Abstract
Purpose
To provide normative pediatric visual acuity data using HOTV optotypes presented on the Electronic Visual Acuity Tester following the Amblyopia Treatment Study (ATS) protocol.
Methods
Monocular testing was conducted on 384 healthy full-term children ranging from 3 to 10 years of age (mean, 5.4 years; SD = 1.8 years). A total of 373 children completed monocular testing of each eye. In addition, 23 adults (mean, 28.7 years; SD = 4.9 years) were tested for comparison. Both monocular visual acuity and interocular acuity differences were recorded.
Results
Mean visual acuity improved by slightly more than one line (0.12 logMAR) from 3 years of age to adulthood, increasing from 0.08 logMAR to −0.04 logMAR (F6,400 = 26.3, p < 2.0 × 10−26). At all ages, mean interocular acuity difference was less than one line on a standard acuity chart (overall mean difference = 0.04 logMAR; SD = 0.06 logMAR).
Conclusions
These results represent the first normative data reported for HOTV optotypes using the ATS protocol on the Electronic Visual Acuity Tester. These data may play an important role in clinical practice, screening, and clinical research.
Accurate and reliable measurement of visual acuity in children is essential for the detection and management of pediatric eye disease. Visual acuity is also a desirable outcome measure for pediatric eye research. Yet, though the Early Treatment Diabetic Retinopathy Study (ETDRS) testing protocol is generally accepted as the gold standard of visual acuity measurement in adults,1,2 there is no widely accepted, standardized visual acuity protocol for young children. To remedy this, the Pediatric Eye Disease Investigator Group (PEDIG) has recently developed the Electronic Visual Acuity (EVA) Tester, a computerized testing system that provides automated presentation of letter optotypes (HOTV or ETDRS).3
The EVA testing system offers a number of features that make it particularly suitable for multiple-site, pediatric vision testing. Most importantly, it offers standardization of optotypes, luminance, and testing procedure across sites and requires limited tester training.3,4 For pediatric use, it incorporates the Amblyopia Treatment Study (ATS) visual acuity testing protocol,5 a four-step modified staircase procedure designed to provide quick, accurate, and reliable measurement of acuity. It uses a single optotype presentation format with crowding bars to maximize both testability and sensitivity to amblyopia.6 Recent studies have verified that the testability of preschool- and school-aged children with the EVA testing system is indeed high and that acuity measurements are very reliable.4,5 To date however, there is a lack of normative data for young children tested with the procedure. In the present study, we report normative data for 3- to 10-year-old children and adults assessed with HOTV optotypes using the ATS protocol on the EVA testing system.
Methods
Participants
Participants included 384 children (177 males, 207 females) between the ages of 3.0 and 10.8 years (mean age, 5.4 years; SD = 1.8 years) participating in ongoing studies. All participants were healthy full-term children who possessed no known eye disease. The ethnicity of the study sample was representative of the Dallas-Fort Worth area as a whole, 80% were Caucasian and 20% were minorities (ie, African American, Hispanic). Note that because the children tested represent a convenience sample, the age distribution is not uniform (Table 1). For comparison, 23 young adults (mean, 28.7 years; SD = 4.9 years) were also tested. Informed, written consent was obtained from all adults and the parents of all participants after an explanation of the nature and any possible consequences of the study. The research protocol followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of the University of Texas Southwestern Medical Center.
Table 1.
Mean and 95% tolerance interval for visual acuity and interocular difference categorized by age group. Unless otherwise stated, visual acuity values are presented in logMAR units. Note that the data of 8- to 10-year-old children have been combined due to limited enrollment for this age group.
| Visual acuity
|
Interocular acuity difference (IOD)
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age group (years) | Number of participants | Number of eyes | Mean visual acuity | Mean visual acuity (Snellen) | 95% tolerance interval | Lower limit | Lower limit (Snellen) | Number of participants | Mean IOD | 95% tolerance interval |
| 3 | 37 | 68* | 0.08 | 20/24 | ±0.21 | 0.29 | 20/39 | 31 | 0.03 | ±0.10 |
| 4 | 182 | 360* | 0.08 | 20/24 | ±0.17 | 0.25 | 20/36 | 178 | 0.05 | ±0.12 |
| 5 | 47 | 93* | 0.03 | 20/21 | ±0.19 | 0.22 | 20/33 | 46 | 0.04 | ±0.10 |
| 6 | 34 | 68 | −0.03 | 20/19 | ±0.18 | 0.15 | 20/28 | 34 | 0.02 | ±0.07 |
| 7 | 35 | 70 | −0.02 | 20/19 | ±0.10 | 0.08 | 20/24 | 35 | 0.04 | ±0.14 |
| 8–10 | 49 | 98 | −0.06 | 20/17 | ±0.12 | 0.06 | 20/23 | 49 | 0.02 | ±0.10 |
| Adults | 23 | 46 | −0.04 | 20/18 | ±0.17 | 0.13 | 20/26 | 23 | 0.03 | ±0.09 |
| Total | 407 | 803 | 396 | |||||||
Not all participants could complete testing of both eyes at 3, 4, and 5 years of age.
Electronic Visual Acuity Testing System
Initially, the EVA testing system consisted of a desktop personal computer connected to a handheld Palm operating system (Palm Inc, Santa Clara California) and a 17-inch monitor with 1600 × 1200 pixel resolution. Later in the study, the desktop and monitor were replaced with a Dell Inspiron 6000 laptop computer (Dell Inc., Round Rock, TX) with a 15.4 inch monitor with 1920 × 1200 pixel resolution. Both versions of the test are equipped to present high-contrast (98%) black-and-white HOTV optotypes with a luminance of 85 to 105 cd/m2. Progression of optotype size approximates a logMAR progression and ranges from 20/800 to 20/15. Stimulus presentation and scoring are automated and controlled through the interaction of the Palm operating system and the computer (see Moke et al3 for details). When testing is completed, the participant’s final score is calculated and displayed on the screen of the Palm operating system.
Procedure
For all participants, testing was attempted on each eye monocularly (right eye first) at a viewing distance of 3 meters. Test stimuli consisted of isolated letter optotypes (H, O, T, or V) surrounded by crowding bars spaced at a half-letter width. Upon presentation, the child was asked to identify the optotype verbally. If the child could not do so, he/she was provided with a lap card containing the four letters and was instructed to match the presented optotype to the correct letter on the lap card. As noted above, testing was automated and followed the ATS protocol, a testing procedure developed to provide sensitive, standardized visual acuity testing of children aged 3 to 6 years.5 The protocol consists of four steps: screening, phase 1 (threshold estimation), reinforcement, and phase 2 (threshold estimation). During screening, a single optotype is presented at several consecutive descending logMAR levels beginning at 0.7 logMAR (20/100) or 1.30 logMAR (20/400), until the child commits an identification error. Once an error is committed, phase 1 begins. Starting at 2 optotype levels above the error committed during screening, up to 4 optotypes are presented per level in order of descending logMAR steps. This phase is complete once 2 errors are made at a single level. Next, the reinforcement phase is conducted to maintain the child’s attention. Starting 3 logMAR levels above that failed in phase 1, a single optotype is presented at 3 consecutive descending logMAR steps. Note that performance during reinforcement has no effect the final acuity score. Finally, during phase 2 the child is presented with up to 4 optotypes per level beginning at that missed in phase 1, in consecutive descending logMAR steps. Visual acuity is recorded as the last level at which the child correctly identified three letters in this phase. Importantly, the ATS protocol measures visual acuity on a line-byline basis as each child’s visual acuity score is equal to the logMAR value of the smallest optotype level at which the he/she correctly identified at least 3 optotypes. Thus, visual acuity is scored in 0.1 logMAR increments (eg, 0, 0.1, 0.2, 0.3 logMAR, etc.).
Results
Mean visual acuity and 95% tolerance interval are categorized by age group and presented in Table 1. Note that these data were corrected for within-subjects correlation for participants who completed testing with each eye. Mean interocular acuity difference and 95% tolerance interval were also calculated and categorized by age group and are provided in Table 1. An ANOVA under the intraclass correlation model7 indicated that visual acuity showed significant improvement from 3 years of age to adulthood (F6,400 = 26.3, p < 2.0 × 10−26). Overall, acuity improved by slightly more than one line (0.12 logMAR) over this age range. According to planned comparisons, the improvement in visual acuity was significant between the ages of 4 and 5 years, 5 and 6 years, and 7 and 8–10 years (p < 0.05 for all of these pairwise comparisons).
To test for a potential order effect, a pairwise t-test was conducted comparing visual acuity values obtained from the eye that was tested first (right eye) in each participant and from the eye that was tested last (the left eye). The analysis indicated that the overall fatigue effect of 0.002 logMAR was not significant (p = 0.8) even in the youngest age group assessed (0.019 logMAR; p = 0.09).
Although a one-way ANOVA indicated that interocular acuity differences were significantly different across age groups (F = 2.76, p = 0.012), there were no clear developmental trends. Mean interocular difference was less than one line at all ages. The 95% tolerance interval was near ±0.10 logMAR at each age and overall, on average, was ±0.11 logMAR.
Discussion
The present study is the first to provide normative pediatric data collected using isolated surrounded HOTV optotypes, presented on the EVA testing system, and using the ATS visual acuity testing protocol. It is difficult to compare these data to those of other studies as few researchers have gathered normative data for preschool- and school-aged children. Furthermore, the normative studies that do exist differ greatly in terms of optotypes, optotype size progression, crowding format, and testing protocol, parameters known to affect visual acuity.8,9 Thus in Figure 1, we compare the normative data from the present study to the most similar studies available in the literature. Specifically, the figure includes only those studies in which visual acuity was measured monocularly using letter optotypes (ie, Tumbling E, Landolt C, Glasgow Acuity Cards, or STYCAR/HOTV) arranged in a crowding format (ie, linear charts, crowding bars, surrounding contours, surrounding pseudo-optotypes).9–17 Although there is some variability in visual acuity, the data of the present study appear to be in agreement with those from other studies. Note however, that the visual acuity scores of participants from the 3 studies that report the best acuities used lenient optotype detection criteria,15 testing protocols that allowed numerous optotype identification mistakes16 or potential learning effects.17
Figure 1.
Normal visual acuity from participants in the present study and those in other studies plotted as a function of age. Note that visual acuity scores from 8–10 year-olds in the present study are combined and plotted at 9 years of age. (-●- Shea & Gaccon, 2006, Glasgow Acuity Cards; -○- Simmers et al., 1997, Glasgow Acuity Cards; -▼-Simmers et al., 1997, Sheridan-Gardiner; -■- Sheridan, 1960, HOTV; -▽- Slataper, 1950, Tumbling E; -□-Simons, 1983, Landolt C; -◇-Wiess, 1973, Tumbling E; -◆-Weiss, 1973, Tumbling E; -
 -Morad et al., 1999, Tumbling E; -
-Morad et al., 1999, Tumbling E; -
 -Morad et al., 1999, Linear Tumbling E; -
-Morad et al., 1999, Linear Tumbling E; -
 - Brant & Novotny, 1976, Snellen; -
- Brant & Novotny, 1976, Snellen; -
 - Brant & Novotny, 1976; Tumbling E; -
- Brant & Novotny, 1976; Tumbling E; -
 - Current Study, HOTV).
- Current Study, HOTV).
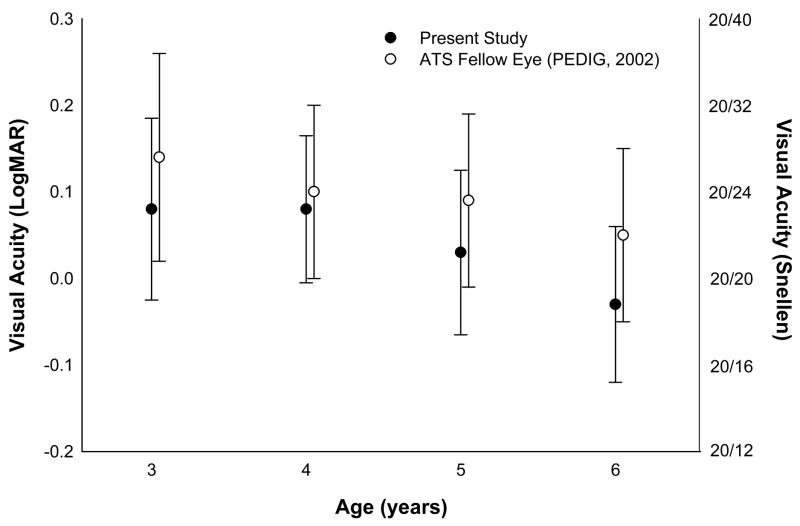
It is also of particular interest to compare the visual acuity data reported here to those of the fellow eye of children with amblyopia who were assessed recently using the ATS protocol.18 Due to the lack of true ATS normative data, researchers have relied upon these fellow eye data to define normal visual acuity in children.19 Yet this practice raises the contentious issue of whether the fellow eye of children with amblyopia should be considered normal as it may possess spatial vision deficits.20–21 In Figure 2, the mean visual acuity of participants in the present study is compared to that of the fellow eyes of 409 3- to 6-year-old children with amblyopia (data are drawn from the ATS study).18 This comparison indicates that visual acuity of the fellow eye is indeed poorer than that of children from the present study (pairwise comparisons by t-test: 3-year-olds: t = 3.09, p = 0.02; 4-year-olds: t = 1.87, p = 0.06; 5-year-olds: t = 4.54, p < 0.001; 6-year-olds: t = 5.49, p < 0.0001). Note however, that for each age group, the difference is less than one line (range, 0.03–0.08 logMAR) and visual acuities of most fellow eyes are well within the 95% tolerance intervals reported here.
Figure 2.
Mean visual acuity from participants in the present study and from the fellow eye of children with amblyopia (fellow eye data are drawn from the Pediatric Eye Disease Investigator Group18). Bars represent one standard deviation from the mean.
It is unclear why the visual acuity of participants in the present study is superior to that of the fellow eye of ATS patients. Although it is possible that visual acuity of the fellow eye of ATS patients is diminished due to occlusion therapy, other researchers report similar spatial deficits in newly identified amblyopic patients who have not undergone occlusion therapy.21 As an alternative explanation, some researchers suggest that amblyopia has a central origin and that the lack of sufficient input is disruptive to the normal visual development of both eyes.20–22 Conversely, it can be argued the reduced visual acuity in the fellow eye is the result of an adaptive process to prevent excessive interocular difference and thus maintain or allow the potential for binocular vision.20 Another possible explanation is that latent nystagmus, which is common in infantile esotropia, may degrade visual acuity in the fellow eye.23
The 95% tolerance intervals for interocular acuity difference from the present study are compared to those of other studies in Table 2. Once again, only studies in which visual acuity was measured using crowded letter optotypes are included.12,13,24 Note that this comparison is limited to 3-, 4-, and 5-year-old children due to a lack of published data for other age groups. As can be seen in Table 2, the intervals of the present study are slightly broader at 4 and 5 years of age than those of other studies. It is possible that this discrepancy is due to a difference in scoring procedures. Specifically, unlike ATS protocol which follows a line-by-line scoring system, the other studies in the Table implement a letter-by-letter protocol in which the child is awarded a score of 0.025 logMAR units per correctly identified letter. Testing stops when the child cannot identify a single optotype at a given optotype level, and the final score is equal to 1.0 minus the overall logMAR value of the optotypes correctly identified. Therefore following this procedure, it is possible for participants to obtain interocular differences (ie, 0.025, 0.05, 0.075 logMAR) smaller than those recorded here. Nevertheless, the intervals of 4- and 5-year-olds of the present study are only about 0.033 logMAR (1.3 letters) broader than those of the other studies in Table 2. Despite our broader intervals, it is clear that an interocular difference of two or more lines (≥0.20 logMAR) using the ATS protocol is well outside the normal limits for these age groups and the older age groups (Table 1), and thus should be considered indicative of an abnormal interocular difference.
Table 2.
Ninety-five percent tolerance intervals for interocular acuity difference from partipants in the present study and those in other studies. Note that all values are in logMAR units.
| Study
|
||||
|---|---|---|---|---|
| Age group (years) | Shea & Gaccon(2006) | McGraw et al (2000) | Simmers et al (1997) | Present study |
| 3 | ±0.12 | ±0.10 | ||
| 4 | ±0.11 | ±0.05 | ±0.12 | |
| 5 | ±0.08 | ±0.10 | ||
The EVA system represents an attempt to standardize visual acuity testing in young children for the detection and clinical management of pediatric eye disease. The system possesses a number of advantages over traditional pediatric optotype tests that make it suitable for clinical, pediatric vision testing across multiple sites.3–5 Furthermore, the ATS visual acuity testing protocol possesses both high testability and test-retest reliability.4,5 The present study provides normative data that will be used in clinical practice, screening, and clinical research.
Literature Search
A literature search for normative pediatric visual acuity was conducted at www.pubmed.gov. The search included the search terms visual acuity, amblyopia treatment study, and HOTV. There were no language or date restrictions.
Acknowledgments
This research was supported by a grant from the National Eye Institute (EY05236)
Footnotes
The study was conducted at The Retina Foundation of the Southwest
The authors have no commercial interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chen SI, Chandna A, Norica AM, Pettet M, Stone D. The repeatability of best corrected acuity in normal and amblyopic children 4 to 12 years of age. Invest Ophthalmol Vis Sci. 2006;47:614–9. doi: 10.1167/iovs.05-0610. [DOI] [PubMed] [Google Scholar]
- 2.Ferris FL, III, Bailey I. Standardizing the measurement of visual acuity for clinical research studies. Guidelines from the Eye Care Technology Forum. Ophthalmology. 1996;103:181–2. doi: 10.1016/s0161-6420(96)30742-2. [DOI] [PubMed] [Google Scholar]
- 3.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: Adaptation of the amblyopia treatment study visual acuity testing protocol. Am J Ophthalmol. 2001;132:903–9. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 4.Kulp MT, Dobson V, Peskin E, et al. The electronic visual acuity tester: Testability in preschool children. Optom Vis Sci. 2004;81:238–44. doi: 10.1097/00006324-200404000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Holmes JM, Beck RW, Repka MX, et al. The Amblyopia Treatment Study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–53. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 6.Simons K. Preschool vision screening: Rationale, methodology and outcome. Surv Ophthalmol. 1996;41:3–30. doi: 10.1016/s0039-6257(97)81990-x. [DOI] [PubMed] [Google Scholar]
- 7.Rosner B. Statistical methods in ophthalmology: An adjustment for the intraclass correlation between eyes. Biometrics. 1982;38:105–14. [PubMed] [Google Scholar]
- 8.Bailey I, Lovie J. New design principles for visual acuity letter charts. Am J Optom Physiol Opt. 1976;53:740–5. doi: 10.1097/00006324-197611000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Simons K. Visual acuity norms in young children. Surv Ophthalmol. 1983;8:84–92. doi: 10.1016/0039-6257(83)90076-0. [DOI] [PubMed] [Google Scholar]
- 10.Slataper FJ. Age norms of refraction and vision. Arch Ophthalmol. 1950;43:466–81. [Google Scholar]
- 11.Brant JC, Nowotny M. Testing of visual acuity in young children: An evaluation of some commonly used methods. Develop Med Child Neurol. 1976;18:568–76. doi: 10.1111/j.1469-8749.1976.tb04203.x. [DOI] [PubMed] [Google Scholar]
- 12.Shea SJ, Gaccon L. In the absence of strabismus what constitutes a visual deficit in children? Brit J Ophthalmol. 2006;90:40–3. doi: 10.1136/bjo.2005.072009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simmers AJ, Gray LS, Spowart K. Screening for amblyopia: A comparison of paediatric letter tests. Brit J Ophthalmol. 1997;81:465–9. doi: 10.1136/bjo.81.6.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheridan MD. Vision screening of very young or handicapped children. Br Med J. 1960:453–6. doi: 10.1136/bmj.2.5196.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weiss JB. Mesure de l’acuite visuelle du jeune enfant. Vision Res. 1973;13:1139–49. doi: 10.1016/0042-6989(73)90149-1. [DOI] [PubMed] [Google Scholar]
- 16.Schmid M, Largo RH. Visual acuity and stereopsis between the ages of 5 and 10 years. Eur J Pediatr. 1986;145:475–9. doi: 10.1007/BF02429046. [DOI] [PubMed] [Google Scholar]
- 17.Morad Y, Werker E, Nemet P. Visual acuity tests using chart, line, and single optotype in healthy and amblyopic children. J AAPOS. 1999;3:94–7. doi: 10.1016/s1091-8531(99)70077-7. [DOI] [PubMed] [Google Scholar]
- 18.The Pediatric Eye Disease Investigator Group. The clinical profile of moderate amblyopia in children younger than 7 years. Arch Ophthalmol. 2002;120:281–7. [PubMed] [Google Scholar]
- 19.Fu VL, Birch EE, Holmes JM. Assessment of a new distance Randot® stereoacuity test. J AAPOS. 2006;10:419–23. doi: 10.1016/j.jaapos.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 20.Chatzistefanou KI, Theodossiadis GP, Damankis AG, et al. Contrast sensitivity in amblyopia: The fellow eye of untreated and successfully treated amblyopes. J AAPOS. 2005;9:468–74. doi: 10.1016/j.jaapos.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 21.Leguire LE, Rogers GL, Bremer DL. Amblyopia: The normal eye is not normal. J Pediatr Ophthalmol Strabismus. 1990;27:32–8. doi: 10.3928/0191-3913-19900101-10. [DOI] [PubMed] [Google Scholar]
- 22.Lewis TL, Maurer D, Tytla ME, et al. Vision in the “good” eye of children treated for unilateral congenital cataract. Ophthalmol. 1992;99:1013–7. doi: 10.1016/s0161-6420(92)31857-3. [DOI] [PubMed] [Google Scholar]
- 23.Simon JW. Pediatric ophthalmology and strabismus. San Francisco: American Academy of Ophthalmology; 2005. Basic and clinical science course. Section 6. 2005–2006; p. 482. [Google Scholar]
- 24.McGraw PV, Winn B, Gray LS, Elliot DB. Improving the reliability of visual acuity measures in young children. Ophthal Physiol Opt. 2000;20:173–84. [PubMed] [Google Scholar]