SYNOPSIS
Objectives.
Many of the 2.5 million Americans assaulted annually by intimate partners seek medical care. This project evaluated diagnostic codes indicative of intimate partner violence (IPV) in Oregon hospital and emergency department (ED) records to determine predictive value positive (PVP), sensitivity, and usefulness in routine surveillance. Statewide incidence of care for IPV was calculated and victims and episodes characterized.
Methods.
The study was a review of medical records assigned ≥1 diagnostic codes thought predictive of IPV. Sensitivity was estimated by comparing the number of confirmed victims identified with the number predicted by statewide telephone survey. Patients were aged ≥12 years, treated in any of 58 EDs or hospitals in Oregon during 2000, and discharged with one of three primary or 12 provisional codes suggestive of IPV. Outcome measures were number of victims detected, PPV and sensitivity of codes for detection of IPV, and description of victims.
Results.
Of 58 hospitals, 52 (90%) provided records. Case finding using primary codes identified 639 victims, 23% of all estimated female victims seen in EDs or hospitalized statewide. PVP was 94% (639/677). Provisional codes increased sensitivity (51%) but reduced PVP (50%). Highest incidence occurred in women aged 20 39 years, and those who were black. Hospitalizations were highest among women aged ≥50 years, black people, or those with comorbid illness.
Conclusions.
Three diagnostic codes used for case finding detect approximately one-quarter of ED- and hospital-treated victims, complement surveys, and facilitate description of injured victims.
Violence by intimate partners is a significant public health problem. In response to a national survey, 25% of U.S. women and 8% of U.S. men aged ≥18 years reported rape or assault by an intimate partner during their lifetime; in 1995–1996, 1.5 million (1.5%) U.S. women reported such violence within the previous 12 months. Approximately 40% of female intimate partner violence (IPV) victims reported having been physically injured, and one-third of these sought medical care.1 The Centers for Disease Control and Prevention (CDC) estimates that $4.1 billion is spent annually on medical care for IPV injuries to women aged ≥18 years; hospitalizations account for the majority of these costs.2
Accurate surveillance methods are integral to building public health programs that aim to limit the burden of IPV.3 Surveillance for IPV is hampered by social stigma, victim reticence to disclose (often based on fears of additional victimization), poor documentation, lack of universal screening, and lack of a gold standard for IPV.4 Current estimates are based primarily on periodic surveys.1,5–9 However, these surveys are typically anonymous, and responses are unverifiable and impossible to link to other information sources. Complementary data sources such as social service, law enforcement, medical examiners, and hospitals and emergency rooms present opportunities to supplement surveys.4,10,11
Data from ED and hospital records offer potentially unique contributions to IPV surveillance. Incidents resulting in ED or hospital care represent particularly severe cases; even small reductions in this subset of IPV would likely result in disproportionate decreases in societal cost and suffering. Moreover, medical record data, in contrast to anonymous surveys, permit identification of victims who might benefit and delivery of effective individual interventions should they be considered by a hospital or public health agency. In addition to Oregon, other U.S. states have embarked upon hospital and ED record surveillance for IPV, but have published only limited descriptions of victims, evaluations of methodologies, scope of victim injuries, or estimates of risks for hospitalization.11–13
In 2000, CDC funded a project wherein Oregon's Department of Human Services Injury Prevention and Epidemiology Program used diagnostic codes to identify possible IPV cases. The objectives of the present study were to: (1) estimate the sensitivity and predictive value positive (PVP) of various diagnostic codes used to screen for IPV cases seen in all Oregon hospitals and EDs, (2) estimate statewide incidence of ED visits and hospitalization for IPV, and (3) describe IPV victims and episodes.
METHODS
Study population and data source
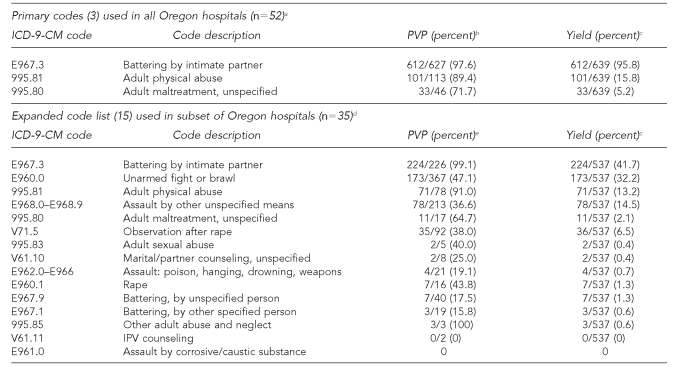
The study population included adolescents (aged ≥12 years) and adults seeking care in Oregon hospitals during 2000. We asked all 58 non-federal Oregon hospitals providing ED or inpatient care to adults during 2000 to make available for review all medical records listing any of three International Classification of Diseases—Clinical Modification, 9th Edition (ICD-9-CM) codes (primary codes) deemed predictive of IPV14–16 for patients aged $12 years seen during 2000 (Table 1). We reviewed electronic or paper records onsite at each hospital. In addition, we asked hospitals to provide all medical records for episodes that did not list one of the primary codes but did list any of 12 additional ICD-9-CM codes (provisional codes) deemed possibly predictive of IPV (Table 1). External cause of injury codes (E-codes) comprised one of the three primary codes and eight of the 12 provisional codes. The use of E-codes is not mandatory in Oregon.
Table 1.
Predictive value positive for IPV and case yield of ICD-9-CM case finding codes in Oregon hospitals, 2000
aFive hospitals that agreed to participate had no eligible records.
bThe PVP of three primary codes combined was 94.5% (639/677).
cYield is proportion of confirmed IPV episodes identified by code(s) out of total confirmed episodes identified by all case finding codes.
dThirty-five hospitals submitted charts listing any code from an expanded list of 15 codes or closely related groups of codes.
eThe PVP of 12 provisional ICD-9-CM codes combined was 35.6% (291/823).
IPV = intimate partner violence
ICD-9-CM = International Classification of Diseases, 9th Edition, Clinical Modification
PVP = predictive value positive
The Program Managers Committee of the Oregon Department of Human Services Office of Disease Prevention and Epidemiology and the Associate Director for Science of the Office of Workforce and Career Development at CDC reviewed the protocol before implementation. Both determined the investigation to be evaluation of public health surveillance, not requiring human subjects committee review.
Case definition
Possible case patients were patients aged ≥12 years who were seen in a participating Oregon hospital during 2000 and whose medical record listed at least one of the three primary or 12 provisional case finding codes. Confirmed cases were those in which an abstractor's review of available medical records confirmed that the visit resulted from intentional physical or sexual assault by a current or former spouse, nonmarital partner, or dating partner.
System attributes
To determine sensitivity of medical record review in detecting women who sought ED care for IPV-related complaints, we divided the number of confirmed female victims of ≥1 assault by a denominator of all IPV victims predicted to have sought care at least once during calendar year 2000 in Oregon. We determined the predicted number of victims during 2000 using estimates from a statewide, population-based, stratified, random telephone survey conducted in Oregon during 2001 and 2002.17 Survey investigators asked women aged 20–55 years whether they had been physically or sexually assaulted by an intimate partner within the preceding year, whether they had sought care in an ED or been hospitalized, and whether they had disclosed the true source of the injuries and the nature of the relationship to the perpetrator. Although hospital and ED cases in all people aged ≥12 years were included in medical record surveillance, for sensitivity estimates, we only considered incidents involving females aged 20–55 years, to coincide with the telephone survey population.
We defined PVP for each individual ICD-9-CM code and for the combined groups of primary and provisional codes as the number of confirmed cases divided by possible cases listing the code or codes. We also defined code “yields” for individual codes and groups of codes as the fraction of all confirmed cases identified by that code or group of codes.
Patient characteristics
One of the investigators (LD) trained the sole record abstractor. She used a standard form to systematically collect patient demographics (name, age, sex, marital status, race, Hispanic ethnicity, and number of children in the household), admission information (emergency or inpatient department status, and admission and discharge dates), incident information (physical and/or sexual violence, location, and weapon use), perpetrator information (gender and relationship to victim), and patient medical information (pregnancy status, referrals, evidence of prior visits for IPV, prolonged recovery or disability >3 months, and complete list of ICD-9-CM discharge diagnosis codes) as recorded in the medical record of all confirmed cases. Record review was completed in 2003.
We calculated incidence of ED care and hospitalization for IPV along with 95% confidence intervals (CIs) by age group, race, and ethnicity using categorical population estimates from the 2000 U.S. Census.18 We also calculated incidence rate ratios and 95% CIs using victims aged ≥50 years, white victims, and non-Hispanic victims as reference groups. We calculated relative risk for hospitalization for age group, race, and natural groupings of common concurrent diagnoses including co-morbid mental or medical illness, scrapes, bruises or strains, and overdose. Because of limited numbers, males were not included in rate estimates.
We described confirmed victims and episodes identified by the three primary ICD-9-CM case finding codes applied in all hospitals and compared them with those identified by the 12 provisional codes (Table 1). We estimated statistical significance of categorical differences among victims identified by primary or provisional codes using the Chi-square test. In circumstances whereby a victim was seen on multiple occasions for separate and distinct episodes during the year, we only included characteristics of the first chronologic episode during 2000. Data were analyzed using SAS® software.19
RESULTS
Hospitals
Fifty-two of the 58 (90%) Oregon hospitals provided records; five small hospitals declined to participate because they lacked convenient methods to review and select records. We excluded one additional hospital because we could not identify qualifying records from the list provided. These 52 hospitals accounted for 884,291 (91.4%) of 967,532 ED visits and 307,522 (94.9%) of 324,156 acute hospital discharges in Oregon during 2000. Of the 52 hospitals that submitted satisfactory records, five small hospitals had no records with qualifying codes, leaving 47 with ≥1 qualifying record for review and analysis. Of these 47, 35 hospitals also provided additional medical records that listed any of the 12 provisional ICD-9-CM case finding codes.
Sensitivity
We identified 677 possible cases by the three primary codes in all 47 hospitals during 2000, and confirmed 639 (94.4%) episodes involving 616 unique victims. In the subset of 35 hospitals that identified charts containing any of the three primary codes plus additional charts containing any of the 12 provisional codes, we identified 1,084 possible cases and confirmed 537 (49.5%) of these.
Based on estimates derived from the 2001–2002 statewide telephone survey, we estimated that 2,371 unique female IPV victims aged 20–55 years were treated in an ED or hospital for physical or sexual assault by an intimate partner at least once during 2000. Seventy-four percent of women who sought care for physical assaults and 56% of women who sought care for sexual assaults reported having disclosed the source of the injuries to the health-care provider. Review of medical records containing any of the three primary codes at all 47 participating hospitals identified 535 confirmed female victims in this age group. Thus, 535 (22.6%) of 2,371 women estimated to have been seen in statewide EDs or hospitalized during 2000 were detected using the three primary case finding codes. In the 35 hospitals where provisional case finding codes were also applied, we identified 203 (44.3%) of 454 female victims aged 20–55 years via one of the primary codes, and the remaining 251 via a provisional code. Extrapolation to all 47 participating hospitals suggests that universal use of the expanded code list would have resulted in detection of 1,208 victims and overall sensitivity of 50.9%.
PVP
The presence of ≥1 of the three primary codes had a PVP for confirmed IPV of 639/677 (94.4%) (Table 1). Of 38 episodes coded with any of the three primary codes for which IPV could not be confirmed, 26 were assaults perpetrated by someone other than an intimate partner, seven represented follow-up care for an earlier episode, and six were possible IPV cases for which insufficient information was available to definitively establish the perpetrator as an intimate partner. Case yield for individual codes was highest (95.8%) for E967.3, “battering by an intimate partner.” In the 35 hospitals also submitting records with provisional codes, PVP for these 12 codes ranged from 0 of 2 for code V61.11 (“IPV counseling”) to 173 of 367 (32.2%) for code E960.0 (“unarmed fight or brawl”). Among confirmed IPV cases from this subset of hospitals, 246 of 537 (45.8%) contained any of the three primary codes, with collective PVP of 94.3% (246/261), whereas the additional 12 codes identified 291/537 (54.3%) of confirmed episodes with collective PVP of 35.6% (291/823). Combined, the 15 primary and provisional codes used in the subset of 35 hospitals had a collective PVP of 49.5% (537/1,084).
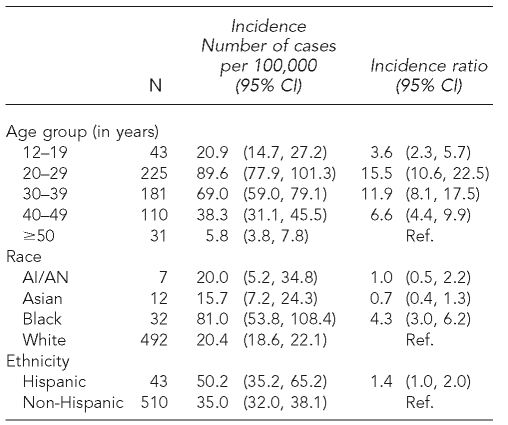
Patient characteristics
Of 616 identified victims seen during 2000, 597 (96.9%) were treated once, 15 (2.4%) twice, and four (0.7%) three times during the year for confirmed IPV episodes. Female victims represented 590 (95.8%) of the cases. Annual incidence was highest among women aged 20–29 years and decreased with age (Table 2).
Table 2.
Incidence of emergency department or inpatient hospital care for IPV by age group, race, and ethnicity—females, Oregon, 2000
IPV = intimate partner violence
CI = confidence interval
AI/AN = American Indian/Alaska Native
Ref. = reference group
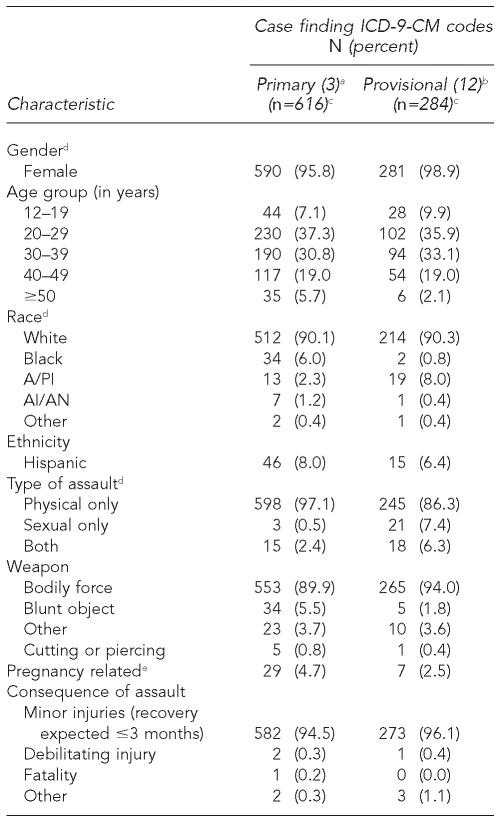
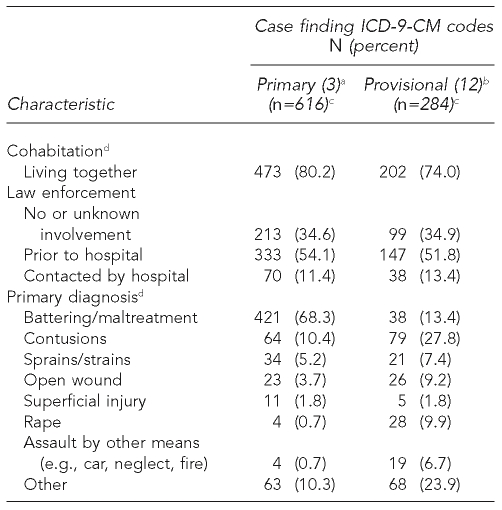
Table 3 lists characteristics of victims and the first episode during 2000 involving each victim for cases identified by primary or provisional codes. Victims were predominantly female and white. Most assaults were not sexual, involved no weapons other than bodily force, and did not result in expected prolonged recovery or long-term disability. The majority of victims lived with the perpetrator. Law enforcement was involved in approximately one-half of cases prior to the ED visit.
Table 3.
Characteristics of confirmed victims and episodes of IPV seen in Oregon hospital emergency or inpatient departments
aThree primary codes (E967.3, 995.81, and 995.80) applied in all 52 participating hospitals.
bTwelve provisional codes (E967.3, E960.0, 995.81, E968.0–E968.9, 995.80, V71.5, 995.83, V61.10, E962.0–E966, E960.1, E967.9, E967.1, 995.85, V61.11, E961.0) applied in the subset of 35 participating hospitals.
cColumn subtotals by category may not sum to this value because of missing values.
dP<0.05 for Chi-square test comparing distribution of victims identified using primary codes compared with victims identified using provisional codes.
eAbsence of information about contemporaneous pregnancy was treated as “not pregnancy related.”
IPV = intimate partner violence
ICD-9-CM = International Classification of Diseases, 9th Edition, Clinical Modification
A/PI = Asian/Pacific Islander
AI/AN = American Indian/Alaska Native
Victims identified by using one of the 12 provisional codes were more likely than those identified by the three primary case finding codes to be Asian or Pacific Islander and less likely to be black, although numbers in these categories were limited. They were also more likely to have suffered a sexual assault, less likely to have been assigned a primary diagnosis consistent with battering or maltreatment, and less likely to live with the perpetrator. Comparison of characteristics of single-episode with multiple-episode victims revealed no significant differences (data not shown). Approximately half of the records reviewed contained explicit information about the number of children living in the household or about previous history of IPV (data not shown). Among victims for whom this information was available, two-thirds were living with at least one child in the household and more than 90% had experienced previous IPV by the same or another perpetrator (data not shown).
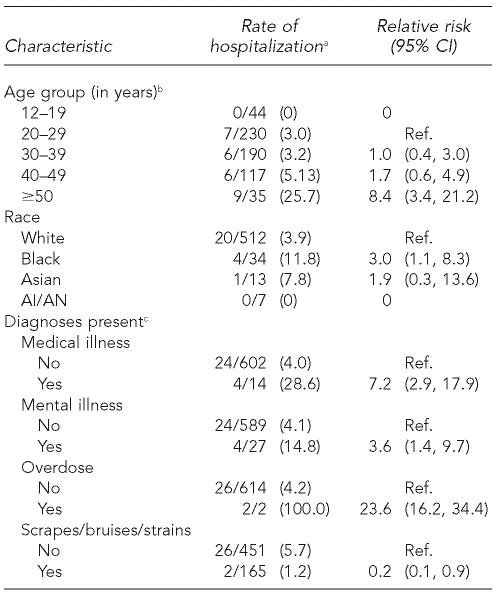
Risk for hospitalization
Twenty-eight of 616 (4.5%) victims identified by primary case finding codes were hospitalized during their first IPV-related visit to an ED or hospital, and two additional victims were hospitalized during a subsequent episode in 2000. Table 4 lists factors associated with hospitalization. Risk for hospitalization increased significantly for female victims aged ≥50 years. Black victims and those with an ICD-9-CM code indicating a comorbid systemic medical or mental diagnosis or an overdose were more frequently hospitalized. Neither victim gender, ethnicity, type of assault, cohabitation status, previous history of IPV, involvement of law enforcement, number of children, nor use of a weapon other than bodily force was associated with hospitalization.
Table 4.
Medical record review, 2000: victim characteristics and circumstances of IPV episodes associated with hospitalization
aTwenty-eight of 616 victims hospitalized. Analysis included only first IPV episode during 2000 for 19 victims treated >1 time during 2000.
bChi-square test for trend: p<0.001
cReference group refers to those without diagnosis.
IPV = intimate partner violence
CI = confidence interval
AI/AN = American Indian or Alaska Native
Ref. = reference group
DISCUSSION
Our evaluation demonstrated that three ICD-9-CM case finding codes detected with high specificity nearly one-quarter of all female Oregon IPV victims aged 20–55 years estimated to have sought hospital or ED care in 2000. The addition of 12 provisional codes doubled sensitivity but reduced PVP from 95% to <50%. Highest incidence occurred in women aged 20–29 years, but hospitalization risk increased among victims who were black, aged ≥50 years, or had comorbid illness.
This study provided the first estimate of sensitivity of diagnosis codes using population-based survey data to estimate the true number of victims treated in EDs and/or hospitalized for IPV-related injuries. Although sensitivity of ED record review for other types of injuries (e.g., firearm-related) may exceed 70%,20,21 IPV is more difficult to detect because of nondisclosure from shame or fear; lack of inquiry,5 recognition, and/or proper documentation by health-care providers; and absence of discrete physical signs or specific clinical presentations. Indeed, among the survey respondents who reported seeking ED or hospital care for a past-year assault, only 56% (sexual assaults) to 74% (physical assaults) said that they had disclosed to the medical perpetrator that the injury had been perpetrated by an intimate partner. Short lists of IPV case finding questions have 65% to 71% sensitivity when compared with longer validated questionnaires in randomly selected women.22 However, this method requires that trained personnel be available to interview patients and depends upon willingness to divulge IPV in the ED setting.
Sensitivity is also affected by coding practices. Investigators elsewhere have found that both E-codes and standard ICD-9-CM codes for abuse (e.g., 995.85) are underused in IPV cases.14,23 Although case finding codes were not restricted to E-codes in this study, a single E-code (E967.3) (identifying an intimate partner as the perpetrator of an assault) identified nearly 96% of confirmed IPV cases detected using the three primary codes. However, E-code use is not mandated in Oregon, and epidemiologists have determined that an appropriate E-code is used for only 65% of injuries (Personal communication, J. Alexander, Oregon Injury Prevention Epidemiology Program, August 2004). Nonetheless, monitoring IPV using a short list of diagnostic codes appears to be a relatively sensitive and cost-efficient method of detecting trends, describing victims and perpetrators, and directing interventions to those at greatest risk for harm.
High PVP of the short list of case finding codes is not surprising because two of the codes, 995.81 (“adult physical abuse”) and E967.3 (“battering by intimate partner”) are intended for use in the setting of IPV.23 Use of 12 additional provisional codes increased sensitivity as expected, but reduced specificity to approximately 50%. Probably because of the nature of the codes involved, cases identified using the provisional codes were more likely than those identified using the three primary codes to involve a sexual assault and a primary diagnosis of something other than battering or maltreatment.
In this study, incidence of IPV leading to ED and/or hospital treatment was highest in women aged 20–29 years or black, and most assaults did not involve weapons. These findings are consistent with those of previous national surveys, including the National Violence Against Women Survey and the National Crime Victimization Survey, and medical record review of violence treated in emergency rooms.1,9,24 However, characteristics of female victims at greatest risk for hospitalization after an episode of IPV are new. Whereas overall IPV rates were highest among women aged 20–29 years, relative risk of hospitalization was significantly higher for women aged ‒50 years. Rate of hospitalization was also significantly higher for black women and for those with comorbid medical or mental illness or a drug overdose. Together, these findings support the assertion that although IPV rates decrease with age, as women age they might suffer more serious consequences when assaulted. Vulnerability to injury could explain a higher inpatient-to-outpatient-care ratio among older victims, but this association also suggests the possibility of survivor bias (i.e., those who stay with violent partners longer might risk increasingly violent assaults).
Why relative risk of hospitalization might be higher for black victims is unclear. Previous studies conflict on whether black victims are at greater risk for IPV than white victims.1,9,15 In addition to the possibility of actual differences in frequency or severity of IPV by race, this finding may reflect cultural differences in willingness to disclose or seek assistance for IPV injuries; use of the ED as a source of primary care; or social, geographic, or financial factors important in the decision to seek medical care and/or to hospitalize an IPV victim.
Limitations
This study has several limitations. Small numbers of non-white and hospitalized victims precluded precise estimates of rates by race and multivariate analysis of risk factors for hospitalization. Race/ethnicity as recorded in the medical record was not uniformly determined. Sometimes, these may have been determined by patient self-report, observed by the clinician or clerk, transferred from another document, or even inferred from a surname. To the extent that ethno-racial misclassification was nonrandom, observed differences in incidence and hospitalization by race or ethnicity should be interpreted with caution. This study also lacked information about perpetrators, a general limitation shared by many IPV studies. In addition, using just three case finding codes maximized specificity but might have distorted the description of IPV victims. One 2004 study determined that the use of codes that specify the relationship to the perpetrator (e.g., E967.3), in addition to being infrequent, was also associated with patient characteristics.23 In our study, differences were observed between victims identified by the short and expanded code lists.
Also, because an agreed-upon gold standard for IPV treated in acute care hospitals was lacking, denominator estimates for sensitivity calculations were based on extrapolation from estimates obtained from a telephone survey. To the degree that respondents underreported IPV or hospital care for IPV injuries, the true number of victims seeking ED care used in the denominator of the sensitivity calculation might have been underestimated. However, the results of the 1994 national study can be used to predict a rate of 306 IPV-related injuries seen in EDs per 100,000 women aged 20–55 years and support the estimate of 276 per 100,000 Oregon women used in this study.25
CONCLUSION
Accurate surveillance methods are a necessary component of programs that aim to prevent IPV. A short list of three ICD-9-CM case finding codes identifies nearly one-quarter of all victims seen in EDs and hospitals, minimizing false positives such that confirmatory medical record review is unnecessary. Subsequent medical record review could be used to confirm IPV, describe injured victims, and evaluate additional diagnostic codes for potential use in routine surveillance without confirmation by chart abstraction. An expanded list of codes increases sensitivity at the expense of false positives. Universal, appropriate use of diagnostic abuse and perpetrator E-codes would increase detection. Should a hospital public health agency contemplate individual intervention on the basis of an IPV specific in the medical record, codes with low yields and/or low specificity would be of diminishing utility.
Acknowledgments
The authors thank LeAnne Mederios, Program Manager of the Oregon Intimate Violence Program, who oversaw day-to-day operation of intimate violence surveillance from 2000 to 2005; Margaret Rhulin, Medical Records Consultant, who abstracted all medical record data; and Lisa Millet, Injury Prevention and Epidemiology Section Manager at the Oregon Department of Human Services, who provided comments on the article.
Footnotes
The Oregon IPV Surveillance Project was funded by Centers for Disease Control and Prevention, Cooperative Agreement IPV Surveillance U17/CCU019413.
REFERENCES
- 1.Tjaden P, Thoennes N. Extent, nature, and consequences of intimate partner violence: findings from the National Violence Against Women Survey. Washington: Department of Justice, National Institute of Justice (US); 2000. [Google Scholar]
- 2.National Center for Injury Prevention and Control (US) Costs of intimate partner violence against women in the United States. Atlanta: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (US); 2003. [Google Scholar]
- 3.Saltzman LE, Green YT, Marks JS, Thacker SB. Violence against women as a public health issue: comments from the CDC. Am J Prev Med. 2000;19:325–9. doi: 10.1016/s0749-3797(00)00241-5. [DOI] [PubMed] [Google Scholar]
- 4.Saltzman LE, Fanslow JL, McMahon PM, Shelley GA. Intimate partner violence surveillance: uniform definitions and recommended data elements. Atlanta: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (US); 1999. [Google Scholar]
- 5.Abbott J, Johnson R, Koziol-McLain J, Lowenstein SR. Domestic violence against women: incidence and prevalence in an emergency department population. JAMA. 1995;273:1763–7. doi: 10.1001/jama.273.22.1763. [DOI] [PubMed] [Google Scholar]
- 6.Lifetime and annual incidence of intimate partner violence and resulting injuries—Georgia, 1995. MMWR Morb Mortal Wkly Rep. 1998;47(10):849–53. [PubMed] [Google Scholar]
- 7.Prevalence of intimate partner violence and injuries—Washington, 1998. MMWR Morb Mortal Wkly Rep. 2000;49(26):589–92. [PubMed] [Google Scholar]
- 8.Use of medical care, police assistance, and restraining orders by women reporting intimate partner violence—Massachusetts, 1996–1997. MMWR Morb Mortal Wkly Rep. 2000;49(22):485–8. [PubMed] [Google Scholar]
- 9.Rennison CM. Intimate partner violence and age of victim, 1993–99. Washington: Department of Justice, Office of Justice Programs (US); 2001. Oct, [Google Scholar]
- 10.Building data systems for monitoring and responding to violence against women: recommendations from a workshop. MMWR Recomm Rep. 2000;49(RR-11):1–18. [PubMed] [Google Scholar]
- 11.Orchowsky S, Weiss J. Domestic violence and sexual assault data collection systems in the United States. Violence Against Women. 2000;6:904–11. [Google Scholar]
- 12.Biroscak BJ, Smith PK. Intimate partner violence against women in Michigan: findings from emergency department surveillance—1999–2000. Lansing (MI): Michigan Department of Community Health and Michigan Public Health Institute; 2003. Aug, [Google Scholar]
- 13.Intimate partner violence injuries—Oklahoma, 2002. MMWR Morb Mortal Wkly Rep. 2005;54(41):1041–5. [PubMed] [Google Scholar]
- 14.Rovi S, Johnson MS. Physician use of diagnostic codes for child and adult abuse. J Am Med Womens Assoc. 1999;54:211–4. [PubMed] [Google Scholar]
- 15.Rudman WJ, Davey D. Identifying domestic violence within inpatient hospital admissions using medical records. Women Health. 2000;30:1–13. doi: 10.1300/J013v30n04_01. [DOI] [PubMed] [Google Scholar]
- 16.Waller AE, Martin SL. Health related surveillance data on violence against women. Violence Against Women. 2000;6:868–903. [Google Scholar]
- 17.Oregon Department of Human Services Office of Disease Prevention and Epidemiology. Intimate partner violence in Oregon: findings from the Oregon Women's Health and Safety Survey. Oregon Department of Human Services, Injury Prevention and Epidemiology Program. [cited 2004 May 5]. Available from: URL: http://www.governor.state.or.us/DHS/ph/ipv/survey.shtml.
- 18.American Factfinder. U.S. Census Bureau. [cited 2004 Jul 15]. Available from: URL: http://factfinder.census.gov.
- 19.SAS Institute Inc. SAS: Version 8.0. Cary (NC): SAS Institute Inc.; 2001. [Google Scholar]
- 20.Archer PJ, Mallonee S, Schmidt AC, Ikeda RM. Oklahoma firearm-related injury surveillance. Am J Prev Med. 1998;15:83–91. doi: 10.1016/s0749-3797(98)00054-3. [DOI] [PubMed] [Google Scholar]
- 21.LeMier M, Cummings P, Keck D, Stehr-Green J, Ikeda R, Saltzman L. Washington state gunshot-wound surveillance system. Am J Prev Med. 1998;15(3) Suppl:92–100. doi: 10.1016/s0749-3797(98)00053-1. [DOI] [PubMed] [Google Scholar]
- 22.Feldhaus KM, Koziol-McLain J, Amsbury HL, Norton IM, Lowenstein SR, Abbott JT. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. JAMA. 1997;277:1357–61. [PubMed] [Google Scholar]
- 23.Weiss HB, Ismailov RM, Lawrence BA, Miller TR. Incomplete and biased perpetrator coding among hospitalized assaults for women in the United States. Inj Prev. 2004;10:119–21. doi: 10.1136/ip.2003.004382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coding Clinic for ICD-9-CM. Vol 13. Chicago: American Hospital Association; 1996. [Google Scholar]
- 25.Rand MR. Violence-related injuries treated in hospital emergency departments. Washington: Department of Justice, Office of Justice Programs (US); 1997. Aug, NCJ-156921. [PubMed] [Google Scholar]