Abstract
Objective To assess the effects on patients, clinicians, and the healthcare system of interventions before consultations to help patients or their representatives gather information in consultations by question asking.
Design Systematic review with meta-analysis.
Data sources Electronic literature searches of seven databases and hand searching of one journal and bibliographies of relevant articles.
Review methods Inclusion criteria included randomised controlled trials.
Main outcome measures Primary outcomes were question asking; patients’ anxiety, knowledge, and satisfaction; and length of consultation.
Results 33 randomised trials of variable quality involving 8244 patients were identified. A few studies showed positive effects. Meta-analyses showed small and statistically significantly increases in question asking (standardised mean difference 0.27, 95% confidence interval 0.19 to 0.36) and patients’ satisfaction (0.09, 0.03 to 0.16). Non-statistically significant changes occurred in patients’ anxiety before consultations (weighted mean difference −1.56, −7.10 to 3.97), patients’ anxiety after consultations (standardised mean difference −0.08, −0.22 to 0.06), patients’ knowledge (−0.34, −0.94 to 0.25), and length of consultation (0.10, −0.05 to 0.25). Interventions comprising written materials had similar effects on question asking, consultation length, and patients’ satisfaction as those comprising the coaching of patients. Interventions with additional training of clinicians had little further effect than those targeted at patients alone for patients’ satisfaction and consultation length.
Conclusions Interventions for patients before consultations produce small benefits for patients. This may be because patients and clinicians have established behaviours in consultations that are difficult to change. Alternatively small increases in question asking may not be sufficient to make notable changes to other outcomes.
Introduction
Patients want more information from doctors and nurses1 2 3 and yet the amount of information usually given is small.4 5 6 w1 Providing information is a key part of clinical care, which influences patients’ satisfaction, compliance, recall, and understanding.7 8 9 It is also associated with improved resolution of symptoms, reduced emotional distress, improved physiological status, reduced use of analgesia, reduced length of hospital stay, and improved quality of life.10 11 12 13 14 Failure to give information or providing unwanted information can cause harm.15
Information giving may be poor because clinicians might underestimate patients’ needs,5 7 16 17 18 overestimate the amount of information they give,19 lack the necessary skills,16 20 21 or use jargon.22 Furthermore, patients may feel unable to ask questions,16 23 24 25 particularly patients with serious or life threatening diseases.26 27 28
Improving information giving presents challenges. Training clinicians can be expensive and may not improve performance or other outcomes.29 30 As an adjunct or alternative, methods for helping patients identify and ask questions in consultations have been proposed, including coaching sessions,w2 videos,w3 and written materials, such as prompt sheets to encourage question asking.w4 These methods are not widely used, however, and their effectiveness is not fully understood. We undertook a systematic review to assess the effects on patients, clinicians, and the healthcare system of interventions delivered before consultations designed to help patients, or their representatives, address their information needs within consultations. We report the principal findings from our published Cochrane review on this topic.31
Methods
We used medical subject headings and text words (see www.cf.ac.uk/medic/contactsandpeople/k/SupplementaryTablesKinnersleyetal.pdf) to search several databases: Cochrane Consumers and Communication Review Group specialised register, Cochrane central register of controlled trials (Cochrane Library, Issue 3, 2006), Medline (Ovid; 1966 to September 2006), Embase (1980 to September 2006), PsycINFO (1985 to September 2006), ERIC (1966 to September 2006), and CINAHL (1982 to September 2006). The searches were done in English but we considered citations in any language and all patient groups.
Selection
We required studies to be peer reviewed publications and to be a randomised controlled trial, to involve interventions directed at patients of any age consulting with doctors or nurses in healthcare settings, and to use interventions targeted at patients, or their representatives, delivered before the consultation and aimed to help patients address their information needs by encouraging, identifying, or otherwise facilitating question asking. We included studies that also provided training for clinicians provided that this was in addition to interventions for patients.
We excluded interventions provided during consultations and other interventions such as information leaflets and diaries of symptoms unless evidence was clear that the intervention was also intended to help patients consider their information needs and ask questions.
We focused on five outcomes (question asking, satisfaction, anxiety, knowledge, consultation length) that enable assessment of effects on both the consultation process and outcomes for patients and service providers. Anxiety was measured before and after consultations. When measured before consultations, if this was at the same time as the intervention we considered it as a baseline measure rather than an outcome of the intervention. If the intervention was delivered some time before the consultation and anxiety measured separately when the patient arrived for the consultation we considered the assessment to indicate the effects of the intervention.
Two reviewers (PK and HP, RR, or NC) independently assessed electronic outputs (abstracts) and the full text articles of potentially relevant studies. We also inspected reference lists of potentially relevant studies and related reviews32 33 34 35 36 and hand searched the contents of Patient Education and Counselling from 1986 to September 2006. Disagreements were resolved by discussion or by seeking a third opinion (AE).
Data extraction and analysis
Two reviewers (PK and RR or NC) extracted data using a template covering key study characteristics. When studies used combined interventions, such as written materials and coaching, we used data on the effects of the combined intervention for the principal outcomes. We assessed the quality of studies by considering selection bias, performance bias, attrition bias, and detection bias.37 In addition we gathered data on the adequacy of randomisation, with particular attention to concealment of allocation. Intention to treat analyses were used when available.
We carried out a narrative synthesis of the included trials. We then pooled data across studies and did meta-analyses for the five main outcomes. We calculated summary estimates of the intervention effects. If the same methods and units were used we determined weighted mean differences.38 For outcomes measured using differing methods or when there was likely to be variation owing to the clinical context (for example, consultation length), we used the standardised mean differences.38 To help with the interpretations of our findings we considered effect sizes of 0.2 as small, 0.5 as moderate, and 0.8 or greater as large.39 When there was homogeneity across studies we used fixed effect models, and when there was heterogeneity we used random effect models to estimate effects. We examined potentially important effect modifiers on the outcomes measured, in particular for the effects of type of intervention (prompt sheets v coaching) and whether additional training for clinicians produced benefits. We undertook sensitivity analyses to take account of those studies without adequate concealment of allocation or that did not account for clustering in their design.
Results
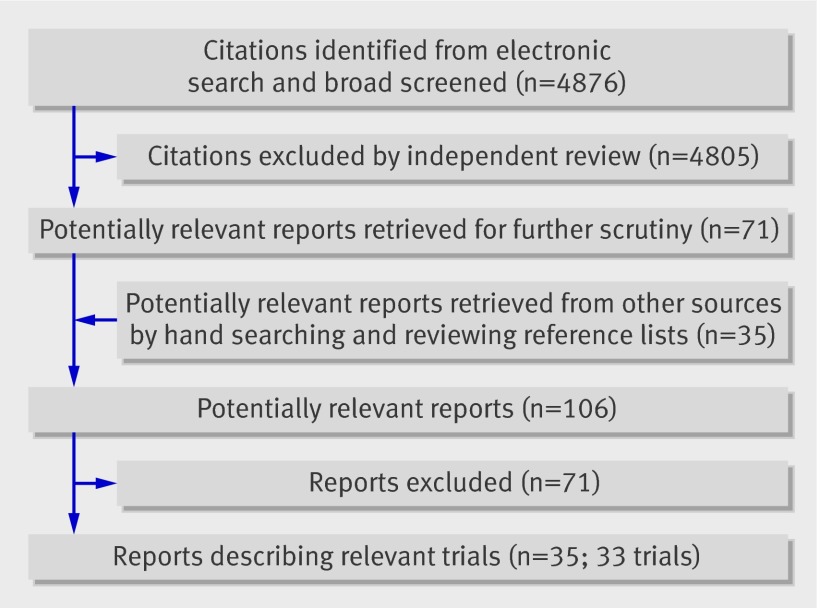
The search strategy identified 4876 citations, with 71 for possible inclusion after assessment of the full reports. Thirty five additional citations were identified from searching reference lists and from hand searching. Appraisal led to the exclusion of 71 papers, leaving 35 papersw1-w35 describing 33 trials for inclusion in the review (fig 1).
Fig 1 Flow of papers
Study characteristics and interventions
Table 1 describes the main characteristics of the 33 trials.w1-w35 All the trials were published and in English. Thirty trialsw1-w14 w16-w28 w31-w35 reported on patients consulting doctors, twow15 w29 w30 on patients consulting doctors or nurses, and onew21 on patients consulting family planning care nurses.
Table 1.
Details of included studies on interventions for patients before consultations to encourage question asking
| Study | Country | No of patients randomised | Setting | Interventions for patients | Timing | Control groups |
|---|---|---|---|---|---|---|
| Bolman 2005w5 | Netherlands | 153 | Cardiology | Question checklist before each of three consultations and training of clinicians | 1 week before consultation | General information booklet |
| Brown 1999w6 | Australia | 60 | Oncology | Question checklist; question checklist and coaching and training of clinicians | Just before consultation | Usual care |
| Brown 2001w7 | Australia | 318 | Oncology | Question checklist and training of clinicians (2×2 design) | Just before consultation | Usual care |
| Bruera 2003w8 | United States | 60 | Oncology | Question checklist | Just before consultation | General information sheet |
| Butow 1994w4 | Australia | 142 | Oncology | Question checklist | Just before consultation | General information sheet |
| Butow 2004w9 | Australia | 164 | Oncology | Question checklist | At least 2 days before consultation | General information sheet |
| Cegala 2000w10-w12 | United States | 150 | Family practice | Question checklist; brief information and coaching | 2-4 days; just before consultation | Usual care |
| Davison 1997w13 | Canada | 60 | Oncology (urology) | Question checklist and coaching | Just before consultation | General information booklet plus “social” interview |
| Davison 2002w14 | Canada | 749 | Oncology (breast cancer) | Computer program and coaching | Just before consultation | General discussion |
| Finney 1990w15 | United States | 32 | Well baby clinic | Coaching | Just before consultation | General discussion |
| Fleissig 1999w16 | United Kingdom | 1208 | Mixed outpatients | Question checklist | 2 weeks before consultation | Usual care |
| Ford 1995w1 | United Kingdom | 117 | Oncology | Audiotape of previous consultation | “Prior to” consultation | Usual care |
| Frederickson 1995w17 | United Kingdom | 80 | General practice | Question checklist | Just before consultation | Usual care |
| Greenfield 1985w18 | United States | 45 | Outpatients (peptic ulcer disease) | Coaching | Just before consultation | Discussion reviewing ulcer disease |
| Greenfield 1988w2 | United States | 73 | Diabetic clinic | Coaching (delivered before each of two linked consultations) | Just before consultation | Discussion reviewing diabetes |
| Hornberger 1997w19 | United States | 101 | Family practice | Question checklist | Just before consultation | General information sheet |
| Kidd 2004w20 | United Kingdom | 202 | Diabetic clinic | Written message; coaching; coaching and rehearsal | Just before consultation | General discussion; usual care |
| Kim 2003w21 | Indonesia | 768 | Family planning clinic | Question checklist and coaching | Just before consultation | Leaflet on HIV/AIDS plus discussion |
| Lewis 1991w3 | United States | 141 | Paediatric clinic | Video, coaching, and written materials and training of clinicians | Just before consultation | Video on bicycle safety |
| Little 2004w22 | United Kingdom | 636 | General practice | Question checklist | Just before consultation | Leaflet on depression; usual care |
| Maly 1999w23 | United States | 265 | Family practice | Question checklist (delivered twice) | Just before consultation | Asked to suggest clinic improvements |
| Martinali 2001w24 | Nether-lands | 142 | Cardiology | Question checklist | 1 week before consultation | Information booklet about heart disease |
| McCann 1996w25 w26 | United Kingdom | 120 | General practice | Question checklist | Just before consultation | Leaflet on healthy eating |
| Middleton 2006w27 | United Kingdom | 955 | General practice | Question checklist and training of clinicians (2×2 design) | Just before consultation | Usual care |
| Oliver 2001w28 | United States | 87 | Oncology | Question checklist and coaching | Just before consultation | Education on controlling cancer pain |
| Roter 1977w29 w30 | United States | 200 | Family practice | Coaching | Just before consultation | Discussion of hospital facilities |
| Sander 1996w31 | United States | 129 | Family practice | Question checklist | Just before consultation | Usual care |
| Sander 1996w31 | United States | 163 | Family practice | Coaching | Just before consultation | Usual care |
| Tabak 1988w32 | United States | 101 | Family practice | Question checklist | Just before consultation | Booklet on hospital facilities |
| Tennstedt 2000w33 | United States | 355 | Family practice (elderly) | Coaching | Up to 3 months before consultation | Usual care |
| Thompson 1990w34 | United States | 66 | Obstetrics and gynaecology | Question checklist | Just before consultation | Questionnaire about waiting room |
| Thompson 1990w34 | United States | 105 | Obstetrics and gynaecology | Question checklist; message encouraging questions | Just before consultation | Questionnaire about waiting room |
| Wilkinson 2002w35 | United States | 278 | Family practice | Question checklist | “Some time” before consultation | Usual care |
A range of interventions was used of varying complexity, with some trials comparing different interventions and some interventions having multiple components (table 1). Twenty five trialsw4-w13 w16-w17 w19-w28 w31-w35 used written materials (question prompt sheets). In six of these,w6 w13 w20 w21 w28 w33 additional coaching was provided to patients on how to ask questions. Five trialsw2 w15 w18 w29-w31 used coaching alone. In two trialsw10-w12 w20 brief instructions were used to encourage patients to ask questions. One trialw14 combined coaching with a computer program and anotherw3 combined coaching with video and written materials. One study accessed patients’ medical records of previous consultationsw23 and another used audiotapes of the previous consultation.w1 In five trialsw3 w5-w7 w27 the clinicians also received training to enable them to answer patients’ questions more effectively.
Methodological quality of included trials
The studies were of variable quality. Randomisation was by patient in 30 trials,w1 w2 w4-w18 w20-w32 w34-w35 by clinician in two trials,w3 w19 and by site of delivery of a community based intervention in one.w33 In the last three trials no attempt was made to account for clustering. Only six trialsw5-w7 w20 w22 w27 provided sample size calculations.
Four trialsw1 w22 w27 w32 provided evidence of adequate concealment of allocation. Twenty four trialsw2-w16 w18 w20 w21 w24 w25 w28-w31 w34 w35 were judged to be unclear, usually as a result of insufficient information. Five trialsw10-w12 w17 w23 w31 w33 had inadequate concealment of allocation.
In the 18 trialsw1-w4 w6-w12 w15 w18-w21 w25 w30-w32 that used audiotapes or videotapes to gather data about the consultation, sevenw2 w8 w10-w12 w15 w18 w20 w32 used assessors blind to the patient’s allocation. In addition, eight trialsw1 w2 w7 w9-w13 w19 w20 reported reliability checks using double rating of tapes. Only two trialsw7 w22 stated they used intention to treat analyses.
Quantitative data synthesis
Question asking
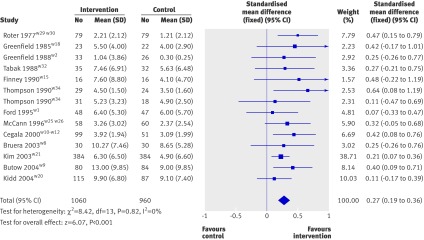
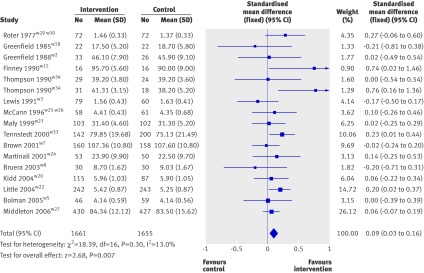
Seventeen studiesw1 w2 w6 w8-w12 w16 w18 w20 w21 w25 w26 w29 w30 w32 w34 measured question asking, with sixw6 w9-w12 w21 w29 w30 w34 finding statistically significant increases and the remainder no effects. Meta-analysis of the 14 studies with extractable data showed a small and statistically significant overall effect (standardised mean difference 0.27, 0.19 to 0.36; table 2 and fig 2).
Table 2.
Effect sizes of interventions to encourage patients to ask questions in consultations
| Outcome | No of studies | No of patients | Standardised mean difference (95% CI) |
|---|---|---|---|
| All studies | |||
| Question asking* | 14 | 2020 | 0.27 (0.19 to 0.36) |
| Patients’ satisfaction* | 17 | 3316 | 0.09 (0.03 to 0.16) |
| Anxiety before consultations | 3 | 372 | −1.56 (−7.10 to 3.97)† |
| Anxiety after consultations | 6 | 809 | −0.08 (−0.22 to 0.06) |
| Patients’ knowledge‡ | 5 | 378 | −0.34 (−0.94 to 0.25) |
| Consultation length | 13 | 3406 | 0.10 (−0.05 to 0.25) |
| Written materials v coaching | |||
| Question asking: | |||
| Written materials | 6 | 563 | 0.42 (0.26 to 0.59) |
| Coaching | 5 | 414 | 0.36 (0.16 to 0.56) |
| Patients’ satisfaction: | |||
| Written materials | 10 | 2354 | 0.08 (0.00 to 0.16) |
| Coaching | 6 | 722 | 0.23 (0.08 to 0.38) |
| Consultation length: | |||
| Written materials | 10 | 2534 | 0.13 (0.05 to 0.21) |
| Coaching | 3 | 872 | 0.07 (−0.07 to 0.20) |
| Clinicians’ training | |||
| Patients’ satisfaction: | |||
| Clinicians’ training | 3 | 821 | −0.01 (−0.15 to 0.12) |
| No clinicians’ training | 15 | 2569 | 0.13 (0.05 to 0.21) |
| Consultation length: | |||
| Clinicians’ training | 2 | 682 | 0.17 (0.01 to 0.32) |
| No clinicians’ training | 12 | 2798 | 0.17 (0.10 to 0.24) |
*Two assumptions were made about data from study by Roterw29—that number analysed in intervention and control groups for outcomes of question asking and patients’ satisfaction were equal and that means for patient’s satisfaction in the two groups were 1.46 and 1.37 and not 146 and 1.37 as stated in text.
†Weighted mean difference.
‡In two studiesw4 w18 intervention for control group could increase patients’ knowledge. Analysis was repeated with remaining three studies and a small and not statistically significant increase in knowledge was found (0.17, −0.09 to 0.43).
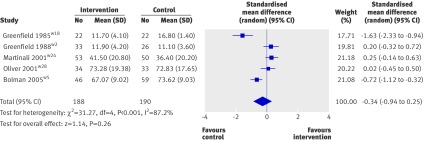
Fig 2 Effect of interventions before consultation to encourage patients to ask questions
Patients’ anxiety
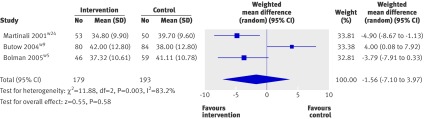
Anxiety before consultations was measured in four studies.w1 w5 w9 w24 Two studiesw5 w24 found a reduction in anxiety, onew9 an increase, and onew1 no effect. Meta-analysis of the three studies with extractable date showed a large but non-statistically significant decrease in patients’ anxiety (weighted mean difference −1.56, −7.10 to 3.97; table 2 and fig 3). In nine studiesw3 w6 w7 w13 w19 w22 w28 w34 anxiety was measured after the index consultation, with two studiesw19 w34 reporting a reduction in patient anxiety, onew7 an increase, and sixw3 w6 w13 w22 w28 w34 no effect. Meta-analysis of the six studies with extractable data showed a small and non-statistically significant decrease (standardised mean difference −0.08, −0.22 to 0.06; table 2 and fig 4).
Fig 3 Effect on patients’ anxiety before consultations of interventions to encourage patients to ask questions in consultations
Fig 4 Effect on patients’ anxiety after consultations of interventions to encourage patients to ask question in consultations
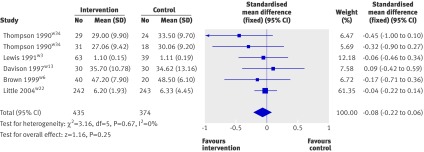
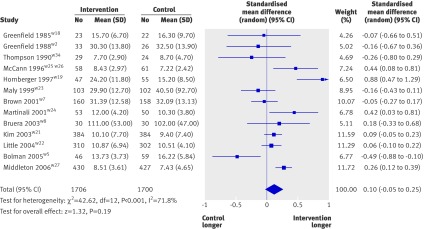
Patients’ knowledge
Patients’ knowledge was measured in five studies. Reductions in knowledge were found in two studiesw2 w5 and no change in three.w18 w24 w28 In both the studies showing a decrease in knowledge, the intervention for the control group could have increased patients’ knowledge, which might have affected the results. Meta-analysis of all five studies assessing knowledge found a small and non-statistically significant decrease (standardised mean difference −0.34, −0.94 to 0.25; table 2 and fig 5). This result was not substantially altered when the two studies of concern were removed from this meta-analysis (−0.26, −0.52 to 0.01; see www.cf.ac.uk/medic/contactsandpeople/k/SupplementaryTablesKinnersleyetal.pdf).
Fig 5 Effect on patients’ knowledge of interventions to encourage patients to ask questions in consultations
Patients’ satisfaction
Patients’ satisfaction was measured in 23 studies. In 14 studiesw2 w4 w5-w9 w14 w19 w24-w26 w28 w34 no changes were found and in fivew16 w22 w23 w29 w30 w34 satisfaction increased.w16 w22 w23 w29 w30 w34 In two additional studies increases occurred only for particular aspects of satisfaction (depth of relationship,w27 interpersonal satisfactionw33). In one studyw3 the satisfaction of child patients was increased but parental satisfaction was unchanged. No immediate effect was found in another trial,w20 but satisfaction was increased at three months. Meta-analysis of 17 studies with extractable data for overall satisfaction immediately after consultation showed a small and statistically significant increase (standardised mean difference 0.09, 0.03 to 0.16; fig 6).
Fig 6 Effect on patients’ satisfaction of interventions to encourage patients to ask questions in consultations
Length of consultations
Seventeen studiesw1 w2 w4 w7-w9 w18 w19 w21-w27 w29 w30 w34 measured the length of consultations; threew19 w25-w27 found statistically significant increases in length and 13w1 w2 w4 w7-w9 w18 w21-w24 w29 w30 w34 no effect. In the study by Bolmanw5 the length of the first of three linked consultations was decreased whereas the third was increased. Meta-analysis of 13 studies with extractable data on the effects of intervention on consultation length found a small and non-statistically significant increase (standardised mean difference 0.10, −0.05 to 0.25; fig 7).
Fig 7 Effect on consultation length of interventions to encourage patients to ask questions in consultations
To explore the effects of inadequate concealment of allocation and of clustering, effects and confidence intervals were recalculated without the five trialsw10-w12 w17 w23 w31 w33 considered to have inadequate concealment (table 3) and the three studiesw3 w19 w33 that used randomisation by clinician (table 4) as these cluster randomised trials may have overestimated effects. Recalculation resulted in small changes. Other studies might have been vulnerable to clustering effects, and the reported standard errors and confidence intervals may be overestimates.
Table 3.
Comparison of meta-analyses with and without data from studies judged to have inadequate concealment of allocation
| Comparison | Effect size all data (95% CI) | Effect size without inadequate studies (95% CI) |
|---|---|---|
| Intervention v control: | ||
| Question asking | 0.27 (0.19 to 0.36) | 0.26 (0.17 to 0.35) |
| Patient satisfaction | 0.09 (0.03 to 0.16) | 0.10 (0.03 to 0.17) |
| Consultation length | 0.10 (−0.05 to 0.25) | 0.12 (−0.03 to 0.28) |
| Written materials v coaching: | ||
| Written materials: question asking | 0.42 (0.26 to 0.59) | 0.37 (0.18 to 0.55) |
| Written materials: satisfaction | 0.08 (0.00 to 0.16) | 0.09 (0.00 to 0.17) |
| Coaching: satisfaction | 0.23 (0.08 to 0.38) | 0.18 (−0.03 to 0.39) |
| Written materials: consultation length | 0.13 (0.05 to 0.21) | 0.16 (0.08 to 0.24) |
| Clinician training: | ||
| Not trained: satisfaction | 0.13 (0.05 to 0.21) | 0.12 (0.04 to 0.21) |
| Not trained: consultation length | 0.17 (0.10 to 0.24) | 0.17 (0.09 to 0.24) |
Table 4.
Comparison of meta-analyses with and without clustered data
| Comparison | Effect size all data (95% CI) | Effect size without clustered studies (95% CI) |
|---|---|---|
| Intervention v control: | ||
| Anxiety (after consultations) | −0.08 (−0.22 to 0.06) | −0.09 (−0.23 to 0.06) |
| Patients’ satisfaction | 0.09 (0.03 to 0.16) | 0.09 (0.02 to 0.16) |
| Consultation length | 0.10 (−0.05 to 0.25) | 0.05 (−0.08 to 0.18) |
| Written materials v coaching: | ||
| Coaching: satisfaction | 0.23 (0.08 to 0.38) | 0.18 (−0.03 to 0.39) |
| Written materials: consultation length | 0.13 (0.05 to 0.21) | 0.10 (0.02 to 0.18) |
| Clinicians’ training: | ||
| Trained: satisfaction | −0.01 (−0.15 to 0.12) | 0.02 (−0.14 to 0.17) |
| Not trained: satisfaction | 0.13 (0.05 to 0.21) | 0.12 (0.03 to 0.20) |
| Not trained: consultation length | 0.17 (0.10 to 0.24) | 0.15 (0.07 to 0.22) |
Effect modifiers
Similar small to moderate and statistically significant increases were found in question asking for written materials (standardised mean difference 0.42, 0.26 to 0.59) and for coaching (0.36, 0.16 to 0.56; see www.cf.ac.uk/medic/contactsandpeople/k/SupplementaryTablesKinnersleyetal.pdf). Written materials led to a small and statistically significant increase in length of consultations (0.13, 0.05 to 0.21), and coaching produced a smaller, non-significant, change (0.07, −0.07 to 0.20; see www.cf.ac.uk/medic/contactsandpeople/k/SupplementaryTablesKinnersleyetal.pdf). Written materials produced a small increase in patients’ satisfaction that was of borderline statistical significance (0.08, 0.00 to 0.16) and for coaching the effect was a small but statistically significant increase (0.23, 0.08 to 0.38; see www.cf.ac.uk/medic/contactsandpeople/k/SupplementaryTablesKinnersleyetal.pdf). The confidence intervals for the analyses of the effects of different types of interventions for all these analyses overlapped (table 2). This suggests that written materials and coaching have similar effects.
Three studiesw3 w7 w27 considered the additional effects of training clinicians and had extractable data on the effects of combined interventions (targeted at patients and clinicians) on consultation length and patients’ satisfaction (control patients received usual care). Additional training had little impact on consultation length compared with patient only interventions (combined 0.17, 0.01 to 0.32 v patient only 0.17, 0.10 to 0.24; see www.cf.ac.uk/medic/contactsandpeople/k/SupplementaryTablesKinnersleyetal.pdf); the corresponding values for patients’ satisfaction were 0.08 (−0.06 to 0.22) and 0.13 (0.05 to 0.21; see www.cf.ac.uk/medic/contactsandpeople/k/SupplementaryTablesKinnersleyetal.pdf). The confidence intervals for these analyses overlapped.
Two studiesw5 w27 assessed the impact of interventions directed at patients in the context of all clinicians receiving training (intervention and control groups). In one studyw5 the intervention produced a small non-statistically significant decrease in consultation length and no effect on patients’ satisfaction (consultation length −0.49, −0.88 to −0.10, patient satisfaction 0.00, −0.39 to 0.39). The other studyw27 showed a small increase in consultation length (0.24, −0.05 to 0.43) and little effect on patient satisfaction (0.03, −0.16 to 0.22).
Although the evidence from these two analyses is limited it could be concluded that providing clinicians with training either combined with interventions directed at patients or delivered before the implementation of interventions directed at patients has no clear benefits.
Similar results to the main analyses were found when the analyses of effect modifiers were repeated without those trials considered to have inadequate allocation concealment and those that randomised by clinician (tables 3 and 4).
Discussion
Thirty three randomised trials of interventions to help patients ask questions and gather information in consultations in a range of settings and countries were identified. Meta-analyses showed that the interventions resulted in small but statistically significant increases in question asking and patients’ satisfaction, a large but not statistically significant decrease in anxiety before consultations, and small but not statistically significant effects on anxiety after consultations and length of consultations. The effects of the interventions on patients’ knowledge are unclear owing to methodological difficulties.
Strengths and weaknesses
We identified a large number of trials that aimed to improve the amount and content of information patients obtain during consultations. We used a comprehensive, externally peer reviewed, search strategy, which identified more trials than other related reviews of broader study designs.32 33 34 35 36 We also clarified published data with the authors. No other review has carried out meta-analyses of these trials as far as we are aware and because the number of trials is relatively large, the new data clarify the effects of the interventions. Other reviews in this area are broadly supportive of interventions to promote information gathering by patients, identifying a range of beneficial outcomes.32 33 Our meta-analyses allowed formal statistical evaluation of the data and suggest that the evidence of benefits is less compelling.
Despite our efforts to search comprehensively we may have missed some studies. Although we contacted authors we only identified published trials for inclusion in the review. Unpublished studies would more likely have shown null results and so our findings may overestimate the effects of interventions. Furthermore, an English language bias may exist because of the databases searched. We restricted the review to studies of patients consulting doctors or nurses but it is possible that interventions have been tested in patients consulting other health professionals. However, as doctors and nurses are considered by patients to be their main source of information about major illnesses, we believe that we have reviewed the most important area of relevant literature. In our meta-analyses we combined the effects of interventions across varied settings (primary and secondary care, short and long consultations). Individual interventions may perform better in particular settings and the process of combining studies may lose an element of specificity in attempting to produce a generalisable example.
The increase in question asking we found shows a direct effect of the interventions and that simple interventions can influence the clinical dialogue. The small increase in patients’ satisfaction is consistent with other reports of benefits from patient centred consulting styles.40 41 42 A possible explanation for the limited effects is that many clinicians and patients adopt ritualised styles of consulting on the basis of previous experience.43 These may not be readily changed by interventions, particularly if delivered only once, immediately before the consultation, as part of research projects, and targeted at only one participant in the consultation. The possibility that interventions could reduce patients’ anxiety before consultations is of interest but the data we reviewed on this are inconclusive. Patients attending consultations may feel uncertain about getting an opportunity to express their concerns. Enabling them to organise their thoughts by considering the questions they might want to ask may reduce anxiety. One study,w9 however, which involved patients with cancer showed an increase in anxiety. Another studyw5 found that fewer patients used the intervention at successive consultations and that anxiety increased before each successive consultation. Anxiety may not improve and may even increase if clinicians do not respond appropriately to questions asked by patients. Secondly, anxiety may increase if the information given in response to a question is worrying. This would be particularly likely, for example, in oncology clinics (nine included studies). We expected that the interventions in this review would foster a sense of control because patients would have identified and possibly practised asking questions. This preparation may have disturbed the delicate balance of power and authority in the consultation, however, and generated difficulties for patients so that they moved back to their usual mode of consulting. The latter phenomenon has also been identified in, for example, studies of the use of information from the internet in consultations.44 More intense interventions such as coaching had few additional benefits over simpler written interventions that required little clinic time to administer. It has been suggestedw9 w16 w29 that interventions would be more effective if supported by training of clinicians. We found no consistent evidence for this from the small number of studies available.
Although evidence is lacking of an increase in consultation length as a result of the interventions, the data could be considered to indicate a trend to longer consultations. It would not be surprising if encouraging patients to ask questions were to lead to an increase in length of consultations, and because of this clinicians might be concerned about the interventions. Data analysed from 17 studies, however, provide some reassurance as these interventions do not lead to sizeable increases in length of consultations. No study explored whether the time within the consultation was spent differently (with overall length remaining unchanged) although this has been found with patient centred interventions in other specialties.45 How the clinician and patient use the time may be as important as the amount of time itself.46
Some patients might find the interventions more helpful than others. Many of the studies were set in oncology clinics. This may reflect oncologists’ interest in providing information to patients and the complex information needs of patients with cancer.47 Two studiesw10-w12 w25-w26 explored the impact of the interventions on different patient groups, showing that young white educated patients from the middle classes, asked more questions than other groups. Further research is needed to identify those patients in whom interventions are likely to be most beneficial. Studies should also assess the possible harms of such interventions—for example, increasing specific anxieties or disparities of access and care across groups. In this review no study explored the use of the same intervention in different settings.
Encouraging patients to participate actively in consultations is an important aspect of patient centred care.48 If, as the evidence here suggests, interventions to help patients address their information needs lead to increases in question asking but little other benefit, it casts doubt on what has been considered an important approach to patient care. Further research is needed before a final conclusion can be reached. In particular, more studies need to be undertaken in which the strength of the intervention is maximised. The goal would be to change the overall culture of the consultation, with patients empowered through question prompt sheets and other interventions that are clearly part of usual care, rather than one-off interventions delivered just before consultations. Similarly, studies should explore more targeted and intensive training for clinicians in parallel with interventions directed at patients and evaluate more thoroughly the effects of their training particularly for providing patients with the information they want. If patients were encouraged routinely to identify questions for their clinicians before consultations, and if clinicians were routinely and effectively trained to address patients’ concerns, it is likely that both patients and clinicians would benefit.
Conclusions
The benefits of the interventions reviewed here are limited. Focusing on the patient alone may not produce long term benefits for patients because of the complexity of the dialogue between patients and clinicians.49 Successful consultations require that patients and clinicians agree on the nature of the problem and what could and should be done.48 50 The interventions reviewed here may assist information exchange. Decision making must be shared, however, and clinicians need to be sufficiently flexible to respond to the varying preferences for information and involvement of different patients or of the same patient in different circumstances.51 52 53 54 Thus a combined approach is probably required in which willing patients are encouraged and helped to participate in their consultations, and clinicians have the skills to identify and adapt to the needs of their patients.
What is already known on this topic
Patients often struggle to ask questions in consultations or get appropriate answers
Studies suggest that prompt sheets or coaching to ask questions might be effective
What this study adds
Question asking and patients’ satisfaction increase with use of prompt sheets and coaching but evidence of other benefits is small
Other interventions might also be needed to help patients gather information from their clinicians
We thank the staff and editors of the Cochrane Consumers and Communication Review Group, particularly Megan Prictor for her overall advice; Sophie Hill (coordinating editor of the review group); Dell Horey (contact editor for the review); Dominique Broclain (contact editor for the protocol); Judy Stoelwinder (former search coordinator for the trials) for her help with the search strategy; Damien Jolley and Kelly Allen for their statistical feedback; Diane Owen for her help with data extraction; other editors and external peer reviewers for their comments; and the following consumers for their helpful feedback: Janine Cooper-Marshall, Pat Oliver, Iris Mackenzie, Peter Palmer, and Richard Berry (University of Wales College of Medicine Simulated Patients); from Amy Zelmer, Nete Villebro, Rosemary Humphreys, Amy Arkle, and Judi Strid (consumer representatives of the Cochrane Consumer and Communication Group). The initial idea for this work came when Paul Kinnersley was working in Australia funded by a grant from the PPP Foundation (now the Health Foundation).
Contributors: PK conceived the study and is guarantor. PK, RR, HP, and NC did the literature searches and reviewed the abstracts. KH directed the meta-analyses. All authors interpreted the results and were involved in the production of the manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not for profit sectors.
Competing interests: PK directs a university unit that generates income by delivering training in communication skills to clinicians.
Ethical approval: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Cite this as: BMJ 2008;337:a485
References
- 1.Boreham P, Gibson D. The informative process in private medical consultations: a preliminary investigation. Soc Sci Med 1978;12(5A):409-16. [PubMed] [Google Scholar]
- 2.Jenkins V, Fallowfield L, Saul J. Information needs of patients with cancer: results from a large study in UK cancer centres. Br J Cancer 2001;84:48-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boberg EW, Gustafson DH, Hawkins RP, Offord KP, Koch C, Wen KY, et al. Assessing the unmet information, support and care delivery needs of men with prostate cancer. Patient Educ Couns 2003;49:233-42. [DOI] [PubMed] [Google Scholar]
- 4.Svarstad BL. The doctor-patient encounter: an observational study of communication and outcome. Doctoral dissertation. University of Wisconsin, 1974.
- 5.Waitzkin H. Doctor-patient communication: clinical implications of social scientific research. JAMA 1984;252:2441-6. [DOI] [PubMed] [Google Scholar]
- 6.Maguire P, Booth K, Elliott C, Jones B. Helping health professionals involved in cancer care acquire key interviewing skills—the impact of workshops. Eur J Cancer 1996;32A:1486-8. [DOI] [PubMed]
- 7.Faden RR, Becker C, Lewis C, Freeman J, Faden AI. Disclosure of information to patients in medical care. Med Care 1981;19:718-33. [DOI] [PubMed] [Google Scholar]
- 8.Deyo RA, Diehl AK. Patient satisfaction with medical care for low back pain. Spine 1986;11:28-30. [DOI] [PubMed] [Google Scholar]
- 9.Hall JA, Roter DL, Katz NR. Meta-analysis of correlates of provider behavior in medical encounters. Med Care 1988;26:657-75. [DOI] [PubMed] [Google Scholar]
- 10.Egbert LD, Batitt GE, Welch CE. Reduction of postoperative pain by encouragement and instruction of patients. N Engl J Med 1964;270:825-7. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan SH, Greenfield S, Ware JE. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care 1989;27:S110-27. [DOI] [PubMed] [Google Scholar]
- 12.Fallowfield LJ, Hall A, Maguire P, Baum M, A’Hern RP. Psychological effects of being offered choice of surgery for breast cancer. BMJ 1994;309:448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roter DL, Hall JA, Kern De, Barker LR, Cole KA, Roca RP. Improving physicians’ interviewing skills and reducing patients’ emotional distress: a randomized controlled trial. Arch Intern Med 1995;155:1877-84. [PubMed] [Google Scholar]
- 14.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ 1995;152:1423-33. [PMC free article] [PubMed] [Google Scholar]
- 15.Fallowfield L, Jenkins V. Effective communication skills are the key to good cancer care. Eur J Cancer 1999;35:1592-7. [DOI] [PubMed] [Google Scholar]
- 16.Tuckett D, Boulton M, Olson I, Williams A. Meetings between experts: an approach to sharing ideas in medical consultations. London: Tavistock, 1985.
- 17.Kindelan K, Kent G. Concordance between patients’ information preferences and general practitioners’ perceptions. Psychol Health 1987;1:399-409. [Google Scholar]
- 18.Beisecker AE, Beisecker TD. Patient information-seeking behaviours when communicating with doctors. Med Care 1990;28:19-28. [DOI] [PubMed] [Google Scholar]
- 19.Makoul G, Arnston P, Schofield T. Health promotion in primary care: physician-patient communication and decision making about prescription medications. Soc Sci Med 1995;41:1241-54. [DOI] [PubMed] [Google Scholar]
- 20.Maguire P, Fairbairn S, Fletcher C. Consultation skills of young doctors. 1. Benefits of feedback training in interviewing as students persist. BMJ 1986;292:1573-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jenkins V, Fallowfield L. Can communication skills training alter physicians’ beliefs and behavior in clinics? J Clin Oncol 2002;20:765-9. [DOI] [PubMed] [Google Scholar]
- 22.Korsch BM, Gozzi EK, Francis V. Gaps in doctor-patient communication. Pediatrics 1968;42:855-71. [PubMed] [Google Scholar]
- 23.Stimson GV, Webb B. Going to see the doctor: the consultation process in general practice. London: Routledge and Kegan Paul, 1975.
- 24.Leydon GM, Boulton M, Moynihan C, Jones A, Mossman J, Boudioni M, et al. Cancer patients’ information needs and information seeking behaviour: in depth interview study. BMJ 2000;320:909-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McKenzie J. Information needs of patients with cancer: similar study had similar findings. BMJ 2000;321:632. [PubMed] [Google Scholar]
- 26.Silverman J, Kurtz S, Draper J. Skills for communicating with patients. Abingdon: Radcliffe Medical Press, 2005.
- 27.Fleissig A. Patients are frightened and their information needs fluctuate. BMJ 2000;321:632. [PMC free article] [PubMed] [Google Scholar]
- 28.Jefford M, Tattersall MH. Informing and involving cancer patients in their own care. Lancet Oncol 2002;3:629-37. [DOI] [PubMed] [Google Scholar]
- 29.Fallowfield L, Jenkins V, Farewell V, Saul J, Duffy A, Eves R. Efficacy of a Cancer Research UK communication skills training model for oncologists: a randomised controlled trial. Lancet 2002;359:650-6. [DOI] [PubMed] [Google Scholar]
- 30.Kramer AWM, Dusman H, Tan LHC, Jansen JJM, Grol RPTM, van der Vleuten CPM. Acquisition of communication skills in postgraduate training for general practice. Med Educ 2004;38:158-67. [DOI] [PubMed] [Google Scholar]
- 31.Kinnersley P, Edwards A, Hood K, Cadbury N, Ryan R, Prout H, et al. Interventions before consultations for helping patients address their information needs. Cochrane Database Syst Rev 2007, Issue 3. Art No CD004565. 10.1002/14651858.CD004565.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cegala DJ. Patient communication skills training: a review with implications for cancer patients. Patient Educ Couns 2003;50:91-4. [DOI] [PubMed] [Google Scholar]
- 33.Harrington J, Noble LM, Newman SP. Improving patients’ communication with doctors: a systematic review of intervention studies. Patient Educ Counsel 2004;52:7-16. [DOI] [PubMed] [Google Scholar]
- 34.Anderson LA, Sharpe PA. Improving patient and provider communication: a synthesis and review of communication interventions. Patient Educ Counsel 1991;17:99-134. [Google Scholar]
- 35.Jadad AR. Asking patients to write lists. BMJ 1995;311:746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gaston CM, Mitchell G. Information giving and decision-making in patients with advanced cancer: a systematic review. Soc Sci Med 2005;61:2252-64. [DOI] [PubMed] [Google Scholar]
- 37.In: Clarke M, Oxman AD, eds. Cochrane Reviewers’ Handbook 4.2.0 [updated March 2003]. In: Cochrane Library, Issue 2. Oxford: Update Software, 2003.
- 38.Higgins JPT, Green S, ed. Cochrane handbook for systematic reviews of interventions 4.2.6 [Updated September 2006]. In: Cochrane Library. Chichester, UK: Wiley, 2006.
- 39.Cohen J. Statistical power analysis for the behavioural sciences. Hillsdale, NJ: Lawrence Erlbaum, 1988.
- 40.Kinnersley P, Stott N, Peters TJ, Harvey I. The patient-centredness of consultations and outcome in primary care. Br J Gen Pract 1999;49:711-6. [PMC free article] [PubMed] [Google Scholar]
- 41.Krupat E, Rosenkranz SL, Yeager CM, Barnard K, Putnam SM, Inui TS. The practice orientations of physicians and patients: the effect of doctor-patient congruence on satisfaction. Patient Educ Counsel 2000;39:49-59. [DOI] [PubMed] [Google Scholar]
- 42.Lewin SA, Skea ZC, Entwistle V, Zwarenstein M, Dick J. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2001, Issue 4. Art No CD003267. 10.1002/14651858.CD003267. [DOI] [PubMed] [Google Scholar]
- 43.Neighbour R. The inner consultation. Abingdon: Radcliffe, 2004.
- 44.Kivits J. Informed patients and the internet: a mediated health context for consultations with health professionals. J Health Psychol 2006;11:269-82. [DOI] [PubMed] [Google Scholar]
- 45.Edwards A, Gray J, Clarke A, Dundon J, Elwyn G, Gaff C, et al. Interventions to improve risk communication in clinical genetics: systematic review. Patient Educ Counsel 2008;7:4-25. [DOI] [PubMed] [Google Scholar]
- 46.Wilson A, Childs S. The relationship between consultation length, process and outcomes in general practice: a systematic review. Br J Gen Pract 2002;52:1012-20. [PMC free article] [PubMed] [Google Scholar]
- 47.Leydon GM, Boulton M, Moynihan C, Jones A, Mossman J, Boudioni M, et al. Faith, hope, and charity: an in-depth interview study of cancer patients’ information needs and information-seeking behavior. West J Med 2000;173:26-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ 1995;152:1423-33. [PMC free article] [PubMed] [Google Scholar]
- 49.Roter D. The enduring and evolving nature of the patient-physician relationship. Patient Educ Counsel 2000;39:5-15. [DOI] [PubMed] [Google Scholar]
- 50.Starfield B, Wray C, Hess K, Gross R, Birk PS, D’Lugoff BC. The influence of patient-practitioner agreement on outcome of care. Am J Public Health 1981;71:127-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Elwyn G, Edwards A, Kinnersley P. Shared decision making in primary care: the neglected second half of the consultation. Br J Gen Pract 1999;49:477-82. [PMC free article] [PubMed] [Google Scholar]
- 52.Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pract 2000;50:892-7. [PMC free article] [PubMed] [Google Scholar]
- 53.Fleissig A. Patients are frightened and their information needs fluctuate. BMJ 2000;321:632. [PMC free article] [PubMed] [Google Scholar]
- 54.Edwards A, Elwyn G. Inside the black box of shared decision making—distinguishing between the process of involvement and who makes the decision. Health Expect 2006;9:307-20. [DOI] [PMC free article] [PubMed] [Google Scholar]