Abstract
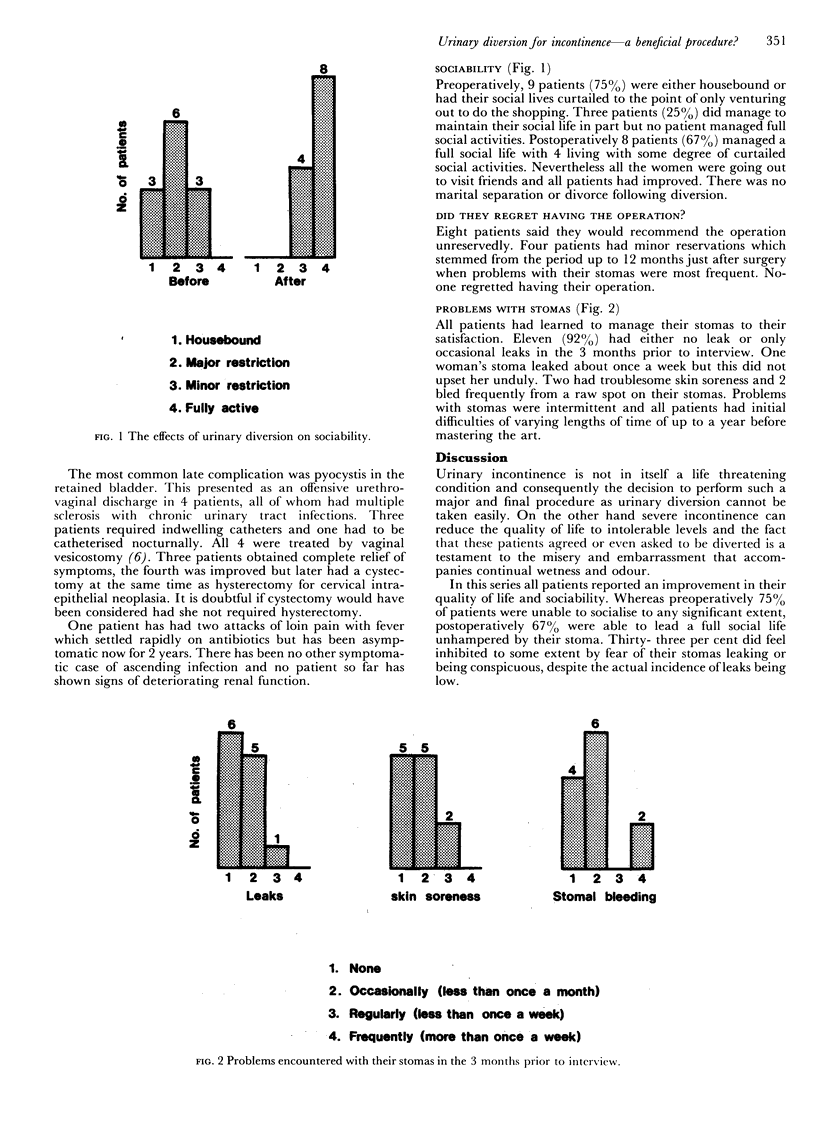
In the past 8 years at St George's Hospital, 13 women underwent urinary diversion for disabling incontinence. Seven patients had multiple sclerosis, 2 had suffered trauma to the lumbar spine and 4 had failed repeated surgery for urethral sphincter incompetence. One patient died several months postoperatively due to relapse of her multiple sclerosis. The remaining 12 were interviewed to determine the effect of the operation on their quality of life. Preoperatively, 9 patients (75%) were either housebound or only ventured out to do the shopping and none led a full social life. Postoperatively 8 patients (67%) managed a full social life and all were improved. Most managed their stomas proficiently and none regretted having the operation. The most common late complication was pyocystis. We conclude that patients with disabling incontinence can have their quality of life substantially improved by urinary diversion. The incidence of pyocystis is probably high enough to warrant vaginal vesicostomy to be performed routinely at the time of diversion, at least in those women with chronic urinary infection.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baskett P. J., Armstrong R. Anaesthetic problems in multiple sclerosis. Are certain agents contraindicated? Anaesthesia. 1970 Jul;25(3):397–401. doi: 10.1111/j.1365-2044.1970.tb00229.x. [DOI] [PubMed] [Google Scholar]
- Desmond A. D., Shuttleworth K. E. The results of urinary diversion in multiple sclerosis. Br J Urol. 1977 Nov;49(6):495–502. doi: 10.1111/j.1464-410x.1977.tb04190.x. [DOI] [PubMed] [Google Scholar]
- Guerrier K., Albert D. J., Persky L. Experiences with pyocystis. Arch Surg. 1971 Jul;103(1):63–65. doi: 10.1001/archsurg.1971.01350070089020. [DOI] [PubMed] [Google Scholar]
- Hargreave T. B., Galloway N. T. Incontinence. Br Med J (Clin Res Ed) 1983 Oct 8;287(6398):1002–1003. doi: 10.1136/bmj.287.6398.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones M. A., Breckman B., Hendry W. F. Life with an ileal conduit: results of questionnaire surveys of patients and urological surgeons. Br J Urol. 1980 Feb;52(1):21–25. doi: 10.1111/j.1464-410x.1980.tb02913.x. [DOI] [PubMed] [Google Scholar]
- Philp N. H., Williams J. L., Byers C. E. Ileal conduit urinary diversion: long-term follow-up in adults. Br J Urol. 1980 Dec;52(6):515–519. doi: 10.1111/j.1464-410x.1980.tb03103.x. [DOI] [PubMed] [Google Scholar]
- Siemkowicz E. Multiple sclerosis and surgery. Anaesthesia. 1976 Nov;31(9):1211–1216. doi: 10.1111/j.1365-2044.1976.tb11973.x. [DOI] [PubMed] [Google Scholar]
- Spence H. M., Allen T. D. Vaginal vesicostomy for empyema of the defunctionalized bladder. J Urol. 1971 Dec;106(6):862–864. doi: 10.1016/s0022-5347(17)61420-4. [DOI] [PubMed] [Google Scholar]
- Stevens P. S., Eckstein H. B. The management of pyocystis following ileal conduit urinary diversion in children. Br J Urol. 1975 Dec;47(6):631–633. doi: 10.1111/j.1464-410x.1975.tb04027.x. [DOI] [PubMed] [Google Scholar]
- Williams N. S., Johnston D. The quality of life after rectal excision for low rectal cancer. Br J Surg. 1983 Aug;70(8):460–462. doi: 10.1002/bjs.1800700805. [DOI] [PubMed] [Google Scholar]
- Wyatt J. K. Ileal conduit diversion for benign disease: a critical review and long-term follow-up. Can J Surg. 1974 Sep;17(5):270–273. [PubMed] [Google Scholar]



