This article presents a comparative analysis of the age-adjusted incident and mortality cancer rates in the European Union (EU) and Poland, and measures taken by Polish authorities against cancer diseases. The main purpose of this study was to provide 2001–2006 cancer data regarding Poland and EU countries to researchers, policy makers, and the public to raise awareness of cancer problems worldwide and in Europe and to use it as a baseline for evaluating further progress of the Polish health policy's efficiency against cancer diseases.
BACKGROUND
Cancer is the second-leading cause of death worldwide (cardiovascular disease is number one). Cancer accounted for 7 million deaths in 2000 and it is expected to account for approximately 10 million deaths in 2020. In Poland, there were 130,000 new cases of cancer and 85,000 deaths from cancer in 2000, and there will be an estimated 160,000 new cases of cancer and 100,000 deaths attributable to cancer in 2010 if the present trends continue. In 2002, 22.4 million people were living with cancer worldwide and 600,000 were living with cancer in Poland. Considering that Poland's population size is 38,518,241, cancer is responsible for 25% of all causes of deaths.1 In 2005, 300 Polish inhabitants were diagnosed each day with cancer and 220 died of cancer, which is equal to 12 new incident cases and nine deaths per day.2
In Poland, the percentage of people undergoing medical treatment during the very early stages of cancer is still very low (20%), while in the U.S. the percentage is much higher (80%). This is mainly due to the widespread promotion of methods of complementary and alternative medicine (i.e., phytotherapy, bioenergotherapy, homeopathy, acupuncture, clairvoyance). According to medical science, such methods should be treated as supportive rather than basic treatments. Approximately 5,000 deaths are recorded annually in Poland as a result of the avoidance of treatment or a delay in treatment. On average, every fourth patient delays treatment for five to six months.2 Both in Poland and in the U.S., a considerable amount of money is designated for complementary and alternative medicine therapies: $30 billion in the U.S. and $1 billion in Poland annually.3
Poland has a poor record in terms of the percentage of cases of complete recovery after oncology treatment. In 2003, cancer survival rates were as follows: 30% in Poland, 45% in the EU, and 60% in the U.S.4,5
EPIDEMIOLOGIC SITUATION
The age-standardized incidence and mortality rates in 2002 for the 15 countries that originally formed the EU (Austria, Belgium, Germany, the Netherlands, Luxemburg, Denmark, Greece, Italy, Portugal, France, Spain, Great Britain, Ireland, Finland, and Sweden) and for Poland were extracted from GLOBOCAN 2002, a project of the International Agency for Research on Cancer.1 Polish and EU incident and mortality rates in 2006 were derived from the Boyle and Ferlay best estimates for Europe.6
The primary types of cancer with the highest age-adjusted incidence rates in 2002 were breast, colorectal, and lung cancer in the 15 EU countries; and lung, colorectal, and breast cancer in Poland. In 2006 in the EU, the most common form of cancer was prostate cancer followed by breast and colorectal cancers. In Poland, the most frequent types were lung, breast, and colorectal cancers.
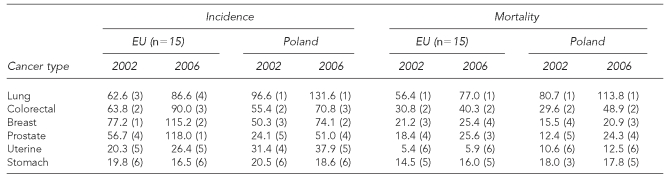
All cancer incident and mortality rates increased in 2006 compared with 2002, both in the EU and in Poland. The highest mortality rates were due to the same causes in the time period 2002–2006 for lung, colorectal, and breast cancers alternately in the EU and in Poland (Table 1).
Table 1.
Age-standardized incidence and mortality rates in the EU and Poland per 100,000 people, in 2002 and 2006, by site and year (both sexes combined)
EU = European Union
In 2002 and 2006, breast cancer was by far the most frequent cancer diagnosed among women in the EU and Poland, and higher breast cancer incident and mortality rates were recorded among women in the EU than in Poland. Breast cancer remains the leading cause of death and it is crucial to organize immediate population programs promoting breast self-examination and facilitating access to mammography screenings. In 2002, colorectal and uterine cancers were the second and third most common forms of cancer among women in the EU, while uterine cancer was the second major threat for women in Poland. This is mainly because women from EU countries are more aware of the necessity to conduct cervical screening tests. Such tests have proven to be an effective and improved way to detect cancer in an early (curable) stage of the disease.7
In 2006, the incident rates of all cancer types (excluding stomach cancer) among women were slightly higher in Poland and in the EU than in 2002, but lung cancer started to be more of a health hazard for women in Poland, with a doubled incident rate at 28.6 in 2006 compared with an incident rate equal to 14.6 in 2002. Polish women also continued to have the highest mortality rate due to lung cancer in 2006. Despite various tobacco-control policies (i.e., raising taxes on tobacco products, restricted access to tobacco products for people younger than age 18, a ban on tobacco advertising),8 there are still many women in Poland who smoke (Tables 2 and 3).
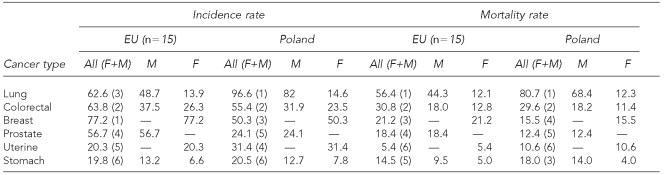
Table 2.
Age-standardized incidence and mortality rates in the EU and Poland per 100,000 people, by site and sex, in 2002
EU = European Union
F = female
M = male
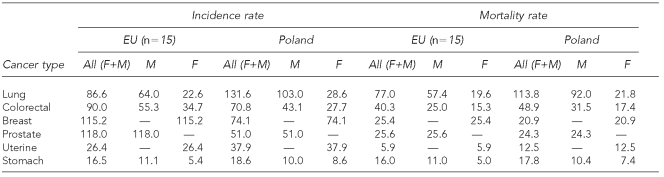
Table 3.
Age-standardized incidence and mortality rates in the EU and Poland per 100,000 people, by site and sex, in 2006
EU = European Union
F = female
M = male
During 2002–2006, lung cancer continued to be the biggest threat for Polish men. In the EU, it was the second most serious health threat after prostate cancer (the incident rates were 56.7 in 2002 and 118.0 in 2006). Mortality rates due to lung cancer were highest in the EU and Poland compared with other cancer types. It is worth emphasizing that tobacco-control programs should be the top priority both in Poland and in the EU. Prostate cancer incident rates in 2006 were much higher than in 2002, and it was the second biggest problem in 2006 for Polish men after lung cancer (with incidence rates of 24.1 in 2002 and 51.0 in 2006). These figures seem to be the result of a rapid increase of the number of men aged 65 and older both in Poland and the EU (Tables 2 and 3).
Colorectal cancer incident rates for Polish men were similar to the corresponding rates for the EU, while mortality rates of men in Poland were slightly higher. An increase of colorectal cancer incident and mortality rates was observed in 2006 compared with 2002. There is a need to take measures aimed at improving the effectiveness of colorectal screenings, increasing physical activity, and modifying dietary habits. Significant progress has been observed in the case of stomach cancer where dietary modifications, better food preservation, and treatment of the Helicobacter pylori infection led to a decrease in the incident and mortality rates.9,10
POLISH POLICY REGARDING CANCER
Polish health-care system
In recent years, the health-care system in Poland has undergone many reforms. Currently it is based on the obligatory public health insurance system. People covered by general health insurance (on a compulsory or voluntary basis) are entitled to free health services by health-care providers who have concluded contracts on providing health services with one of 16 branches of the National Health Fund (NHF) in every voivodship.11 A voivodship is a principal administrative division of a country—much like the states in the U.S. In Poland, there are 16 voivodships. The NHF is the institution responsible for providing and financing health services for insured people within assigned means.
The state budget and units of self-government are other sources of health-care financing. However, in the reformed health-care system, their part in health-care financing is very limited. In general, health insurance premiums for specific groups of the population (i.e., the unemployed receiving social security benefits, people receiving social pensions, farmers, war veterans, and others) and investments in public health-care institutions are financed from those sources. The majority of funds allocated for health program implementation are transferred to the NHF. The state budget funds are used to cover the costs of health-care services provided to uninsured people in life-threatening situations and in case of accidents during childbirth. The Minister of Health may consent to covering the costs of treatment or diagnostic procedures that are not available in the country but performed abroad.12
There is a wide range of health services under the insurance scheme that includes health services aimed at maintaining and restoring human health and preventing diseases, early diagnosis, medical examination and consultation, diagnostic examinations, medical treatment, prevention and alleviation of disabilities, outpatient health care, medical emergency services, medical rehabilitation, nursing, supply of drugs and medical services, supply of orthopaedic devices and aids, perinatal care during pregnancy, palliative care, and certification of temporary or permanent disability.
Due to the wide range of health services, a natural consequence is the formation of queues (i.e., the number of patients and the mean period of waiting for the health service). Regarding oncology patients, the situation is different in every voivodship. The mean waiting time for patients with cancer ranges from several days (for chemotherapy) to one month (for radiotherapy) or three months (for positron emission tomography diagnosis).
Patients can take advantage of free access to hospital care based on a referral from a general practitioner. Patients also have the right to choose a doctor, nurse, midwife, and hospital from all available public (mainly hospitals) and private (individual or group medical practices) health-care providers. The most basic type of organization in the Polish health-care system is the independent health-care institution (HCI), which is completely separate from a founder and dependent only on health insurance contributions. HCIs are the successors of the former Zespol Opieki Zdrowotnej (ZOZ). ZOZs are integrated management units including hospitals, outpatient clinics, specialists, and primary health-care organizations that resemble health maintenance organizations in the U.S.
Polish internal policies for cancer care: international regulations
Poland is a member of the World Health Organization (WHO) and the EU, and its authorities are required to implement the health policies of these two organizations. In 1979, WHO formulated the global strategy “Health for All in the Year 2000,” which included a set of guidelines for other countries to follow to create national strategies and programs as instruments of health policy.13 In 2000, a new strategy known as “Health for All in the 21st Century” (hereafter: “Health 21”) was formulated.14 The program was a continuation of the “Health for All in the Year 2000” global strategy, which drew attention to inequalities in the health status and the problem of unequal access to health services.
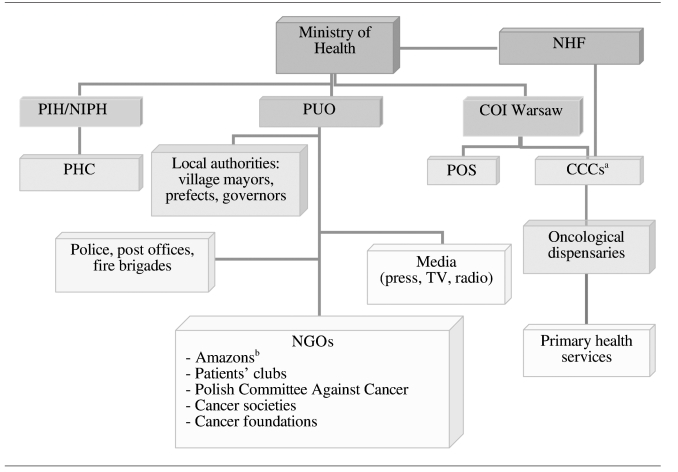
In 1990, Polish policy makers formulated the National Health Program, which aimed to decrease mortality rates of cardiovascular diseases, neoplasms and injuries, accidents, and poisoning (the main causes of death in Poland).15 Regional representatives were appointed in public health centers (PHCs) to initiate, accomplish, and monitor the national health strategy. Poland's health situation was presented at conferences and seminars organized by the National Institute of Hygiene in Warsaw, Poland, which ranks higher than the PHCs (Figure 1).
Figure 1.
Organizational chart of the system of implementation and financing of the National Program Against Cancer Diseases
aCCCs provide overall cancer treatment, including chemotherapy, radiotherapy, and surgery, in one institution.
bThe Amazons Club (women after mastectomy) was inspired by the “Reach to Recovery” movement.
NHF = National Health Fund
PIH/NIPH = Polish Institute of Hygiene/National Institute of Public Health
COI Warsaw = Center of Oncology Institute in Warsaw
PHC = public health center
PUO = Polish Union of Oncology
POS = Polish Oncological Society
NGO = nongovernmental organization
CCC = comprehensive cancer center
The main goals of the Polish policy against cancer specified in the National Health Program in 1990 were as follows:
-
Decrease mortality rates of all types of cancer, especially tobacco-related ones, by 10%. From 1990 to 2002, the following positive trends were noted:
A decrease in the percentage of men who never smoked, from 52% in 1990 to 38% in 2002;
A lower frequency of everyday smoking;
A decrease in the number of smoked cigarettes by women aged 20 to 39 with a higher education; and
A decline in the rate of new smokers and a decrease in the mortality rate of lung cancer in these groups as a result of advantageous changes in the profile of tobacco smoking. But taking into account all age groups, lung cancer is still a serious health hazard, especially for men.15
Improve the methods of early diagnosis and the effectiveness of treating uterine and breast cancers. In Poland, malignant neoplasms are the second-leading cause of death among women, but first among women older than 65 years of age. The biggest dangers for women are breast and uterine cancers. In comparison to other countries, breast cancer morbidity is similar whereas uterine cancer morbidity is alarmingly high in Poland. Regarding uterine cancer, an increase in morbidity and mortality has been observed. Breast cancer is still the biggest killer of women and more and more new incident cases are recorded every year.
This goal will be accomplished by intensifying health education to make women aware of the necessity of breast self-exams, screening mammography, and cervical cytology exams. Research conducted in Poland as well as in other countries during a considerable period of time showed that mortality due to breast and uterine cancers could be decreased by population screening programs (screening mammography and cervical cytology exams).16
From 1990 to 2002, the following positive trends were noted:
The percentage of women conducting breast self-exams increased from 24% in 1998 to 28% in 2001.
The awareness of the necessity of screening mammography exams increased from 31% in 1998 to 52% in 2001.
The percentage of women who had prophylactic mammography exams performed increased from 10.0% in 1998 to 27.8% in 2001.
However, despite some positive changes in the health behavior of women, the problem is still very serious mainly due to ineffective primary prevention because of its slight effect on the disease; insignificant improvement of the five-year survival rate; and insufficient secondary prevention due to deficiencies in diagnostic and treatment standards and underuse of mammography and cytology as screening tools.
In light of the emergency situation concerning mortality and morbidity rates of cancer, on July 1, 2005, the Polish government enacted a bill implementing the National Program Against Cancer Diseases (NPACD) for the years 2005 to 2010.17 The government designated approximately $1 billion for the program (or about $250 million/year). Furthermore, a number of institutions were founded to implement, coordinate, and evaluate the NPACD (Figure 1).
The main coordinating and supervising institutions are the Ministry of Health and the Polish Union of Oncology. The Ministry of Health enacted a bill on the NPACD, but the Polish Union of Oncology was the first institution to initiate discussions about the program's necessity. The NHF is responsible for financing the program and cooperating with the health-care providers. The Center of Oncology Institute in Warsaw is the primary institution for treating cancer patients from the whole country. Comprehensive cancer centers supply health services in all of the 16 voivodships. Oncology dispensaries and primary health-care physicians provide screening services, early diagnosis, and treatment of oncology patients.
The Polish Union of Oncology cooperates with a wide range of institutions from outside the health sector, including the press, TV stations, radio, local authorities, nongovernmental organizations, police, the post office, and fire brigades. The Polish Oncological Society is responsible for creating oncology guidelines and integrating medical professionals.
PHCs in every voivodship are responsible for preparing reports about the health situation in a given unit of self-government. The Polish Institute of Hygiene/National Institute of Public Health performs the same function on a countrywide scale, making reports about the health status of Polish citizens and organizing conferences and seminars.
The main goals of the NPACD are:
Prevent new cancer incidents and mortality rates from growing.
Achieve the level of the European indicators of early cancer diagnosis and treatment.
Take advantage of the most recent research findings and achievements of cancer aetiopathology.
Implement methods of early diagnosis and treatment.
Monitor the efficacy of activities against cancer diseases in Poland.
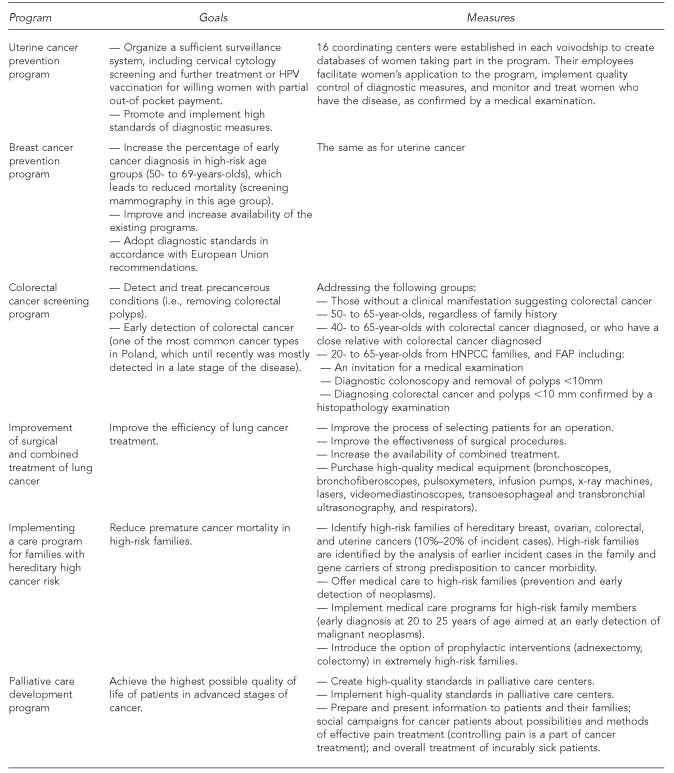
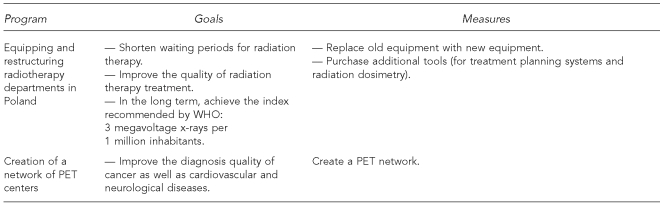
The main programs, their goals, measures taken, and entities responsible for the implementation, assessment, and evaluation are listed in Figure 2.
Figure 2.
The main activities of the National Program Against Cancer Diseasesa
aFor all programs, implementation is provided by health-care providers who have concluded contracts with the National Health Fund (i.e., individual and group medical practices, independent health-care institutions) and assessment and evaluation is conducted by the Ministry of Health and Polish Union of Oncology.
HPV = human papillomavirus
PET = positron emission tomography
WHO = World Health Organization
FAP = familial adenomatous polyposis
HNPCC = hereditary nonpolyposis colorectal cancer
As a member of the EU, Poland conforms to the European Cancer Code.18,19 Its essential tenets are:
-
Many aspects of general health can be improved, and certain cancers avoided, if a healthier lifestyle is adopted. The following guidelines should be followed:
—Do not smoke. If you smoke, stop doing so. If you fail to stop, do not smoke in the presence of nonsmokers.
—Avoid obesity and maintain a body mass index of 18.5 to 25 kg/m2.
—Undertake brisk, physical activity every day; a minimum of half an hour per day three times per week.
-
—Increase your daily intake and variety of vegetables and fruits. Eat at least five meals daily. Limit your intake of food containing fats from animal sources.
A diet based on the five-a-day rule (minimum 400 g/day, i.e., two pieces of fruit and 200 g of vegetables) is promoted in the campaign.
Fruits and vegetables should be eaten as part of every meal as well as between meals and instead of sweets.
—The consumption of alcohol should be limited to two drinks per day for men and one drink per day for women. One drink is equivalent to one beer, one glass of wine, or one shot of spirits.
-
—Avoid excessive sun exposure.
It is especially important to protect children and adolescents.
For individuals who have a tendency to burn in the sun, active protective measures must be taken throughout their life.
-
—Conform strictly to regulations aimed at preventing any exposure to known cancer-causing substances.
Follow all health and safety instructions enclosed with substances that may cause cancer.
Follow advice from national radiation protection offices.
-
—Participate in vaccination programs against hepatitis B virus (HBV) infection.
In Poland, prophylactic vaccinations are carried out in the following groups: newborns, young people up to 14 years of age, high-risk groups, people close to others with HBV infection, and patients suffering from chronic hepatitis (especially those with hepatitis C virus). Moreover, hospitals in Poland require patients to be vaccinated against HBV infection before an operation. Prophylactic vaccination programs in Poland do not cover vaccinating against HBV infection of people traveling to medium and high endemic regions of HBV infection.
-
Implement public health programs that could prevent cancers from developing and increase the probability of a successful treatment.
Women aged 25 years and older should participate in cervical screenings.
Women aged 50 years and older should participate in breast screenings.
Men and women aged 50 years and older should participate in colorectal screenings.
Implementing European Cancer Code guidelines and raising societal awareness is conducted by a highly qualified medical staff that also cooperates with the media.
Epidemiologic surveys conducted by Doll and Peto in 1981 identified main causes of cancer deaths that could be avoided.20 Based on the current state of knowledge about the causes of cancer, the scientists concluded that a significant part of incident cases (from about 10% to 70%) could be prevented. Percentages of various cancer-causing factors that could be avoided in the U.S., according to Doll and Peto, are:
Tobacco (25% to 40%)
Diet (10% to 70%)
Alcohol (2% to 4%)
Sexual behaviors (1% to 13%)
Occupation (2% to 8%)
Polution: air, water, food (1% to 5%)
Infection: parasites, bacteria, viruses (10%)
Ionizing and ultraviolet light (2% to 4%)
CONCLUSION
Until recently, Poland has had a poor record compared with other EU countries regarding the efficiency of population screening programs. Such a state of affairs is mainly due to health unawareness and health ignorance of Polish society, as well as inadequate participation of primary health-care doctors in health education for the Polish population.
Significant progress in cancer control can be accomplished only by widespread primary prevention programs, population screenings, early diagnosis programs, and improved treatment. It is extremely important to develop existing health promotion programs focusing on healthy lifestyles. Such measures are in conformance with the guidelines of the NPACD and the European Cancer Code.
REFERENCES
- 1.International Agency for Research on Cancer. GLOBOCAN 2002. [cited 2008 Apr 1]. Available from: URL: http://www-dep.iarc.fr.
- 2.Meder J. Oncological issues in the field of public health. Warsaw (Poland): Postgraduate Medical Center and Oncological Center Institute; 2006. [Google Scholar]
- 3.MacLennan AH, Wilson DH, Taylor AW. The escalating costs and prevalence of alternative medicine. Prev Med. 2002;35:166–73. doi: 10.1006/pmed.2002.1057. [DOI] [PubMed] [Google Scholar]
- 4.National Cancer Institute. Surveillance Epidemiology and End Results (SEER) [cited 2008 Mar 30]. Available from: URL: http://seer.cancer.gov/faststats/sites.php?site=All+Cancer+Sites&stat=Survival5rel.
- 5.EUROCARE. Survival of cancer patients in Europe: the EUROCARE-3 Study. [cited 2008 Mar 30]. Available from: URL: http://www.eurocare.it/CDEu3/Index.htm.
- 6.Ferlay J, Autier P, Boniol M, Heanue M, Colombet M, Boyle P. Estimates of the cancer incidence and mortality in Europe in 2006. Ann Oncol. 2007;18:581–92. doi: 10.1093/annonc/mdl498. [DOI] [PubMed] [Google Scholar]
- 7.American Society of Cytopathology. Position statement regarding new technologies in cervical cytology screening. [cited 2008 Apr 1]. Available from: URL: http://www.cytopathology.org/website/article.asp?id=10.
- 8.The Polish Chamber of Physicians and Dentists. Polish tobacco-control policy. [cited 2008 Apr 1]. Available from: URL: www.gazetalekarska.pl/xml/nil/gazeta/numery/n2002/n200203/n20020310.
- 9.Wojtyniak B, Gorynski P. The health situation in Poland and the National Health Program. Reumatologia. 2007;45(1) Suppl 1:5–17. (in Polish) [Google Scholar]
- 10.Mayo Clinic. Stomach cancer. [cited 2008 Apr 1]. Available from: URL: http://www.mayoclinic.com/health/stomach-cancer/DS00301/DSECTION=4.
- 11.Golinowska S CASE Foundation. Polish healthcare system. Forum Ochrony Zdrowia i Nowych Mozżliwości. [cited 2008 Apr 1]. Available from: URL: http://www.qcm2.quicksilver.pl/img/27/Referat%20Stanislawa%20Golinowska.pdf.
- 12.Ministry of Health. [cited 2008 Apr 6]. Available from: URL: http://www.mz.gov.pl.
- 13.World Health Organization. Global strategy for health for all by the year 2000. Geneva: WHO; 1981. [cited 2008 Feb 26]. Also available from: URL: http://whqlibdoc.who.int/publications/9241800038.pdf. [Google Scholar]
- 14.Antezana FS, Chollat-Traquet CM, Yach D. Health for all in the 21st century. World Health Stat Q. 1998;51:3–6. [PubMed] [Google Scholar]
- 15.Department of Medical Statistics, National Institute of Hygiene. Health programme for years 1996–2005. [cited 2008 Apr 1]. Available from: URL: http://www.medstat.waw.pl/nhp_p/1_p.html.
- 16.Hendrick RE, Smith RA, Rutledge JH, III, Smart CR. Benefit of screening mammography in women aged 40 49: a new meta-analysis of randomized controlled trials. J Natl Cancer Inst Monogr. 1997;22:87–92. doi: 10.1093/jncimono/1997.22.87. [DOI] [PubMed] [Google Scholar]
- 17.The Ministry of Health in Poland. The National Program Against Cancer Diseases. [cited 2008 Apr 1]. Available from: URL: http://www.mz.gov.pl/wwwmz/index?mr=q101&ms=&ml=pl&mi=40&mx=0&mt=my=40&ma=04806.
- 18.Europe Against Cancer programme of the European Community. European Code Against Cancer and Science Justification: third version. 2003. [cited 2008 Feb 26]. Available from: URL: http://www.cancercode.org/code_01.htm.
- 19.Zatonski W, editor. European cancer code. Polish edition. Warsaw: Oncological Center Institute; 2007. 3rd version. [Google Scholar]
- 20.Doll R, Peto R. The causes of cancer; quantitative estimates of avoidable risks of cancer in the United States today. J Natl Cancer Inst. 1981;66:1191–308. [PubMed] [Google Scholar]