5, mean = 15.5, standard deviation [SD] = 28.4, mode = 0) was dichotomized by performing a median split. T-tests were used to assess bivariate significance for the two measures of condom use with the scale measures. Odds ratios and their 95% confidence intervals were calculated to examine bivariate associations between the remaining correlates and the two outcomes. Correlates achieving bivariate significance were next entered into multiple logistic regression analyses.
RESULTS
Of the 1,867 eligible adolescents at all sites, 1,410 (76%) were enrolled. Of those 1,410 enrolled youth, more than half (56.5%) were females. Nearly one-half were African American (51.2%), 23.5% were Hispanic, and almost 19% were white. Slightly more than half (55%) were 18 years of age or younger, approximately 50% had not yet completed high school, and a majority (66%) reported living in their parents' or guardians' home. Nearly one-fifth of the sample (17%) was living with a partner. Nearly two-thirds of the sample (63%) did not use a condom at last intercourse, and 26% never used condoms during sex in the past 90 days. The mean number of unprotected sexual acts in the past 90 days was 15.5 (median = 5). The mean number of partners was 2.0 (SD=2.3).
Bivariate findings
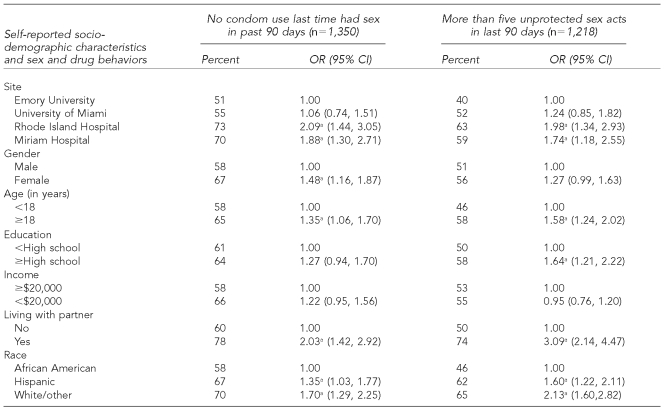
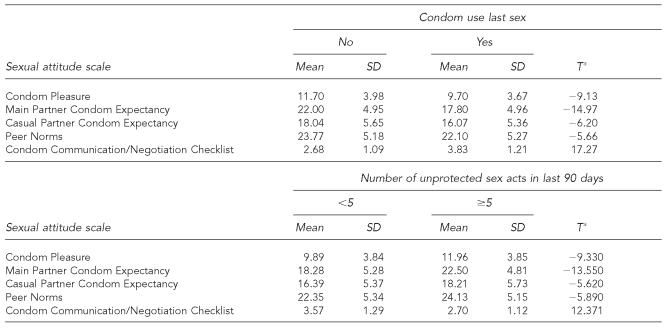
Table 1 presents the bivariate analyses describing the associations between the assessed correlates and the two outcome measures. Being female, older, and Hispanic or white were significantly associated both with a decreased likelihood of using condoms at last sex and reporting more unprotected sex acts in the past 90 days. Adolescents with at least a high school education reported more unprotected sex acts than their peers. Adolescents living with sexual partners were less likely to have used a condom during last sex and to report more unprotected sex than those who did not live with a partner. Consistent with racial, economic, and sampling strategy differences among sites, there were differences in reports of sexual risk behavior. Emory University was randomly chosen as the referent category. All of the attitude measures (Table 2) were significantly associated with using a condom during the last sex act and with the number of unprotected sex acts over the last 90 days.
Table 1.
Use of condoms and unprotected sex acts in last 90 days by sociodemographic factors
ap<0.05
OR = odds ratio
CI = confidence interval
Table 2.
Use of condoms and number of unprotected sex acts in last 90 days by sexual attitudes
ap<0.0001
SD = standard deviation
Multivariate findings
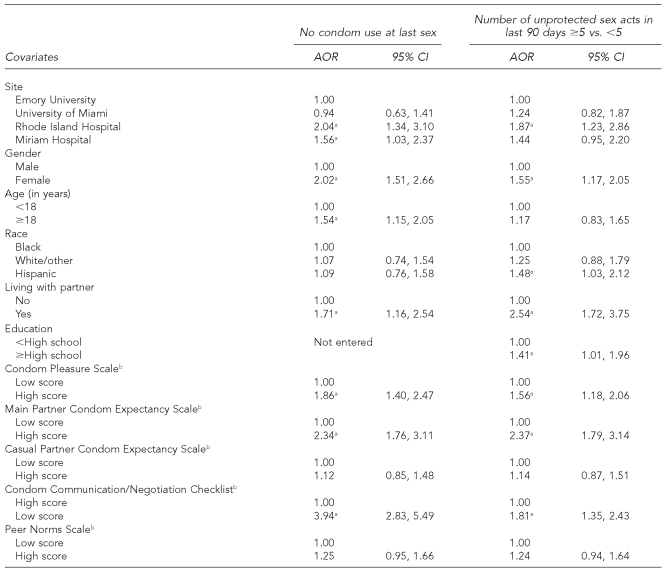
A logistic regression analysis with condom use at last sex as the outcome variable used a forward stepwise entry method and data from the 1,277 adolescents for whom complete data on all scales and the outcome were available (Table 3). The model was significant (X2=261.71, degree of freedom [DF] = 13, p<0.0001) and classified 82% correctly. Controlling for site difference, higher scores on the Main Partner Condom Expectancy and Sexual Pleasure scales (indicating greater barriers to condom use with a main partner and greater pleasure-related barriers, respectively) and lower scores on the Condom Communication and Negotiation Checklist were associated with a higher likelihood of not using a condom during the most recent act of intercourse. Females were more likely than males and those aged 18 or older more likely than younger teens to report not using a condom during their last act of intercourse.
Table 3.
Multiple logistic regression analyses on not using condoms at last sex and number of unprotected sex acts
ap<0.05
bScales split at median for ease of interpretation
AOR = adjusted odds ratio
CI = confidence interval
Table 3 also presents results from a logistic regression analysis pertaining to the number of unprotected sex acts (divided at the median of 5). Using a forward stepwise entry, the final model represented data from 1,181 adolescents for whom all data were available for this outcome and scale. The model was significant (X2=224.58, DF511, p<0.0001) and classified 79% correctly. Controlling for site difference, higher scores on the Main Partner Condom Expectancy and Sexual Pleasure scales and lower scores on the Condom Communication and Negotiation Checklist were significantly associated with a greater number of unprotected acts. In addition, being older, female, and having a main partner were associated with more unprotected sex.
DISCUSSION
This study provided important data documenting the risk behaviors that place adolescents at risk of sexually transmitted infections (STIs), including HIV. Risk behaviors were substantial among the youth who had unprotected sex in the past 90 days. For example, many adolescents reported never using condoms in the past 90 days, most had not used a condom at the time of last intercourse, and the median number of unprotected sex acts in the past 90 days was substantial. Adolescents reported a mean of two partners during the last 90 days. Seventeen percent were living with a main sexual partner—which is not surprising given the age of the sample—and was a significant predictor of sexual risk. This overall risk was documented in an ethnically and racially diverse sample of sexually active at-risk adolescents and young adults.
In analyses controlling for multiple aspects of this diverse sample (e.g., race, age, gender, geography), we quantified the significant impact of the psychosocial correlates of adolescents' sexual risk behavior. Adolescents' perceptions regarding loss of sexual pleasure because of condom use, their perceptions concerning negative reactions from a partner regarding condom use, and their lack of communication with partners all predicted less condom use. These factors were each independently associated with lack of condom use despite being considered in a model that controlled for several demographics and other variables. We also found that these factors were associated with two indices of sexual risk (condom use at last sex and unprotected sex in the past 90 days). These findings emphasize the relationship that adolescent perceptions of loss of sexual pleasure and from partners' reactions have with condom use and imply the need to focus on such attitudes in clinical and public health sexual risk-reduction efforts.
The findings can inform clinical care in several ways. First, the findings suggest that adolescents' sexual risk behavior should be carefully and routinely assessed at all clinical encounters. More specifically, clinicians can target several attitudes of adolescents to promote increased condom use. For example, the perceived negative reactions of partners to condom use could be mitigated by teaching adolescents how to effectively communicate with partners to use condoms. Clinicians could, for example, teach adolescents when to initiate condom use discussions and how to approach this discussion in a tactful and respectful manner. With these communication skills, adolescents' fears of negative partner reactions could be reduced. Further, many adolescents may say that sex with condoms is less pleasurable for them or their partners. Therefore, clinicians have an opportunity to counsel adolescent clients about finding condom brands and sizes that provide optimal fit, comfort, and sensation. Unfortunately, the pace and complexity of clinical care may make extensive counseling about condom use impractical. Also, the lack of reimbursement for prevention services and other systemic factors may make these recommendations difficult to implement. Clinics, however, can provide adolescents with a variety of condoms to, perhaps, find a brand and size that improves their level of sexual pleasure. Also, clinicians have the opportunity to refer adolescents to small-group sexual risk-reduction programs.
Data also have implications for community-based sexual risk-reduction programs for adolescents. For example, small-group workshops are an excellent opportunity to challenge adolescents' perceptions that partners will have negative reactions to condom use. Facilitators can engage in norm-setting exercises designed to dispel the perception that negative reactions are inevitable. Further, facilitators can engage adolescents in discussions that bring out instances where partners have agreed to use condoms, thereby reinforcing the idea that partners may be agreeable to using condoms. To demonstrate and reinforce effective condom negotiation skills, facilitators can use role-play techniques that emphasize timing, style, and content of effective communication. Also, it may be useful to include adolescents' partners in these intervention efforts, further enhancing program efficacy. This study found that nearly 20% of the sample was living with a main sex partner, thereby suggesting the potential to incorporate partners into interventions. Indeed, involving partners may be the most direct strategy to dispel misconceptions and build healthy communication. Recent meta-analyses and reviews of adolescent HIV prevention interventions suggest that these strategies are likely to be effective.15,16
Limitations
Findings are limited by the validity of the self-reported data; however, the design included multiple strategies to enhance validity. For example, A-CASI was used because it has been demonstrated to increase the reporting of sexual behaviors and consistency checks in A-CASI queried adolescents when they provided conflicting data.17 In addition, the observed associations are cross-sectional; thus, causality cannot be determined. Clearly, prospective analyses and interventions that target relevant condom use attitudes are needed to corroborate these findings. Also, adolescents with a history of unprotected sex were enrolled, so these findings may not generalize to less-at-risk youth. Nevertheless, the multiple recruitment methods employed at each site resulted in a convenience sample of ethnically and racially diverse sexually active adolescents in several locations in the U.S. These conditions allow for conclusions that are not limited to one city or ethnic/racial group.
CONCLUSION
Even across racial/ethnic groups, gender, and geographic locations, several important determinants of adolescents' sexual risk reduction were identified. Of importance, many adolescents may feel that condoms reduce their sexual pleasure and fear partners' reactions if they initiate condom use. Fortunately, these attitudes may be malleable through clinical and community-based interventions. Interventions that account for these attitudes may reduce adolescents' risk of STIs and promote their sexual health.
Acknowledgments
The authors thank the other participants in the Project SHIELD Study Group: Principal Investigators: Timothy Flanigan, MD, of Miriam Hospital; Deborah Haller, PhD, of Virginia Commonwealth University in Richmond, Virginia; Lori Leonard, ScD, of the University of Texas, Houston Health Science Center in Houston, Texas; and Lydia O'Donnell, EdD, of the Education Development Center in Newton, Massachusetts; Site Investigators: Caryl Gay, PhD, of the University of Miami; Janet Knisely, PhD, of Virginia Commonwealth University, Kevin Lourie, PhD, of Rhode Island Hospital; Louise Masse, PhD, of the University of Texas, Houston Health Science Center; Janet O'Connell, MPH, of Miriam Hospital; Eve Rose, PhD, of Emory University; Ann Stueve, PhD, of Columbia School of Public Health in New York, New York; Leah Varga, MA, of the University of Miami; Sue Vargo, PhD, of the Education Development Center; and Gina Wingood, ScD, MPH, of Emory University; Coordinating Center Investigators: Jamia L. Bacharach, JD, Courtney Johnson, PhD, and Allison Rose, PhD, all of the Research Triangle Institute in Research Triangle Park, North Carolina; and Consumer Representatives: Christian Aldridge, Beri Hull, and Sean Scott.
Footnotes
This research was supported by a Substance Abuse & Mental Health Services Administration grant #U10 SM52073 to the cooperating adolescent sites: Rhode Island Hospital in Providence, Rhode Island; Miriam Hospital in Providence; Emory University in Atlanta, Georgia; and the University of Miami in Miami, Florida.
REFERENCES
- 1.Felice ME, Feinstein RA, Fisher MM, Kaplan DW, Olmedo LF, Rome ES, et al. Adolescent pregnancy—current trends and issues: 1998 American Academy of Pediatrics Committee on Adolescence, 1998–1999. Pediatrics. 1999;103:516–20. doi: 10.1542/peds.103.2.516. [DOI] [PubMed] [Google Scholar]
- 2.DiClemente RJ, Crosby RA. Sexually transmitted diseases among adolescents: risk factors, antecedents, and prevention strategies. In: Adams GR, Berzonsky M, editors. Blackwell handbook of adolescence. Oxford: Blackwell Publishers Ltd.; 2003. pp. 573–605. [Google Scholar]
- 3.Kann L, Kinchen SA, Williams BI, Ross JG, Lowry R, Grunbaum JA, et al. Youth risk behavior surveillance—United States, 1999. MMWR CDC Surveill Summ. 2000;49(51):1–32. [PubMed] [Google Scholar]
- 4.Department of Health and Human Services (US) Healthy people 2010. 2001. [cited 2001 Dec 30]. Available from: URL: http://www.health.gov/healthypeople.
- 5.Eng TR, Butler WT. The hidden epidemic: confronting sexually transmitted diseases. Washington: National Academy Press; 1997. [PubMed] [Google Scholar]
- 6.Trends in sexual risk behaviors among high school students—United States, 1991–1997. MMWR Morb Mortal Wkly Rep. 1998;47(36):749–52. [PubMed] [Google Scholar]
- 7.DiClemente RJ, Salazar LF, Crosby RA, Rosenthal SL. Prevention and control of sexually transmitted infections among adolescents: the importance of a socio-ecological perspective—a commentary. Public Health. 2005;119:825–36. doi: 10.1016/j.puhe.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 8.Lescano CM, Vazquez EA, Brown LK, Litvin EB, Pugatch D Project SHIELD Study Group. Condom use with “casual” and “main” partners: what's in a name? J Adolesc Health. 2006;39:443.e1–7. doi: 10.1016/j.jadohealth.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Rosengard C, Adler NE, Gurvey JE, Ellen JM. Adolescent partner type experience: psychosocial and behavioral differences. Perspect Sex Reprod Health. 2005;37:141–7. doi: 10.1363/psrh.37.141.05. [DOI] [PubMed] [Google Scholar]
- 10.Santelli JS, DiClemente RJ, Miller KS, Kirby D. Sexually transmitted diseases, unintended pregnancy, and adolescent health promotion. Adolesc Med. 1999;10:87–108. [PubMed] [Google Scholar]
- 11.Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: a meta-analysis. Psychol Bull. 1999;125:90–132. doi: 10.1037/0033-2909.125.1.90. [DOI] [PubMed] [Google Scholar]
- 12.The National Institute of Mental Health (NIMH) Multisite HIV Prevention Trial Group. The NIMH multisite HIV prevention trial: reducing HIV sexual risk behavior. Science. 1999;280:1889–94. doi: 10.1126/science.280.5371.1889. [DOI] [PubMed] [Google Scholar]
- 13.Crosby RA, DiClemente RJ, Wingood GM, Salazar LF, Rose E, Levine D, et al. Condom failure among adolescents: implications for STD prevention. J Adolesc Health. 2005;36:534–6. doi: 10.1016/j.jadohealth.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 14.Houck CD, Lescano CM, Brown LK, Tolou-Shams M, Thompson J, DiClemente R, et al. “Islands of risk”: subgroups of adolescents at risk for HIV. J Pediatr Psychol. 2006;31:619–29. doi: 10.1093/jpepsy/jsj067. [DOI] [PubMed] [Google Scholar]
- 15.Johnson BT, Carey MP, Marsh KL, Levin KD, Scott-Sheldon LA. Interventions to reduce sexual risk for the human immunodeficiency virus in adolescents, 1985–2000. Arch Pediatr Adolesc Med. 2003;157:381–8. doi: 10.1001/archpedi.157.4.381. [DOI] [PubMed] [Google Scholar]
- 16.Pedlow CT, Carey MP. Developmentally appropriate sexual risk reduction intervention for adolescents: rationale, review of interventions, and recommendations for research and practice. Ann Behav Med. 2004;27:172–84. doi: 10.1207/s15324796abm2703_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Romer D, Hornik R, Stanton B, Black M, Li X, Ricardo I, et al. “Talking” computers: a reliable and private method to conduct interviews on sensitive topics with children. J Sex Res. 1997;34:3–9. [Google Scholar]