Abstract
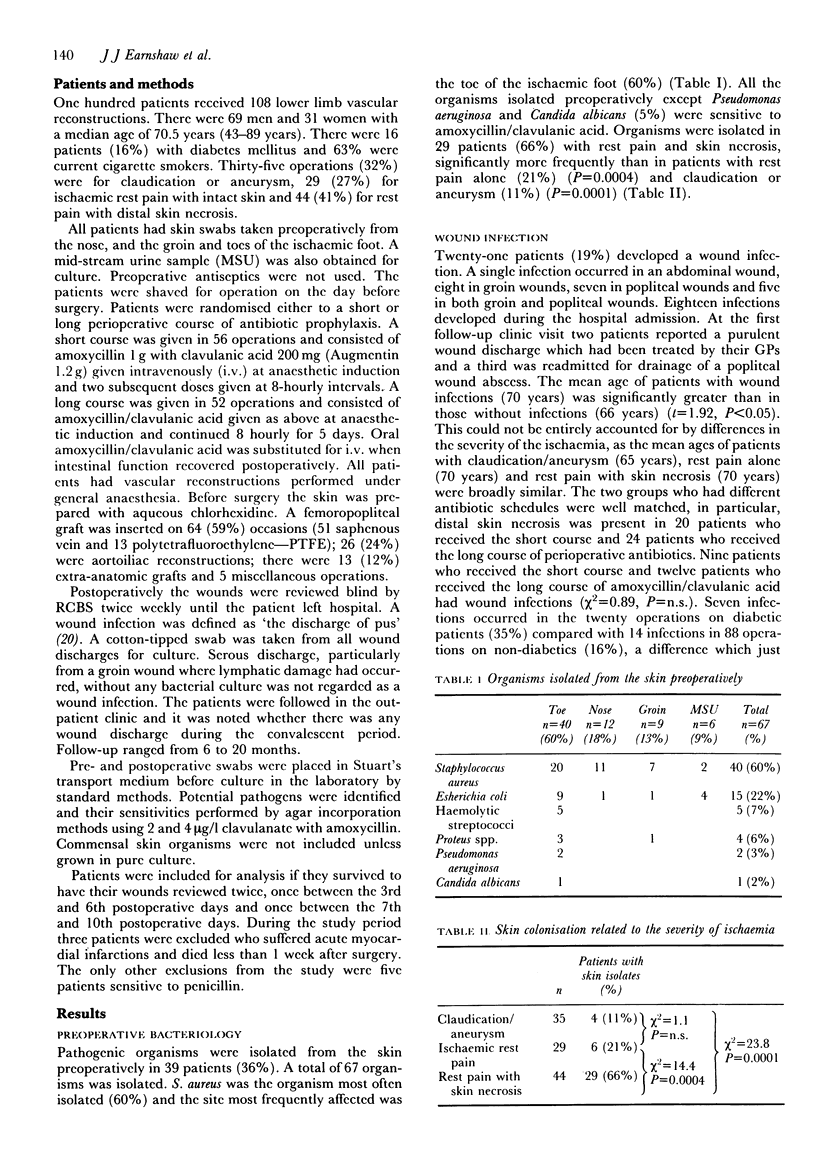
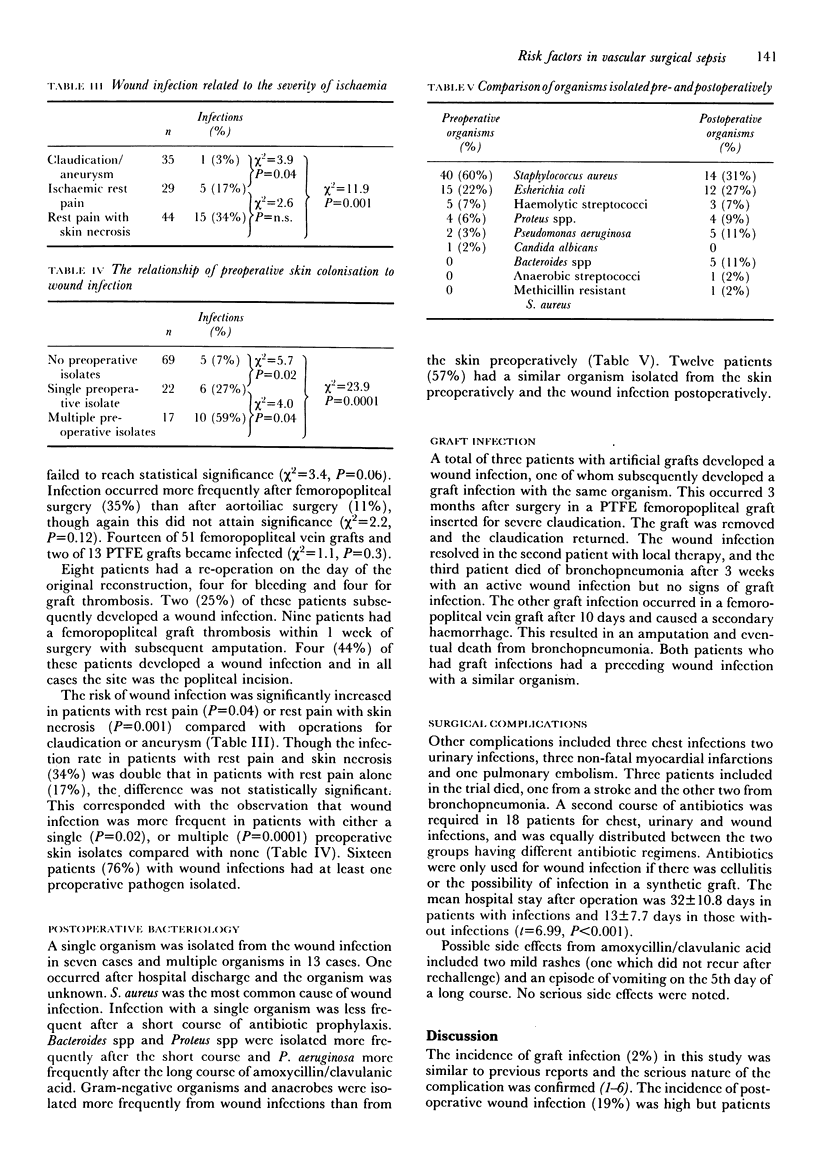
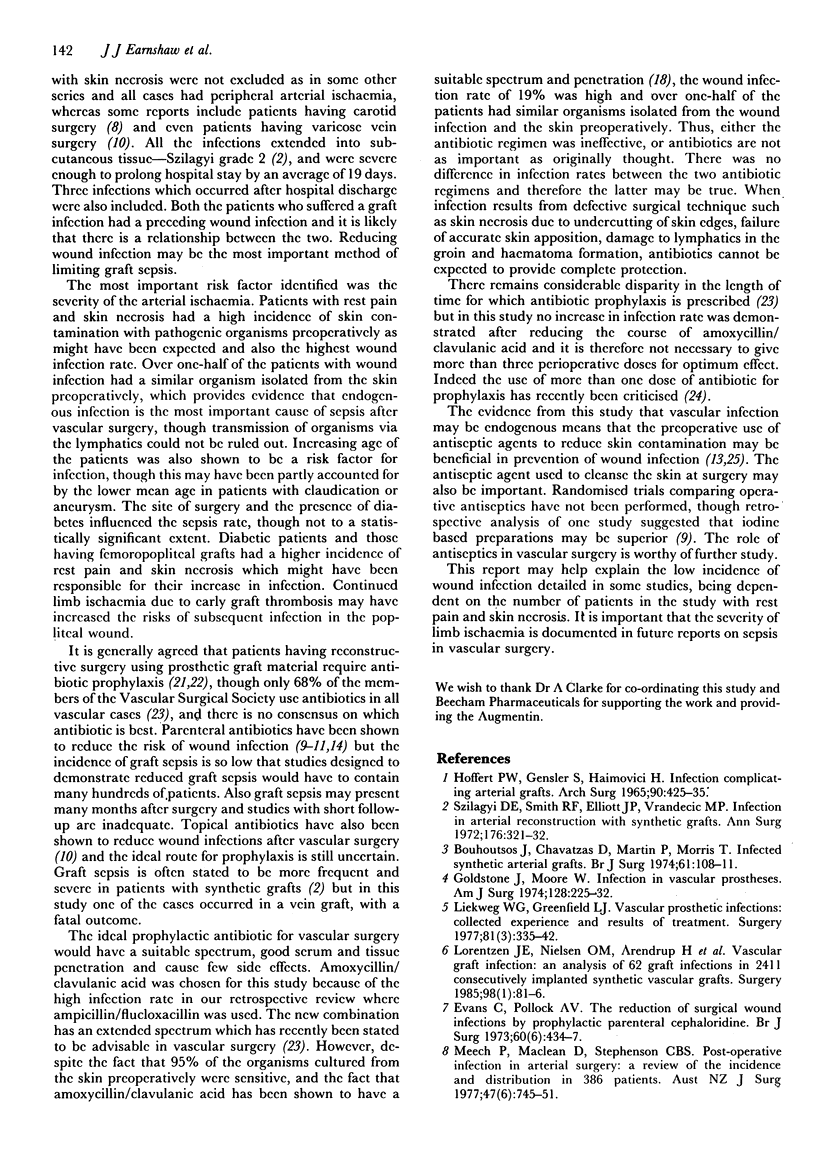
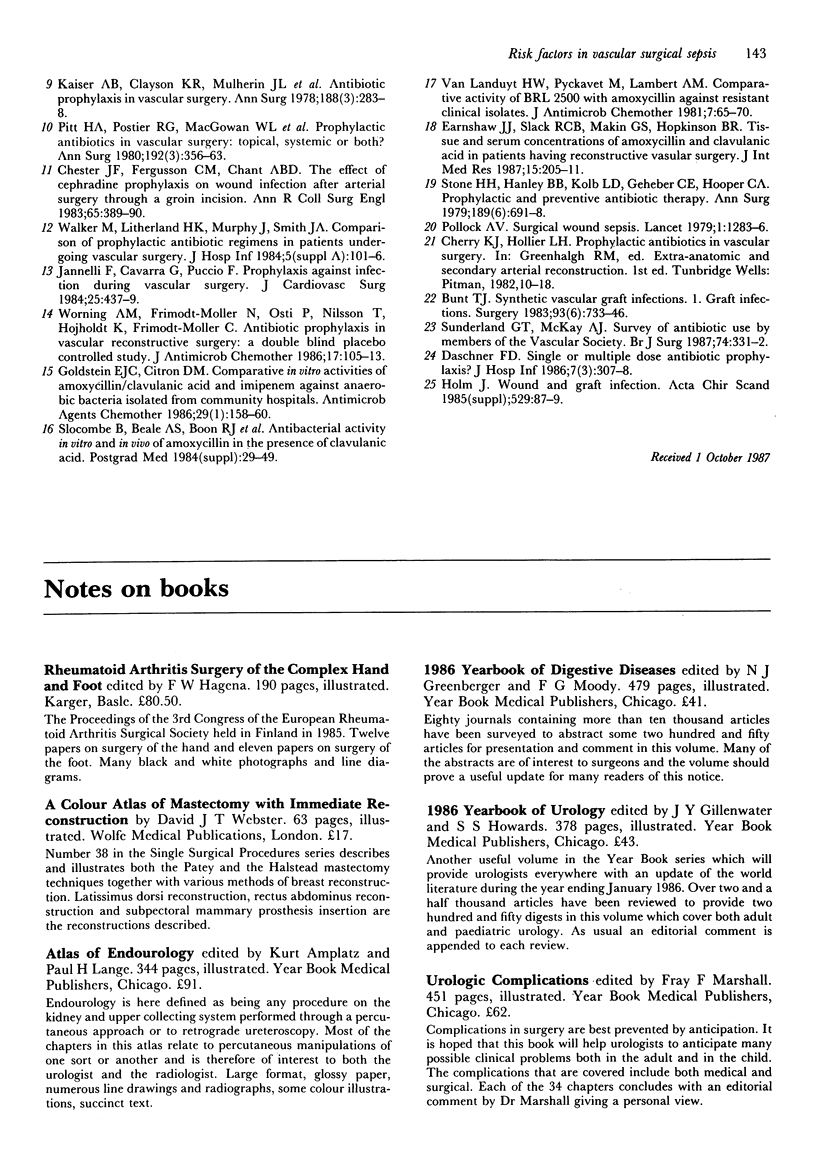
The risk factors for sepsis after vascular surgery were studied in 100 consecutive patients with lower limb arterial ischaemia. Patients were randomised either to a short or long course of antibiotic prophylaxis with amoxycillin/clavulanic acid combination (Augmentin). Pathogenic organisms were isolated from the skin preoperatively in 39 (36%) cases, significantly more frequently in patients with ischaemic rest pain and skin necrosis (66%) than rest pain alone (21%) (P = 0.0004) or claudication/aneurysm (11%) (P = 0.0001). All but three organisms isolated (5%) were sensitive to amoxycillin/clavulanic acid. A wound infection occurred after 21 (19%) reconstructions, significantly more frequently both in patients suffering rest pain with skin necrosis (P = 0.001) and rest pain without skin necrosis (P = 0.04) compared with claudication/aneurysm. Sixteen of the 21 patients with a wound infection had at least one organism isolated from their skin preoperatively (P = 0.0001). Twelve patients (57%) had a similar organism isolated from the skin preoperatively and from the postoperative wound infection. Reducing the course of antibiotic prophylaxis from 5 days to 3 doses did not significantly increase the infection rate. The only other significant risk factor for sepsis was increasing age of the patient. Although prophylaxis is undisputed in patients having synthetic grafts, antibiotics may not be as important in the prevention of wound sepsis as had been thought. The role of antiseptic agents requires further evaluation.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Benbrook D. M., Miller R. V. Effects of norfloxacin on DNA metabolism in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1986 Jan;29(1):1–6. doi: 10.1128/aac.29.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouhoutsos J., Chavatzas D., Martin P., Morris T. Infected synthetic arterial grafts. Br J Surg. 1974 Feb;61(2):108–111. doi: 10.1002/bjs.1800610208. [DOI] [PubMed] [Google Scholar]
- Bunt T. J. Synthetic vascular graft infections. I. Graft infections. Surgery. 1983 Jun;93(6):733–746. [PubMed] [Google Scholar]
- Chester J. F., Fergusson C. M., Chant A. D. The effect of cephradine prophylaxis on wound infection after arterial surgery through a groin incision. Ann R Coll Surg Engl. 1983 Nov;65(6):389–390. [PMC free article] [PubMed] [Google Scholar]
- Daschner F. D. Single- or multiple-dose antibiotic prophylaxis? J Hosp Infect. 1986 May;7(3):307–308. doi: 10.1016/0195-6701(86)90090-3. [DOI] [PubMed] [Google Scholar]
- Earnshaw J. J., Slack R. C., Makin G. S., Hopkinson B. R. Tissue and serum concentrations of amoxycillin and clavulanic acid in patients having reconstructive vascular surgery. J Int Med Res. 1987 Jul-Aug;15(4):205–211. doi: 10.1177/030006058701500403. [DOI] [PubMed] [Google Scholar]
- Evans C., Pollock A. V. The reduction of surgical wound infections by prophylactic parenteral cephaloridine. A controlled clinical trial. Br J Surg. 1973 Jun;60(6):434–437. doi: 10.1002/bjs.1800600605. [DOI] [PubMed] [Google Scholar]
- Goldstone J., Moore W. S. Infection in vascular prostheses. Clinical manifestations and surgical management. Am J Surg. 1974 Aug;128(2):225–233. doi: 10.1016/0002-9610(74)90097-x. [DOI] [PubMed] [Google Scholar]
- Jannelli F., Cavarra G., Puccio F. Prophylaxis against infection during vascular surgery. J Cardiovasc Surg (Torino) 1984 Sep-Oct;25(5):437–439. [PubMed] [Google Scholar]
- Kaiser A. B., Clayson K. R., Mulherin J. L., Jr, Roach A. C., Allen T. R., Edwards W. H., Dale W. A. Antibiotic prophylaxis in vascular surgery. Ann Surg. 1978 Sep;188(3):283–289. doi: 10.1097/00000658-197809000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liekweg W. G., Jr, Greenfield L. J. Vascular prosthetic infections: collected experience and results of treatment. Surgery. 1977 Mar;81(3):335–342. [PubMed] [Google Scholar]
- Lorentzen J. E., Nielsen O. M., Arendrup H., Kimose H. H., Bille S., Andersen J., Jensen C. H., Jacobsen F., Røder O. C. Vascular graft infection: an analysis of sixty-two graft infections in 2411 consecutively implanted synthetic vascular grafts. Surgery. 1985 Jul;98(1):81–86. [PubMed] [Google Scholar]
- Meech P., Maclean D. M., Stephenson C. B. Postoperative infection in arterial surgery: a review of the incidence and distribution in 386 patients. Aust N Z J Surg. 1977 Dec;47(6):745–751. doi: 10.1111/j.1445-2197.1977.tb06616.x. [DOI] [PubMed] [Google Scholar]
- Pitt H. A., Postier R. G., MacGowan A. W., Frank L. W., Surmak A. J., Sitzman J. V., Bouchier-Hayes D. Prophylactic antibiotics in vascular surgery. Topical, systemic, or both? Ann Surg. 1980 Sep;192(3):356–364. doi: 10.1097/00000658-198009000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollock A. V. Surgical wound sepsis. Lancet. 1979 Jun 16;1(8129):1283–1286. doi: 10.1016/s0140-6736(79)92239-6. [DOI] [PubMed] [Google Scholar]
- Stone H. H., Haney B. B., Kolb L. D., Geheber C. E., Hooper C. A. Prophylactic and preventive antibiotic therapy: timing, duration and economics. Ann Surg. 1979 Jun;189(6):691–699. doi: 10.1097/00000658-197906000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szilagyi D. E., Smith R. F., Elliott J. P., Vrandecic M. P. Infection in arterial reconstruction with synthetic grafts. Ann Surg. 1972 Sep;176(3):321–333. doi: 10.1097/00000658-197209000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Landuyt H. W., Pyckavet M., Lambert A. M. Comparative activity of BRL 25.000 with amoxycillin against resistant clinical isolates. J Antimicrob Chemother. 1981 Jan;7(1):65–70. doi: 10.1093/jac/7.1.65. [DOI] [PubMed] [Google Scholar]
- Walker M., Litherland H. K., Murphy J., Smith J. A. Comparison of prophylactic antibiotic regimens in patients undergoing vascular surgery. J Hosp Infect. 1984 Dec;5 (Suppl A):101–106. doi: 10.1016/0195-6701(84)90039-2. [DOI] [PubMed] [Google Scholar]
- Worning A. M., Frimodt-Møller N., Ostri P., Nilsson T., Højholdt K., Frimodt-Møller C. Antibiotic prophylaxis in vascular reconstructive surgery: a double-blind placebo-controlled study. J Antimicrob Chemother. 1986 Jan;17(1):105–113. doi: 10.1093/jac/17.1.105. [DOI] [PubMed] [Google Scholar]


