Abstract
The metabolic and endocrine response to surgery has been investigated in detail for many years. The current view is that the response is detrimental to the patient and that the prevention or reduction of the changes may be beneficial in aiding recovery from surgery. Three main methods are available at present for modifying the response. First, the use of afferent neuronal blockage, by epidural or spinal analgesia, to inhibit the transmission of impulses from the site of trauma. Secondly, the intravenous administration of large doses of potent opiate analgesics to block hypothalamic-pituitary function. Thirdly, the hormonal status of the patient may be changed, either by the use of agents to inhibit the secretion or action of the catabolic hormones, or by the infusion of anabolic hormones such as insulin.
Full text
PDF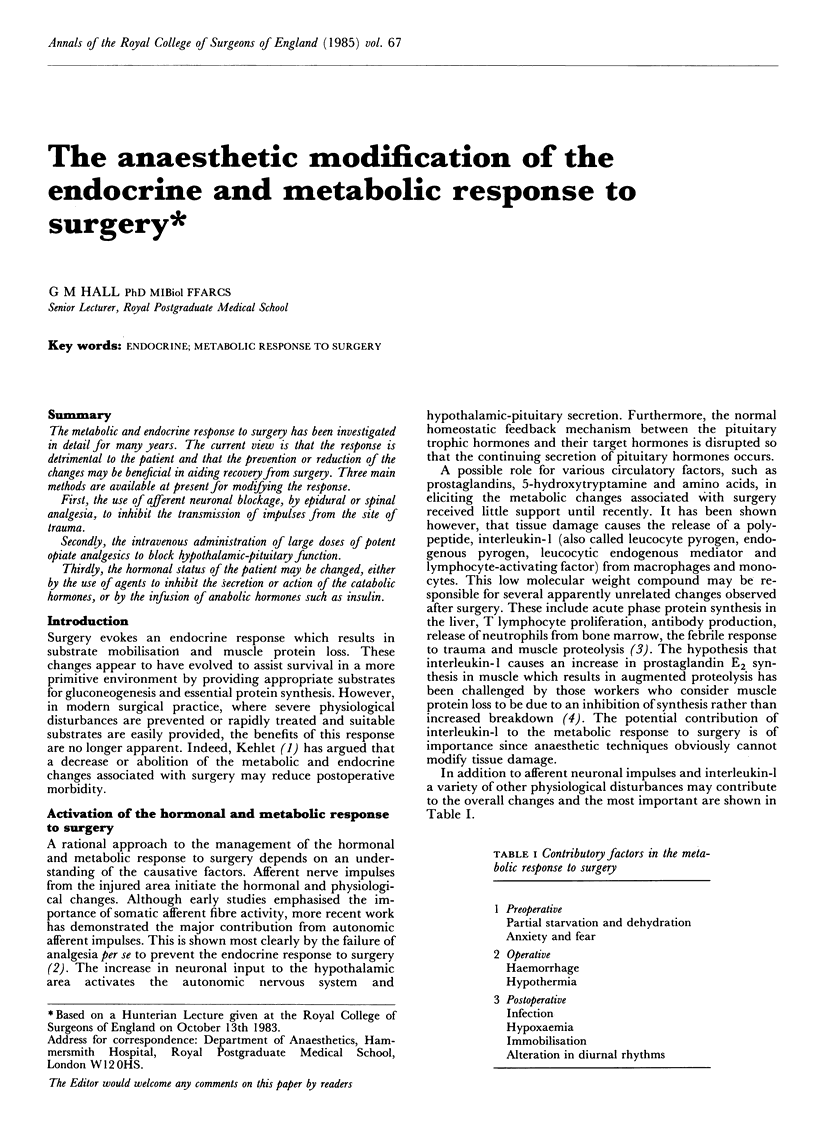

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beisel W. R. Mediators of fever and muscle proteolysis. N Engl J Med. 1983 Mar 10;308(10):586–587. doi: 10.1056/NEJM198303103081009. [DOI] [PubMed] [Google Scholar]
- Bent J. M., Paterson J. L., Mashiter K., Hall G. M. Effects of high-dose fentanyl anaesthesia on the established metabolic and endocrine response to surgery. Anaesthesia. 1984 Jan;39(1):19–23. doi: 10.1111/j.1365-2044.1984.tb09447.x. [DOI] [PubMed] [Google Scholar]
- Bromage P. R., Shibata H. R., Willoughby H. W. Influence of prolonged epidural blockade on blood sugar and cortisol responses to operations upon the upper part of the abdomen and the thorax. Surg Gynecol Obstet. 1971 Jun;132(6):1051–1056. [PubMed] [Google Scholar]
- Carli F., Clark M. M., Woollen J. W. Investigation of the relationship between heat loss and nitrogen excretion in elderly patients undergoing major abdominal surgery under general anaesthetic. Br J Anaesth. 1982 Oct;54(10):1023–1029. doi: 10.1093/bja/54.10.1023. [DOI] [PubMed] [Google Scholar]
- Cooper G. M., Holdcroft A., Hall G. M., Alaghband-Zadeh J. Epidural analgesia and the metabolic response to surgery. Can Anaesth Soc J. 1979 Sep;26(5):381–385. doi: 10.1007/BF03006452. [DOI] [PubMed] [Google Scholar]
- Cooper G. M., Paterson J. L., Mashiter K., Hall G. M. Beta-adrenergic blockade and the metabolic response to surgery. Br J Anaesth. 1980 Dec;52(12):1231–1236. doi: 10.1093/bja/52.12.1231. [DOI] [PubMed] [Google Scholar]
- Cooper G. M., Paterson J. L., Ward I. D., Hall G. M. Fentanyl and the metabolic response to gastric surgery. Anaesthesia. 1981 Jul;36(7):667–671. doi: 10.1111/j.1365-2044.1981.tb08777.x. [DOI] [PubMed] [Google Scholar]
- Engquist A., Brandt M. R., Fernandes A., Kehlet H. The blocking effect of epidural analgesia on the adrenocortical and hyperglycemic responses to surgery. Acta Anaesthesiol Scand. 1977;21(4):330–335. doi: 10.1111/j.1399-6576.1977.tb01227.x. [DOI] [PubMed] [Google Scholar]
- George J. M., Reier C. E., Lanese R. R., Rower M. Morphine anesthesia blocks cortisol and growth hormone response to surgical stress in humans. J Clin Endocrinol Metab. 1974 May;38(5):736–741. doi: 10.1210/jcem-38-5-736. [DOI] [PubMed] [Google Scholar]
- Hall G. M., Adrian T. E., Bloom S. R., Mashiter K. The effects of naloxone on circulating metabolites, glycoregulatory hormones and gut peptides during pelvic surgery. Clin Physiol. 1983 Feb;3(1):49–58. doi: 10.1111/j.1475-097x.1983.tb00698.x. [DOI] [PubMed] [Google Scholar]
- Hall G. M., Walsh E. S., Paterson J. L., Mashiter K. Low-dose insulin infusion and substrate mobilization during surgery. Br J Anaesth. 1983 Oct;55(10):939–945. doi: 10.1093/bja/55.10.939. [DOI] [PubMed] [Google Scholar]
- Hall G. M., Young C., Holdcroft A., Alaghband-Zadeh J. Substrate mobilisation during surgery. A comparison between halothane and fentanyl anaesthesia. Anaesthesia. 1978 Nov-Dec;33(10):924–930. [PubMed] [Google Scholar]
- Kehlet H., Brandt M. R., Rem J. Role of neurogenic stimuli in mediating the endocrine-metabolic response to surgery. JPEN J Parenter Enteral Nutr. 1980 Mar-Apr;4(2):152–156. doi: 10.1177/014860718000400216. [DOI] [PubMed] [Google Scholar]
- McDONALD R. K., EVANS F. T., WEISE V. K., PATRICK R. W. Effect of morphine and nalorphine on plasma hydrocortisone levels in man. J Pharmacol Exp Ther. 1959 Mar;125(3):241–247. [PubMed] [Google Scholar]
- Møller W., Rem J., Brandt R., Kehlet H. Effect of posttraumatic epidural analgesia on the cortisol and hyperglycaemic response to surgery. Acta Anaesthesiol Scand. 1982 Feb;26(1):56–58. doi: 10.1111/j.1399-6576.1982.tb01726.x. [DOI] [PubMed] [Google Scholar]
- Rennie M. J., Millward D. J. 3-Methylhistidine excretion and the urinary 3-methylhistidine/creatinine ratio are poor indicators of skeletal muscle protein breakdown. Clin Sci (Lond) 1983 Sep;65(3):217–225. doi: 10.1042/cs0650217. [DOI] [PubMed] [Google Scholar]
- Traynor C., Hall G. M. Endocrine and metabolic changes during surgery: anaesthetic implications. Br J Anaesth. 1981 Feb;53(2):153–160. doi: 10.1093/bja/53.2.153. [DOI] [PubMed] [Google Scholar]
- Traynor C., Paterson J. L., Ward I. D., Morgan M., Hall G. M. Effects of extradural analgesia and vagal blockade on the metabolic and endocrine response to upper abdominal surgery. Br J Anaesth. 1982 Mar;54(3):319–323. doi: 10.1093/bja/54.3.319. [DOI] [PubMed] [Google Scholar]
- Tsuji H., Asoh T., Takeuchi Y., Shirasaka C. Attenuation of adrenocortical response to upper abdominal surgery with epidural blockade. Br J Surg. 1983 Feb;70(2):122–124. doi: 10.1002/bjs.1800700223. [DOI] [PubMed] [Google Scholar]
- Tsuji H., Shirasaka C., Asoh T., Takeuchi Y. Influences of splanchnic nerve blockade on endocrine-metabolic responses to upper abdominal surgery. Br J Surg. 1983 Jul;70(7):437–439. doi: 10.1002/bjs.1800700716. [DOI] [PubMed] [Google Scholar]
- Walsh E. S., Paterson J. L., Mashiter K., Hall G. M. Effect of phentolamine on the metabolic response to gynaecological surgery. Br J Anaesth. 1982 May;54(5):517–521. doi: 10.1093/bja/54.5.517. [DOI] [PubMed] [Google Scholar]
- Woolfson A. M., Heatley R. V., Allison S. P. Insulin to inhibit protein catabolism after injury. N Engl J Med. 1979 Jan 4;300(1):14–17. doi: 10.1056/NEJM197901043000104. [DOI] [PubMed] [Google Scholar]


