Abstract
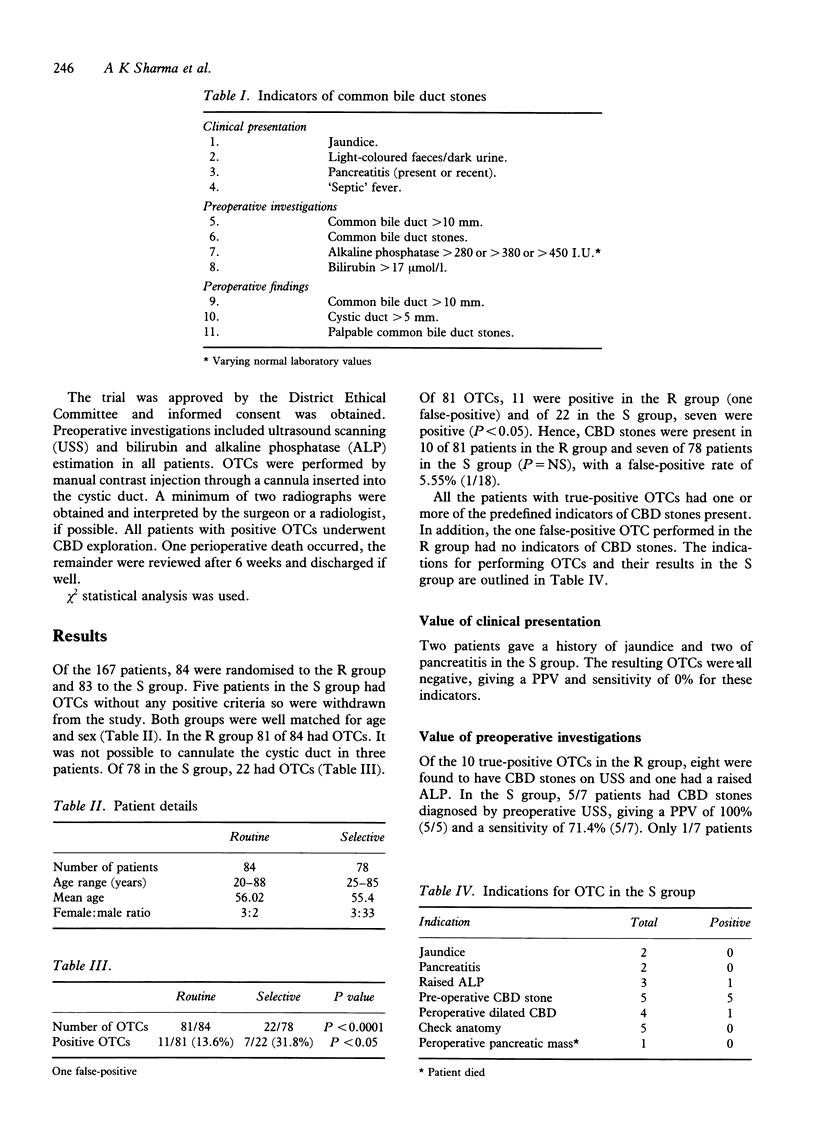
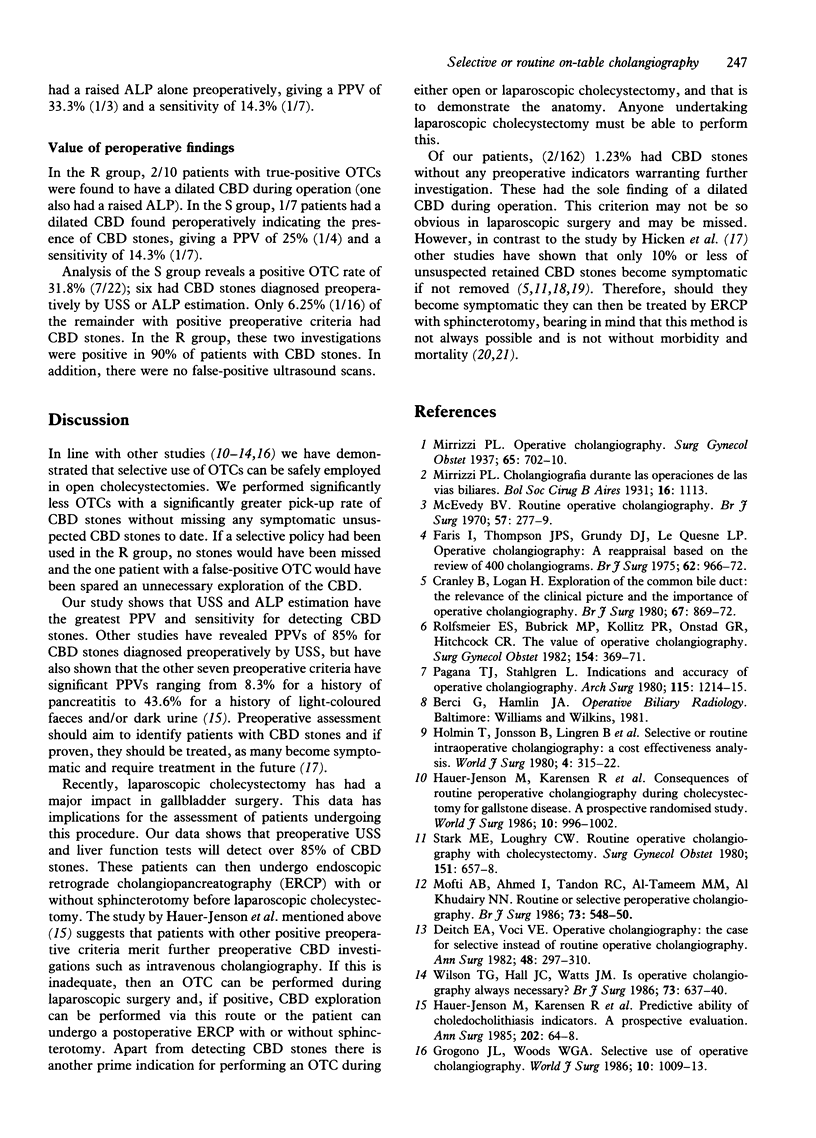
To assess the value of pre- and peroperative indicators of common bile duct (CBD) stones, 167 patients undergoing cholecystectomy were randomised to receive either routine (R) or selective (S) on-table cholangiography (OTC). In all, 81/84 patients in the R group and 22/78 in the S group had OTCs (P < 0.0001). In the R group 11/81 were positive (one false-positive) and in the S group 7/22 were positive (P < 0.05). CBD stones were present in 10/81 in the R group and 7/78 in the S group (P = NS). In the R group 8/10 and in the S group 5/7 had CBD stones diagnosed preoperatively by ultrasound scanning (USS), giving USS a positive predictive value (PPV) of 100% and a sensitivity of 71.4% in the S group. A raised preoperative alkaline phosphatase (ALP) was found in 1/10 in the R group and 1/7 in the S group (PPV = 33.3%, sensitivity = 14.3%). In the R group 1/10 and in the S group 1/7 (PPV = 25%, sensitivity = 14.3%) were found to have a dilated CBD during operation suggesting CBD stones. There have been no cases of symptomatic unsuspected retained CBD stones during follow-up to date. Our study has demonstrated that selective use of OTCs can be safely employed in open cholecystectomies. Over 85% (6/7 in the S group and 15/17 overall) of CBD stones can be diagnosed preoperatively by USS and liver function tests, with USS having the greatest PPV and sensitivity.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cranley B., Logan H. Exploration of the common bile duct--the relevance of the clinical picture and the importance of peroperative cholangiography. Br J Surg. 1980 Dec;67(12):869–872. doi: 10.1002/bjs.1800671210. [DOI] [PubMed] [Google Scholar]
- Deitch E. A., Voci V. E. Operative cholangiography. The case for selective instead of routine operative cholangiography. Am Surg. 1982 Jul;48(7):297–301. [PubMed] [Google Scholar]
- Faris I., Thomson J. P., Grundy D. J., Le Quesne L. P. Operative cholangiography: a reappraisal based on a review of 400 cholangiograms. Br J Surg. 1975 Dec;62(12):966–972. doi: 10.1002/bjs.1800621211. [DOI] [PubMed] [Google Scholar]
- Grogono J. L., Woods W. G. Selective use of operative cholangiography. World J Surg. 1986 Dec;10(6):1009–1013. doi: 10.1007/BF01658660. [DOI] [PubMed] [Google Scholar]
- HICKEN N. F., MCALLISTER A. J. OPERATIVE CHOLANGIOGRAPHY AS AN AID IN REDUCING THE INCIDENCE OF "OVERLOOKED" COMMON BILE DUCT STONES: A STUDY OF 1,293 CHOLEDOCHOLITHOTOMIES. Surgery. 1964 Jun;55:753–758. [PubMed] [Google Scholar]
- Hauer-Jensen M., Kåresen R., Nygaard K., Solheim K., Amlie E., Havig O., Viddal K. O. Consequences of routine peroperative cholangiography during cholecystectomy for gallstone disease: a prospective, randomized study. World J Surg. 1986 Dec;10(6):996–1002. doi: 10.1007/BF01658656. [DOI] [PubMed] [Google Scholar]
- Hauer-Jensen M., Kåresen R., Nygaard K., Solheim K., Amlie E., Havig O., Viddal K. O. Predictive ability of choledocholithiasis indicators. A prospective evaluation. Ann Surg. 1985 Jul;202(1):64–68. doi: 10.1097/00000658-198507000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmin T., Jönsson B., Lingren B., Olson S. A., Petersson B. G., Sörbris R., Bengmark S. Selective or routine intraoperative cholangiography: a cost-effectiveness analysis. World J Surg. 1980 May;4(3):315–322. doi: 10.1007/BF02393390. [DOI] [PubMed] [Google Scholar]
- Jolly P. C., Baker J. W., Schmidt H. M., Walker J. H., Holm J. C. Operative cholangiography: a case for its routine use. Ann Surg. 1968 Sep;168(3):551–565. doi: 10.1097/00000658-196809000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leese T., Neoptolemos J. P., Carr-Locke D. L. Successes, failures, early complications and their management following endoscopic sphincterotomy: results in 394 consecutive patients from a single centre. Br J Surg. 1985 Mar;72(3):215–219. doi: 10.1002/bjs.1800720325. [DOI] [PubMed] [Google Scholar]
- McEvedy B. V. Routine operative cholangiography. Br J Surg. 1970 Apr;57(4):277–279. doi: 10.1002/bjs.1800570410. [DOI] [PubMed] [Google Scholar]
- Mofti A. B., Ahmed I., Tandon R. C., Al-Tameem M. M., Al-Khudairy N. N. Routine or selective peroperative cholangiography. Br J Surg. 1986 Jul;73(7):548–550. doi: 10.1002/bjs.1800730710. [DOI] [PubMed] [Google Scholar]
- Pagana T. J., Stahlgren L. H. Indications and accuracy of operative cholangiography. Arch Surg. 1980 Oct;115(10):1214–1215. doi: 10.1001/archsurg.1980.01380100060014. [DOI] [PubMed] [Google Scholar]
- Rolfsmeyer E. S., Bubrick M. P., Kollitz P. R., Onstad G. R., Hitchcock C. R. The value of operative cholangiography. Surg Gynecol Obstet. 1982 Mar;154(3):369–371. [PubMed] [Google Scholar]
- Stark M. E., Loughry C. W. Routine operative cholangiography with cholecystectomy. Surg Gynecol Obstet. 1980 Nov;151(5):657–658. [PubMed] [Google Scholar]
- Thurston O. G. Proceedings: Nonroutine operative cholangiography. Arch Surg. 1974 Apr;108(4):512–515. doi: 10.1001/archsurg.1974.01350280116019. [DOI] [PubMed] [Google Scholar]
- Vaira D., D'Anna L., Ainley C., Dowsett J., Williams S., Baillie J., Cairns S., Croker J., Salmon P., Cotton P. Endoscopic sphincterotomy in 1000 consecutive patients. Lancet. 1989 Aug 19;2(8660):431–434. doi: 10.1016/s0140-6736(89)90602-8. [DOI] [PubMed] [Google Scholar]
- Wilson T. G., Hall J. C., Watts J. M. Is operative cholangiography always necessary? Br J Surg. 1986 Aug;73(8):637–640. doi: 10.1002/bjs.1800730820. [DOI] [PubMed] [Google Scholar]



