Abstract
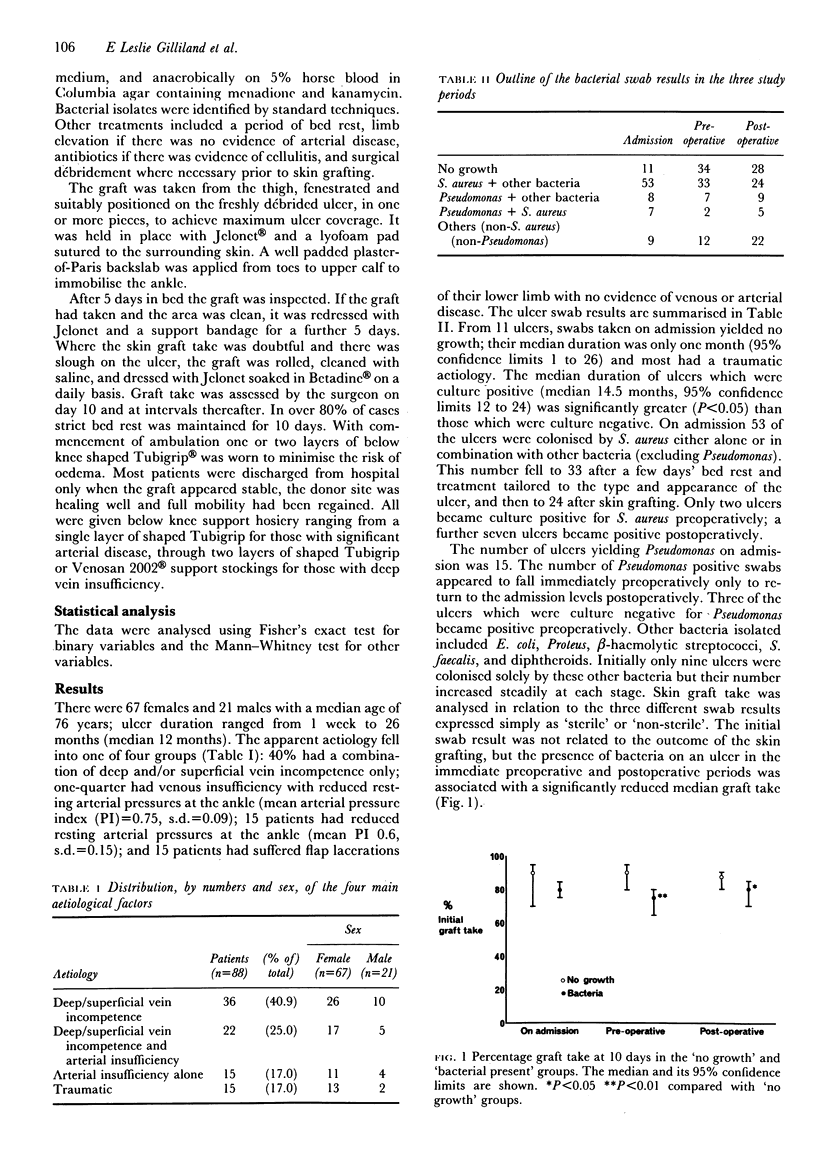
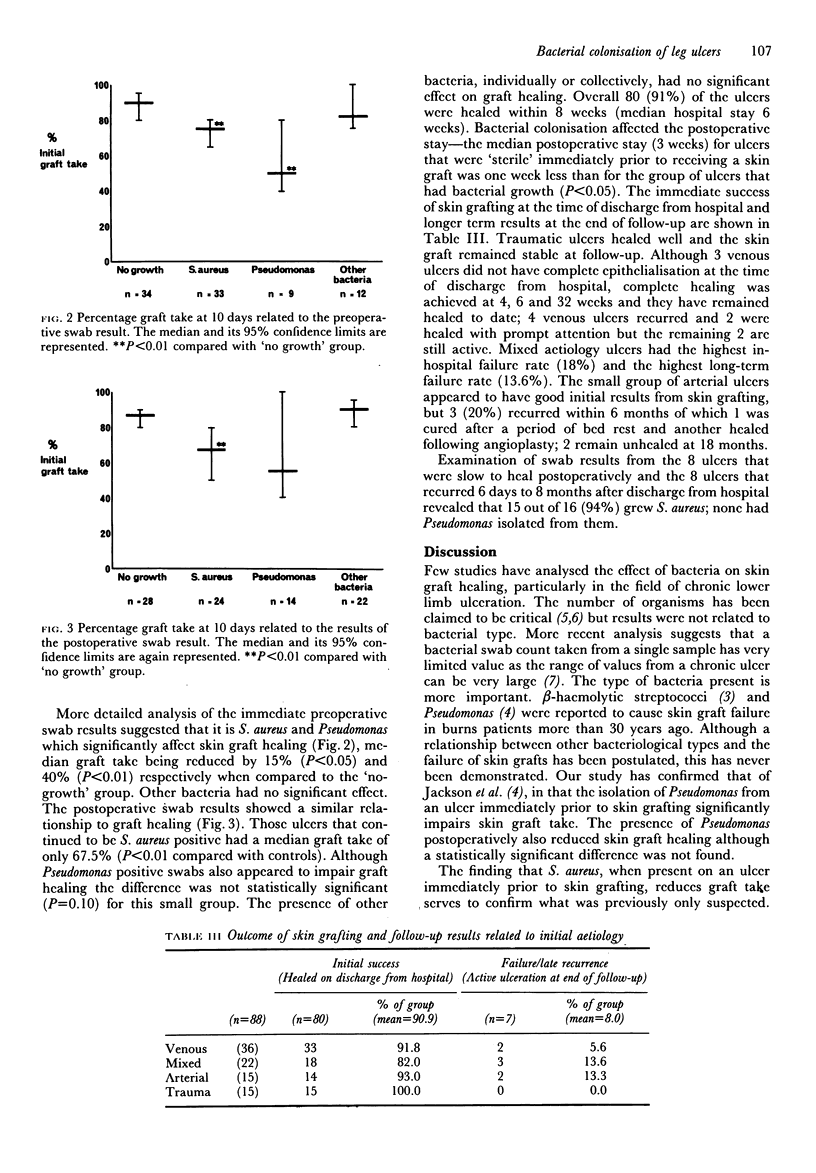
There is little information on the immediate and long-term results of skin grafting to chronic lower limb ulcers. Our experience in their management had led us to analyse, retrospectively, the results of split thickness skin grafts applied to lower limb ulcers in 88 consecutive patients. Graft take has been related to bacterial growth from ulcer swabs taken on admission, preoperatively and postoperatively. Follow-up was for a median of 18 months. Initial graft take varied from 20% to 100% (median 85%). Bacterial flora grown from the ulcer swabs varied with the duration of the ulcer and the treatment. Analysis by bacterial type has shown that Staphylococcus aurcus and Pseudomonas significantly reduced skin graft healing. Overall, 90% of these ulcers had healed with a median of 6 weeks' in-patient treatment. Examination of the swab results from the 8 ulcers that were slow to heal postoperatively and the 8 ulcers that recurred 6 days to 8 months after discharge from hospital revealed that 15 out of 16 (94%) grew S. aurcus; none had Pseudomonas isolated from them. After eighteen months 8% of these ulcers remain active. Aetiology appears important as this figure is 6% for limbs affected by venous disease only, 13.3% for limbs with arterial disease only and 13.6% for limbs with both venous and arterial disease.
Full text
PDF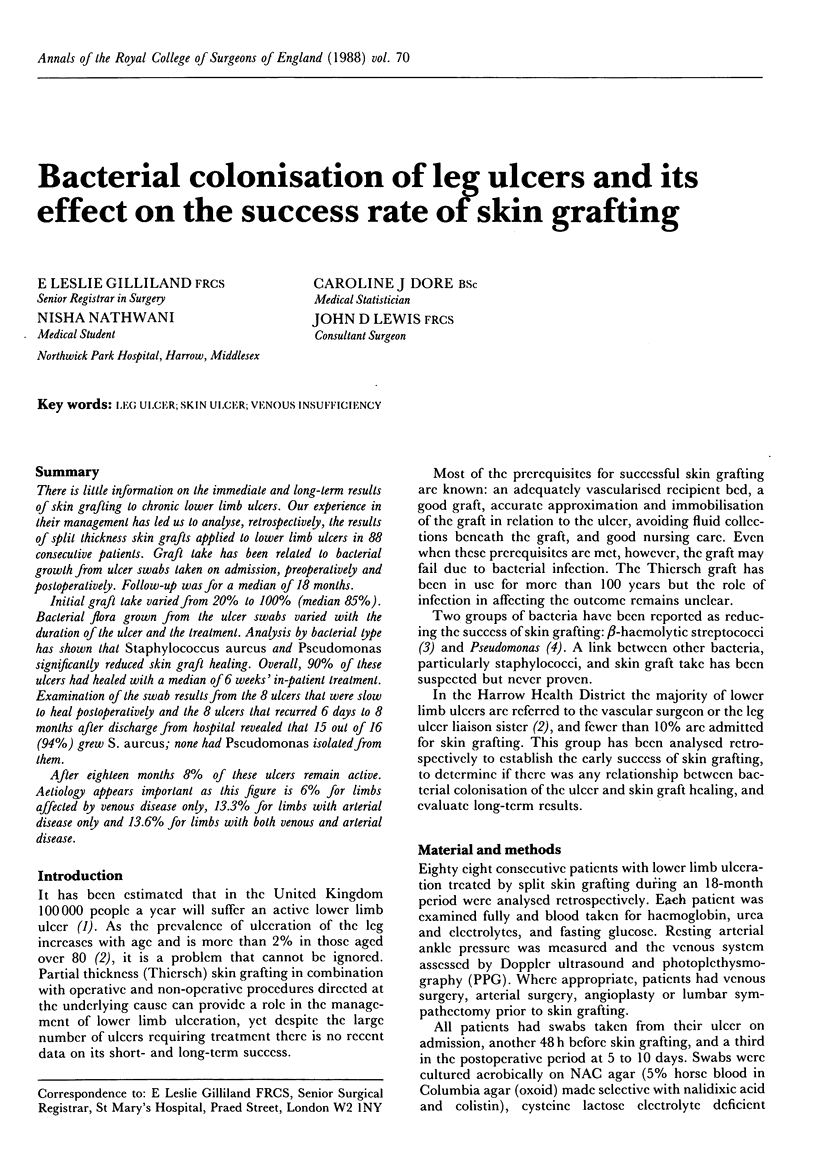

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Callam M. J., Ruckley C. V., Harper D. R., Dale J. J. Chronic ulceration of the leg: extent of the problem and provision of care. Br Med J (Clin Res Ed) 1985 Jun 22;290(6485):1855–1856. doi: 10.1136/bmj.290.6485.1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwall J. V., Doré C. J., Lewis J. D. Leg ulcers: epidemiology and aetiology. Br J Surg. 1986 Sep;73(9):693–696. doi: 10.1002/bjs.1800730905. [DOI] [PubMed] [Google Scholar]
- JACKSON D. M., LOWBURY E. J. L., TOPLEY E. Chemotherapy of Streptococcus pyogenes infection of burns. Lancet. 1951 Oct 20;2(6686):705–711. doi: 10.1016/s0140-6736(51)91478-x. [DOI] [PubMed] [Google Scholar]
- JACKSON D. M., LOWBURY E. J. L., TOPLEY E. Pseudomonas pyocyanea in burns; its role as a pathogen, and the value of local polymyxin therapy. Lancet. 1951 Jul 28;2(6674):137–147. doi: 10.1016/s0140-6736(51)91396-7. [DOI] [PubMed] [Google Scholar]
- Krizek T. J., Robson M. C. Biology of surgical infection. Surg Clin North Am. 1975 Dec;55(6):1261–1267. doi: 10.1016/s0039-6109(16)40779-6. [DOI] [PubMed] [Google Scholar]
- Schneider M., Vildozola C. W., Brooks S. Quantitative assessment of bacterial invasion of chronic ulcers. Statistical analysis. Am J Surg. 1983 Feb;145(2):260–262. doi: 10.1016/0002-9610(83)90075-2. [DOI] [PubMed] [Google Scholar]
- Teh B. T. Why do skin grafts fail? Plast Reconstr Surg. 1979 Mar;63(3):323–332. doi: 10.1097/00006534-197903000-00005. [DOI] [PubMed] [Google Scholar]


